
- •Overview
- •Preface
- •Translator’s Note
- •Contents
- •1. Fundamentals
- •Microscopic Anatomy of the Nervous System
- •Elements of Neurophysiology
- •Elements of Neurogenetics
- •General Genetics
- •Neurogenetics
- •Genetic Counseling
- •2. The Clinical Interview in Neurology
- •General Principles of History Taking
- •Special Aspects of History Taking
- •3. The Neurological Examination
- •Basic Principles of the Neurological Examination
- •Stance and Gait
- •Examination of the Head and Cranial Nerves
- •Head and Cervical Spine
- •Cranial Nerves
- •Examination of the Upper Limbs
- •Motor Function and Coordination
- •Muscle Tone and Strength
- •Reflexes
- •Sensation
- •Examination of the Trunk
- •Examination of the Lower Limbs
- •Coordination and Strength
- •Reflexes
- •Sensation
- •Examination of the Autonomic Nervous System
- •Neurologically Relevant Aspects of the General Physical Examination
- •Neuropsychological and Psychiatric Examination
- •Psychopathological Findings
- •Neuropsychological Examination
- •Special Considerations in the Neurological Examination of Infants and Young Children
- •Reflexes
- •4. Ancillary Tests in Neurology
- •Fundamentals
- •Imaging Studies
- •Conventional Skeletal Radiographs
- •Computed Tomography (CT)
- •Magnetic Resonance Imaging (MRI)
- •Angiography with Radiological Contrast Media
- •Myelography and Radiculography
- •Electrophysiological Studies
- •Fundamentals
- •Electroencephalography (EEG)
- •Evoked potentials
- •Electromyography
- •Electroneurography
- •Other Electrophysiological Studies
- •Ultrasonography
- •Other Ancillary Studies
- •Cerebrospinal Fluid Studies
- •Tissue Biopsies
- •Perimetry
- •5. Topical Diagnosis and Differential Diagnosis of Neurological Syndromes
- •Fundamentals
- •Muscle Weakness and Other Motor Disturbances
- •Sensory Disturbances
- •Anatomical Substrate of Sensation
- •Disturbances of Consciousness
- •Dysfunction of Specific Areas of the Brain
- •Thalamic Syndromes
- •Brainstem Syndromes
- •Cerebellar Syndromes
- •6. Diseases of the Brain and Meninges
- •Congenital and Perinatally Acquired Diseases of the Brain
- •Fundamentals
- •Special Clinical Forms
- •Traumatic Brain injury
- •Fundamentals
- •Traumatic Hematomas
- •Complications of Traumatic Brain Injury
- •Intracranial Pressure and Brain Tumors
- •Intracranial Pressure
- •Brain Tumors
- •Cerebral Ischemia
- •Nontraumatic Intracranial Hemorrhage
- •Infectious Diseases of the Brain and Meninges
- •Infections Mainly Involving the Meninges
- •Infections Mainly Involving the Brain
- •Intracranial Abscesses
- •Congenital Metabolic Disorders
- •Acquired Metabolic Disorders
- •Diseases of the Basal Ganglia
- •Fundamentals
- •Diseases Causing Hyperkinesia
- •Other Types of Involuntary Movement
- •Cerebellar Diseases
- •Dementing Diseases
- •The Dementia Syndrome
- •Vascular Dementia
- •7. Diseases of the Spinal Cord
- •Anatomical Fundamentals
- •The Main Spinal Cord Syndromes and Their Anatomical Localization
- •Spinal Cord Trauma
- •Spinal Cord Compression
- •Spinal Cord Tumors
- •Myelopathy Due to Cervical Spondylosis
- •Circulatory Disorders of the Spinal Cord
- •Blood Supply of the Spinal Cord
- •Arterial Hypoperfusion
