
- •Preface and Acknowledgments
- •Contents
- •Contributors
- •1: Embryology for Urologists
- •Introduction
- •Renal Development
- •Pronephros
- •Mesonephros
- •Metanephros
- •Development of the Collecting System
- •Critical Steps in Further Development
- •Anomalies of the Kidney
- •Renal Agenesis
- •Renal Aplasia
- •Renal Hypoplasia
- •Renal Ectopia
- •Renal Fusion
- •Ureteral Development
- •Anomalies of Origin
- •Anomalies of Number
- •Incomplete Ureteral Duplication
- •Complete Ureteral Duplication
- •Ureteral Ectopia
- •Embryology of Ectopia
- •Clinical Correlation
- •Location of Ectopic Ureteral Orifices – Male (in Descending Order According to Incidence)
- •Symptoms
- •Ureteroceles
- •Congenital Ureteral Obstruction
- •Pipestem Ureter
- •Megaureter-Megacystis Syndrome
- •Prune Belly Syndrome
- •Vascular Ureteral Obstructions
- •Division of the Urogenital Sinus
- •Bladder Development
- •Urachal Anomalies
- •Cloacal Duct Anomalies
- •Other Bladder Anomalies
- •Bladder Diverticula
- •Bladder Extrophy
- •Gonadal Development
- •Testicular Differentiation
- •Ovarian Differentiation
- •Gonadal Anomalies
- •Genital Duct System
- •Disorders of Testicular Function
- •Female Ductal Development
- •Prostatic Urethral Valves
- •Gonadal Duct Anomalies
- •External Genital Development
- •Male External Genital Development
- •Female External Genital Development
- •Anomalies of the External Genitalia
- •References
- •2: Gross and Laparoscopic Anatomy of the Upper Urinary Tract and Retroperitoneum
- •Overview
- •The Kidneys
- •The Renal Vasculature
- •The Renal Collecting System
- •The Ureters
- •Retroperitoneal Lymphatics
- •Retroperitoneal Nerves
- •The Adrenal Glands
- •References
- •3: Gross and Laparoscopic Anatomy of the Lower Urinary Tract and Pelvis
- •Introduction
- •Female Pelvis
- •Male Pelvis
- •Pelvic Floor
- •Urinary Bladder
- •Urethra
- •Male Urethra
- •Female Urethra
- •Sphincter Mechanisms
- •The Bladder Neck Component
- •The Urethral Wall Component
- •The External Urethral Sphincter
- •Summary
- •References
- •4: Anatomy of the Male Reproductive System
- •Testis and Scrotum
- •Spermatogenesis
- •Hormonal Regulation of Spermatogenesis
- •Genetic Regulation of Spermatogenesis
- •Epididymis and Ductus Deferens
- •Accessory Sex Glands
- •Prostate
- •Seminal Vesicles
- •Bulbourethral Glands
- •Penis
- •Erection and Ejaculation
- •References
- •5: Imaging of the Upper Tracts
- •Anatomy of the Upper Tracts and Introduction to Imaging Modalities
- •Introduction
- •Renal Upper Tract Basic Anatomy
- •Modalities Used for Imaging the Upper Tracts
- •Ultrasound
- •Radiation Issues
- •Contrast Issues
- •Renal and Upper Tract Tumors
- •Benign Renal Tumors
- •Transitional Cell Carcinoma
- •Renal Mass Biopsy
- •Renal Stone Disease
- •Ultrasound
- •Plain Radiographs and IVU
- •Renal Cystic Disease
- •Benign Renal Cysts
- •Hereditary Renal Cystic Disease
- •Complex Renal Cysts
- •Renal Trauma
- •References
- •Introduction
- •Pathophysiology
- •Susceptibility and Resistance
- •Epidemiological Breakpoints
- •Clinical Breakpoints
- •Pharmacodynamic Parameters
- •Pharmacokinetic Parameters
- •Fosfomycin
- •Nitrofurantoin
- •Pivmecillinam
- •b-Lactam-Antibiotics
- •Penicillins
- •Cephalosporins
- •Carbapenems
- •Aminoglycosides
- •Fluoroquinolones
- •Trimethoprim, Cotrimoxazole
- •Glycopeptides
- •Linezolid
- •Conclusion
- •References
- •7: An Overview of Renal Physiology
- •Introduction
- •Body Fluid Compartments
- •Regulation of Potassium Balance
- •Regulation of Acid–Base Balance
- •Diuretics
- •Suggested Reading
- •8: Ureteral Physiology and Pharmacology
- •Ureteral Anatomy
- •Modulation of Peristalsis
- •Ureteral Pharmacology
- •Conclusion
- •References
- •Introduction
- •Afferent Signaling Pathways
- •Efferent Signaling
- •Parasympathetic Nerves
- •Sympathetic Nerves
- •Vesico-Spinal-Vesical Micturition Reflex
- •Peripheral Targets
- •Afferent Signaling Mechanisms
- •Urothelium
- •Myocytes
- •Cholinergic Receptors
- •Muscarinic Receptors
- •Nicotinic Receptors
- •Adrenergic Receptors (ARs)
- •a-Adrenoceptors
- •b-Adrenoceptors
- •Transient Receptor Potential (TRP) Receptors
- •Phosphodiesterases (PDEs)
- •CNS Targets
- •Opioid Receptors
- •Serotonin (5-HT) Mechanisms
- •g-Amino Butyric Acid (GABA) Mechanisms
- •Gabapentin
- •Neurokinin and Neurokinin Receptors
- •Summary
- •References
- •10: Pharmacology of Sexual Function
- •Introduction
- •Sexual Desire/Arousal
- •Endocrinology
- •Steroids in the Male
- •Steroids in the Female
- •Neurohormones
- •Neurotransmitters
- •Dopamine
- •Serotonin
- •Pharmacological Strategies
- •CNS Drugs
- •Enzyme-inducing Antiepileptic Drugs
- •Erectile Function
- •Ejaculatory Function
- •Premature Ejaculation
- •Abnormal Ejaculation
- •Conclusions
- •References
- •Epidemiology
- •Calcium-Based Urolithiasis
- •Uric Acid Urolithiasis
- •Infectious Urolithiasis
- •Cystine-Based Urolithiasis
- •Aims
- •Who Deserves Metabolic Evaluation?
