
- •Preface and Acknowledgments
- •Contents
- •Contributors
- •1: Embryology for Urologists
- •Introduction
- •Renal Development
- •Pronephros
- •Mesonephros
- •Metanephros
- •Development of the Collecting System
- •Critical Steps in Further Development
- •Anomalies of the Kidney
- •Renal Agenesis
- •Renal Aplasia
- •Renal Hypoplasia
- •Renal Ectopia
- •Renal Fusion
- •Ureteral Development
- •Anomalies of Origin
- •Anomalies of Number
- •Incomplete Ureteral Duplication
- •Complete Ureteral Duplication
- •Ureteral Ectopia
- •Embryology of Ectopia
- •Clinical Correlation
- •Location of Ectopic Ureteral Orifices – Male (in Descending Order According to Incidence)
- •Symptoms
- •Ureteroceles
- •Congenital Ureteral Obstruction
- •Pipestem Ureter
- •Megaureter-Megacystis Syndrome
- •Prune Belly Syndrome
- •Vascular Ureteral Obstructions
- •Division of the Urogenital Sinus
- •Bladder Development
- •Urachal Anomalies
- •Cloacal Duct Anomalies
- •Other Bladder Anomalies
- •Bladder Diverticula
- •Bladder Extrophy
- •Gonadal Development
- •Testicular Differentiation
- •Ovarian Differentiation
- •Gonadal Anomalies
- •Genital Duct System
- •Disorders of Testicular Function
- •Female Ductal Development
- •Prostatic Urethral Valves
- •Gonadal Duct Anomalies
- •External Genital Development
- •Male External Genital Development
- •Female External Genital Development
- •Anomalies of the External Genitalia
- •References
- •2: Gross and Laparoscopic Anatomy of the Upper Urinary Tract and Retroperitoneum
- •Overview
- •The Kidneys
- •The Renal Vasculature
- •The Renal Collecting System
- •The Ureters
- •Retroperitoneal Lymphatics
- •Retroperitoneal Nerves
- •The Adrenal Glands
- •References
- •3: Gross and Laparoscopic Anatomy of the Lower Urinary Tract and Pelvis
- •Introduction
- •Female Pelvis
- •Male Pelvis
- •Pelvic Floor
- •Urinary Bladder
- •Urethra
- •Male Urethra
- •Female Urethra
- •Sphincter Mechanisms
- •The Bladder Neck Component
- •The Urethral Wall Component
- •The External Urethral Sphincter
- •Summary
- •References
- •4: Anatomy of the Male Reproductive System
- •Testis and Scrotum
- •Spermatogenesis
- •Hormonal Regulation of Spermatogenesis
- •Genetic Regulation of Spermatogenesis
- •Epididymis and Ductus Deferens
- •Accessory Sex Glands
- •Prostate
- •Seminal Vesicles
- •Bulbourethral Glands
- •Penis
- •Erection and Ejaculation
- •References
- •5: Imaging of the Upper Tracts
- •Anatomy of the Upper Tracts and Introduction to Imaging Modalities
- •Introduction
- •Renal Upper Tract Basic Anatomy
- •Modalities Used for Imaging the Upper Tracts
- •Ultrasound
- •Radiation Issues
- •Contrast Issues
- •Renal and Upper Tract Tumors
- •Benign Renal Tumors
- •Transitional Cell Carcinoma
- •Renal Mass Biopsy
- •Renal Stone Disease
- •Ultrasound
- •Plain Radiographs and IVU
- •Renal Cystic Disease
- •Benign Renal Cysts
- •Hereditary Renal Cystic Disease
- •Complex Renal Cysts
- •Renal Trauma
- •References
- •Introduction
- •Pathophysiology
- •Susceptibility and Resistance
- •Epidemiological Breakpoints
- •Clinical Breakpoints
- •Pharmacodynamic Parameters
- •Pharmacokinetic Parameters
- •Fosfomycin
- •Nitrofurantoin
- •Pivmecillinam
- •b-Lactam-Antibiotics
- •Penicillins
- •Cephalosporins
- •Carbapenems
- •Aminoglycosides
- •Fluoroquinolones
- •Trimethoprim, Cotrimoxazole
- •Glycopeptides
- •Linezolid
- •Conclusion
- •References
- •7: An Overview of Renal Physiology
- •Introduction
- •Body Fluid Compartments
- •Regulation of Potassium Balance
- •Regulation of Acid–Base Balance
- •Diuretics
- •Suggested Reading
