
- •Overview
- •Preface
- •Translator’s Note
- •Contents
- •1. Fundamentals
- •Microscopic Anatomy of the Nervous System
- •Elements of Neurophysiology
- •Elements of Neurogenetics
- •General Genetics
- •Neurogenetics
- •Genetic Counseling
- •2. The Clinical Interview in Neurology
- •General Principles of History Taking
- •Special Aspects of History Taking
- •3. The Neurological Examination
- •Basic Principles of the Neurological Examination
- •Stance and Gait
- •Examination of the Head and Cranial Nerves
- •Head and Cervical Spine
- •Cranial Nerves
- •Examination of the Upper Limbs
- •Motor Function and Coordination
- •Muscle Tone and Strength
- •Reflexes
- •Sensation
- •Examination of the Trunk
- •Examination of the Lower Limbs
- •Coordination and Strength
- •Reflexes
- •Sensation
- •Examination of the Autonomic Nervous System
- •Neurologically Relevant Aspects of the General Physical Examination
- •Neuropsychological and Psychiatric Examination
- •Psychopathological Findings
- •Neuropsychological Examination
- •Special Considerations in the Neurological Examination of Infants and Young Children
- •Reflexes
- •4. Ancillary Tests in Neurology
- •Fundamentals
- •Imaging Studies
- •Conventional Skeletal Radiographs
- •Computed Tomography (CT)
- •Magnetic Resonance Imaging (MRI)
- •Angiography with Radiological Contrast Media
- •Myelography and Radiculography
- •Electrophysiological Studies
- •Fundamentals
- •Electroencephalography (EEG)
- •Evoked potentials
- •Electromyography
- •Electroneurography
- •Other Electrophysiological Studies
- •Ultrasonography
- •Other Ancillary Studies
- •Cerebrospinal Fluid Studies
- •Tissue Biopsies
- •Perimetry
- •5. Topical Diagnosis and Differential Diagnosis of Neurological Syndromes
- •Fundamentals
- •Muscle Weakness and Other Motor Disturbances
- •Sensory Disturbances
- •Anatomical Substrate of Sensation
- •Disturbances of Consciousness
- •Dysfunction of Specific Areas of the Brain
- •Thalamic Syndromes
- •Brainstem Syndromes
- •Cerebellar Syndromes
- •6. Diseases of the Brain and Meninges
- •Congenital and Perinatally Acquired Diseases of the Brain
- •Fundamentals
- •Special Clinical Forms
- •Traumatic Brain injury
- •Fundamentals
- •Traumatic Hematomas
- •Complications of Traumatic Brain Injury
- •Intracranial Pressure and Brain Tumors
- •Intracranial Pressure
- •Brain Tumors
- •Cerebral Ischemia
- •Nontraumatic Intracranial Hemorrhage
- •Infectious Diseases of the Brain and Meninges
- •Infections Mainly Involving the Meninges
- •Infections Mainly Involving the Brain
- •Intracranial Abscesses
- •Congenital Metabolic Disorders
- •Acquired Metabolic Disorders
- •Diseases of the Basal Ganglia
- •Fundamentals
- •Diseases Causing Hyperkinesia
- •Other Types of Involuntary Movement
- •Cerebellar Diseases
- •Dementing Diseases