- •Metabolic Workup for Stone Producers
- •Medical History and Physical Examination
- •Stone Analysis
- •Serum Chemistry
- •Urine Evaluation
- •Urine Cultures
- •Urinalysis
- •Twenty-Four Hour Urine Collections
- •Radiologic Imaging
- •Medical Management
- •Conservative Management
- •Increased Fluid Intake
- •Citrus Juices
- •Dietary Restrictions
- •Restricted Oxalate Diet
- •Conservative Measures
- •Selective Medical Therapy
- •Absorptive Hypercalciuria
- •Thiazide
- •Orthophosphate
- •Renal Hypercalciuria
- •Primary Hyperparathyroidism
- •Hyperuricosuric Calcium Oxalate Nephrolithiasis
- •Enteric Hyperoxaluria
- •Hypocitraturic Calcium Oxalate Nephrolithiasis
- •Distal Renal Tubular Acidosis
- •Chronic Diarrheal States
- •Thiazide-Induced Hypocitraturia
- •Idiopathic Hypocitraturic Calcium Oxalate Nephrolithiasis
- •Hypomagnesiuric Calcium Nephrolithiasis
- •Gouty Diathesis
- •Cystinuria
- •Infection Lithiasis
- •Summary
- •References
- •12: Molecular Biology for Urologists
- •Introduction
- •Inherited Changes in Cancer Cells
- •VEGR and Cell Signaling
- •Targeting mTOR
- •Conclusion
- •References
- •13: Chemotherapeutic Agents for Urologic Oncology
- •Introduction
- •Bladder Cancer
- •Muscle Invasive Bladder Cancer
- •Metastatic Bladder Cancer
- •Conclusion
- •Prostate Cancer
- •Other Chemotherapeutic Drugs or Combinations for Treating HRPC
- •Conclusion
- •Renal Cell Carcinoma
- •Chemotherapy
- •Immunotherapy
- •Angiogenesis Inhibitor Drugs
- •Conclusion
- •Testicular Cancer
- •Stage I Seminoma
- •Stage I non-seminomatous Germ Cell Tumours (NSGCT)
- •Metastatic Germ Cell Tumours
- •Low-Volume Metastatic Disease (Stage II A/B)
- •Advanced Metastatic Disease
- •Salvage Chemotherapy for Relapsed or Refractory Disease
- •Conclusion
- •Penile Cancer
- •Side Effects of Chemotherapy
- •Conclusion
- •References
- •14: Tumor and Transplant Immunology
- •Antibodies
- •Cytotoxic and T-helper Cells
- •Immunosuppression
- •Induction Therapy
- •Maintenance Therapy
- •Rejection
- •Posttransplant Lymphoproliferative Disease
- •Summary
- •References
- •15: Pathophysiology of Renal Obstruction
- •Causes of Renal Obstruction
- •Effects on Prenatal Development
- •Prenatal Hydronephrosis
- •Spectrum of Renal Abnormalities
- •Renal Functional Changes
- •Renal Growth/Counterbalance
- •Vascular Changes
- •Inflammatory Mediators
- •Glomerular Development Changes
- •Mechanical Stretch of Renal Tubules
- •Unilateral Versus Bilateral
- •Limitations of Animal Models
- •Future Research
- •Issues in Patient Management
- •Diagnostic Imaging
- •Ultrasound
- •Intravenous Urography
- •Antegrade Urography and the Whitaker Test
- •Nuclear Renography
- •Computed Tomography
- •Magnetic Resonance Urography
- •Hypertension
- •Postobstructive Diuresis
- •References
- •Introduction
- •The Normal Lower Urinary Tract
- •Anatomy
- •Storage Function
- •Voiding Function
- •Neural Control
- •Symptoms
- •Flow Rate and Post-void Residual
- •Voiding Cystometry
- •Male
- •Female
- •Neurourology
- •Conclusions
- •References
- •17: Urologic Endocrinology
- •The Testis
- •Normal Androgen Metabolism
- •Epidemiological Aspects
- •Prostate
- •Brain
- •Muscle Mass and Adipose Tissue
- •Bones
- •Ematopoiesis
- •Metabolism
- •Cardiovascular System
- •Clinical Assessment
- •Biochemical Assessment
- •Treatment Modalities
- •Oral Preparations
- •Parenteral Preparations
- •Transdermal Preparations
- •Side Effects and Treatment Monitoring
- •Body Composition
- •Cognitive Decline
- •Bone Metabolism
- •The Kidneys
- •Endocrine Functions of the Kidney
- •Erythropoietin
- •Calcitriol
- •Renin
- •Paraneoplastic Syndromes
- •Hypercalcemia
- •Hypertension
- •Polycythemia
- •Other Endocrine Abnormalities
- •References
- •General Physiology
- •Prostate Innervation
- •Summary
- •References
- •Wound Healing
- •Inflammation
- •Proliferation
- •Remodeling
- •Principles of Plastic Surgery
- •Tissue Characteristics
- •Grafts
- •Flap
