
- •Preface and Acknowledgments
- •Contents
- •Contributors
- •1: Embryology for Urologists
- •Introduction
- •Renal Development
- •Pronephros
- •Mesonephros
- •Metanephros
- •Development of the Collecting System
- •Critical Steps in Further Development
- •Anomalies of the Kidney
- •Renal Agenesis
- •Renal Aplasia
- •Renal Hypoplasia
- •Renal Ectopia
- •Renal Fusion
- •Ureteral Development
- •Anomalies of Origin
- •Anomalies of Number
- •Incomplete Ureteral Duplication
- •Complete Ureteral Duplication
- •Ureteral Ectopia
- •Embryology of Ectopia
- •Clinical Correlation
- •Location of Ectopic Ureteral Orifices – Male (in Descending Order According to Incidence)
- •Symptoms
- •Ureteroceles
- •Congenital Ureteral Obstruction
- •Pipestem Ureter
- •Megaureter-Megacystis Syndrome
- •Prune Belly Syndrome
- •Vascular Ureteral Obstructions
- •Division of the Urogenital Sinus
- •Bladder Development
- •Urachal Anomalies
- •Cloacal Duct Anomalies
- •Other Bladder Anomalies
- •Bladder Diverticula
- •Bladder Extrophy
- •Gonadal Development
- •Testicular Differentiation
- •Ovarian Differentiation
- •Gonadal Anomalies
- •Genital Duct System
- •Disorders of Testicular Function
- •Female Ductal Development
- •Prostatic Urethral Valves
- •Gonadal Duct Anomalies
- •External Genital Development
- •Male External Genital Development
- •Female External Genital Development
- •Anomalies of the External Genitalia
- •References
- •2: Gross and Laparoscopic Anatomy of the Upper Urinary Tract and Retroperitoneum
- •Overview
- •The Kidneys
- •The Renal Vasculature
- •The Renal Collecting System
- •The Ureters
- •Retroperitoneal Lymphatics
- •Retroperitoneal Nerves
- •The Adrenal Glands
- •References
- •3: Gross and Laparoscopic Anatomy of the Lower Urinary Tract and Pelvis
- •Introduction
- •Female Pelvis
- •Male Pelvis
- •Pelvic Floor
- •Urinary Bladder
- •Urethra
- •Male Urethra
- •Female Urethra
- •Sphincter Mechanisms
- •The Bladder Neck Component
- •The Urethral Wall Component
- •The External Urethral Sphincter
- •Summary
- •References
- •4: Anatomy of the Male Reproductive System
- •Testis and Scrotum
- •Spermatogenesis
- •Hormonal Regulation of Spermatogenesis
- •Genetic Regulation of Spermatogenesis
- •Epididymis and Ductus Deferens
- •Accessory Sex Glands
- •Prostate
- •Seminal Vesicles
- •Bulbourethral Glands
- •Penis
- •Erection and Ejaculation
- •References
- •5: Imaging of the Upper Tracts
- •Anatomy of the Upper Tracts and Introduction to Imaging Modalities
- •Introduction
- •Renal Upper Tract Basic Anatomy
- •Modalities Used for Imaging the Upper Tracts
- •Ultrasound
- •Radiation Issues
- •Contrast Issues
- •Renal and Upper Tract Tumors
- •Benign Renal Tumors
- •Transitional Cell Carcinoma
- •Renal Mass Biopsy
- •Renal Stone Disease
- •Ultrasound
- •Plain Radiographs and IVU
- •Renal Cystic Disease
- •Benign Renal Cysts
- •Hereditary Renal Cystic Disease
- •Complex Renal Cysts
- •Renal Trauma
- •References
- •Introduction
- •Pathophysiology
- •Susceptibility and Resistance
- •Epidemiological Breakpoints
- •Clinical Breakpoints
- •Pharmacodynamic Parameters
- •Pharmacokinetic Parameters
- •Fosfomycin
- •Nitrofurantoin
- •Pivmecillinam
- •b-Lactam-Antibiotics
- •Penicillins
- •Cephalosporins
- •Carbapenems
- •Aminoglycosides
- •Fluoroquinolones
- •Trimethoprim, Cotrimoxazole
- •Glycopeptides
- •Linezolid
- •Conclusion
- •References
- •7: An Overview of Renal Physiology
- •Introduction
- •Body Fluid Compartments
- •Regulation of Potassium Balance
- •Regulation of Acid–Base Balance
- •Diuretics
- •Suggested Reading
- •8: Ureteral Physiology and Pharmacology
- •Ureteral Anatomy
- •Modulation of Peristalsis
- •Ureteral Pharmacology
- •Conclusion
- •References
- •Introduction
- •Afferent Signaling Pathways
- •Efferent Signaling
- •Parasympathetic Nerves
- •Sympathetic Nerves
- •Vesico-Spinal-Vesical Micturition Reflex
- •Peripheral Targets
- •Afferent Signaling Mechanisms
- •Urothelium
- •Myocytes
- •Cholinergic Receptors
- •Muscarinic Receptors
- •Nicotinic Receptors
- •Adrenergic Receptors (ARs)
- •a-Adrenoceptors
- •b-Adrenoceptors
- •Transient Receptor Potential (TRP) Receptors
- •Phosphodiesterases (PDEs)
- •CNS Targets
- •Opioid Receptors
- •Serotonin (5-HT) Mechanisms
- •g-Amino Butyric Acid (GABA) Mechanisms
- •Gabapentin
- •Neurokinin and Neurokinin Receptors
- •Summary
- •References
- •10: Pharmacology of Sexual Function
- •Introduction
- •Sexual Desire/Arousal
- •Endocrinology
- •Steroids in the Male
- •Steroids in the Female
- •Neurohormones
- •Neurotransmitters
- •Dopamine
- •Serotonin
- •Pharmacological Strategies
- •CNS Drugs
- •Enzyme-inducing Antiepileptic Drugs
- •Erectile Function
- •Ejaculatory Function
- •Premature Ejaculation
- •Abnormal Ejaculation
- •Conclusions
- •References
- •Epidemiology
- •Calcium-Based Urolithiasis
- •Uric Acid Urolithiasis
- •Infectious Urolithiasis
- •Cystine-Based Urolithiasis
- •Aims
- •Who Deserves Metabolic Evaluation?