- •The Dementia Syndrome
- •Vascular Dementia
- •7. Diseases of the Spinal Cord
- •Anatomical Fundamentals
- •The Main Spinal Cord Syndromes and Their Anatomical Localization
- •Spinal Cord Trauma
- •Spinal Cord Compression
- •Spinal Cord Tumors
- •Myelopathy Due to Cervical Spondylosis
- •Circulatory Disorders of the Spinal Cord
- •Blood Supply of the Spinal Cord
- •Arterial Hypoperfusion
- •Impaired Venous Drainage
- •Infectious and Inflammatory Diseases of the Spinal Cord
- •Syringomyelia and Syringobulbia
- •Diseases Mainly Affecting the Long Tracts of the Spinal Cord
- •Diseases of the Anterior Horns
- •8. Multiple Sclerosis and Other Myelinopathies
- •Fundamentals
- •Myelin
- •Multiple Sclerosis
- •Other Demyelinating Diseases of Unknown Pathogenesis
- •9. Epilepsy and Its Differential Diagnosis
- •Types of Epilepsy
- •Classification of the Epilepsies
- •Generalized Seizures
- •Partial (Focal) Seizures
- •Status Epilepticus
- •Episodic Neurological Disturbances of Nonepileptic Origin
- •Episodic Disturbances with Transient Loss of Consciousness and Falling
- •Episodic Loss of Consciousness without Falling
- •Episodic Movement Disorders without Loss of Consciousness
- •10. Polyradiculopathy and Polyneuropathy
- •Fundamentals
- •Polyradiculitis
- •Cranial Polyradiculitis
- •Polyradiculitis of the Cauda Equina
- •Polyneuropathy
- •Fundamentals
- •11. Diseases of the Cranial Nerves
- •Fundamentals
- •Disturbances of Smell (Olfactory Nerve)
- •Neurological Disturbances of Vision (Optic Nerve)
- •Visual Field Defects
- •Impairment of Visual Acuity
- •Pathological Findings of the Optic Disc
- •Disturbances of Ocular and Pupillary Motility
- •Fundamentals of Eye Movements
- •Oculomotor Disturbances
- •Supranuclear Oculomotor Disturbances
- •Lesions of the Nerves to the Eye Muscles and Their Brainstem Nuclei
- •Ptosis
- •Pupillary Disturbances
- •Lesions of the Trigeminal Nerve
- •Lesions of the Facial Nerve
- •Disturbances of Hearing and Balance; Vertigo
- •Neurological Disturbances of Hearing
- •Disequilibrium and Vertigo
- •The Lower Cranial Nerves
- •Accessory Nerve Palsy
- •Hypoglossal Nerve Palsy
- •Multiple Cranial Nerve Deficits
- •12. Diseases of the Spinal Nerve Roots and Peripheral Nerves
- •Fundamentals
- •Spinal Radicular Syndromes
- •Peripheral Nerve Lesions
- •Fundamentals
- •Diseases of the Brachial Plexus
- •Diseases of the Nerves of the Trunk
- •13. Painful Syndromes
- •Fundamentals
- •Painful Syndromes of the Head And Neck
- •IHS Classification of Headache
- •Approach to the Patient with Headache
- •Migraine
- •Cluster Headache
- •Tension-type Headache
- •Rare Varieties of Primary headache
- •Symptomatic Headache
- •Painful Syndromes of the Face
- •Dangerous Types of Headache
- •“Genuine” Neuralgias in the Face
- •Painful Shoulder−Arm Syndromes (SAS)