- •References
- •Lower Urinary Tract Symptoms
- •Storage Phase
- •Voiding Phase
- •Return to Storage Phase
- •Urodynamic Parameters
- •Urodynamic Techniques
- •Volume Voided Charts
- •Pad Testing
- •Typical Test Schedule
- •Uroflowmetry
- •Post Voiding Residual
- •Further Diagnostic Evaluation of Patients
- •Cystometry with or Without Video
- •Cystometry
- •Videocystometrography (Cystometry + Cystourethrography)
- •Cystometric Findings
- •Comment:
- •Measurements During the Storage Phase:
- •Measurements During the Voiding Phase:
- •Abnormal Function
- •Disorders of Sensation
- •Causes of Hypersensitive Bladder Sensation
- •Causes of Hyposensitive Bladder Sensation
- •Disorders of Detrusor Motor Function
- •Bladder Outflow Tract Dysfunction
- •Detrusor–Urethral Dyssynergia
- •Detrusor–Bladder Neck Dyssynergia
- •Detrusor–Sphincter Dyssynergia
- •Complex Urodynamic Investigation
- •Urethral Pressure Measurement
- •Technique
- •Neurophysiological Evaluation
- •Conclusion
- •References
- •Endoscopy
- •Cystourethroscopy
- •Ureteroscopy and Ureteropyeloscopy
- •Nephroscopy
- •Virtual Reality Simulators
- •Lasers
- •Clinical Application of Lasers
- •Condylomata Acuminata
- •Urolithiasis
- •Benign Prostatic Hyperplasia
- •Ureteral and Urethral Strictures
- •Conclusion
- •References
- •Introduction
- •The Prostatitis Syndromes
- •The Scope of the Problem
- •Category III CP/CPPS
- •The Goal of Treatment
- •Conservative Management
- •Drug Therapy
- •Antibiotics
- •Anti-inflammatories
- •Alpha blockers
- •Hormone Therapies
- •Phytotherapies
- •Analgesics, muscle relaxants and neuromodulators
- •Surgery
- •A Practical Management Plan
- •References
- •Orchitis
- •Definition and Etiology
- •Clinical Signs and Symptoms
- •Diagnostic Evaluation
- •Treatment of Infectious Orchitis
- •Epididymitis
- •Definition and Etiology
- •Clinical Signs and Symptoms
- •Diagnostic Evaluation of Epididymitis
- •Treatment of Acute Epididymitis
- •Treatment of Chronic Epididymitis
- •Treatment of Spermatic Cord Torsion
- •Fournier’s Gangrene
- •Definition and Etiology
- •Risk Factors
- •Clinical Signs and Symptoms
- •Diagnostic Evaluation
- •Treatment
- •References
- •Fungal Infections
- •Candidiasis
- •Aspergillosis
- •Cryptococcosis
- •Blastomycosis
- •Coccidioidomycosis
- •Histoplasmosis
- •Radiographic Findings
- •Treatment
- •Tuberculosis
- •Clinical Manifestations
- •Diagnosis
- •Treatment
- •Schistosomiasis
- •Clinical Manifestations
- •Diagnosis
- •Treatment
- •Filariasis
- •Clinical Manifestations
- •Diagnosis
- •Treatment
- •Onchocerciasis
- •References
- •25: Sexually Transmitted Infections
- •Introduction
- •STIs Associated with Genital Ulcers
- •Herpes Simplex Virus
- •Diagnosis
- •Treatment
- •Chancroid
- •Diagnosis
- •Treatment
- •Syphilis
- •Diagnosis
- •Treatment
- •Lymphogranuloma Venereum
- •Diagnosis
- •Treatment
- •Chlamydia
- •Diagnosis
- •Treatment
- •Gonorrhea
- •Diagnosis
- •Treatment
- •Trichomoniasis
- •Diagnosis
- •Treatment
- •Human Papilloma Virus
- •Diagnosis
- •Treatment
- •Scabies
- •Diagnosis
- •Treatment
- •References
- •26: Hematuria: Evaluation and Management
- •Introduction
- •Classification of Hematuria
- •Macroscopic Hematuria
- •Microscopic Hematuria
- •Dipstick Hematuria
- •Pseudohematuria
- •Factitious Hematuria
- •Menstruation
- •Aetiology
- •Malignancy
- •Urinary Calculi
- •Infection and Inflammation
- •Benign Prostatic Hyperplasia
- •Trauma
- •Drugs
- •Nephrological Causes
- •Assessment
- •History
- •Examination
- •Investigations
- •Dipstick Urinalysis
- •Cytology
- •Molecular Tests
- •Blood Tests
- •Flexible Cystoscopy
- •Upper Urinary Tract Evaluation
- •Renal USS
- •KUB Abdominal X-Ray
- •Intravenous Urography (IVU)
- •Computed Tomography (CT)
- •Retrograde Urogram Studies
- •Magnetic Resonance Imaging (MRI)
- •Additional Tests and Renal Biopsy
- •Intractable Hematuria
- •Loin Pain Hematuria Syndrome
- •References
- •27: Benign Prostatic Hyperplasia (BPH)