- •Metabolic Workup for Stone Producers
- •Medical History and Physical Examination
- •Stone Analysis
- •Serum Chemistry
- •Urine Evaluation
- •Urine Cultures
- •Urinalysis
- •Twenty-Four Hour Urine Collections
- •Radiologic Imaging
- •Medical Management
- •Conservative Management
- •Increased Fluid Intake
- •Citrus Juices
- •Dietary Restrictions
- •Restricted Oxalate Diet
- •Conservative Measures
- •Selective Medical Therapy
- •Absorptive Hypercalciuria
- •Thiazide
- •Orthophosphate
- •Renal Hypercalciuria
- •Primary Hyperparathyroidism
- •Hyperuricosuric Calcium Oxalate Nephrolithiasis
- •Enteric Hyperoxaluria
- •Hypocitraturic Calcium Oxalate Nephrolithiasis
- •Distal Renal Tubular Acidosis
- •Chronic Diarrheal States
- •Thiazide-Induced Hypocitraturia
- •Idiopathic Hypocitraturic Calcium Oxalate Nephrolithiasis
- •Hypomagnesiuric Calcium Nephrolithiasis
- •Gouty Diathesis
- •Cystinuria
- •Infection Lithiasis
- •Summary
- •References
- •12: Molecular Biology for Urologists
- •Introduction
- •Inherited Changes in Cancer Cells
- •VEGR and Cell Signaling
- •Targeting mTOR
- •Conclusion
- •References
- •13: Chemotherapeutic Agents for Urologic Oncology
- •Introduction
- •Bladder Cancer
- •Muscle Invasive Bladder Cancer
- •Metastatic Bladder Cancer
- •Conclusion
- •Prostate Cancer
- •Other Chemotherapeutic Drugs or Combinations for Treating HRPC
- •Conclusion
- •Renal Cell Carcinoma
- •Chemotherapy
- •Immunotherapy
- •Angiogenesis Inhibitor Drugs
- •Conclusion
- •Testicular Cancer
- •Stage I Seminoma
- •Stage I non-seminomatous Germ Cell Tumours (NSGCT)
- •Metastatic Germ Cell Tumours
- •Low-Volume Metastatic Disease (Stage II A/B)
- •Advanced Metastatic Disease
- •Salvage Chemotherapy for Relapsed or Refractory Disease
- •Conclusion
- •Penile Cancer
- •Side Effects of Chemotherapy
- •Conclusion
- •References
- •14: Tumor and Transplant Immunology
- •Antibodies
- •Cytotoxic and T-helper Cells
- •Immunosuppression
- •Induction Therapy
- •Maintenance Therapy
- •Rejection
- •Posttransplant Lymphoproliferative Disease
- •Summary
- •References
- •15: Pathophysiology of Renal Obstruction
- •Causes of Renal Obstruction
- •Effects on Prenatal Development
- •Prenatal Hydronephrosis
- •Spectrum of Renal Abnormalities
- •Renal Functional Changes
- •Renal Growth/Counterbalance
- •Vascular Changes
- •Inflammatory Mediators
- •Glomerular Development Changes
- •Mechanical Stretch of Renal Tubules
- •Unilateral Versus Bilateral
- •Limitations of Animal Models
- •Future Research
- •Issues in Patient Management
- •Diagnostic Imaging
- •Ultrasound
- •Intravenous Urography
- •Antegrade Urography and the Whitaker Test
- •Nuclear Renography
- •Computed Tomography
- •Magnetic Resonance Urography
- •Hypertension
- •Postobstructive Diuresis
- •References
- •Introduction
- •The Normal Lower Urinary Tract
- •Anatomy
- •Storage Function
- •Voiding Function
- •Neural Control
- •Symptoms
- •Flow Rate and Post-void Residual
- •Voiding Cystometry
- •Male
- •Female
- •Neurourology
- •Conclusions
- •References
- •17: Urologic Endocrinology
- •The Testis
- •Normal Androgen Metabolism
- •Epidemiological Aspects
- •Prostate
- •Brain
- •Muscle Mass and Adipose Tissue
- •Bones
- •Ematopoiesis
- •Metabolism
- •Cardiovascular System
- •Clinical Assessment
- •Biochemical Assessment
- •Treatment Modalities
- •Oral Preparations
- •Parenteral Preparations
- •Transdermal Preparations
- •Side Effects and Treatment Monitoring
- •Body Composition
- •Cognitive Decline
- •Bone Metabolism
- •The Kidneys
- •Endocrine Functions of the Kidney
- •Erythropoietin
- •Calcitriol
- •Renin
- •Paraneoplastic Syndromes
- •Hypercalcemia
- •Hypertension
- •Polycythemia
- •Other Endocrine Abnormalities
- •References
- •General Physiology
- •Prostate Innervation
- •Summary
