
Borchers Andrea Ann (ed.) Handbook of Signs & Symptoms 2015
.pdf
Medical Causes
Basal cell carcinoma. Most common in postmenopausal women, this nodular tumor has a central ulcer and a raised, poorly rolled border. Typically asymptomatic, the tumor may occasionally cause pruritus, bleeding, discharge, and a burning sensation.
Benign cysts. Epidermal inclusion cysts, the most common vulvar cysts, appear primarily on the labia majora and are usually round and asymptomatic. Occasionally, they become erythematous and tender.
Bartholin’s duct cysts are usually unilateral, tense, nontender, and palpable; they appear on the posterior labia minora and may cause minor discomfort during intercourse or, when large, difficulty with intercourse or even walking. Bartholin’s abscess, infection of a Bartholin’s duct cyst, causes gradual pain and tenderness and possibly vulvar swelling, redness, and deformity.
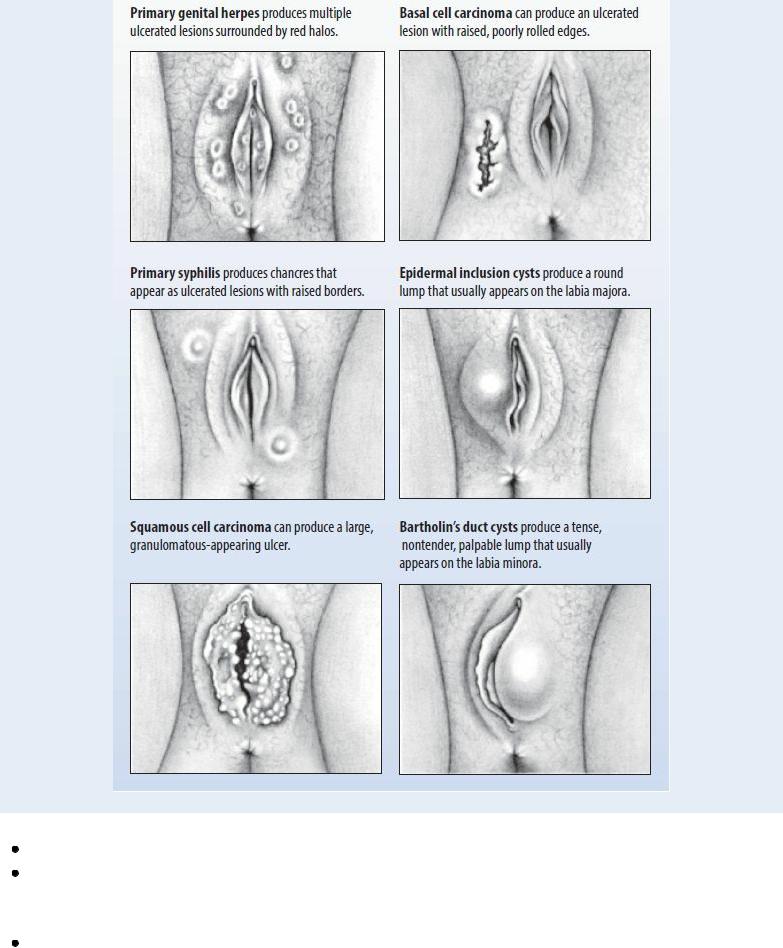
Recognizing Common Vulvar Lesions
Various disorders can cause vulvar lesions. For example, sexually transmitted diseases account for most vulvar lesions in premenopausal women, whereas vulvar tumors and cysts account for most lesions in women age 50 to 70. The illustrations below will help you recognize some of the most common lesions.
Benign vulvar tumors. Cystic or solid benign vulvar tumors are usually asymptomatic. Chancroid. Chancroid, a rare, sexually transmitted disease, causes painful vulvar lesions. Headache, malaise, and fever of 102.2°F (39°C) may occur, with enlarged, tender inguinal lymph nodes.