- •8: Ureteral Physiology and Pharmacology
- •Ureteral Anatomy
- •Modulation of Peristalsis
- •Ureteral Pharmacology
- •Conclusion
- •References
- •Introduction
- •Afferent Signaling Pathways
- •Efferent Signaling
- •Parasympathetic Nerves
- •Sympathetic Nerves
- •Vesico-Spinal-Vesical Micturition Reflex
- •Peripheral Targets
- •Afferent Signaling Mechanisms
- •Urothelium
- •Myocytes
- •Cholinergic Receptors
- •Muscarinic Receptors
- •Nicotinic Receptors
- •Adrenergic Receptors (ARs)
- •a-Adrenoceptors
- •b-Adrenoceptors
- •Transient Receptor Potential (TRP) Receptors
- •Phosphodiesterases (PDEs)
- •CNS Targets
- •Opioid Receptors
- •Serotonin (5-HT) Mechanisms
- •g-Amino Butyric Acid (GABA) Mechanisms
- •Gabapentin
- •Neurokinin and Neurokinin Receptors
- •Summary
- •References
- •10: Pharmacology of Sexual Function
- •Introduction
- •Sexual Desire/Arousal
- •Endocrinology
- •Steroids in the Male
- •Steroids in the Female
- •Neurohormones
- •Neurotransmitters
- •Dopamine
- •Serotonin
- •Pharmacological Strategies
- •CNS Drugs
- •Enzyme-inducing Antiepileptic Drugs
- •Erectile Function
- •Ejaculatory Function
- •Premature Ejaculation
- •Abnormal Ejaculation
- •Conclusions
- •References
- •Epidemiology
- •Calcium-Based Urolithiasis
- •Uric Acid Urolithiasis
- •Infectious Urolithiasis
- •Cystine-Based Urolithiasis
- •Aims
- •Who Deserves Metabolic Evaluation?
- •Metabolic Workup for Stone Producers
- •Medical History and Physical Examination
- •Stone Analysis
- •Serum Chemistry
- •Urine Evaluation
- •Urine Cultures
- •Urinalysis
- •Twenty-Four Hour Urine Collections
- •Radiologic Imaging
- •Medical Management
- •Conservative Management
- •Increased Fluid Intake
- •Citrus Juices
- •Dietary Restrictions
- •Restricted Oxalate Diet
- •Conservative Measures
- •Selective Medical Therapy
- •Absorptive Hypercalciuria
- •Thiazide
- •Orthophosphate
- •Renal Hypercalciuria
- •Primary Hyperparathyroidism
- •Hyperuricosuric Calcium Oxalate Nephrolithiasis
- •Enteric Hyperoxaluria
- •Hypocitraturic Calcium Oxalate Nephrolithiasis
- •Distal Renal Tubular Acidosis
- •Chronic Diarrheal States
- •Thiazide-Induced Hypocitraturia
- •Idiopathic Hypocitraturic Calcium Oxalate Nephrolithiasis
- •Hypomagnesiuric Calcium Nephrolithiasis
- •Gouty Diathesis
- •Cystinuria
- •Infection Lithiasis
- •Summary
- •References
- •12: Molecular Biology for Urologists
- •Introduction
- •Inherited Changes in Cancer Cells
- •VEGR and Cell Signaling
- •Targeting mTOR
- •Conclusion
- •References
- •13: Chemotherapeutic Agents for Urologic Oncology
- •Introduction
- •Bladder Cancer
- •Muscle Invasive Bladder Cancer
- •Metastatic Bladder Cancer
- •Conclusion
- •Prostate Cancer
- •Other Chemotherapeutic Drugs or Combinations for Treating HRPC
- •Conclusion
- •Renal Cell Carcinoma
- •Chemotherapy
- •Immunotherapy
- •Angiogenesis Inhibitor Drugs
- •Conclusion
- •Testicular Cancer
- •Stage I Seminoma
- •Stage I non-seminomatous Germ Cell Tumours (NSGCT)
- •Metastatic Germ Cell Tumours
- •Low-Volume Metastatic Disease (Stage II A/B)
- •Advanced Metastatic Disease
- •Salvage Chemotherapy for Relapsed or Refractory Disease
- •Conclusion
- •Penile Cancer
- •Side Effects of Chemotherapy
- •Conclusion
- •References
- •14: Tumor and Transplant Immunology
- •Antibodies
- •Cytotoxic and T-helper Cells
- •Immunosuppression
- •Induction Therapy
- •Maintenance Therapy
- •Rejection
- •Posttransplant Lymphoproliferative Disease
- •Summary
- •References
- •15: Pathophysiology of Renal Obstruction
- •Causes of Renal Obstruction
- •Effects on Prenatal Development