- •References
- •Wound Healing
- •Inflammation
- •Proliferation
- •Remodeling
- •Principles of Plastic Surgery
- •Tissue Characteristics
- •Grafts
- •Flap
- •References
- •Lower Urinary Tract Symptoms
- •Storage Phase
- •Voiding Phase
- •Return to Storage Phase
- •Urodynamic Parameters
- •Urodynamic Techniques
- •Volume Voided Charts
- •Pad Testing
- •Typical Test Schedule
- •Uroflowmetry
- •Post Voiding Residual
- •Further Diagnostic Evaluation of Patients
- •Cystometry with or Without Video
- •Cystometry
- •Videocystometrography (Cystometry + Cystourethrography)
- •Cystometric Findings
- •Comment:
- •Measurements During the Storage Phase:
- •Measurements During the Voiding Phase:
- •Abnormal Function
- •Disorders of Sensation
- •Causes of Hypersensitive Bladder Sensation
- •Causes of Hyposensitive Bladder Sensation
- •Disorders of Detrusor Motor Function
- •Bladder Outflow Tract Dysfunction
- •Detrusor–Urethral Dyssynergia
- •Detrusor–Bladder Neck Dyssynergia
- •Detrusor–Sphincter Dyssynergia
- •Complex Urodynamic Investigation
- •Urethral Pressure Measurement
- •Technique
- •Neurophysiological Evaluation
- •Conclusion
- •References
- •Endoscopy
- •Cystourethroscopy
- •Ureteroscopy and Ureteropyeloscopy
- •Nephroscopy
- •Virtual Reality Simulators
- •Lasers
- •Clinical Application of Lasers
- •Condylomata Acuminata
- •Urolithiasis
- •Benign Prostatic Hyperplasia
- •Ureteral and Urethral Strictures
- •Conclusion
- •References
- •Introduction
- •The Prostatitis Syndromes
- •The Scope of the Problem
- •Category III CP/CPPS
- •The Goal of Treatment
- •Conservative Management
- •Drug Therapy
- •Antibiotics
- •Anti-inflammatories
- •Alpha blockers
- •Hormone Therapies
- •Phytotherapies
- •Analgesics, muscle relaxants and neuromodulators
- •Surgery
- •A Practical Management Plan
- •References
- •Orchitis
- •Definition and Etiology
- •Clinical Signs and Symptoms
- •Diagnostic Evaluation
- •Treatment of Infectious Orchitis
- •Epididymitis
- •Definition and Etiology
- •Clinical Signs and Symptoms
- •Diagnostic Evaluation of Epididymitis
- •Treatment of Acute Epididymitis
- •Treatment of Chronic Epididymitis
- •Treatment of Spermatic Cord Torsion
- •Fournier’s Gangrene
- •Definition and Etiology
- •Risk Factors
- •Clinical Signs and Symptoms
- •Diagnostic Evaluation
- •Treatment
- •References
- •Fungal Infections
- •Candidiasis
- •Aspergillosis
- •Cryptococcosis
- •Blastomycosis
- •Coccidioidomycosis
- •Histoplasmosis
- •Radiographic Findings
- •Treatment
- •Tuberculosis
- •Clinical Manifestations
- •Diagnosis
- •Treatment
- •Schistosomiasis
- •Clinical Manifestations
- •Diagnosis
- •Treatment
- •Filariasis
- •Clinical Manifestations
- •Diagnosis
- •Treatment
- •Onchocerciasis
- •References
- •25: Sexually Transmitted Infections
- •Introduction
- •STIs Associated with Genital Ulcers
- •Herpes Simplex Virus
- •Diagnosis
- •Treatment
- •Chancroid
- •Diagnosis
- •Treatment
- •Syphilis
- •Diagnosis
- •Treatment
- •Lymphogranuloma Venereum
- •Diagnosis
- •Treatment
- •Chlamydia
- •Diagnosis
- •Treatment
- •Gonorrhea
- •Diagnosis
- •Treatment
- •Trichomoniasis
- •Diagnosis
- •Treatment
- •Human Papilloma Virus
- •Diagnosis
- •Treatment
- •Scabies
- •Diagnosis
- •Treatment
- •References
- •26: Hematuria: Evaluation and Management
- •Introduction
- •Classification of Hematuria
- •Macroscopic Hematuria
- •Microscopic Hematuria
- •Dipstick Hematuria
- •Pseudohematuria
- •Factitious Hematuria
- •Menstruation
- •Aetiology
- •Malignancy
- •Urinary Calculi
- •Infection and Inflammation
- •Benign Prostatic Hyperplasia
- •Trauma
- •Drugs
- •Nephrological Causes
- •Assessment
- •History
- •Examination
- •Investigations
- •Dipstick Urinalysis
- •Cytology
- •Molecular Tests
- •Blood Tests
- •Flexible Cystoscopy
- •Upper Urinary Tract Evaluation