Genital warts. Genital warts, a sexually transmitted disease, produce painless warts on the vulva, vagina, and cervix. Warts start as tiny red or pink swellings that grow and become pedunculated. Multiple swellings with a cauliflower appearance are common. Other findings include pruritus, erythema, and a profuse, mucopurulent vaginal discharge. Patients frequently

complain of burning or paresthesia in the vaginal introitus.
Gonorrhea. Vulvar lesions, which usually are confined to Bartholin’s glands, may develop along with pruritus, a burning sensation, pain, and a green-yellow vaginal discharge, but most patients are asymptomatic. Other findings include dysuria and urinary incontinence; vaginal redness, swelling, bleeding, and engorgement; and severe pelvic and lower abdominal pain.
Granuloma inguinale. Initially, a single painless macule or papule appears on the vulva, ulcerating into a raised, beefy-red lesion with a granulated, friable border. Other painless and possibly foul-smelling lesions may occur on the labia, vagina, or cervix. These become infected and painful, and regional lymph nodes enlarge and may become tender. Systemic effects include fever, weight loss, and malaise.
Herpes simplex (genital). With herpes simplex, fluid-filled vesicles appear on the cervix and, possibly, on the vulva, labia, perianal skin, vagina, or mouth. The vesicles, initially painless, may rupture and develop into extensive, shallow, painful ulcers, with redness, marked edema, and tender inguinal lymph nodes. Other findings include fever, malaise, and dysuria.
Lymphogranuloma venereum. Patients with lymphogranuloma venereum, a bacterial infection, commonly present with a single, painless papule or ulcer on the posterior vulva that heals in a few days. Painful, swollen lymph nodes, usually unilateral, develop 2 to 6 weeks later. Other findings include fever, chills, headache, anorexia, myalgias, arthralgias, weight loss, and perineal edema.
Squamous cell carcinoma. Invasive carcinoma occurs primarily in postmenopausal women and may produce vulvar pruritus, pain, and a vulvar lump. As the tumor enlarges, it may encroach on the vagina, anus, and urethra, causing bleeding, discharge, or dysuria. Carcinoma in situ is most common in premenopausal women, producing a vulvar lesion that may be white or red, raised, well defined, moist, crusted, and isolated.
Squamous cell hyperplasia. Formerly known as hyperplastic dystrophy, these vulvar lesions may be well delineated or poorly defined; localized or extensive; and red, brown, white, or both red and white. However, intense pruritus, possibly with vulvar pain, intense burning, and dyspareunia, is the cardinal symptom. With lichen sclerosis, a type of vulvar dystrophy, vulvar skin has a parchment-like appearance. Fissures may develop between the clitoris and urethra or other vulvar areas.
Syphilis. Chancres, the primary vulvar lesions of syphilis, may appear on the vulva, vagina, or cervix 10 to 90 days after initial contact. Usually painless, they start as papules that then erode, with indurated, raised edges and clear bases. Condylomata lata, highly contagious secondary vulvar lesions, are raised, gray, flat topped, and commonly ulcerated. Other findings include a maculopapular, pustular, or nodular rash; headache; malaise; anorexia; weight loss; fever; nausea; vomiting; generalized lymphadenopathy; and a sore throat.
Viral disease (systemic). Varicella, measles, and other systemic viral diseases may produce vulvar lesions.
Special Considerations
Expect to administer systemic an antibiotic, antiviral, topical corticosteroid, topical testosterone, or an antipruritic.
Patient Counseling
Explain that sitz baths may make the patient more comfortable. Provide instruction in safer sex practices.
Pediatric Pointers
Vulvar lesions in children may result from congenital syphilis or gonorrhea. Evaluate for sexual abuse.
Geriatric Pointers
Vulvar dystrophies and neoplasia increase in frequency with advancing age. All vulvar lesions must be suspected of being malignant until proven otherwise. Also, many women remain sexually active well into their older years and may come from a time when sexually transmitted diseases were not openly discussed. These patients should be questioned about sexual activities and educated about safer sex practices.
REFERENCES
Schuiling, K. D. (2013). Women’s gynecologic health. Burlington, MA: Jones & Bartlett Learning.