- •Prenatal Hydronephrosis
- •Spectrum of Renal Abnormalities
- •Renal Functional Changes
- •Renal Growth/Counterbalance
- •Vascular Changes
- •Inflammatory Mediators
- •Glomerular Development Changes
- •Mechanical Stretch of Renal Tubules
- •Unilateral Versus Bilateral
- •Limitations of Animal Models
- •Future Research
- •Issues in Patient Management
- •Diagnostic Imaging
- •Ultrasound
- •Intravenous Urography
- •Antegrade Urography and the Whitaker Test
- •Nuclear Renography
- •Computed Tomography
- •Magnetic Resonance Urography
- •Hypertension
- •Postobstructive Diuresis
- •References
- •Introduction
- •The Normal Lower Urinary Tract
- •Anatomy
- •Storage Function
- •Voiding Function
- •Neural Control
- •Symptoms
- •Flow Rate and Post-void Residual
- •Voiding Cystometry
- •Male
- •Female
- •Neurourology
- •Conclusions
- •References
- •17: Urologic Endocrinology
- •The Testis
- •Normal Androgen Metabolism
- •Epidemiological Aspects
- •Prostate
- •Brain
- •Muscle Mass and Adipose Tissue
- •Bones
- •Ematopoiesis
- •Metabolism
- •Cardiovascular System
- •Clinical Assessment
- •Biochemical Assessment
- •Treatment Modalities
- •Oral Preparations
- •Parenteral Preparations
- •Transdermal Preparations
- •Side Effects and Treatment Monitoring
- •Body Composition
- •Cognitive Decline
- •Bone Metabolism
- •The Kidneys
- •Endocrine Functions of the Kidney
- •Erythropoietin
- •Calcitriol
- •Renin
- •Paraneoplastic Syndromes
- •Hypercalcemia
- •Hypertension
- •Polycythemia
- •Other Endocrine Abnormalities
- •References
- •General Physiology
- •Prostate Innervation
- •Summary
- •References
- •Wound Healing
- •Inflammation
- •Proliferation
- •Remodeling
- •Principles of Plastic Surgery
- •Tissue Characteristics
- •Grafts
- •Flap
- •References
- •Lower Urinary Tract Symptoms
- •Storage Phase
- •Voiding Phase
- •Return to Storage Phase
- •Urodynamic Parameters
- •Urodynamic Techniques
- •Volume Voided Charts
- •Pad Testing
- •Typical Test Schedule
- •Uroflowmetry
- •Post Voiding Residual
- •Further Diagnostic Evaluation of Patients
- •Cystometry with or Without Video
- •Cystometry
- •Videocystometrography (Cystometry + Cystourethrography)
- •Cystometric Findings
- •Comment:
- •Measurements During the Storage Phase:
- •Measurements During the Voiding Phase:
- •Abnormal Function
- •Disorders of Sensation
- •Causes of Hypersensitive Bladder Sensation
- •Causes of Hyposensitive Bladder Sensation
- •Disorders of Detrusor Motor Function
- •Bladder Outflow Tract Dysfunction
- •Detrusor–Urethral Dyssynergia
- •Detrusor–Bladder Neck Dyssynergia
- •Detrusor–Sphincter Dyssynergia
- •Complex Urodynamic Investigation
- •Urethral Pressure Measurement
- •Technique
- •Neurophysiological Evaluation
- •Conclusion
- •References
- •Endoscopy
- •Cystourethroscopy
- •Ureteroscopy and Ureteropyeloscopy
- •Nephroscopy
- •Virtual Reality Simulators
- •Lasers
- •Clinical Application of Lasers
- •Condylomata Acuminata
- •Urolithiasis
- •Benign Prostatic Hyperplasia
- •Ureteral and Urethral Strictures
- •Conclusion
- •References
- •Introduction
- •The Prostatitis Syndromes
- •The Scope of the Problem
- •Category III CP/CPPS
- •The Goal of Treatment
- •Conservative Management
- •Drug Therapy
- •Antibiotics
- •Anti-inflammatories
- •Alpha blockers
- •Hormone Therapies
- •Phytotherapies
- •Analgesics, muscle relaxants and neuromodulators
- •Surgery
- •A Practical Management Plan
- •References
- •Orchitis
- •Definition and Etiology
- •Clinical Signs and Symptoms
- •Diagnostic Evaluation
- •Treatment of Infectious Orchitis
- •Epididymitis