- •Historical Background
- •Pathophysiology
- •Patient Assessment
- •Treatment of BPH
- •Watchful Waiting
- •Drug Therapy
- •Interventional Therapies
- •Conclusions
- •References
- •28: Practical Guidelines for the Treatment of Erectile Dysfunction and Peyronie´s Disease
- •Erectile Dysfunction
- •Introduction
- •Diagnosis
- •Basic Evaluation
- •Cardiovascular System and Sexual Activity
- •Optional Tests
- •Treatment
- •Medical Treatment
- •Oral Agents
- •Phosphodiesterase Type 5 (PDE 5) Inhibitors
- •Nonresponders to PDE5 Inhibitors
- •Apomorphine SL
- •Yohimbine
- •Intracavernosal and Intraurethral Therapy
- •Intracavernosal Injection (ICI) Therapy
- •Intraurethral Therapy
- •Vacuum Constriction Devices
- •Surgical Therapy
- •Conclusion
- •Peyronie´s Disease (PD)
- •Introduction
- •Oral Drug Therapy
- •Intralesional Drug Therapy
- •Iontophoresis
- •Radiation Therapy
- •Surgical Therapy
- •References
- •29: Premature Ejaculation
- •Introduction
- •Epidemiology
- •Defining Premature Ejaculation
- •Voluntary Control
- •Sexual Satisfaction
- •Distress
- •Psychosexual Counseling
- •Pharmacological Treatment
- •On-Demand Treatment with Tramadol
- •Topical Anesthetics
- •Phosphodiesterase Inhibitors
- •Surgery
- •Conclusion
- •References
- •30: The Role of Interventional Management for Urinary Tract Calculi
- •Contraindications to ESWL
- •Complications of ESWL
- •PCNL Access
- •Instrumentation for PCNL
- •Nephrostomy Drains Post PCNL
- •Contraindications to PCNL
- •Complications of PCNL
- •Semirigid Ureteroscopy
- •Flexible Ureteroscopy
- •Electrohydraulic Lithotripsy (EHL)
- •Ultrasound
- •Ballistic Lithotripsy
- •Laser Lithotripsy
- •Ureteric Stents
- •Staghorn Calculi
- •Lower Pole Stones
- •Horseshoe Kidneys and Stones
- •Calyceal Diverticula Stones
- •Stones and PUJ Obstruction
- •Treatment of Ureteric Colic
- •Medical Expulsive Therapy (MET)
- •Intervention for Ureteric Stones
- •Stones in Pregnancy
- •Morbid Obesity
- •References
- •Anatomy and Function
- •Pathophysiology
- •Management
- •Optical Urethrotomy/Dilatation
- •Urethral Stents
- •Preoperative Assessment
- •Urethroplasty
- •Anastomotic Urethroplasty
- •Substitution Urethroplasty
- •Grafts Versus Flaps
- •Oral Mucosal Grafts
- •Tissue Engineering
- •Graft Position
- •Conclusion
- •References
- •32: Urinary Incontinence
- •Epidemiology and Risk Factors
- •Pathophysiology
- •Urge Incontinence
- •Conservative Treatments
- •Pharmacotherapy
- •Invasive/ Surgical Therapies
- •Stress Urinary Incontinence
- •Male SUI Therapies
- •Female SUI Therapies
- •Mixed Urinary Incontinence
- •Conclusions
- •References
- •33: Neurogenic Bladder
- •Introduction
- •Examination and Diagnostic Tests
- •History and Physical Examination
- •Imaging
- •Urodynamics (UDS)
- •Evoked Potentials
- •Classifications
- •Somatic Pathways
- •Brain Lesions
- •Cerebrovascular Accident (CVA)
- •Parkinson’s Disease (PD)
- •Multiple Sclerosis
- •Huntington’s Disease
- •Dementias
- •Normal Pressure Hydrocephalus (NPH)
- •Tumors
- •Psychiatric Disorders
- •Spinal Lesions and Pathology
- •Intervertebral Disk Prolapse
- •Spinal Cord Injury (SCI)
- •Transverse Myelitis
- •Peripheral Neuropathies
- •Metabolic Neuropathies
- •Pelvic Surgery
- •Treatment
- •Summary
- •References
- •34: Pelvic Prolapse
- •Introduction
- •Epidemiology
- •Anatomy and Pathophysiology
- •Evaluation and Diagnosis
- •Outcome Measures
- •Imaging
- •Urodynamics
- •Indications for Management
- •Biosynthetics
- •Surgical Management
- •Anterior Compartment Repair
- •Uterine/Apical Prolapse
- •Enterocele Repair
- •Conclusion
- •References
- •35: Urinary Tract Fistula
- •Introduction
- •Urogynecologic Fistula
- •Vesicovaginal Fistula
- •Etiology and Risk Factors
- •Clinical Factors
- •Evaluation and Diagnosis
- •Pelvic Examination
- •Cystoscopy
- •Imaging
- •Treatment
- •Conservative Management
- •Surgical Management
- •Urethrovaginal Fistula
- •Etiology and Presentation