Sommers, M. S., & Brunner, L. S. (2012). Pocket diseases. Philadelphia, PA: F.A. Davis.

WXYZ
Weight Gain, Excessive
Weight gain occurs when ingested calories exceed body requirements for energy, causing increased adipose tissue storage. It can also occur when fluid retention causes edema. When weight gain results from overeating, emotional factors — most commonly anxiety, guilt, and depression — and social factors may be the primary causes.
Among the elderly, weight gain commonly reflects a sustained food intake in the presence of the normal, progressive fall in basal metabolic rate. Among women, a progressive weight gain occurs with pregnancy, whereas a periodic weight gain usually occurs with menstruation.
Weight gain, a primary sign of many endocrine disorders, also occurs with conditions that limit activity, especially cardiovascular and pulmonary disorders. It can also result from drug therapy that increases appetite or causes fluid retention or from cardiovascular, hepatic, and renal disorders that cause edema.
History and Physical Examination
Determine your patient’s previous patterns of weight gain and loss. Does he have a family history of obesity, thyroid disease, or diabetes mellitus? Assess his eating and activity patterns. Has his appetite increased? Does he exercise regularly or at all? Next, ask about associated symptoms. Has he experienced visual disturbances, hoarseness, paresthesia, or increased urination and thirst? Has he become impotent? If the patient is female, has she had menstrual irregularities or experienced weight gain during menstruation?
Form an impression of the patient’s mental status. Is he anxious or depressed? Does he respond slowly? Is his memory poor? What medications is he using?
During your physical examination, measure skinfold thickness to estimate fat reserves. (See Evaluating Nutritional Status, pages 756 and 757.) Note fat distribution and the presence of localized or generalized edema and overall nutritional status. Inspect for other abnormalities, such as abnormal body hair distribution or hair loss and dry skin. Take and record the patient’s vital signs.
Medical Causes
Acromegaly. Acromegaly causes moderate weight gain. Other findings include coarsened facial features, prognathism, enlarged hands and feet, increased sweating, oily skin, deep voice, back and joint pain, lethargy, sleepiness, and heat intolerance. Occasionally, hirsutism may occur.
Diabetes mellitus. The increased appetite associated with diabetes mellitus may lead to weight gain, although weight loss sometimes occurs instead. Other findings include fatigue, polydipsia, polyuria, nocturia, weakness, polyphagia, and somnolence.
Hypercortisolism. Excessive weight gain, usually over the trunk and the back of the neck (buffalo hump), characteristically occurs in this disorder. Other cushingoid features include slender extremities, moon face, weakness, purple striae, emotional lability, and increased
susceptibility to infection. Gynecomastia may occur in men; hirsutism, acne, and menstrual irregularities may occur in women.
Hyperinsulinism. Hyperinsulinism increases appetite, leading to weight gain. Emotional lability, indigestion, weakness, diaphoresis, tachycardia, visual disturbances, and syncope also occur.
Hypogonadism. Weight gain is common in hypogonadism. Prepubertal hypogonadism causes eunuchoid body proportions with relatively sparse facial and body hair and a high-pitched voice. Postpubertal hypogonadism causes loss of libido, impotence, and infertility.
Hypothalamic dysfunction. Conditions such as Laurence-Moon-Bardet-Biedl syndrome cause a voracious appetite with subsequent weight gain, along with altered body temperature and sleep rhythms.
Hypothyroidism. With hypothyroidism, weight gain occurs despite anorexia. Related signs and symptoms include fatigue; cold intolerance; constipation; menorrhagia; slowed intellectual and motor activity; dry, pale, cool skin; dry, sparse hair; and thick, brittle nails. Myalgia, hoarseness, hypoactive deep tendon reflexes, bradycardia, and abdominal distention may occur. Eventually, the face assumes a dull expression with periorbital edema.
Evaluating Nutritional Status
If your patient exhibits excessive weight loss or gain, you can help assess his nutritional status by measuring his skinfold thickness and midarm circumference and by calculating his midarm muscle circumference. Skinfold measurements reflect adipose tissue mass (subcutaneous fat accounts for about 50% of the body's adipose tissue). Midarm measurements reflect both skeletal muscle and adipose tissue mass.