- •Definition and Etiology
- •Clinical Signs and Symptoms
- •Diagnostic Evaluation of Epididymitis
- •Treatment of Acute Epididymitis
- •Treatment of Chronic Epididymitis
- •Treatment of Spermatic Cord Torsion
- •Fournier’s Gangrene
- •Definition and Etiology
- •Risk Factors
- •Clinical Signs and Symptoms
- •Diagnostic Evaluation
- •Treatment
- •References
- •Fungal Infections
- •Candidiasis
- •Aspergillosis
- •Cryptococcosis
- •Blastomycosis
- •Coccidioidomycosis
- •Histoplasmosis
- •Radiographic Findings
- •Treatment
- •Tuberculosis
- •Clinical Manifestations
- •Diagnosis
- •Treatment
- •Schistosomiasis
- •Clinical Manifestations
- •Diagnosis
- •Treatment
- •Filariasis
- •Clinical Manifestations
- •Diagnosis
- •Treatment
- •Onchocerciasis
- •References
- •25: Sexually Transmitted Infections
- •Introduction
- •STIs Associated with Genital Ulcers
- •Herpes Simplex Virus
- •Diagnosis
- •Treatment
- •Chancroid
- •Diagnosis
- •Treatment
- •Syphilis
- •Diagnosis
- •Treatment
- •Lymphogranuloma Venereum
- •Diagnosis
- •Treatment
- •Chlamydia
- •Diagnosis
- •Treatment
- •Gonorrhea
- •Diagnosis
- •Treatment
- •Trichomoniasis
- •Diagnosis
- •Treatment
- •Human Papilloma Virus
- •Diagnosis
- •Treatment
- •Scabies
- •Diagnosis
- •Treatment
- •References
- •26: Hematuria: Evaluation and Management
- •Introduction
- •Classification of Hematuria
- •Macroscopic Hematuria
- •Microscopic Hematuria
- •Dipstick Hematuria
- •Pseudohematuria
- •Factitious Hematuria
- •Menstruation
- •Aetiology
- •Malignancy
- •Urinary Calculi
- •Infection and Inflammation
- •Benign Prostatic Hyperplasia
- •Trauma
- •Drugs
- •Nephrological Causes
- •Assessment
- •History
- •Examination
- •Investigations
- •Dipstick Urinalysis
- •Cytology
- •Molecular Tests
- •Blood Tests
- •Flexible Cystoscopy
- •Upper Urinary Tract Evaluation
- •Renal USS
- •KUB Abdominal X-Ray
- •Intravenous Urography (IVU)
- •Computed Tomography (CT)
- •Retrograde Urogram Studies
- •Magnetic Resonance Imaging (MRI)
- •Additional Tests and Renal Biopsy
- •Intractable Hematuria
- •Loin Pain Hematuria Syndrome
- •References
- •27: Benign Prostatic Hyperplasia (BPH)
- •Historical Background
- •Pathophysiology
- •Patient Assessment
- •Treatment of BPH
- •Watchful Waiting
- •Drug Therapy
- •Interventional Therapies
- •Conclusions
- •References
- •28: Practical Guidelines for the Treatment of Erectile Dysfunction and Peyronie´s Disease
- •Erectile Dysfunction
- •Introduction
- •Diagnosis
- •Basic Evaluation
- •Cardiovascular System and Sexual Activity
- •Optional Tests
- •Treatment
- •Medical Treatment
- •Oral Agents
- •Phosphodiesterase Type 5 (PDE 5) Inhibitors
- •Nonresponders to PDE5 Inhibitors
- •Apomorphine SL
- •Yohimbine
- •Intracavernosal and Intraurethral Therapy
- •Intracavernosal Injection (ICI) Therapy
- •Intraurethral Therapy
- •Vacuum Constriction Devices
- •Surgical Therapy
- •Conclusion
- •Peyronie´s Disease (PD)
- •Introduction
- •Oral Drug Therapy
- •Intralesional Drug Therapy
- •Iontophoresis
- •Radiation Therapy
- •Surgical Therapy
- •References
- •29: Premature Ejaculation
- •Introduction
- •Epidemiology
- •Defining Premature Ejaculation
- •Voluntary Control
- •Sexual Satisfaction
- •Distress
- •Psychosexual Counseling
- •Pharmacological Treatment
- •On-Demand Treatment with Tramadol
- •Topical Anesthetics
- •Phosphodiesterase Inhibitors
- •Surgery
- •Conclusion
- •References
- •30: The Role of Interventional Management for Urinary Tract Calculi
- •Contraindications to ESWL
- •Complications of ESWL
- •PCNL Access
- •Instrumentation for PCNL