- •Neurogenic Arm Pain
- •Vasogenic Arm Pain
- •“Arm Pain of Overuse”
- •Other Types of Arm Pain
- •Pain in the Trunk and Back
- •Thoracic and Abdominal Wall Pain
- •Back Pain
- •Groin Pain
- •Leg Pain
- •Pseudoradicular Pain
- •14. Diseases of Muscle (Myopathies)
- •Structure and Function of Muscle
- •General Symptomatology, Evaluation, and Classification of Muscle Diseases
- •Muscular Dystrophies
- •Autosomal Muscular Dystrophies
- •Myotonic Syndromes and Periodic Paralysis Syndromes
- •Rarer Types of Muscular Dystrophy
- •Diseases Mainly Causing Myotonia
- •Metabolic Myopathies
- •Acute Rhabdomyolysis
- •Mitochondrial Encephalomyopathies
- •Myositis
- •Other Diseases Affecting Muscle
- •Myopathies Due to Systemic Disease
- •Congenital Myopathies
- •Disturbances of Neuromuscular Transmission−Myasthenic Syndromes
- •15. Diseases of the Autonomic Nervous System
- •Anatomy
- •Normal and Pathological Function of the Autonomic Nervous System
- •Sweating
- •Bladder, Bowel, and Sexual Function
- •Generalized Autonomic Dysfunction
- •Index
252 13 Painful Syndromes
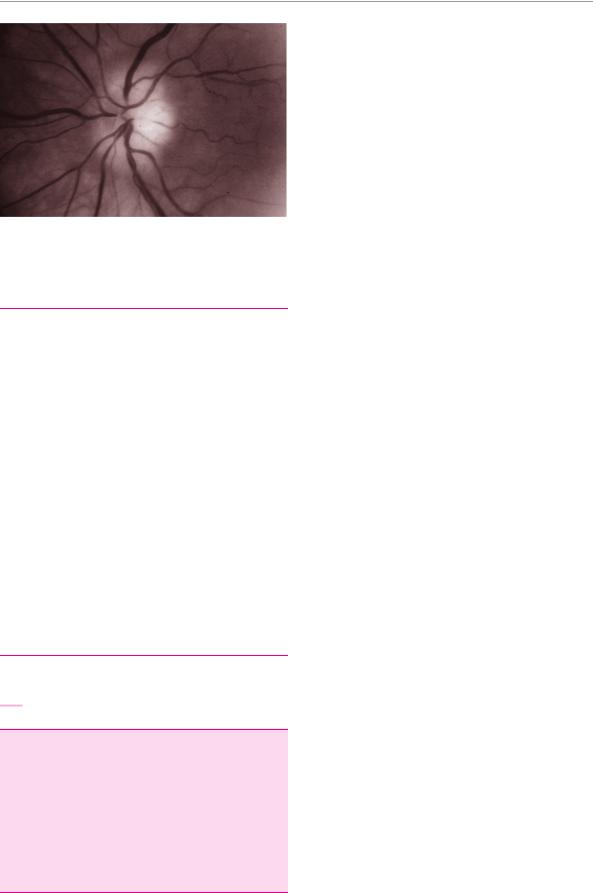
Fig. 13.6 Atrophic optic disc in a 79-year-old woman with temporal arteritis. Note the abnormal disc pallor; the patient is blind in this eye.
Table 13.8 Diagnostic criteria for spondylogenic headache
Characteristics of pain
radiating from occipital to frontal
usually unilateral
coming in attacks, or
permanent pain of variable intensity
not throbbing
moderately severe
Cervical spine
prior history of trauma to the head or cervical spine
or prior whiplash injury
or episodes of torticollis (wry neck),
perhaps accompanied by arm pain
clinical or radiological evidence of cervical spine pathology
Precipitating and alleviating factors
pain induced by movement (or manipulation) of the cervical spine
or by keeping the head in a particular position for a longer than usual time
or by local pressure on the nape of the neck or the occiput
pain temporarily alleviated by infiltration of the greater occipital n. or the C2 nerve root with local anaesthetic
Accompanying symptoms
dizziness
nausea
blurred vision
phonoand photophobia
dysphagia
Diagnostic evaluation. The erythrocyte sedimentation rate is nearly always markedly elevated. The diagnosis is confirmed by temporal artery biopsy: histopathological examination reveals giant cell arteritis. A biopsy should be performed in all suspected cases, because there is no other way to establish the diagnosis with the certainty required before starting long-term treatment with corticosteroids. These often need to be given continuously for a year or more.
Spondylogenic Headache (“Migraine Cervicale”)
Our experience suggests that this condition is overdiagnosed. The appropriate diagnostic criteria to be used are summarized in Table 13.8.