Use the steps described here to gather these measurements. Then, express them as a percentage of standard by using this formula:
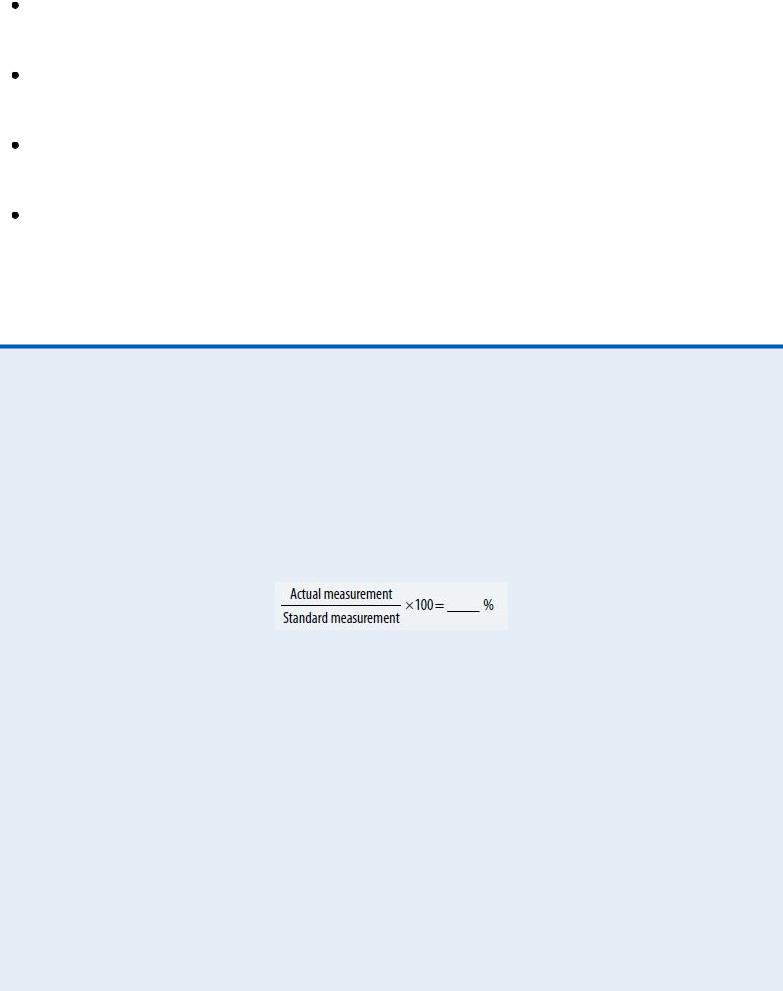
Standard anthropometric measurements vary according to the patient's age and sex and can be found in a chart of normal anthropometric values. The abridged chart below lists standard arm measurements for adult men and women.
A triceps or subscapular skinfold measurement below 60% of the standard value indicates severe depletion of fat reserves, measurement between 60% and 90% indicates moderate to mild depletion, and above 90% indicates significant fat reserves. A midarm circumference of less than 90% of the standard value indicates caloric deprivation; greater than 90% indicates adequate or ample muscle and fat. A midarm muscle circumference of less than 90% indicates protein depletion; greater than 90% indicates adequate or ample protein reserves.