- •Nephrostomy Drains Post PCNL
- •Contraindications to PCNL
- •Complications of PCNL
- •Semirigid Ureteroscopy
- •Flexible Ureteroscopy
- •Electrohydraulic Lithotripsy (EHL)
- •Ultrasound
- •Ballistic Lithotripsy
- •Laser Lithotripsy
- •Ureteric Stents
- •Staghorn Calculi
- •Lower Pole Stones
- •Horseshoe Kidneys and Stones
- •Calyceal Diverticula Stones
- •Stones and PUJ Obstruction
- •Treatment of Ureteric Colic
- •Medical Expulsive Therapy (MET)
- •Intervention for Ureteric Stones
- •Stones in Pregnancy
- •Morbid Obesity
- •References
- •Anatomy and Function
- •Pathophysiology
- •Management
- •Optical Urethrotomy/Dilatation
- •Urethral Stents
- •Preoperative Assessment
- •Urethroplasty
- •Anastomotic Urethroplasty
- •Substitution Urethroplasty
- •Grafts Versus Flaps
- •Oral Mucosal Grafts
- •Tissue Engineering
- •Graft Position
- •Conclusion
- •References
- •32: Urinary Incontinence
- •Epidemiology and Risk Factors
- •Pathophysiology
- •Urge Incontinence
- •Conservative Treatments
- •Pharmacotherapy
- •Invasive/ Surgical Therapies
- •Stress Urinary Incontinence
- •Male SUI Therapies
- •Female SUI Therapies
- •Mixed Urinary Incontinence
- •Conclusions
- •References
- •33: Neurogenic Bladder
- •Introduction
- •Examination and Diagnostic Tests
- •History and Physical Examination
- •Imaging
- •Urodynamics (UDS)
- •Evoked Potentials
- •Classifications
- •Somatic Pathways
- •Brain Lesions
- •Cerebrovascular Accident (CVA)
- •Parkinson’s Disease (PD)
- •Multiple Sclerosis
- •Huntington’s Disease
- •Dementias
- •Normal Pressure Hydrocephalus (NPH)
- •Tumors
- •Psychiatric Disorders
- •Spinal Lesions and Pathology
- •Intervertebral Disk Prolapse
- •Spinal Cord Injury (SCI)
- •Transverse Myelitis
- •Peripheral Neuropathies
- •Metabolic Neuropathies
- •Pelvic Surgery
- •Treatment
- •Summary
- •References
- •34: Pelvic Prolapse
- •Introduction
- •Epidemiology
- •Anatomy and Pathophysiology
- •Evaluation and Diagnosis
- •Outcome Measures
- •Imaging
- •Urodynamics
- •Indications for Management
- •Biosynthetics
- •Surgical Management
- •Anterior Compartment Repair
- •Uterine/Apical Prolapse
- •Enterocele Repair
- •Conclusion
- •References
- •35: Urinary Tract Fistula
- •Introduction
- •Urogynecologic Fistula
- •Vesicovaginal Fistula
- •Etiology and Risk Factors
- •Clinical Factors
- •Evaluation and Diagnosis
- •Pelvic Examination
- •Cystoscopy
- •Imaging
- •Treatment
- •Conservative Management
- •Surgical Management
- •Urethrovaginal Fistula
- •Etiology and Presentation
- •Diagnosis and Management
- •Ureterovaginal Fistula
- •Etiology and Presentation
- •Diagnosis and Management
- •Vesicouterine Fistula
- •Etiology and Presentation
- •Diagnosis and Management
- •Uro-Enteric Fistula
- •Vesicoenteric Fistula
- •Pyeloenteric Fistula
- •Urethrorectal Fistula
- •References
- •36: Urologic Trauma
- •Introduction
- •Kidney
- •Expectant Management
- •Endovascular Therapy
- •Operative Intervention
- •Operative Management: Follow-up
- •Reno-Vascular Injuries
- •Pediatric Renal Injuries
- •Adrenal
- •Ureter
- •Diagnosis
- •Treatment
- •Delayed Diagnosis
- •Bladder and Posterior Urethra
- •Bladder Injuries: Initial Management
- •Bladder Injuries: Formal Repair
- •Anterior Urethral Trauma
- •Fractured Penis
- •Penile Amputation
- •Scrotal and Testicular Trauma
- •Imaging
- •CT-IVP (CT with Delayed Images)
- •Technique
- •Cystogram
- •Technique
- •Retrograde Urethrogram (RUG)
- •Technique
- •Retrograde Pyelogram (RPG)
- •Technique
- •One-Shot IVP
- •Technique
- •References
- •37: Bladder Cancer
- •Who Should Be Investigated?