Dangerous Types of Headache
All patients who consult a physician because of headache are in pain and therefore deserve our full attention and respect. More than 90 % of them, however, will turn out not to have a serious medical problem. One of the important tasks facing the physician is to be on guard for those few, unusual cases of headache that are, in fact, due to a dangerous underlying condition. The main alarm signals are the following:
headache of an unusual nature in a patient who never had headaches before;
headache arising at an advanced age;
headache of sudden (lightning-like) onset;
headache that always occurs in precisely the same location (except cluster headache or trigeminal neuralgia, both of which, by definition, always occur in the same place);
progressively severe headache (crescendo headache);
continuous headache;
headache accompanied by:
personality change,
impairment of consciousness,
epileptic seizures;
neurological deficits revealed on physical examination.
If any of the above applies, further investigation is needed, usually with an imaging study.
Painful Syndromes of the Face
Facial pain is often due to a lesion of a sensory nerve in the face, most commonly the trigeminal n. It typically presents with very brief, but very intense attacks of pain (“classic” or “genuine” neuralgia in the face). There are also a variety of other kinds of facial pain with other pathogenetic mechanisms, e. g., a structural anomaly of the jaw. The pain may resemble neuralgia in these other conditions as well; thus, patients with any kind of facial pain always require careful evaluation to establish the differential diagnosis.
“Genuine” Neuralgias in the Face
Typical manifestations of “genuine” neuralgia in the face are the following:
pain is located in the face or the mucous membranes of the head,
usually comes in brief attacks lasting a few seconds to a few minutes at most,
is usually very intense;
is described as electrical, knifelike, cutting, stabbing, or lightninglike;
arises either spontaneously or on provocation by touch or other mechanical or thermal stimuli;
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme All rights reserved. Usage subject to terms and conditions of license.
Painful Syndromes of the Face 253
is always on the same side of the face (in most patients);
and is always in the same location.
In addition, the attacks are very frequent, up to several times a day,
with no pain in between attacks, except, possibly, for
a dull background pain. |
|
|
|
Finally, there are no objective neurological abnor- |
4 |
5 |
|
malities, except in the rare forms of symptomatic |
|||
|
|
||
neuralgia. |
|
3 |
|
|
1 |
||
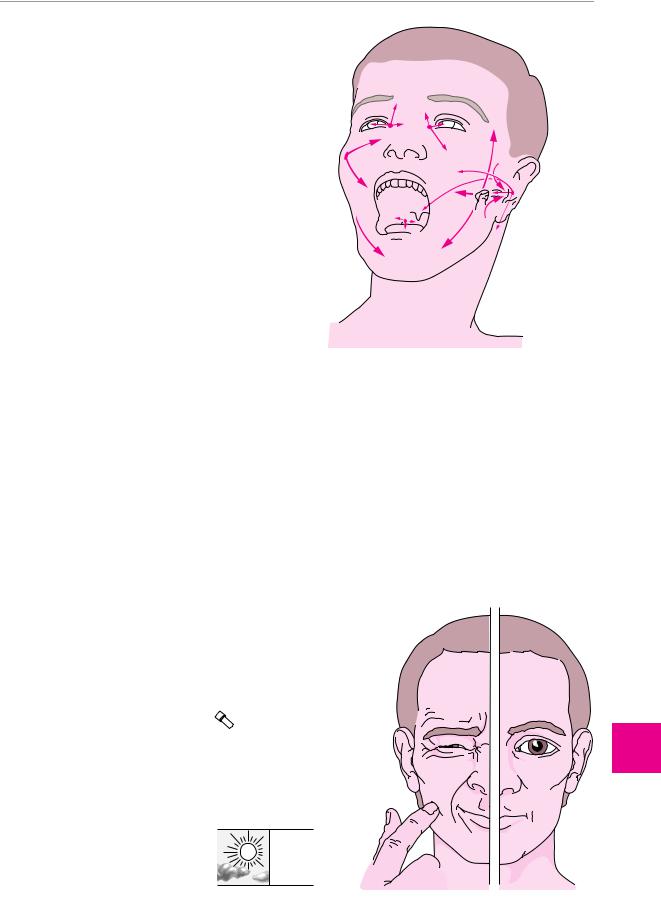
The most common “genuine” neuralgias in the face are |
|
||
|
|
||
described in the following paragraphs. The localization |
|
7 |
|
and radiation of pain in the various types of neuralgia |
|
8 |
|
are depicted in Fig. 13.7. |
2 |
6 |
|
3 |
|||
|
|
Trigeminal Neuralgia |
|
|
Idiopathic trigeminal neuralgia, which is far more com- |
|
|
mon than the symptomatic type, only affects individu- |
|
|
als over age 50. |
|
|
Pathogenesis. Idiopathic trigeminal neuralgia appears |
|
|
to have more than one possible cause. In many patients, |
|
|
neuroimaging studies reveal a looping blood vessel that |
Fig. 13.7 Localization of various types of facial pain and neural- |
|
makes contact with the trigeminal n. at its zone of entry |
||
gia. 1 Trigeminal neuralgia in the distribution of the maxillary nerve |
||
into the pons. In other patients, defective myelin sheaths |