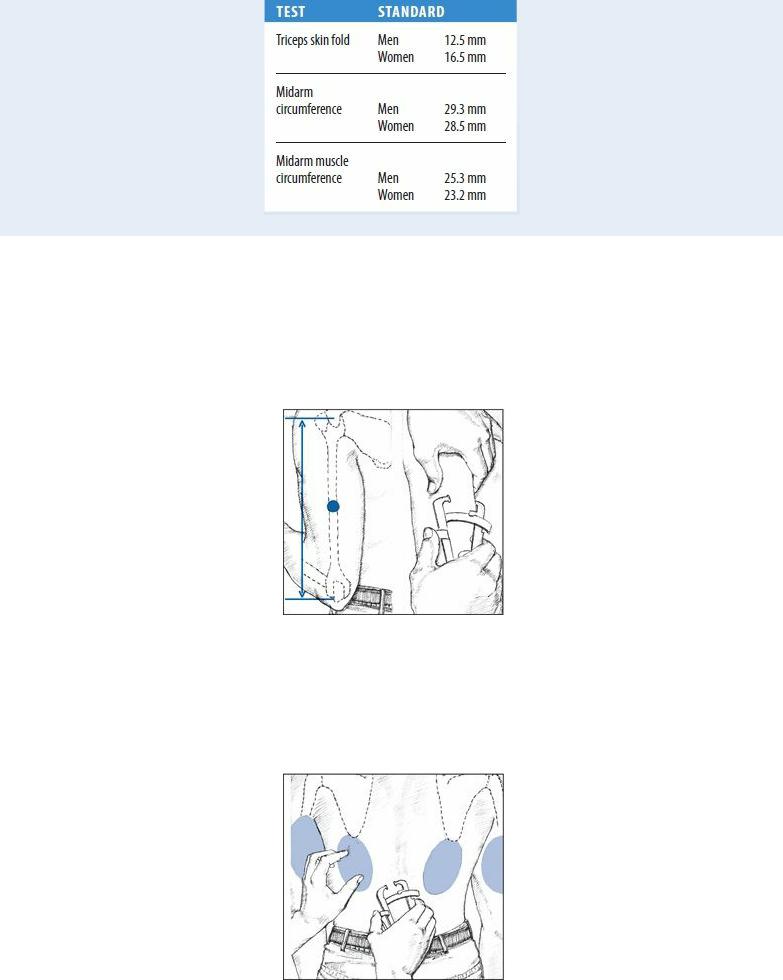
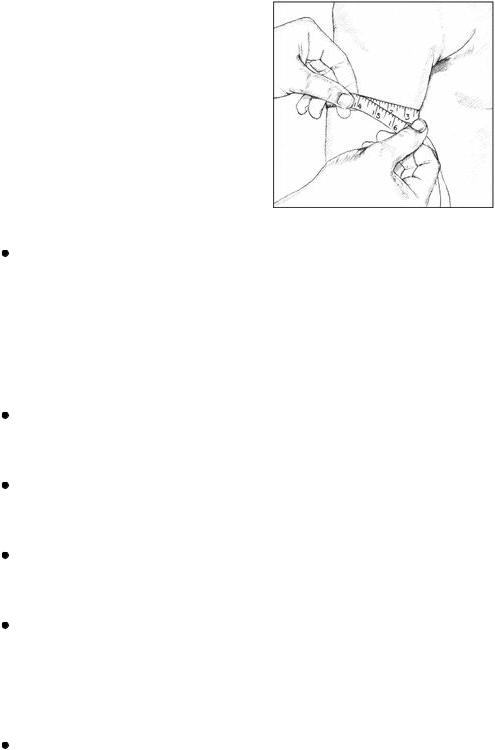
To measure the triceps skin fold, locate the midpoint of the patient's upper arm, using a nonstretch tape measure. Mark the midpoint with a felt-tip pen. Then, grasp the skin with your thumb and forefinger about 1 cm above the midpoint. Place the calipers at the midpoint, and squeeze them for about 3 seconds. Record the measurement registered on the handle gauge to the nearest 0.5 mm. Take two more readings, and average all three to compensate for any measurement error.
To measure the subscapular skin fold, use your thumb and forefinger to grasp the skin just below the angle of the scapula, in line with the natural cleavage of the skin. Apply the calipers, and proceed as you would when measuring the triceps skin fold. Both subscapular and triceps skinfold measurements are reliable measurements of fat loss or gain during hospitalization.
To measure midarm circumference, return to the midpoint you marked on the patient's upper arm.