- •Renal USS
- •KUB Abdominal X-Ray
- •Intravenous Urography (IVU)
- •Computed Tomography (CT)
- •Retrograde Urogram Studies
- •Magnetic Resonance Imaging (MRI)
- •Additional Tests and Renal Biopsy
- •Intractable Hematuria
- •Loin Pain Hematuria Syndrome
- •References
- •27: Benign Prostatic Hyperplasia (BPH)
- •Historical Background
- •Pathophysiology
- •Patient Assessment
- •Treatment of BPH
- •Watchful Waiting
- •Drug Therapy
- •Interventional Therapies
- •Conclusions
- •References
- •28: Practical Guidelines for the Treatment of Erectile Dysfunction and Peyronie´s Disease
- •Erectile Dysfunction
- •Introduction
- •Diagnosis
- •Basic Evaluation
- •Cardiovascular System and Sexual Activity
- •Optional Tests
- •Treatment
- •Medical Treatment
- •Oral Agents
- •Phosphodiesterase Type 5 (PDE 5) Inhibitors
- •Nonresponders to PDE5 Inhibitors
- •Apomorphine SL
- •Yohimbine
- •Intracavernosal and Intraurethral Therapy
- •Intracavernosal Injection (ICI) Therapy
- •Intraurethral Therapy
- •Vacuum Constriction Devices
- •Surgical Therapy
- •Conclusion
- •Peyronie´s Disease (PD)
- •Introduction
- •Oral Drug Therapy
- •Intralesional Drug Therapy
- •Iontophoresis
- •Radiation Therapy
- •Surgical Therapy
- •References
- •29: Premature Ejaculation
- •Introduction
- •Epidemiology
- •Defining Premature Ejaculation
- •Voluntary Control
- •Sexual Satisfaction
- •Distress
- •Psychosexual Counseling
- •Pharmacological Treatment
- •On-Demand Treatment with Tramadol
- •Topical Anesthetics
- •Phosphodiesterase Inhibitors
- •Surgery
- •Conclusion
- •References
- •30: The Role of Interventional Management for Urinary Tract Calculi
- •Contraindications to ESWL
- •Complications of ESWL
- •PCNL Access
- •Instrumentation for PCNL
- •Nephrostomy Drains Post PCNL
- •Contraindications to PCNL
- •Complications of PCNL
- •Semirigid Ureteroscopy
- •Flexible Ureteroscopy
- •Electrohydraulic Lithotripsy (EHL)
- •Ultrasound
- •Ballistic Lithotripsy
- •Laser Lithotripsy
- •Ureteric Stents
- •Staghorn Calculi
- •Lower Pole Stones
- •Horseshoe Kidneys and Stones
- •Calyceal Diverticula Stones
- •Stones and PUJ Obstruction
- •Treatment of Ureteric Colic
- •Medical Expulsive Therapy (MET)
- •Intervention for Ureteric Stones
- •Stones in Pregnancy
- •Morbid Obesity
- •References
- •Anatomy and Function
- •Pathophysiology
- •Management
- •Optical Urethrotomy/Dilatation
- •Urethral Stents
- •Preoperative Assessment
- •Urethroplasty
- •Anastomotic Urethroplasty
- •Substitution Urethroplasty
- •Grafts Versus Flaps
- •Oral Mucosal Grafts
- •Tissue Engineering
- •Graft Position
- •Conclusion
- •References
- •32: Urinary Incontinence
- •Epidemiology and Risk Factors
- •Pathophysiology
- •Urge Incontinence
- •Conservative Treatments
- •Pharmacotherapy
- •Invasive/ Surgical Therapies
- •Stress Urinary Incontinence
- •Male SUI Therapies
- •Female SUI Therapies
- •Mixed Urinary Incontinence
- •Conclusions
- •References
- •33: Neurogenic Bladder
- •Introduction
- •Examination and Diagnostic Tests
- •History and Physical Examination
- •Imaging
- •Urodynamics (UDS)
- •Evoked Potentials
- •Classifications
- •Somatic Pathways
- •Brain Lesions
- •Cerebrovascular Accident (CVA)
- •Parkinson’s Disease (PD)
- •Multiple Sclerosis
- •Huntington’s Disease
- •Dementias
- •Normal Pressure Hydrocephalus (NPH)
- •Tumors
- •Psychiatric Disorders
- •Spinal Lesions and Pathology
- •Intervertebral Disk Prolapse
- •Spinal Cord Injury (SCI)
- •Transverse Myelitis
- •Peripheral Neuropathies
- •Metabolic Neuropathies
- •Pelvic Surgery
- •Treatment
- •Summary
- •References
- •34: Pelvic Prolapse
- •Introduction
- •Epidemiology
- •Anatomy and Pathophysiology
- •Evaluation and Diagnosis
- •Outcome Measures
- •Imaging
- •Urodynamics
- •Indications for Management