(V2). 2 Trigeminal neuralgia in the distribution of the mandibular |
|
are found in the Gasserian ganglion (naturally only at |
nerve (V3). 3 Auriculotemporal neuralgia. 4 Nasociliary neuralgia. |
|
postmortem examination). In symptomatic trigeminal |
5 Sluder’s neuralgia. 6 Glossopharyngeal neuralgia. 7 Neuralgia of |
|
neuralgia, on the other hand, the pain is due to an under- |
the geniculate ganglion. 8 Temporomandibular joint “neuralgia” |
|
lying neurological disease, e. g., multiple sclerosis. |
(myofacial pain syndrome). |
|
|
||
Clinical manifestations. The painful attacks of id- |
usual sense of a primary movement disorder). The pain |
|
iopathic trigeminal neuralgia are usually located in the |
is unbearably intense. The attacks occur spontaneously |
|
distribution of the second trigeminal division (the maxil- |
or on provocation by eating, speaking, tooth brushing, |
|
lary n.), less commonly in that of the first or third divi- |
or touch; they may come dozens of times per day. Some |
|
sions. The pain is nearly always unilateral; it is felt on |
patients eat and speak so little to avoid the pain that |
|
both sides simultaneously, or in alternation, in only 3 % |
they lose weight, even to the point of cachexia. Attacks |
|
of patients. The individual attacks last only a few sec- |
generally do not occur during sleep. The typical clinical |
|
onds and cause a reflexive grimace or pulling of the face |
manifestations of trigeminal neuralgia are depicted in |
|
(“tic douloureux,” not to be confused with a tic in the |
Fig. 13.8. Sometimes, a long period with frequent attacks |
Fig. 13.8 Trigeminal neuralgia: schematic diagram.
duration of pain: 5–10 seconds
maximum in 1 second 
up to 100 times per day
ThiemeARgoOneBoldThiemeArgoOne
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme
All rights reserved. Usage subject to terms and conditions of license.
Painful Syndromes
13
254 13 Painful Syndromes
is followed by a pain-free interval that may last for |
side the nostril. This condition is sometimes difficult to |
|
months until the attacks return. |
distinguish from cluster headache (p. 248). On rare oc- |
|
In the rarer symptomatic cases of trigeminal neural- |
casions, it is also confused with dissection of the inter- |
|
gia, the clinical manifestations are slightly different. The |
nal carotid a., which produces a similar type of pain. |
|
attacks are more commonly bilateral (either simul- |
|
|
taneously or in alternation) and a neurological deficit |
Sluder Neuralgia |
|
may be found, depending on the underlying etiology, |
||
This condition is thought to be due to a pathological |
||
e. g., multiple sclerosis or a tumor compressing the |
||
trigeminal n. |
process affecting the pterygopalatine ganglion. Its clini- |
|
Diagnostic evaluation. As stated above, the neurologi- |
cal manifestations closely resemble those of nasociliary |
|
neuralgia (see above). In many patients, the attacks are |
||
cal examination generally reveals no abnormality. |
accompanied by the urge to sneeze. Sluder neuralgia is |
|
About one-quarter of patients who have suffered from |
occasionally associated with sphenoid or ethmoid |
|
idiopathic trigeminal neuralgia for a long time have a |
sinusitis. |
|
mild sensory deficit in the affected area of the face. |
|
Treatment. About 80 % of patients initially respond to correctly dosed treatment with carbamazepine or gabapentin. The medication must be taken every day and the dose must be steadily increased until the pain is relieved.