- •Impaired Venous Drainage
- •Infectious and Inflammatory Diseases of the Spinal Cord
- •Syringomyelia and Syringobulbia
- •Diseases Mainly Affecting the Long Tracts of the Spinal Cord
- •Diseases of the Anterior Horns
- •8. Multiple Sclerosis and Other Myelinopathies
- •Fundamentals
- •Myelin
- •Multiple Sclerosis
- •Other Demyelinating Diseases of Unknown Pathogenesis
- •9. Epilepsy and Its Differential Diagnosis
- •Types of Epilepsy
- •Classification of the Epilepsies
- •Generalized Seizures
- •Partial (Focal) Seizures
- •Status Epilepticus
- •Episodic Neurological Disturbances of Nonepileptic Origin
- •Episodic Disturbances with Transient Loss of Consciousness and Falling
- •Episodic Loss of Consciousness without Falling
- •Episodic Movement Disorders without Loss of Consciousness
- •10. Polyradiculopathy and Polyneuropathy
- •Fundamentals
- •Polyradiculitis
- •Cranial Polyradiculitis
- •Polyradiculitis of the Cauda Equina
- •Polyneuropathy
- •Fundamentals
- •11. Diseases of the Cranial Nerves
- •Fundamentals
- •Disturbances of Smell (Olfactory Nerve)
- •Neurological Disturbances of Vision (Optic Nerve)
- •Visual Field Defects
- •Impairment of Visual Acuity
- •Pathological Findings of the Optic Disc
- •Disturbances of Ocular and Pupillary Motility
- •Fundamentals of Eye Movements
- •Oculomotor Disturbances
- •Supranuclear Oculomotor Disturbances
- •Lesions of the Nerves to the Eye Muscles and Their Brainstem Nuclei
- •Ptosis
- •Pupillary Disturbances
- •Lesions of the Trigeminal Nerve
- •Lesions of the Facial Nerve
- •Disturbances of Hearing and Balance; Vertigo
- •Neurological Disturbances of Hearing
- •Disequilibrium and Vertigo
- •The Lower Cranial Nerves
- •Accessory Nerve Palsy
- •Hypoglossal Nerve Palsy
- •Multiple Cranial Nerve Deficits
- •12. Diseases of the Spinal Nerve Roots and Peripheral Nerves
- •Fundamentals
- •Spinal Radicular Syndromes
- •Peripheral Nerve Lesions
- •Fundamentals
- •Diseases of the Brachial Plexus
- •Diseases of the Nerves of the Trunk
- •13. Painful Syndromes
- •Fundamentals
- •Painful Syndromes of the Head And Neck
- •IHS Classification of Headache
- •Approach to the Patient with Headache
- •Migraine
- •Cluster Headache
- •Tension-type Headache
- •Rare Varieties of Primary headache
- •Symptomatic Headache
- •Painful Syndromes of the Face
- •Dangerous Types of Headache
- •“Genuine” Neuralgias in the Face
- •Painful Shoulder−Arm Syndromes (SAS)
- •Neurogenic Arm Pain
- •Vasogenic Arm Pain
- •“Arm Pain of Overuse”
- •Other Types of Arm Pain
- •Pain in the Trunk and Back
- •Thoracic and Abdominal Wall Pain
- •Back Pain
- •Groin Pain
- •Leg Pain
- •Pseudoradicular Pain
- •14. Diseases of Muscle (Myopathies)
- •Structure and Function of Muscle
- •General Symptomatology, Evaluation, and Classification of Muscle Diseases
- •Muscular Dystrophies
- •Autosomal Muscular Dystrophies
- •Myotonic Syndromes and Periodic Paralysis Syndromes
- •Rarer Types of Muscular Dystrophy
- •Diseases Mainly Causing Myotonia
- •Metabolic Myopathies
- •Acute Rhabdomyolysis
- •Mitochondrial Encephalomyopathies
- •Myositis
- •Other Diseases Affecting Muscle
- •Myopathies Due to Systemic Disease
- •Congenital Myopathies