- •Biosynthetics
- •Surgical Management
- •Anterior Compartment Repair
- •Uterine/Apical Prolapse
- •Enterocele Repair
- •Conclusion
- •References
- •35: Urinary Tract Fistula
- •Introduction
- •Urogynecologic Fistula
- •Vesicovaginal Fistula
- •Etiology and Risk Factors
- •Clinical Factors
- •Evaluation and Diagnosis
- •Pelvic Examination
- •Cystoscopy
- •Imaging
- •Treatment
- •Conservative Management
- •Surgical Management
- •Urethrovaginal Fistula
- •Etiology and Presentation
- •Diagnosis and Management
- •Ureterovaginal Fistula
- •Etiology and Presentation
- •Diagnosis and Management
- •Vesicouterine Fistula
- •Etiology and Presentation
- •Diagnosis and Management
- •Uro-Enteric Fistula
- •Vesicoenteric Fistula
- •Pyeloenteric Fistula
- •Urethrorectal Fistula
- •References
- •36: Urologic Trauma
- •Introduction
- •Kidney
- •Expectant Management
- •Endovascular Therapy
- •Operative Intervention
- •Operative Management: Follow-up
- •Reno-Vascular Injuries
- •Pediatric Renal Injuries
- •Adrenal
- •Ureter
- •Diagnosis
- •Treatment
- •Delayed Diagnosis
- •Bladder and Posterior Urethra
- •Bladder Injuries: Initial Management
- •Bladder Injuries: Formal Repair
- •Anterior Urethral Trauma
- •Fractured Penis
- •Penile Amputation
- •Scrotal and Testicular Trauma
- •Imaging
- •CT-IVP (CT with Delayed Images)
- •Technique
- •Cystogram
- •Technique
- •Retrograde Urethrogram (RUG)
- •Technique
- •Retrograde Pyelogram (RPG)
- •Technique
- •One-Shot IVP
- •Technique
- •References
- •37: Bladder Cancer
- •Who Should Be Investigated?
- •Epidemiology
- •Risk Factors
- •Role of Screening
- •Signs and Symptoms
- •Imaging
- •Cystoscopy
- •Urine Tests
- •PDD-Assisted TUR
- •Pathology
- •NMIBC and Risk Groups
- •Intravesical Chemotherapy
- •Intravesical Immunotherapy
- •Immediate Cystectomy and CIS
- •Radical Cystectomy with Pelvic Lymph Node Dissection
- •sexual function-preserving techniques
- •Bladder-Preservation Treatments
- •Neoadjuvant Chemotherapy
- •Adjuvant Chemotherapy
- •Preoperative Radiotherapy
- •Follow-up After TUR in NMIBC
- •References
- •38: Prostate Cancer
- •Introduction
- •Epidemiology
- •Race
- •Geographic Variation
- •Risk Factors and Prevention
- •Family History
- •Diet and Lifestyle
- •Prevention
- •Screening and Diagnosis
- •Current Screening Recommendations
- •Biopsy
- •Pathology
- •Prognosis
- •Treatment of Prostate Cancer
- •Treatment for Localized Prostate Cancer (T1, T2)
- •Radical Prostatectomy
- •EBRT
- •IMRT
- •Brachytherapy
- •Treatment for Locally Advanced Prostate Cancer (T3, T4)
- •EBRT with ADT
- •Radical Prostatectomy
- •Androgen-Deprivation Therapy
- •Summary
- •References
- •39: The Management of Testis Cancer
- •Presentation and Diagnosis
- •Serum Tumor Markers
- •Primary Surgery
- •Testis Preserving Surgery
- •Risk Stratification
- •Surveillance Versus Primary RPLND
- •Primary RPLND
- •Adjuvant Treatment for High Risk
- •Clinical Stage 1 Seminoma
- •Risk-Stratified Adjuvant Treatment
- •Adjuvant Radiotherapy
- •Adjuvant Low Dose Chemotherapy
- •Primary Combination Chemotherapy
- •Late Toxicity
- •Salvage Strategies
- •Conclusion
- •References
- •Index
271
ovErviEw oF tHE EvalUation oF lowEr Urinary tract dysFUnction
It is our practice to fill the bladder initially in the supine position and the volume at first sensation of filling is noted. When the subject first experiences discomfort, the radiographic table is tipped toward the standing position and subsequent bladder filling discontinued when at the maximum tolerated capacity.During bladder filling the patient is asked to consciously suppress bladder contraction and may be asked to cough or heel bounce. The patient is then turned to the oblique position relative to the X-ray machine and asked to void into the flowmeter provided.