Then, use a tape measure to determine the arm circumference at this point. This measurement reflects both skeletal muscle and adipose tissue mass and helps evaluate protein and calorie reserves. To calculate midarm muscle circumference, multiply the triceps skinfold thickness (in centimeters) by 3.143, and subtract this figure from the midarm circumference. Midarm muscle circumference reflects muscle mass alone, providing a more sensitive index of protein reserves.
Metabolic syndrome. Excessive weight gain, particularly the accumulation of fat around the midsection or a disproportionate waist-hip ratio (apple shape), is a risk factor of this disease. Other risk factors include increased blood pressure, elevated glucose and insulin levels, and abnormal cholesterol, triglyceride, and high-density lipoprotein levels. It’s estimated that more than 50 million people in the United States have metabolic syndrome. Implementing a healthier lifestyle, incorporating better eating habits, losing weight, and increasing physical activity are ways to decrease or delay the risks associated with metabolic syndrome.
Nephrotic syndrome. With nephrotic syndrome, weight gain results from edema. In severe cases, anasarca develops — increasing body weight up to 50%. Related effects include abdominal distention, orthostatic hypotension, and lethargy.
Pancreatic islet cell tumor. Pancreatic islet cell tumor causes excessive hunger, which leads to weight gain. Other findings include emotional lability, weakness, malaise, fatigue, restlessness, diaphoresis, palpitations, tachycardia, visual disturbances, and syncope.
Preeclampsia. With preeclampsia, rapid weight gain (exceeding the normal weight gain of pregnancy) may accompany nausea and vomiting, epigastric pain, elevated blood pressure, and visual blurring or double vision.
Sheehan’s syndrome. Most common in women who experience severe obstetric hemorrhage, Sheehan’s syndrome may cause weight gain.
Other Causes
Drugs. Corticosteroids, phenothiazines, and tricyclic antidepressants cause weight gain from fluid retention and increased appetite. Other drugs that can lead to weight gain include hormonal contraceptives, which cause fluid retention; cyproheptadine, which increases appetite; and lithium, which can induce hypothyroidism.
Special Considerations
Psychological counseling may be necessary for patients with weight gain, particularly when it results from emotional problems or when uneven weight distribution alters body image. If the patient is obese or has a cardiopulmonary disorder, any exercises should be monitored closely. Further study to rule out possible secondary causes should include serum thyroid-stimulating hormone determination and dexamethasone suppression testing. Laboratory test results of all patients ideally include cardiac risk factors: serum cholesterol, triglyceride, and glucose levels.
Patient Counseling
Discuss the importance of weight control, and provide guidance in appropriate exercise. Also, explain the importance of behavior modification and dietary compliance.
Pediatric Pointers
Weight gain in children can result from an endocrine disorder, such as hypercortisolism. Other causes include inactivity caused by Prader-Willi syndrome, Down syndrome, Werdnig-Hoffmann disease, late stages of muscular dystrophy, and severe cerebral palsy.
Nonpathologic causes include poor eating habits, sedentary recreation, and emotional problems, especially among adolescents. Regardless of the cause, discourage fad diets and provide a balanced weight loss program. The incidence of obesity is increasing among children.
Geriatric Pointers
Desired weights (associated with lowest mortality rates) increase with age.
REFERENCES
Buttaro, T. M., Tybulski, J., Bailey, P. P. , & Sandberg-Cook, J. (2008) . Primary care: A collaborative practice (pp. 444–447) . St. Louis, MO: Mosby Elsevier.
Colyar, M. R. (2003). Well-child assessment for primary care providers. Philadelphia, PA: F.A. Davis. Lehne, R. A. (2010). Pharmacology for nursing care (7th ed.). St. Louis, MO: Saunders Elsevier.
McCance, K. L., Huether, S. E., Brashers, V. L. , & Rote, N. S. (2010). Pathophysiology: The biologic basis for disease in adults and children. Maryland Heights, MO: Mosby Elsevier.
Schuiling, K. D. (2013). Women’s gynecologic health. Burlington, MA: Jones & Bartlett Learning. Sommers, M. S., & Brunner, L. S. (2012). Pocket diseases. Philadelphia, PA: F.A. Davis.