- •Disturbances of Neuromuscular Transmission−Myasthenic Syndromes
- •15. Diseases of the Autonomic Nervous System
- •Anatomy
- •Normal and Pathological Function of the Autonomic Nervous System
- •Sweating
- •Bladder, Bowel, and Sexual Function
- •Generalized Autonomic Dysfunction
- •Index
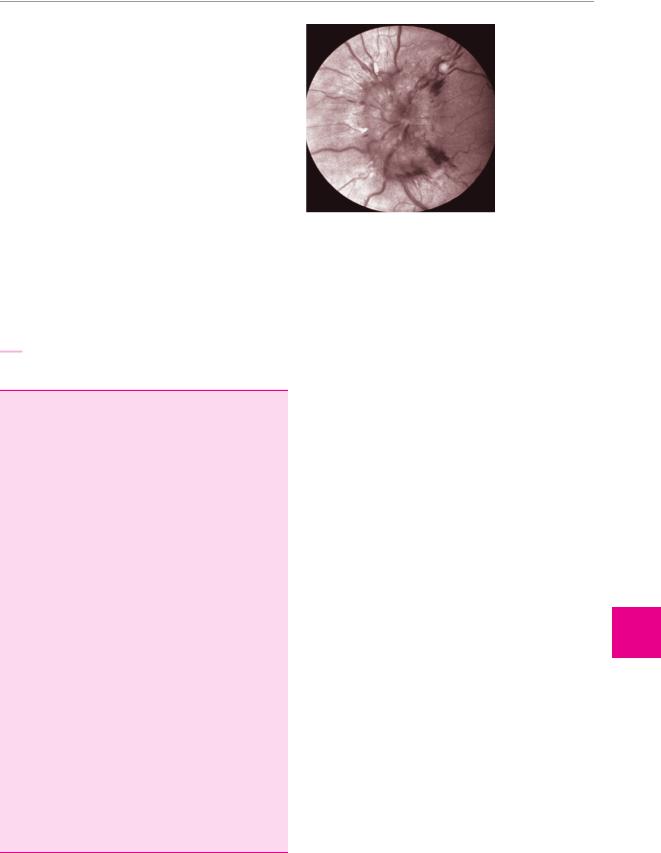
matory disorders, such as syphilis. The typical findings include a somewhat enlarged, hyperemic optic disc with blurred margins, enlarged veins, and usually hemorrhages (Fig. 11.2). Inexperienced clinicians often have difficulty distinguishing papilledema from other changes of the optic disc.
Optic nerve atrophy is a permanent residual finding after lesions of the optic n. The extent of visual loss, however, need not reflect the degree of visible atrophy. The optic disc is pale all the way to the disc margin, which remains sharp. These findings are typically seen after retrobulbar neuritis, for example (Fig. 3.4, p. 18), but also after optic nerve compression (whether from outside, as by a meningioma, or from inside by an optic glioma). Further causes of optic nerve atrophy include chronic papilledema, syphilis, Leber hereditary optic nerve atrophy (LHON, a mitochondrial disease occurring in men), many types of spinocerebellar degeneration, ischemia, and exogenous intoxication.
183
Fig. 11.2 Acute papilledema (left eye) in a patient with a brain tumor. The optic disc is swollen, with blurred margins and small, linear hemorrhages.
Disturbances of Ocular and Pupillary Motility
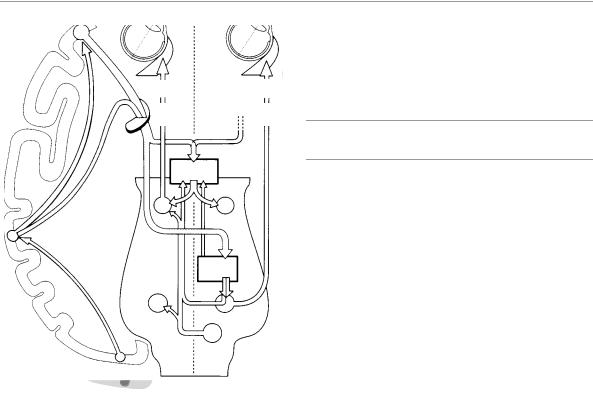
Eye movements enable the fixation of gaze and the visual pursuit of objects that are in motion relative to the observer, whether the object itself of the observer is actually moving. The anatomical substrate of eye movements consists of the frontal and posterior eye fields, whose major projections descend to the paramedian pontine reticular formation (PPRF) on both sides of the pons. The PPRF, in turn, controls movements for horizontal gaze, as well as movements for vertical gaze through its interaction with the midbrain reticular formation. Vestibular afferent input and cerebellar connections also play important roles in the control of eye movements. Lesions of these supranuclear structures, whatever their etiology, cause horizontal or vertical gaze palsy or internuclear ophthalmoplegia. Clinically, it is important to distinguish nuclear from infranuclear disturbances of the oculomotor, trochlear, and abducens nerves, all of which can have a variety of causes. In addition, the motor functions of the brainstem, including eye movements, can also be disturbed in myasthenia gravis, muscle diseases, and orbital processes, any of which can cause diplopia. Pupillary motility can be altered by many different disease processes. Retinal and optic nerve lesions affect the afferent arm of the pupillary light reflex loop, while oculomotor nerve lesions affect its efferent arm. In the former case, the pupil constricts only upon illumination of the ipsilateral eye; in the latter case, the pupil is dilated and remains so regardless of which eye is illuminated. Loss of the sympathetic nerve supply to the eye causes Horner syndrome.