- •Epidemiology
- •Risk Factors
- •Role of Screening
- •Signs and Symptoms
- •Imaging
- •Cystoscopy
- •Urine Tests
- •PDD-Assisted TUR
- •Pathology
- •NMIBC and Risk Groups
- •Intravesical Chemotherapy
- •Intravesical Immunotherapy
- •Immediate Cystectomy and CIS
- •Radical Cystectomy with Pelvic Lymph Node Dissection
- •sexual function-preserving techniques
- •Bladder-Preservation Treatments
- •Neoadjuvant Chemotherapy
- •Adjuvant Chemotherapy
- •Preoperative Radiotherapy
- •Follow-up After TUR in NMIBC
- •References
- •38: Prostate Cancer
- •Introduction
- •Epidemiology
- •Race
- •Geographic Variation
- •Risk Factors and Prevention
- •Family History
- •Diet and Lifestyle
- •Prevention
- •Screening and Diagnosis
- •Current Screening Recommendations
- •Biopsy
- •Pathology
- •Prognosis
- •Treatment of Prostate Cancer
- •Treatment for Localized Prostate Cancer (T1, T2)
- •Radical Prostatectomy
- •EBRT
- •IMRT
- •Brachytherapy
- •Treatment for Locally Advanced Prostate Cancer (T3, T4)
- •EBRT with ADT
- •Radical Prostatectomy
- •Androgen-Deprivation Therapy
- •Summary
- •References
- •39: The Management of Testis Cancer
- •Presentation and Diagnosis
- •Serum Tumor Markers
- •Primary Surgery
- •Testis Preserving Surgery
- •Risk Stratification
- •Surveillance Versus Primary RPLND
- •Primary RPLND
- •Adjuvant Treatment for High Risk
- •Clinical Stage 1 Seminoma
- •Risk-Stratified Adjuvant Treatment
- •Adjuvant Radiotherapy
- •Adjuvant Low Dose Chemotherapy
- •Primary Combination Chemotherapy
- •Late Toxicity
- •Salvage Strategies
- •Conclusion
- •References
- •Index

485
Urinary tract FistUla
urography, or MR urography. Retrograde pyelo- |
successful in small fistulas only,less than 2–3 mm |
|||
grams may be utilized if the distal ureter is not |
in diameter. |
|
||
well visualized, and a concomitant ureterovagi- |
|
|
||
nal fistula is suspected but has not been demon- |
Surgical Management |
Once the decision has been |
||
strated on alterative upper urinary-tract |
||||
imaging.1,11 Delayed visualization of contrast |
made by the patient and physician to pursue |
|||
within the vagina on CT urogram or direct con- |
definitive surgical repair, it is essential to |
|||
trast extravasation into the fistula tract on CT |
carefully plan an operative approach that will |
|||
cystogram provide alternate means of evalua- |
maximize the chance of success.The first attempt |
|||
tion, with the added ability to detect additional |
at VVF repair is usually the best opportunity for |
|||
intra-abdominal pathology.23 |
fistula closure, due to later scarring and |
|||
|
|
anatomical distortion. There is no “best” |
||
|
|
approach for VVF repair as long as the basic |
||
Treatment |
|
principles are followed. |
||
The goal of treatment of VVF should be the |
Classic teaching suggests a minimal waiting |
|||
period of several months after diagnosis for |
||||
timely and complete cessation of urinary leak- |
||||
definitive repair; however, delayed management |
||||
age with minimal effect on normal urinary and |
||||
has fallen out of favor over the past few decades. |
||||
genital function. |
|
|||
|
Immediate management, especially in cases of |
|||
|
|
|||
|
|
uncomplicated iatrogenic fistula, can minimize |
||
Conservative Management |
Conservative management |
patient discomfort and anguish without com- |
||
of small VVF can be attempted prior to surgical |
promising the surgical repair.11,27-33 However, in |
|||
intervention. Although there is some morbidity |
cases of continued infection, obstetric fistula, |
|||
and discomfort associated with indwelling |
or radiation-induced fistula, demarcation of |
|||
catheterization, a trial of continuous bladder |
inflamed or devascularized tissues may require |
|||
drainage and anticholinergic medication for |
a waiting period of 1–6 months and 6–12 months, |
|||
2–3 weeks can be associated with spontaneous |
respectively.18,34,35 Medical factors and wound |
|||
healing in properly selected patients.24 Small |
care also should be addressed and optimized |