- •Diagnosis and Management
- •Ureterovaginal Fistula
- •Etiology and Presentation
- •Diagnosis and Management
- •Vesicouterine Fistula
- •Etiology and Presentation
- •Diagnosis and Management
- •Uro-Enteric Fistula
- •Vesicoenteric Fistula
- •Pyeloenteric Fistula
- •Urethrorectal Fistula
- •References
- •36: Urologic Trauma
- •Introduction
- •Kidney
- •Expectant Management
- •Endovascular Therapy
- •Operative Intervention
- •Operative Management: Follow-up
- •Reno-Vascular Injuries
- •Pediatric Renal Injuries
- •Adrenal
- •Ureter
- •Diagnosis
- •Treatment
- •Delayed Diagnosis
- •Bladder and Posterior Urethra
- •Bladder Injuries: Initial Management
- •Bladder Injuries: Formal Repair
- •Anterior Urethral Trauma
- •Fractured Penis
- •Penile Amputation
- •Scrotal and Testicular Trauma
- •Imaging
- •CT-IVP (CT with Delayed Images)
- •Technique
- •Cystogram
- •Technique
- •Retrograde Urethrogram (RUG)
- •Technique
- •Retrograde Pyelogram (RPG)
- •Technique
- •One-Shot IVP
- •Technique
- •References
- •37: Bladder Cancer
- •Who Should Be Investigated?
- •Epidemiology
- •Risk Factors
- •Role of Screening
- •Signs and Symptoms
- •Imaging
- •Cystoscopy
- •Urine Tests
- •PDD-Assisted TUR
- •Pathology
- •NMIBC and Risk Groups
- •Intravesical Chemotherapy
- •Intravesical Immunotherapy
- •Immediate Cystectomy and CIS
- •Radical Cystectomy with Pelvic Lymph Node Dissection
- •sexual function-preserving techniques
- •Bladder-Preservation Treatments
- •Neoadjuvant Chemotherapy
- •Adjuvant Chemotherapy
- •Preoperative Radiotherapy
- •Follow-up After TUR in NMIBC
- •References
- •38: Prostate Cancer
- •Introduction
- •Epidemiology
- •Race
- •Geographic Variation
- •Risk Factors and Prevention
- •Family History
- •Diet and Lifestyle
- •Prevention
- •Screening and Diagnosis
- •Current Screening Recommendations
- •Biopsy
- •Pathology
- •Prognosis
- •Treatment of Prostate Cancer
- •Treatment for Localized Prostate Cancer (T1, T2)
- •Radical Prostatectomy
- •EBRT
- •IMRT
- •Brachytherapy
- •Treatment for Locally Advanced Prostate Cancer (T3, T4)
- •EBRT with ADT
- •Radical Prostatectomy
- •Androgen-Deprivation Therapy
- •Summary
- •References
- •39: The Management of Testis Cancer
- •Presentation and Diagnosis
- •Serum Tumor Markers
- •Primary Surgery
- •Testis Preserving Surgery
- •Risk Stratification
- •Surveillance Versus Primary RPLND
- •Primary RPLND
- •Adjuvant Treatment for High Risk
- •Clinical Stage 1 Seminoma
- •Risk-Stratified Adjuvant Treatment
- •Adjuvant Radiotherapy
- •Adjuvant Low Dose Chemotherapy
- •Primary Combination Chemotherapy
- •Late Toxicity
- •Salvage Strategies
- •Conclusion
- •References
- •Index
32
Urinary Incontinence
Priya Padmanabhan and Roger Dmochowski
Urinary incontinence (UI) or the involuntary leakage of urine is a distressing and serious health problem. Its psychosocial and economic burden leads to significant quality of life issues. The prevalence of urinary incontinence (UI) differs by type, etiology, gender, age, and distribution1 (see Fig. 32.1). The three most common types of UI are stress urinary incontinence (SUI), urge urinary incontinence (UUI), or a combination of both, mixed urinary incontinence (MUI). The International Continence Society (ICS) defines SUI as involuntary leakage on effort or exertion, or on sneezing or coughing. UUI refers to involuntary leakage accompanied or immediately preceded by urgency. MUI is defined as a complaint of involuntary leakage associated with urgency and also with exertion, effort, sneezing, or coughing.3 UI is a manifestation of different types of injury and disease processes of the lower urinary tract or the nervous system that regulates it.4 This chapter describes the epidemiology, economics, and pathophysiology of incontinence. The importance of a proper work-up for accurate diagnosis is included. Conservative, pharmacological, and surgical therapy for women and men is delineated.