Weight Loss, Excessive
Weight loss can reflect decreased food intake, decreased food absorption, increased metabolic requirements, or a combination of the three. Its causes include endocrine, neoplastic, GI, and psychiatric disorders; nutritional deficiencies; infections; and neurologic lesions that cause paralysis and dysphagia. However, weight loss may accompany conditions that prevent sufficient food intake, such as painful oral lesions, ill-fitting dentures, and loss of teeth. It may be the metabolic effect of poverty, fad diets, excessive exercise, or certain drugs.
Weight loss may occur as a late sign in such chronic diseases as heart failure and renal disease. In these diseases, however, it’s the result of anorexia. (See Anorexia, pages 49 to 52.)
History and Physical Examination

Begin with a thorough diet history because weight loss almost always is caused by inadequate caloric intake. If the patient hasn’t been eating properly, try to determine why. Ask him about previous weight and if the recent loss was intentional. Be alert to lifestyle or occupational changes that may be a source of anxiety or depression. For example, has he gotten separated or divorced? Has a family member or friend died recently? Has he recently changed jobs?
Inquire about recent changes in bowel habits, such as diarrhea or bulky, floating stools. Has the patient had nausea, vomiting, or abdominal pain, which may indicate a GI disorder? Has he had excessive thirst, excessive urination, or heat intolerance, which may signal an endocrine disorder? Take a careful drug history, noting especially any use of diet pills and laxatives.
Carefully check the patient’s height and weight, and ask about his previous weight. Take his vital signs, and note his general appearance: Is he well nourished? Do his clothes fit? Is muscle wasting evident? Ask about exact weight changes (with approximate dates).
Next, examine the patient’s skin for turgor and abnormal pigmentation, especially around the joints. Does he have pallor or jaundice? Examine his mouth, including the condition of his teeth or dentures. Look for signs of infection or irritation on the roof of the mouth, and note any hyperpigmentation of the buccal mucosa. Also, check the patient’s eyes for exophthalmos and his neck for swelling; evaluate his lungs for adventitious sounds. Inspect his abdomen for signs of wasting, and palpate for masses, tenderness, and an enlarged liver.
Conventional laboratory and radiologic investigations such as complete blood count, serum albumin levels, urinalysis, chest X-ray, and upper GI series usually reveal the cause. Almost all physical causes are clinically evident during the initial evaluation. Cancer, GI disorders, and depression are the most common pathologic causes.
Medical Causes
Adrenal insufficiency. Weight loss occurs with adrenal insufficiency, along with anorexia, weakness, fatigue, irritability, syncope, nausea, vomiting, abdominal pain, and diarrhea or constipation. Hyperpigmentation may occur at the joints, belt line, palmar creases, lips, gums, tongue, and buccal mucosa.
Anorexia nervosa. Anorexia nervosa is a psychogenic disorder, most common in young women, and is characterized by a severe, self-imposed weight loss ranging from 10% to 50% of premorbid weight, which typically was normal or not more than 5 lb (2.3 kg) over ideal weight. Related findings include skeletal muscle atrophy, loss of fatty tissue, hypotension, constipation, dental caries, susceptibility to infection, blotchy or sallow skin, cold intolerance, hairiness on the face and body, dryness or loss of scalp hair, and amenorrhea. The patient usually demonstrates restless activity and vigor and may also have a morbid fear of becoming fat. Selfinduced vomiting or use of laxatives or diuretics may lead to dehydration or to metabolic alkalosis or acidosis.
Cancer. Weight loss is often a sign of cancer. Other findings reflect the type, location, and stage of the tumor and can include fatigue, pain, nausea, vomiting, anorexia, abnormal bleeding, and a palpable mass.
Crohn’s disease. Weight loss occurs with chronic cramping, abdominal pain, and anorexia. Other signs and symptoms include diarrhea, nausea, fever, tachycardia, abdominal tenderness and guarding, hyperactive bowel sounds, abdominal distention, and pain. Perianal lesions and a palpable mass in the right or left lower quadrant may also be present.