In units where a tipping table is not available, the study can be carried out in the sitting or standing position initially; but it is important to subsequently stand the patient upright at the end of the study to assess where there is postural detrusor instability and to determine whether there is stress incontinence; in the absence of radiological screening this is assessed with the patient standing with legs slightly apart and squatting.
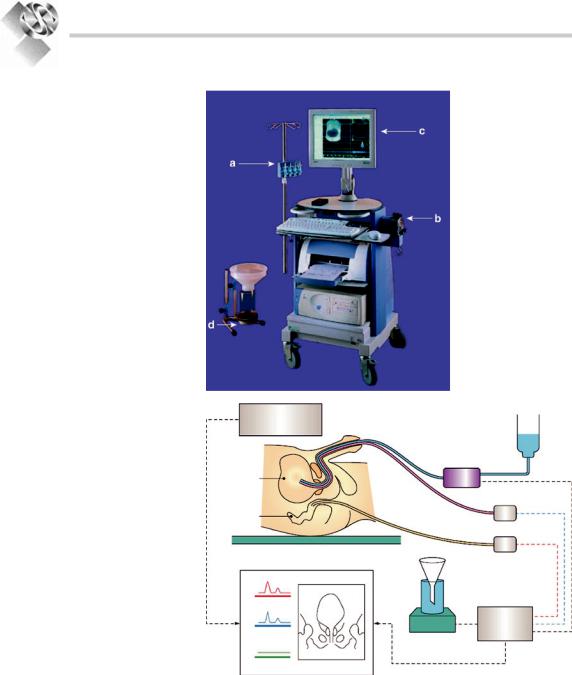
Throughout the study continuous rectal pressure, total bladder pressure and electronically subtracted detrusor pressure (total bladder pressure minus rectal pressure) measurements are sampled at a predetermined rate (usually 1 Hz) and the results displayed on the video display unit / stored to disc / polygraph chart recorder; depending on the equipment in use. Figure 20.4a and b shows a typical workstation and schematic.
Videodynamics provides an excellent method of evaluating the urethral outlet in female patients with urinary incontinence, males with complex voiding problems and are essential to the optimum management of neurological patients. Standing quietly and partially obliqued,the bladder neck position may be abnormally low, below the level of the upper third of the symphysis pubis, signifying loss of pelvic floor support in female patients with hypermobile urethras/ anatomical stress incontinence. Coughing or valsalva maneuvers cause these vesicourethral units to descend and leak. With termination of the increased intra-abdominal pressure the bladder neck quickly “springs back” to its original position terminating leakage. The semi-lateral/ oblique position enables to distinguish between the bladder neck from a dependent cystocele and it also helps to evaluate the size and functional significance of the cystocele.
Breaking or funneling of the bladder neck probably represents a normal finding,is common
in continent females, but should be distinguished from a rectangular-shaped incompetent bladder neck common in patients with intrinsic sphincter deficiency (ISD). Typically patients with pure ISD as the cause of their incontinence demonstrate severe leakage with minimal intra-abdom- inalpressureincreasesandminimalurethrovesical hypermobility. The urethra does not spring back but appears to hold open and continue leaking even after the stress event. Patients often have both bladder neck hypermobility and ISD and experience is necessary in order to interpret their relative functional significance.
Cystourethrography via the adjacent X-ray screening apparatus allows the synchronous display of pressure and flow, and also radiographic data relating to bladder morphology e.g. diverticula, vesicoureteric reflux and the appearances of the bladder outlet and urethra, to be displayed alongside the numerical data on a video display unit.