Epidemiology and Risk Factors
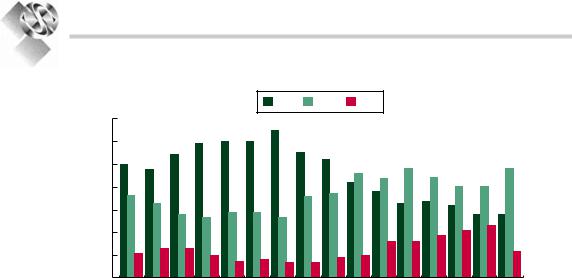
with fewer than half of all patients willing to report their symptoms to their physicians. The incidence of UI is estimated at 2.79 per 1,000 person-years.8 The prevalence rates are higher with advanced age. Of middle-aged and younger individuals, UI affects 4% of men and 28% of women, whereas in older individuals, UI affects 17% of men and 35% of women.4 The EPINCONT study, containing a cohort of 27,936 Norwegian women, showed a gradual increase in prevalence until 50 years (30%); a stabilization; slight decline until 70 years; and then an increased prevalence again. Of these women, 50% had SUI, 11% had UUI, and 36% had MUI9 (Fig. 32.2). Recently, the Boston Area Community Health (BACH) Survey identified the prevalence and
|
Mixed |
|
|
symptoms |
|
SUI |
OAB |
|
symptoms |
||
|
||
|
Mixed |
|
|
incontinence |
|
|
UUI |
UI cannot be excluded from the discussion of chronic diseases. UI is more prevalent than hypertension, depression, and diabetes.5-7 While UI is exceedingly prevalent, it is underreported
Figure 32.1. Spectrum of urinary incontinence (Reprinted from Wein2. Copyright 2006, with permission from Elsevier).
C.R. Chapple and W.D. Steers (eds.), Practical Urology: Essential Principles and Practice, |
437 |
DOI: 10.1007/978-1-84882-034-0_32, © Springer-Verlag London Limited 2011 |
|
438
PRaCtiCal URology: ESSEntial PRinCiPlES and PRaCtiCE
|
|
|
|
|
|
|
SUI |
|
MUI |
UUI |
|
|
|
|
|
|
women |
70 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
60 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
incontinent |
50 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
40 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
30 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
of |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Percentage |
20 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
10 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
0 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Total 2025- |
30- |
35- |
40- |
45- |
50- |
55- |
6065- 70- |
75- |
80- |
85- |
90+ |
||||
|
|
|||||||||||||||
|
|
24 |
29 |
34 |
39 |
44 |
49 |
54 |
59 |
64 |
69 |
74 |
79 |
84 |
89 |
|
|
|
|
|
|
|
|
|
Age |
|
|
|
|
|
|
|
|
Figure 32.2. Prevalence of incontinence by subtype and age among incontinent women as reported in the EPinCont survey.10
risk factors for UI in racially diverse populations.11 The survey reported a weekly UI prevalence rate of 8%, 10.4% in women and 5.3% in men. White women were more likely than Black and Hispanic women to report UI (11.7% vs. 9.4% and 14.5%, respectively). White women also reported more SUI (35.4% vs. 9.4% and 14.5%, respectively) and UUI (13.4% vs. 3.3% and 10.8%, respectively). No variability was reported among men based on race or ethnicity.
Aging and age-related changes in bladder function play a significant role in the development of UI. There is an increased frequency of uninhibited detrusor contractions, impaired bladder contractility, abnormal detrusor relaxation, and reduction in bladder capacity.12 This parallels an age-related increase in nocturnal urine production, increase in prostatic size in men, and urethral shortening and sphincter weakening in women. Elderly are more likely to become incontinent following incontinencepromoting factors, such as constipation, obesity, and polyuria from uncontrolled hypoglycemia, hypercalcemia, or diuretic therapy.13-16 Other risk factors include cognitive dysfunction, functional impairment, gait abnormality, diuretic therapy, obesity, and coexisting morbidities, i.e., cerebrovascular disease, diabetes radical pelvic surgery, or autonomic neuropathy. The occurrence of cerebrovascular disease doubles the risk for UI in older women. It is clear that UI increases proportionally with a rising BMI. The effects of smoking cannot be underestimated. Smoking-related illnesses, directly or indirectly,
cause increased coughing (chronic obstructive pulmonary disease) and subsequent UI. Female gender alone remains an irreversible predisposing factor for UI. Childbearing (particularly vaginal) and parity are two of the most wellestablished risk factors among women for developing UI. Genital abnormalities such as hypospadias, epispadias, and ambiguous genitalia can compromise continence.17-21
Complications
and Consequences
The impact of UI on quality of life in terms of psychosocial and economic burden cannot be understated. UI leads to embarrassment, loss of self-confidence, poor self-esteem,12 and avoidance of social activities. Sixty percent will develop depressive symptoms. The unpredictability of UI leads to withdrawal and social isolation. Physical limitations of elderly with UI compromise functional status and hasten the progression of their immobility. Sexual relationships are affected due to a fear of involuntary urine loss during sexual intercourse. Sexual dysfunction is independently associated with incontinence in older men.22-25
The incidence of falls and consequent fractures increases significantly in women aged over 65 years. Twenty percent to 40% of these age women will fall within 1 year, and 10% of these falls will result in a fracture (usually hip). Thirty