|||
epithelializedfistulasmaybenefitfromminimally |
prior to intervention in these and all other fis- |
|||
invasive cystoscopic electrocoagulation of the |
tula cases. |
|
||
fistula tract, followed by bladder catheterization. |
Vesicovaginal |
fistula can be repaired via |
||
In patients with |
fistula diameter less than |
a transvaginal or transabdominal approach. |
||
3.5 mm,11/15 had successful fistula tract ablation |
Each approach has benefits and drawbacks, |
|||
with cauterization and catheter drainage in a |
but each results in traditionally high rates of |
|||
study by Stovsky et al.25 Fibrin sealant has also |
successful fistula closure, usually greater than |
|||
been utilized with some success to plug the |
90% (Table 35.3).7,36-38 Consideration of fac- |
|||
fistula tract, presumably until tissue ingrowth |
tors such as size, location, and need for adjunc- |
|||
occurs.26 In general, conservative measures are |
tive procedures can affect the approach, but |
|||
Table 35.3. surgical management of vesicovaginal fistula. comparison of transabdominal and transvaginal approaches to repair
Approach |
Transabdominal |
Transvaginal |
timing |
delayed (3–6 month) |
immediate/delayed |
Ureteral involvement |
reimplant possible if indicated |
no reimplant possible |
sexual function |
no change in vaginal depth |
risk of vaginal shortening |
Flaps |
omental, peritoneal |
labial, peritoneal, gluteal, gracilis |
indications |
large fistula, high fistula in narrow vault, radiation, failed |
low fistulas, failed taFr |
|
vaginal approach, other procedures (augment) |
|
Morbidity |
High |
low |

|
|
486 |
|
|
|
|
|
Practical Urology: EssEntial PrinciPlEs and PracticE |
the most important factor should be surgeon |
throughout the case. Ureteral stents are placed |
|
experience and comfort. Surgical mobilization |
if the fistula is in close proximity to the ureteral |
|
of well-vascularized flaps, followed by a sepa- |
orifices. A urethral catheter is placed, and a |
|
rate water-tight closure of the urinary and |
supra-pubic catheter may also be utilized for |
|
genital tracts with nonoverlapping suture lines |
bladder drainage. An inverted U-shaped inci- |
|
is the intraoperative goal regardless of the |
sion is made which circumscribes the fistula |
|
approach. |
site. Anterior and posterior vaginal wall flaps |
|
Transabdominal approaches for fistula repair |
are developed after hydro-dissection with ster- |
|
include supravesical or transvesical approaches, |
ile saline, and retracted using the ring retractor. |
|
and laparoscopic/robotic techniques. The |
Using double-armed SAS, the fistula is closed in |
|
O’Conor transabdominal VVF repair has been |
an interrupted fashion. The perivesical tissue is |
|
well described.39 The patient is positioned in a |
then closed over the initial suture line in an |
|
low lithotomy position, with access to the vagina |
interrupted imbricated fashion, 90° in respect |
|
and abdomen. Ureteral catheters may be placed |
to the first layer. A peritoneal flap or a martius |
|
and are recommended if the fistula is near the |
flap can be positioned over the imbricated layer |
|
ureteral orifices or the trigone. A lower midline |
of peri-vesical tissue. The posterior vaginal wall |
|
incision is performed and the bladder is mobi- |
flap is advanced over the suture line anteriorly |
|
lized. The bladder is then bivalved vertically to |
to complete the closure. |
|
the level of the fistula, and dissection is contin- |
Adjacent tissue flaps can be useful in the |
|
ued distally to open the vesicovaginal space, |
setting of complex fistula with compromised |
|
2–3 cm distal to the fistula site. Following mobi- |
surrounding tissue, or in patients with prior |
|
lization of the vaginal wall from the bladder wall |
failed repairs, radiotherapy, obstetric fistula, or |
|
distal to the fistula tract, the fistula tract is |
large fistula tracts. For patients undergoing a |
|
excised, and the vaginal wall is closed with run- |
transvaginal approach, a labial fat pad (Martius) |