Cystometric Findings
As filling continues the patient is asked to confirm the following bladder sensations which are recorded on the computer:
•First desire to void
•Strong desire to void
•Desire at which the patient cannot delay micturition (Maximum cystometric capacity)
•Urgency – sudden compelling desire to void
•Bladder pain – should not occur during filling
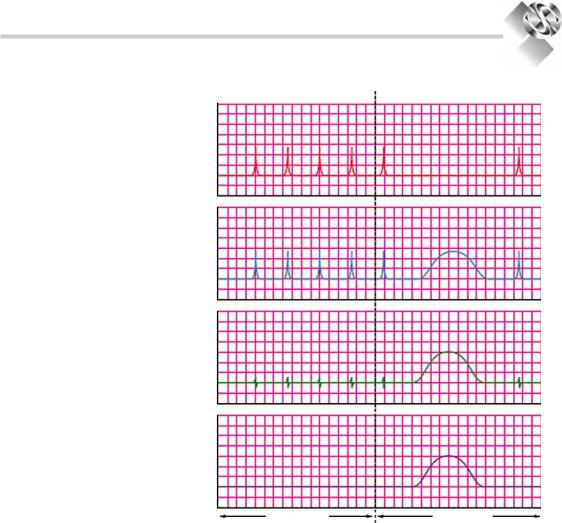
The computer calculates the pressures and plots them on a temporal graph. The above sensations are recorded at specific times and give an indication of how full the bladder was when these sensations occurred. Figure 20.5 shows a typical readout from the study, showing both storage and voiding phases with regular quality controls (coughing). The detrusor pressure is the result of the intravesical pressure minus the intra-abdominal pressure.
The four graphs in the order produced are:
•Intra-abdominal pressure (Pabd)
•Intra-vesical pressure (Pves)
•Detrusor pressure (Pdet)
•Urinary flow rate (Q)
272
Practical Urology: EssEntial PrinciPlEs and PracticE
Figure 20.4. (a) a typical workstation |
a |
|||||||
comprising: (a) transducers to be |
|
|
|
|
|
|
|
|
placed at height of patients symphysis |
|
|
|
|
|
|
|
|
pubis, (B) Pump for bladder filling, |
|
|
|
|
C |
|
|
|
|
|
|
|
|
|
|
|
|
(c) display, (d) uroflowmeter. (b) the |
|
|
|
|
|
|
|
|
bladder is filled at a predetermined |
|
|
|
|
|
|
|
|
A |
||||||||
rate with a radio-opaque contrast |
|
|
|
|
|
|
|
|
medium, with the simultaneous |
|
|
|
|
|
|
|
|
measurement of intra-vesical pressure |
|
|
|
|
|
|
|
|
and intra-abdominal pressure.the |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
B |
||
subtracted detrusor pressure is |
|
|
|
|
|
|
|
|
calculated automatically and flow is |
|
|
|
|
|
|
|
|
recorded with the flow meter.this |
|
|
|
|
|
|
|
|
information with accompanying |
|
|
|
|
|
|
|
|
radiographic pictures and a sound |
|
|
|
|
|
|
|
|
track can be recorded allowing |
|
|
|
|
|
|
|
|
subsequent review and analysis.22 |
|
|
|
|
|
|
|
|
|
D |
|
||||||
b |
X-ray |
|
|
|
|
|
screening unit |
|
|
|
Peristaltic |
|
|
pump |
|
Bladder |
|
|
Rectum |
|
|
Tilting table |
Pressure |
|
|
|
|
X-ray |
transducers |
|
|
|
|
Pabd |
|
|
Pves |
Control |
|
|
computer |
|
Pdet |
Flow |
|
meter |
|
|
|
|
|
Monitor display |
|
Practical Points: Since a number of variations in technique are currently available, the following points deserve specific consideration.
i.Type of catheter
a.Fluid-filled catheter – specify number of catheters, single or multiple lumens, type of catheter, size of catheter.
b.Catheter tip transducer – specifications vary between manufacturers; these catheters
tend to be expensive and rather too fragile for routine use.
ii.Measuring equipment.
A number of commercial urodynamic systems are currently available. These vary greatly in terms of sampling rate, associated computer software backup,and price.A major problem with existing computer programs is the ease with which such programs will
273
ovErviEw oF tHE EvalUation oF lowEr Urinary tract dysFUnction
Figure 20.5. a typical graphical display of the pressure flow data, showing both storage and voiding phases with regular coughing acting as a quality control (small blips in Pdet).the graph shows good contraction of the detrusor during the voiding phase and no contractions during the storage phase. not included are the sensations as described by the patient, which will be plotted along the x-axis at the time they occurred, allowing us to calculate volumes at which sensory perceptions occur.22
Pabd
(cm H2O)
Pves
(cm H2O)
Pdet
(cm H2O)
Flow rate (Q) (ml/s)
Filing phase |
Voiding phase |
record artifacts which can then bias the results of the subsequent automatic data analysis. The investigator is strongly advised not to rely upon the computer generated data sheets but to use an appropriate standardized reading sheet which allows interpretation of the urodynamic findings by the investigator.
iii.Test medium (liquid or gas)
This is obviously not applicable to catheter tip transducers. The advantage of equipment using gas as a medium is that it can be more compact and is therefore more easily portable. A major drawback with gas cystometry is its susceptibility to artifact being introduced by changes in the temperature of the gaseous medium; a far less important consideration when fluid is used.
iv.Position of patient (e.g. supine, sitting, or standing).
v.Type of filling
This may be by diuresis or catheter. Filling by catheter may be continuous or incremental; the precise filling rate should be stated (vide infra).When the incremental method is used the volume increment should be stated.
vi.Continuous or intermittent pressure measurement
Continuous pressure measurement is of greatest usefulness in clinical practice; in patients for example with a suprapubic catheter and no urethral access, staged measurement of pressures can be carried out through the suprapubic catheter.

