
- •Overview
- •Preface
- •Translator’s Note
- •Contents
- •1. Fundamentals
- •Microscopic Anatomy of the Nervous System
- •Elements of Neurophysiology
- •Elements of Neurogenetics
- •General Genetics
- •Neurogenetics
- •Genetic Counseling
- •2. The Clinical Interview in Neurology
- •General Principles of History Taking
- •Special Aspects of History Taking
- •3. The Neurological Examination
- •Basic Principles of the Neurological Examination
- •Stance and Gait
- •Examination of the Head and Cranial Nerves
- •Head and Cervical Spine
- •Cranial Nerves
- •Examination of the Upper Limbs
- •Motor Function and Coordination
- •Muscle Tone and Strength
- •Reflexes
- •Sensation
- •Examination of the Trunk
- •Examination of the Lower Limbs
- •Coordination and Strength
- •Reflexes
- •Sensation
- •Examination of the Autonomic Nervous System
- •Neurologically Relevant Aspects of the General Physical Examination
- •Neuropsychological and Psychiatric Examination
- •Psychopathological Findings
- •Neuropsychological Examination
- •Special Considerations in the Neurological Examination of Infants and Young Children
- •Reflexes
- •4. Ancillary Tests in Neurology
- •Fundamentals
- •Imaging Studies
- •Conventional Skeletal Radiographs
- •Computed Tomography (CT)
- •Magnetic Resonance Imaging (MRI)
- •Angiography with Radiological Contrast Media
- •Myelography and Radiculography
- •Electrophysiological Studies
- •Fundamentals
- •Electroencephalography (EEG)
- •Evoked potentials
- •Electromyography
- •Electroneurography
- •Other Electrophysiological Studies
- •Ultrasonography
- •Other Ancillary Studies
- •Cerebrospinal Fluid Studies
- •Tissue Biopsies
- •Perimetry
- •5. Topical Diagnosis and Differential Diagnosis of Neurological Syndromes
- •Fundamentals
- •Muscle Weakness and Other Motor Disturbances
- •Sensory Disturbances
- •Anatomical Substrate of Sensation
- •Disturbances of Consciousness
- •Dysfunction of Specific Areas of the Brain
- •Thalamic Syndromes
- •Brainstem Syndromes
- •Cerebellar Syndromes
- •6. Diseases of the Brain and Meninges
- •Congenital and Perinatally Acquired Diseases of the Brain
- •Fundamentals
- •Special Clinical Forms
- •Traumatic Brain injury
- •Fundamentals
- •Traumatic Hematomas
- •Complications of Traumatic Brain Injury
- •Intracranial Pressure and Brain Tumors
- •Intracranial Pressure
- •Brain Tumors
- •Cerebral Ischemia
- •Nontraumatic Intracranial Hemorrhage
- •Infectious Diseases of the Brain and Meninges
- •Infections Mainly Involving the Meninges
- •Infections Mainly Involving the Brain
- •Intracranial Abscesses
- •Congenital Metabolic Disorders
- •Acquired Metabolic Disorders
- •Diseases of the Basal Ganglia
- •Fundamentals
- •Diseases Causing Hyperkinesia
- •Other Types of Involuntary Movement
- •Cerebellar Diseases
- •Dementing Diseases
- •The Dementia Syndrome
- •Vascular Dementia
- •7. Diseases of the Spinal Cord
- •Anatomical Fundamentals
- •The Main Spinal Cord Syndromes and Their Anatomical Localization
- •Spinal Cord Trauma
- •Spinal Cord Compression
- •Spinal Cord Tumors
- •Myelopathy Due to Cervical Spondylosis
- •Circulatory Disorders of the Spinal Cord
- •Blood Supply of the Spinal Cord
- •Arterial Hypoperfusion
- •Impaired Venous Drainage
- •Infectious and Inflammatory Diseases of the Spinal Cord
- •Syringomyelia and Syringobulbia
- •Diseases Mainly Affecting the Long Tracts of the Spinal Cord
- •Diseases of the Anterior Horns
- •8. Multiple Sclerosis and Other Myelinopathies
- •Fundamentals
- •Myelin
- •Multiple Sclerosis
- •Other Demyelinating Diseases of Unknown Pathogenesis
- •9. Epilepsy and Its Differential Diagnosis
- •Types of Epilepsy
- •Classification of the Epilepsies
- •Generalized Seizures
- •Partial (Focal) Seizures
- •Status Epilepticus
- •Episodic Neurological Disturbances of Nonepileptic Origin