|
ning synthetic absorbable suture (SAS). The |
or peritoneal flaps are most frequently utilized |
|
bladder is closed in multiple layers with running |
with success rates of greater than 90%.7 The |
|
SAS. An additional layer of tissue can be placed |
Martius graft is harvested from the fibrofatty |
|
between the suture lines utilizing an omental |
tissue of the labia majora. It maintains blood |
|
interposition flap or peritoneal flap. It is impor- |
supply from the external pudendal artery supe- |
|
tant to secure the interpositional flap distally |
riorly and the inferior labial artery inferiorly, |
|
beyond the fistula. |
allowing rotation and mobilization from either |
|
In the transvesical approach, the bladder is |
pedicle. Once mobilized via a labial incision, this |
|
opened via a midline cystotomy on the anterior |
flap can be tunneled into the vaginal dissection |
|
surface of the bladder. The VVF tract is then cir- |
for additional layers of fistula closure. In high |
|
cumscribed and excised.Following mobilization |
VVF repairs from a transvaginal approach, the |
|
of the vesicovaginal space surrounding the fis- |
peritoneum is often encountered during the |
|
tula site, the vaginal and vesical tissues are |
course of dissection. The peritoneum can be |
|
closed separately. A flap of adjacent bladder tis- |
advanced over the fistula repair as an additional |
|
sue may be advanced to avoid overlapping suture |
layer of closure, with success rates of 91–96%.7,41 |
|
lines as described by Gil-Vernet.40 |
As noted previously, omental interposition flaps |
|
The transvaginal approach for fistula repair |
are useful adjunctive procedures when perform- |
|
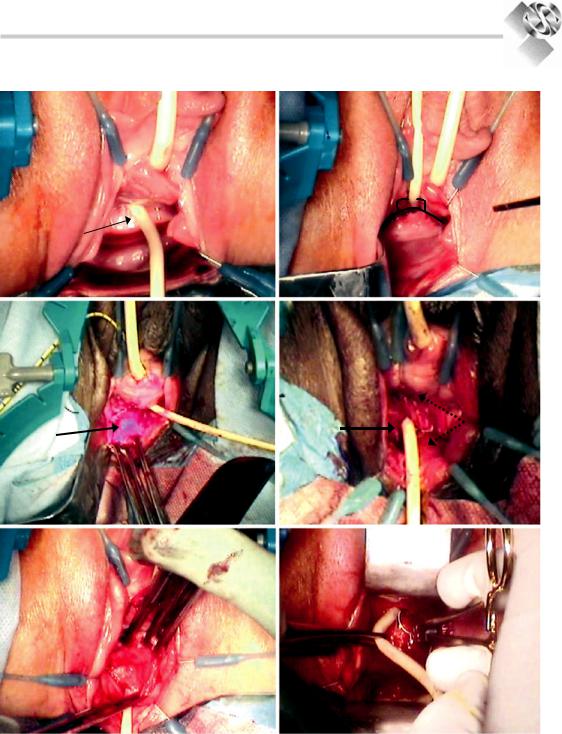
is shown in Fig. 35.3.7,41,42 The patient is placed |
ing transabdominal VVF repairs in the manner |
|
in the dorsal lithotomy position, and a rectal |
of O’Conor. Interposition flaps or peritoneal |
|
pack is placed. Labial retraction sutures are |
flaps can be incorporated into transabdominal |
|
placed as well as a weighted speculum. A self- |
fistula repairs between bladder and vaginal wall |
|
retaining ring retractor with hooks is very use- |
suture lines. The omental vascular supply is |
|
ful for visualization and retraction. Cystoscopy |
based on the right and left gastroepiploic arter- |
|
is performed to localize the fistula tract, and a |
ies. In order to provide sufficient length for the |
|
guide wire is placed though the fistula into the |
flap to reach the pelvis, the omentum can be |
|
vagina. A 10–12 French foley catheter should be |
mobilized along the greater curvature of the |
|
placed though the fistula site, using the previ- |
stomach, sacrificing the left gastroepiploic |
|
ously placed guide wire. This catheter provides |
artery and allowing larger right gastroepiploic |
|
traction of the fistula toward the introitus |
artery to maintain blood supply. |
|
487
Urinary tract FistUla
a |
b |
c |
d |
e |
f |
Figure 35.3. (a–j) transvaginal repair of vesicovaginal fistula.(a) Foley catheter within the urethra and vesicovaginal fistula (arrow). (b) anterior curvo-linear vaginal wall incision (black line) incorporating the fistula site. (c) dissected posterior vaginal wall flap (arrow) retracted inferiorly. (d) Perivesical tissue (solid arrow) and retracted superior and inferior vaginal wall flaps (dashed arrow). (e) dissection of perivesical tissue from the underlying detrusor muscle to provide an additional layer of closure. (f) initial suture
placement, closing the detrusor and bladder mucosa. (g) sutures retracted to visualize the initial layer of closure.the foley catheter is then removed from the fistula, and the sutures are tied. (h) second line of closure with imbricated interrupted sutures to reinforce the initial layer of closure. (i) third tissue layer of interrupted sutures, bringing together the previously dissected perivesical fascial layers. Arrows identify the perivesical tissue flaps. (j) closure of the vaginal wall (reprinted from chapple).