|
|
|
|
274 |
|
|
|
|
|
|
|
|
|
|
|
Practical Urology: EssEntial PrinciPlEs and PracticE |
|
vii. Who carries out the study and how? – data |
Our experience would support the use of |
||||
quality |
|
|
graduated coughs as a means of assessing leakage, |
||
It is essential that urodynamic studies are |
ideally coupled with cystourethrography or vid- |
||||
carried out or supervised by experienced |
eocystometry. Basically, both tests suffer limita- |
||||
investigators:- |
|
|
tions.Since women leak with stress efforts in their |
||
a. Always take a clinical history of the patient |
everyday life and not with Valsalva, the Valsalva |
||||
leak point pressure serves at best as a surrogate |
|||||
before carrying out the study and counsel |
marker of sphincter competency. For the urethral |
||||
the patient before they attend on the day |
pressure profile, the methodology imposed by the |
||||
and at the start of the study as to the nature |
test (passive measurement, supine position) |
||||
of the test. |
|
|
negates the real life effect of the stress component |
||
|
|
over a presumably deficient sphincter. |
|||
b. Make sure the urodynamic equipment is |
|||||
|
|||||
regularly serviced and calibrate the trans- |
Comment: |
||||
ducers on a regular basis. |
|
||||
c. Make sure that the lines are zeroed at the |
i. Before starting to fill the bladder, the residual |
||||
start of the |
study, check subtraction is |
||||
urine may be measured.However,the removal |
|||||
perfect before starting the study with a |
|||||
of a large volume of residual urine may alter |
|||||
detrusor pressure between 0 and 5 cm |
|||||
detrusor function especially in neuropathic |
|||||
H2O, and every minute during the study |
|||||
disorders. Certain cystometric parameters |
|||||
ask the patient to cough and verify that |
may be significantly altered by the speed of |
||||
the rectal and vesical pressure lines track |
|||||
bladder filling. |
|||||
together in |
their response. If in doubt |
||||
ii. During cystometry it is taken for granted that |
|||||
about artifact, repeat the study. |
|
||||
|
the patient is awake, unanasthetized, and nei- |
||||
d. Choose the |
correct filling rate for |
the |
|||
ther sedated nor taking drugs that affect |
|||||
study, e.g. normal filling at 50 mL/min and |
|||||
bladder function. Any variations from this |
|||||
slower filling at a rate of 10–20 mL/min for |
|||||
ideal must be taken into account when inter- |
|||||
neuropaths and patients with a reduced |
|||||
preting results. |
|||||
functional capacity. |
|
||||
|
iii. In a small group of women who present with |
||||
e. Leak point pressure: |
|
||||
|
incontinence, urinary leakage cannot be |
||||
|
|
|
|
||
The abdominal pressure or vesical pres- |
demonstrated either clinically or radiograph- |
||||
ically. Conventional testing can be repeated |
|||||
sure at which leakage occurs is a major |
|||||
problem because there is no standard |
or continuous ambulatory urodynamic mon- |
||||
technique with regard to: |
|
itoring considered if available. |
|||
• |
Catheter caliber |
|
Measurements During the Storage Phase: |
||
• |
Presence of prolapse |
|
|||
|
|
||||
• Bladder volume at which the leakage is |
• Detrusor activity – during the storage phase |
||||
|
measured |
|
|
the detrusor muscle should be inactive.Any |
|
• |
Valsalva versus cough |
|
activity should be correlated with episodes |
||
• |
Straining |
(contraction/relaxation |
of |
of urgency and/or incontinence. The vol- |
|
|
pelvic floor) |
|
ume at which this occurred should be noted. |
||
• Absolute measurement or relative mea- |
Provocation maneuvers may be employed |
||||
to stimulate detrusor overactivity. |
|||||
|
surement compared to baseline |
|
|||
|
|
• Bladder compliance – describes the intrin- |
|||
• |
No defined threshold values for treat- |
||||
sic ability of the bladder to change in vol- |
|||||
|
ment decision |
|
|||
|
|
ume without significantly altering detrusor |
|||
The literature abounds with contradictory reports |
|||||
pressure. |
|||||
as to whether there is any correlation between |
• Bladder capacity – is the volume at the end |
||||
urethral pressure and leak point pressure.17,18 |
of the storage phase. It may be reduced |
|