- •Episodic Disturbances with Transient Loss of Consciousness and Falling
- •Episodic Loss of Consciousness without Falling
- •Episodic Movement Disorders without Loss of Consciousness
- •10. Polyradiculopathy and Polyneuropathy
- •Fundamentals
- •Polyradiculitis
- •Cranial Polyradiculitis
- •Polyradiculitis of the Cauda Equina
- •Polyneuropathy
- •Fundamentals
- •11. Diseases of the Cranial Nerves
- •Fundamentals
- •Disturbances of Smell (Olfactory Nerve)
- •Neurological Disturbances of Vision (Optic Nerve)
- •Visual Field Defects
- •Impairment of Visual Acuity
- •Pathological Findings of the Optic Disc
- •Disturbances of Ocular and Pupillary Motility
- •Fundamentals of Eye Movements
- •Oculomotor Disturbances
- •Supranuclear Oculomotor Disturbances
- •Lesions of the Nerves to the Eye Muscles and Their Brainstem Nuclei
- •Ptosis
- •Pupillary Disturbances
- •Lesions of the Trigeminal Nerve
- •Lesions of the Facial Nerve
- •Disturbances of Hearing and Balance; Vertigo
- •Neurological Disturbances of Hearing
- •Disequilibrium and Vertigo
- •The Lower Cranial Nerves
- •Accessory Nerve Palsy
- •Hypoglossal Nerve Palsy
- •Multiple Cranial Nerve Deficits
- •12. Diseases of the Spinal Nerve Roots and Peripheral Nerves
- •Fundamentals
- •Spinal Radicular Syndromes
- •Peripheral Nerve Lesions
- •Fundamentals
- •Diseases of the Brachial Plexus
- •Diseases of the Nerves of the Trunk
- •13. Painful Syndromes
- •Fundamentals
- •Painful Syndromes of the Head And Neck
- •IHS Classification of Headache
- •Approach to the Patient with Headache
- •Migraine
- •Cluster Headache
- •Tension-type Headache
- •Rare Varieties of Primary headache
- •Symptomatic Headache
- •Painful Syndromes of the Face
- •Dangerous Types of Headache
- •“Genuine” Neuralgias in the Face
- •Painful Shoulder−Arm Syndromes (SAS)
- •Neurogenic Arm Pain
- •Vasogenic Arm Pain
- •“Arm Pain of Overuse”
- •Other Types of Arm Pain
- •Pain in the Trunk and Back
- •Thoracic and Abdominal Wall Pain
- •Back Pain
- •Groin Pain
- •Leg Pain
- •Pseudoradicular Pain
- •14. Diseases of Muscle (Myopathies)
- •Structure and Function of Muscle
- •General Symptomatology, Evaluation, and Classification of Muscle Diseases
- •Muscular Dystrophies
- •Autosomal Muscular Dystrophies
- •Myotonic Syndromes and Periodic Paralysis Syndromes
- •Rarer Types of Muscular Dystrophy
- •Diseases Mainly Causing Myotonia
- •Metabolic Myopathies
- •Acute Rhabdomyolysis
- •Mitochondrial Encephalomyopathies
- •Myositis
- •Other Diseases Affecting Muscle
- •Myopathies Due to Systemic Disease
- •Congenital Myopathies
- •Disturbances of Neuromuscular Transmission−Myasthenic Syndromes
- •15. Diseases of the Autonomic Nervous System
- •Anatomy
- •Normal and Pathological Function of the Autonomic Nervous System
- •Sweating
- •Bladder, Bowel, and Sexual Function
- •Generalized Autonomic Dysfunction
- •Index
204 11 |
Diseases of the Cranial Nerves |
|
|
|
|
|
|
|
|
Pathological processes affecting the central motor |
Another frequent occurrence is psychogenic vertigo, |
|
|
structures (e. g., paralysis, cerebellar or extrapy- |
particularly due to phobias, in the setting of depres- |
|
|
ramidal disease, brainstem disorders) impair the |
sion, neurotic conflict situations, and panic attacks. |
|
|
patient’s motor adaptation to changes in position, or |
Finally, any general medical conditions that can tem- |
|
|
cause oculomotor disturbances that can give rise to |
porarily diminish blood flow to the brain must be in- |
|
|
“dizziness.” |
cluded in the differential diagnosis of “dizziness” and |
|
Partial impairment of consciousness, e. g., in presyn- |
vertigo, e. g., arterial hypotension and heart disease. |
|
cope or certain types of epilepsy (particularly temporal lobe epilepsy and absence seizures), is often experienced by the patient as “dizziness.”