439
URinaRy inContinEnCE
percent of women with UI over 65 years will be |
these theories. In summary, there is damage to |
hospitalized within 1 year. Older men with UI |
afferent or efferent pathways, leading to |
are twice as likely to be hospitalized over a |
decreased capacity for increased afferent infor- |
12-month period. There is a strong association |
mation, decreased suprapontine inhibition, and |
between UI, acute hospitalization, institutional- |
increased sensitivity to contraction-mediated |
ization, and death. UI is most alarmingly associ- |
transmitters.33,34 |
ated with increased mortality.12,26 |
The micturition reflexes involve several neu- |
Daily costs associated with UI are not insig- |
rotransmitters and transmitter systems which |
nificant. Protective garments and bedding are |
may be targets for drugs aimed at micturition |
expensive and often not covered by private |
control. Glutamate likely acts as an excitatory |
insurance or Medicare. The productivity of the |
transmitter in the supraspinal control circuitry |
individual and relative caregiver may be com- |
and in the efferent limb of the pontine micturi- |
promised in coping with the unpredictability of |
tion center and the preganglionic neuron. Other |
UI. UI is the most common cause of institution- |
substances, such as GABA, serotonin, dopamine, |
alization of elderly with relatives unable to meet |
and norepinephrine, can exert modulatory |
their needs. In long-term care facilities, there is |
effects on the glutamatergic mechanisms con- |
an additional $5,000 burden to total health care |
trolling micturition, and the receptors for these |
cost per resident with UI. In 2000, the estimated |
substances may be potential sites for drug inter- |
direct cost of UI in the United States was $19.5 |
vention. GABA may act as an inhibitory neu- |
billion.12,22,27 |
rotransmitter in the brain and depress excitatory |
|
(diencephalon) or inhibitory (mesencephalon |
Pathophysiology |
and telencephalon) mechanisms for micturition |
control. The serotonergic input from the raphe |
|
|
nucleus and multiple serotonin 5-HT receptors |
Classically, the pathophysiology of UI is |
at afferent and efferent impulse processing sites |
described as either an overactive detrusor (OAB) |
causes inhibition of bladder contractions. Thus, |
or an incompetent urethral sphincter. The |
drugs interfering with serotonin reuptake (i.e., |
underlying pathophysiology of OAB can relate |
serotonin reuptake inhibitors) may have the |
to alterations in any of the reflex cycles in nor- |
opposite effect. Central dopaminergic and nora- |
mal micturition or morphological changes in |
drenergic pathways may have excitatory and |
the smooth muscle, nerves, or urothelium. The |
inhibitory effects on bladder function, yet drugs |
three main theories for the cause of OAB are: the |
selectively acting at the dopaminergic and |
myogenic or muscle-related theory, neurogenic |
adrenoreceptors have not been established.35 |
or nerve-related theory, and the autonomous |
SUI results from bladder neck/urethral |
bladder theory. In the myogenic theory, partial |
hypermobility and/or neuromuscular defects, |
denervation of the detrusor, regardless of etiol- |
i.e., intrinsic sphincter deficiency. This occurs |
ogy, can alter the smooth muscle leading to |
when the intra-abdominal pressure exceeds |
increased excitability and electrical coupling |
urethral resistance. Among women, these |
between cells.28-30 The neurogenic theory sug- |
changes occur due to weak collagen, advanced |
gests that damage to central inhibitory pathways |
age, pregnancy, obesity, advanced pelvic pro- |
in the brain or spinal cord or sensitization of |
lapse,and chronic obstructive airway disease.4,36 |
peripheral afferent terminals in the bladder can |
In men, SUI is due to an iatrogenic cause. A rad- |
unmask primitive voiding reflexes that trigger |
ical prostatectomy can injure the sphincteric |
detrusor overactivity (DO).31 The newest of the |
mechanism (rhabdosphincter) or cause bladder |
three theories, autonomous bladder theory, |
dysfunction. Suggested mechanisms for sphinc- |
notes that the detrusor is modular (i.e., circum- |
teric injury following a radical prostatectomy |
scribed areas of muscle). During normal filling, |
include: ischemia and immobilization by scar, |
the autonomous activity with nonmicturition |
atrophy, direct pudendal nerve injury, or short- |
contractions and phasic sensory discharge can |
ening of urethra below a critical functional |
become modified. This may lead to excessive |
length.37 |
excitatory inputs or failure of inhibiting inputs.32 |
Controversy surrounds urethral length as a |
Either way, the etiology is variable in different |
cause of incontinence. Technical modifications |
individuals and may include one or more of |
have been made to preserve as much external |

|
|
|
|
|
440 |
|
|
|
|
||||
|
|
PRaCtiCal URology: ESSEntial PRinCiPlES and PRaCtiCE |
||||