!The pharmacological treatment of trigeminal neuralgia often fails because of underdosing or irregular consumption of the prescribed drug.
If pharmacological treatment does not eliminate the pain despite a high dose of medication (in some patients, just below the threshold for intolerable side effects, which varies greatly from one patient to the next), neurosurgical treatment is indicated. The available, effective procedures include open microvascular decompression of the trigeminal n. (requires craniotomy) and percutaneous techniques such as selective radiofrequency coagulation of the Gasserian ganglion, balloon compression of the ganglion, and glycerol injection into Meckel’s cave.
Auriculotemporal Neuralgia
In this disorder, the pain is located in the temple and in front of the ear. It is usually a sequela of disease of the ipsilateral parotid gland, appearing a few days or months after the parotid condition resolves.
The attacks of pain can be provoked by chewing or by chemical stimuli, particularly sour (acidic) food. The pain is of a burning quality. It is often accompanied by erythema and increased sweating in the preauricular area.
The differential diagnosis of this condition includes temporomandibular joint syndrome.
Nasociliary Neuralgia
The attacks of pain are located in the nose and on the inner canthus of the eye. There may be a continuous, background pain in addition to the typical, lightninglike, shooting pain. In this condition, as in the other neuralgias of the face, the pain is provoked by chewing or by touch—here, by touching the eye. The attacks are often accompanied by redness of the eye, swelling of the nasal mucosa, and lacrimation. They can often be aborted by the application of a 5 % cocaine solution in-
Glossopharyngeal Neuralgia
This condition is usually seen in the elderly. Its typical manifestations are lightninglike pain in the base of the tongue, the hypopharynx, and the tonsillar fossa, radiating toward the ear. The pain can be provoked by swallowing (especially of cold liquids), speaking, or sticking out the tongue. The painful attacks are, on rare occasions, accompanied by syncope. The pharmacological treatment of this disorder is like that of trigeminal neuralgia. If surgical treatment is required, resection of the glossopharyngeal n. and the upper root of the vagus n. has a good chance of success.
Rarer Types of Neuralgia
The neuralgias of the geniculate ganglion, the superior laryngeal n., and the auricular branch of the vagus n. are all very rare. The existence of occipital neuralgia is still debated.
Other Diseases Causing
Facial Pain
Temporomandibular Joint Syndrome
This condition has many other names, including myofacial syndrome and Costen syndrome. Our experience suggests that it is overdiagnosed.
Pathogenesis. This condition is thought to be due to abnormal mechanical stress on the jaw joint caused by malocclusion, e. g., after tooth extraction, or by local changes in the joint itself. This, in turn, causes the muscles of mastication to be activated in nonphysiological ways, which leads to pain in the muscles, so that their pattern of activation is distorted even further. A vicious circle arises in which pain produces more pain.
Clinical manifestations. Patients typically suffer from more or less continuous preauricular pain, which is described as dull or neuralgia-like. The pain can be brought on, or made worse, by chewing.
Diagnostic evaluation. The jaw joint is tender to pressure on one or both sides. CT or MRI occasionally demonstrates an abnormality of the joint.
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme All rights reserved. Usage subject to terms and conditions of license.