The Lower Cranial Nerves
Here we consider the clinical presentations of dysfunction of cranial nerves IX−XII. Lesions of the glossopharyngeal and vagus nn. produce dysphagia, hoarseness, and dysphonia. Lesions of the accessory n., depending on their level, produce weakness of the sternocleidomastoid m. and trapezius m. Lesions of the hypoglossal n. produce ipsilateral weakness of the tongue.
Lesions of the Glossopharyngeal and
Vagus Nerves
Anatomy. The anatomical course and distribution of these nerves is described above on p. 18.
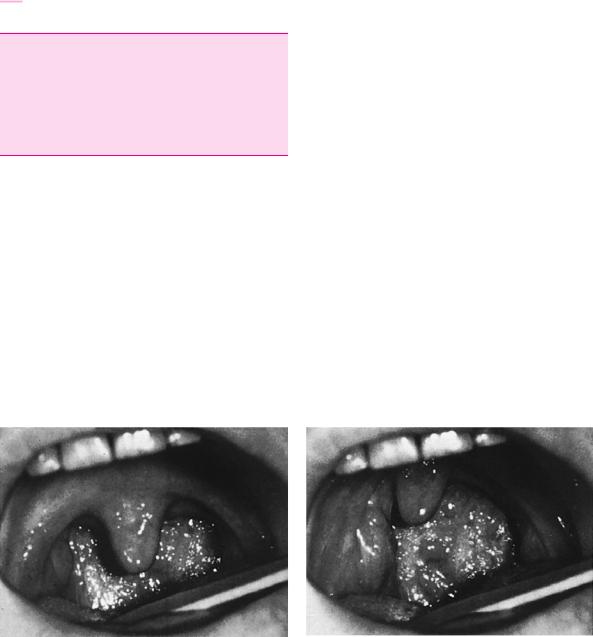
Typical deficits. A unilateral lesion of the glossopharyngeal and vagus nn. causes ipsilateral weakness of the soft palate and posterior pharyngeal wall, which is evident as the curtain sign (Fig. 11.23, see also Fig. 3.13, p. 26). The associated sensory deficit causes dysphagia and unilateral paralysis of the vocal cord causes hoarseness. The patient usually does not notice the loss of sensation in the external auditory canal or the loss of taste on the posterior third of the tongue.
Causes. Palsy affecting the ninth and tenth cranial nerves can be caused by infarction of the corresponding brainstem nuclei (e. g., in Wallenberg syndrome, p. ).
Lesions of the peripheral nerve trunks can be caused by a mass in the posterior fossa or by a bony fracture impinging on the nerves at their site of exit from the jugular foramen. In the latter case, the injury involves not only these nerves, but also the accessory n. (Siebenmann syndrome). Finally, isolated neuritis of these nerves can occur, e. g., in the setting of herpes zoster, or as a cryptogenic event.
Accessory Nerve Palsy
The anatomy and method of examination of the accessory n. are described above.