sphincter as possible following a radical pros- |
assessment should include a urinalysis (urine |
|||||
tatectomy.38 During a TURP, the verumontanum |
culture as needed) to exclude infection, hematu- |
|||||
marks the proximal part of the rhabdosphincter. |
ria or glucosuria, measurement of postvoid |
|||||
Resection distal to the verumontanum can lead |
residual to identify possible bladder dysfunction |
|||||
to sphincteric incompetence. Sphincteric dener- |
or obstruction, and a quality of life (QoL) ques- |
|||||
vation can also occur following other radical |
tionnaire34 for assessment of patient-reported |
|||||
pelvic procedures, i.e., abdominoperineal resec- |
outcomes (PRO). |
|
|
|||
tion, pelvic radiation. |
PROs are the best measure of patient health |
|||||
Among postprostatectomy incontinence (PPI) |
status as directly reported by the patient. They |
|||||
patients, 60% experience detrusor overactivity. |
assess outcomes of health-related quality of life |
|||||
The bladder dysfunction leading to UUI must |
(HRQL), symptoms, patient satisfaction, and |
|||||
be addressed prior to discussing surgical treat- |
social, emotional, and physical functioning. The |
|||||
ment of SUI.39 Groutz et al. used urodynamic |
value of these outcomes relies on the validity |
|||||
and clinical evidence to report on 83 men with |
and reliability of the survey tools being used. |
|||||
PPI. Intrinsic sphincter dysfunction was the |
PROs require linguistic validation and psycho- |
|||||
most common videourodynamic finding and |
metric evaluation of multiple language versions |
|||||
cause of incontinence in 73 (88%) men. Bladder |
of a questionnaire. Psychometric characteristics |
|||||
overactivity was the main cause of incontinence |
include: internal consistency, reliability, con- |
|||||
among 6 (7.2%) men. Overflow incontinence |
struct validity, and responsiveness. There are |
|||||
secondary to a bladder neck contracture was a |
multiple |
International Continence Society |
||||
significant cause of intrinsic sphincter defi- |
(ICS)–validated assessments which are actively |
|||||
ciency in 25 (30.1%) patients.40 |
utilized for incontinence in men and women, |
|||||
|
|
such as the ICS Male Questionnaire, Urogenital |
||||
Clinical Assessment |
Distress |
Index |
(UDI-6), or |
International |
||
Consultation on |
Incontinence |
Questionnaire |
||||
|
|
|||||
of Incontinent Patient |
(ICIQ). For example, the overactive bladder |
|||||
questionnaire (OAB-q) is a 33-item, self-admin- |
||||||
|
|
istered, disease-specific questionnaire to assess |
||||
Incontinence can cause tremendous suffering. |
symptom bother and HRQL in patients with |
|||||
Hence, it should be assessed thoroughly and |
OAB. This questionnaire was recently validated |
|||||
treated appropriately. A full and thorough his- |
and shown to have acceptable psychometric |
|||||
tory and physical exam is an important first step |
characteristics in multiple languages (Danish, |
|||||
in directing appropriate investigations.Providers |
German, Polish, Sweden, and Turkish).41 |
|||||
should examine fluid intake, assess volume of |
Patient-completed voiding diaries are an inte- |
|||||
urine lost, number and type of pads used, |
gral measurement tool for those presenting with |
|||||
strength of urinary stream, stress maneuvers or |
complaints of incontinence associated with |
|||||
changes in posture associated with urine loss, |
urgency. Patients are given standard instruc- |
|||||
and if urgency is associated with leakage. Add- |
tions to record micturition events (± voided vol- |
|||||
itional information should be collected regard- |
umes) and incontinence episodes, while also |
|||||
ing risk factors and predisposing factors. |
recording whether the void or leakage episode is |
|||||
Medication history,including diuretics or hyper- |
associated with a sense of urgency. Brown et al. |
|||||
osmolar infusions, anticholinergics, narcotics, |
examined the test-retest reliability and validity |
|||||
sedatives, and hypnotics, is important to docu- |
of 7-day voiding diaries in the assessment of |
|||||
ment. These may be associated with functional |
OAB symptoms. The diary demonstrated excel- |
|||||
incontinence, especially among the elderly.12 |
lent reliability with respect to the symptoms of |
|||||
Physical examination should include a complete |
“strong urge,” diurnal and nocturnal micturi- |
|||||
neurologic, abdominal, urogenital, pelvic, and |
tions, total incontinence, and urgency inconti- |
|||||
rectal examination. Female pelvic exam should |
nence episodes.42 Short voiding diaries have |
|||||
make note of urethral pathology, urethral hyper- |
been shown to be just as reliable and valid as |
|||||
mobility, prolapse, and apical support. Anal bul- |
traditional 7-day diaries and are less burden- |
|||||
bocavernosus reflexes should be assessed. |
some to patients.43,44 |
|
||||
Urethral sphincteric response to cough or |
Urodynamic studies are not mandatory, but |
|||||
Valsalva should be documented. The basic |
are crucial when |
a diagnosis |
is unclear, in |
|||