|
Painful Syndromes of the Face 255 |
||
|
|
|
|
Treatment. Optimization of the dental occlusion (bite) |
patient. Atypical facial pain is difficult to treat; perhaps |
||
sometimes relieves the pain to some extent. Unfor- |
the most important aspect of treatment is the avoidance |
||
tunately, however, many dental and surgical procedures |
of further surgery. Serotonin reuptake inhibitors, |
||
on the teeth and jaws are performed for this condition |
flunarizine, or tricyclic antidepressants have been used |
||
to no avail. |
for this condition. |
||
|
Glossodynia is a rare type of atypical facial pain con- |
||
Atypical Facial Pain |
sisting of dysesthesia of the tongue, often of a burning |
||
character. It usually affects elderly women. |
|||
This term refers to unilateral, diffuse pain in the face. The |
|||
|
|
||
pain is often of a burning or dull character and is mad- |
General Differential Diagnosis of Head- |
||
deningly persistent. The condition generally affects |
|||
middle-aged women. It may be of spontaneous onset, |
ache and Facial Pain |
||
but, in many patients, the pain first appears (or becomes |
|
|
|
severe) in the aftermath of a dental procedure. This |
The location and clinical course of headache and facial |
||
often leads to a series of further dental procedures, |
|||
pain often provide important clues to its etiology. Im- |
|||
which the dentist or oral surgeon characteristically per- |
|||
portant aspects of differential diagnosis are sum- |
|||
forms only after being urgently entreated to do so by the |
|||
marized in Table 13.9. |
|||
|
|||
Table 13.9 Differential diagnosis of headache and facial pain
Clinical features |
Syndrome |
|
|
|
|
Recurrent attacks of intense headache with pain-free intervals |
migraine (unilateral headache) |
|
|
|
cluster headache (unilateral pain in the temporal region, eye, |
|
|
and face) |
|
hypertensive crises (diffuse pain) |
|
Recurrent attacks of intense facial pain with pain-free intervals |
trigeminal neuralgia (duration, seconds; localization, usually |
|
|
|
mid-face) |
|
auriculotemporal neuralgia (duration, minutes ; localization, |
|
|
|
preauricular) |
|
nasociliary neuralgia (duration, minutes to hours; localization, |
|
|
|
inner canthus) |
|
Sluder neuralgia (duration, minutes; localization, inner can- |
|
|
|
thus) |
|
glossopharyngeal neuralgia (duration, seconds; localization, |
|
|
|
base of tongue and tonsillar fossa) |
|
geniculate ganglion neuralgia (duration, seconds; localization, |
|
|
|
external auditory canal and palatal roof) |
Continuous facial pain |
atypical facial pain (diffuse, usually unilateral pain) |
|
|
|
temporomandibular joint (TMJ) syndrome (preauricular) |
Intense headache of sudden onset, which then persists |
subarachnoid hemorrhage |
|
|
|
intracerebral hemorrhage |
Diffuse, usually intense headache of subacute onset, which then |
meningitis, encephalitis (accompanied by meningism) |
|
persists |
|
|
Headache on standing or sitting that improves when the patient |
intracranial hypotension |
|
lies down |
|
|
Chronic, or chronically relapsing, diffuse headache of insidious |
tension-type headache |
|
onset and mild to moderate severity |
|
headache due to hypertension |
|
|
headache due to intracranial mass |
|
|
posttraumatic headache |
|
|
headache due to systemic illness (particularly febrile illness); |
|
|
toxic/iatrogenic headache; psychogenic or depressive head- |
|
|
ache |
Chronic, localized headache and facial pain |
spondylogenic headache (pain mainly in the back of the |
|
|
|
head) |
|
cranial (temporal) arteritis (pain mainly temporal) |
|
|
|
eye diseases (pain mainly frontal) |
|
|
ENT diseases (esp. sinusitis, pain mainly frontal, worse on for- |
|
|
ward bending of the head) |
|
odontogenic headache (jaw and temporal region) |
|
|
|
|
Painful Syndromes
13
ThiemeARgoOneBoldThiemeArgoOne
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme All rights reserved. Usage subject to terms and conditions of license.