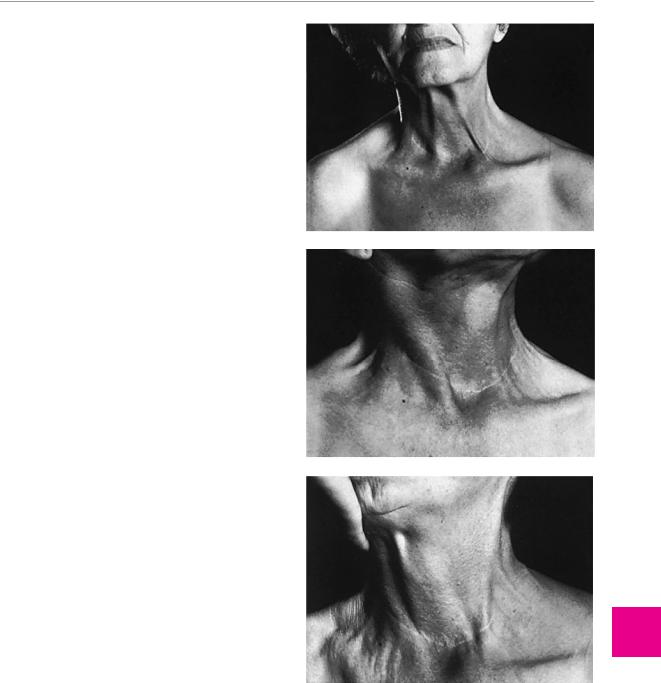
Typical deficits. A lesion of the purely motor main trunk of the accessory n. causes paralysis of the sternocleidomastoid m. and of the upper portion of the trapezius m. (Fig. 11.24). Lesions of the accessory n. in the lateral triangle of the neck, however, are much more common. These spare the sternocleidomastoid m. and weaken only the upper portion of the trapezius m., causing a shoulder droop and an externally rotated position of the scapula (i. e., tilting of the caudal angle of the scapula
a
Fig. 11.23 Curtain sign revealing left-sided palatopharyngeal weakness in a 36-year-old patient with Wallenberg syndrome. a Normal appearance at rest. b Elicitation of the gag reflex is fol-
b
lowed by pulling of the palate and posterior pharyngeal wall to the unaffected right side. (From: Mumenthaler M.: Didaktischer Atlas der klinischen Neurologie. 2nd edn, Springer, Heidelberg 1986.)
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme All rights reserved. Usage subject to terms and conditions of license.
The Lower Cranial Nerves 205
toward the midline). This condition is depicted in Fig. 11.25.
Causes. Dysfunction of the main trunk of the accessory n. is caused by mass lesions in the posterior fossa or at the base of the skull (Siebenmann syndrome, see above). Accessory nerve palsy due to interruption of the nerve in the lateral triangle of the neck is practically always iatrogenic, e. g., as a complication of lymph node biopsy at the posterior border of the sternocleidomastoid m.
Hypoglossal Nerve Palsy
The anatomy and technique of examination of the hypoglossal n. are described above on p. 27.
Typical deficits. The ipsilateral half of the tongue is paretic and, in the course of time, becomes atrophic. When the tongue is protruded, it deviates to the paretic side. This condition is illustrated in Fig. 3.16, p. 27.
Causes. Unilateral hypoglossal nerve palsy is usually due to a bony fracture or a mass lesion—rarely, a congenital malformation—in the posterior cranial fossa. Carotid dissection is another possible cause. Rarely, isolated hypoglossal nerve palsy arises as a postinfectious or cryptogenic event.
Differential diagnosis. Unilateral tongue weakness can also be of central origin, i. e., due to a lesion of the corticobulbar pathway to the hypoglossal nerve nucleus (Fig. 11.18). Central weakness is unaccompanied by atrophy.
Bilateral tongue weakness and atrophy in the setting of true bulbar palsy (p. 80, p. 155) is due to progressive loss of motor neurons in the nucleus of the hypoglossal nerve on both sides of the medulla. The observable abnormalities are slowly progressive and accompanied by fasciculations of the tongue.
Tongue weakness in pseudobulbar palsy (p. 80) is due to bilateral, usually ischemic damage of the central corticobulbar pathways. Because the lesion is central, no atrophy or fasciculations are seen. Examination reveals dysarthria, dysphagia, and abnormal prominence of the perioral reflexes.
a
b Nerves Cranialthe
ofDiseases
11
c
Fig. 11.24 Proximal left accessory nerve palsy with weakness of both the sternocleidomastoid m. and the trapezius m. a Even in the resting position, the upper edge of the trapezius m. is visibly thinner than on the right side, and the left sternocleidomastoid m. is barely discernible. b When the patient turns her head to the left, the intact right sternocleidomastoid m. is clearly seen. c When the head is turned to the right, there is only faint contraction of the left sternocleidomastoid m. (From: Mumenthaler M.: Didaktischer Atlas der klinischen Neurologie. 2nd edn, Springer, Heidelberg 1986.)
Thieme Argo OneArgo bold
ArgoOneBold
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme All rights reserved. Usage subject to terms and conditions of license.