Fundamentals of Eye Movements
The anatomical substrate of eye movements consists of the following structures:
cortical areas in the frontal, occipital, and temporal lobes, in which the impulses for voluntary, conjugate eye movements and ocular pursuit movements are generated;
a number of important gaze centers in the brainstem
(particularly the paramedian pontine reticular formation, PPRF, and midbrain nuclei) that relay the cortical impulses onward to the motor nuclei innervating the eye muscles in such a way that coordinated movements of the eyes can occur along the three major axes (horizontal, vertical, and rotatory movements). Special white matter tracts play an important role in this process, particularly the medial longitudinal fasciculus (MLF, Fig. 11.3);
finally, the motor nuclei and cranial nerves that innervate the eye muscles (cf. Fig. 3.8a, p. 21);
the entire process is also affected by cerebellar impulses and by vestibular impulses that enter the central nervous system through the eighth cranial nerve.
Types of eye movement. Eye movements can be divided into the following types:
Saccades are rapid conjugate movements that are executed voluntarily or in reflex fashion in response to stimuli of various kinds. They serve to fix a new object in the center of vision. Small microsaccades have an angular velocity of 20°/s, larger ones up to 700°/s. Saccades are the elementary type of rapid eye movement.
Once the gaze has been fixated on a given object, slow pursuit movements serve to keep it in view if it is moving. The pursuit system is responsible for executing these conjugate eye movements: from the
Thieme Argo OneArgo bold
ArgoOneBold
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme All rights reserved. Usage subject to terms and conditions of license.
Diseases of the Cranial Nerves
11
184 11 Diseases of the Cranial Nerves
frontal eye |
|
|
field |
|
|
(area 8) |
|
|
|
medial |
lateral |
|
rectus m. |
rectus m. |
internal |
|
|
capsule |
|
|
|
riMLF |
|
posterior |
III |
III |
|
|
|
eye fields |
|
|
in temporal |
|
|
and parietal |
medial |
|
cortex |
longitu- |
PPRF |
|
dinal |
|
|
fasciculus |
|
|
VI |
VI |
|
|
|
|
|
VIII |
visual cortex |
|
|
(areas 17, 18, 19) |
|
|
Fig. 11.3 Anatomical substrate of conjugate eye movements.
The diagram shows the anatomical pathways for a conjugate movement to the right: neural impulses flow from the cortical eye fields of the left hemisphere to the right PPRF and onward to the nucleus of the right abducens n. Impulses in the abducens n. induce contraction of the lateral rectus m. of the right eye. Meanwhile, cortical impulses also travel by way of the medial longitudinal fasciculus to the nucleus of the left oculomotor n., and impulses in this nerve induce contraction of the medial rectus m. of the left eye. Thus, lesions of the hemispheres or of the PPRF result in a palsy of conjugate horizontal gaze (hemispheric lesion: contralateral gaze palsy, PPRF lesion: ipsilateral gaze palsy). On the other hand, lesions of the medial longitudinal fasciculus cause an isolated loss of adduction of one eye during horizontal eye movement (internuclear ophthalmoplegia). Vertical eye movements are generated by the midbrain reticular formation (riMLF, p. 188), which receives input from both the cerebral cortex and the PPRF.
visual cortex in the occipital lobe, impulses travel to the eye fields of the temporal lobe (“medial superior temporal visual area,” MST) and the neighboring parietal cortex. These areas are interconnected with the paramedian pontine reticular formation (PPRF) and with the cerebellum. Impulses from the PPRF control the nuclei of the eye muscles either directly or by way of interneurons.
Disturbances of the pursuit system cause pursuit movements to break up into saccades. If the saccade system is also damaged, gaze palsy can result (see below).
Convergence movements serve to fix a nearby object in view and involve simultaneous adduction of both eyes.
Oculomotor Disturbances
Nystagmus
In purely descriptive terms, nystagmus is an involuntary, repetitive, rhythmic movement of the eyes. Nystagmus is often, but not always, pathological.
! Nystagmus is sometimes physiological.
Examples of physiological nystagmus include optokinetic nystagmus (p. 186) and the type of vestibular nystagmus that is induced by rotation in a swivel chair. End-gaze nystagmus (p. 185) is also physiological, as long as it occurs symmetrically in both directions. Pathological nystagmus, on the other hand, indicates the presence of a lesion in the anatomical structures subserving eye movements. A large number of components in this system can be damaged and nystagmus has a correspondingly wide spectrum of possible causes (see below).
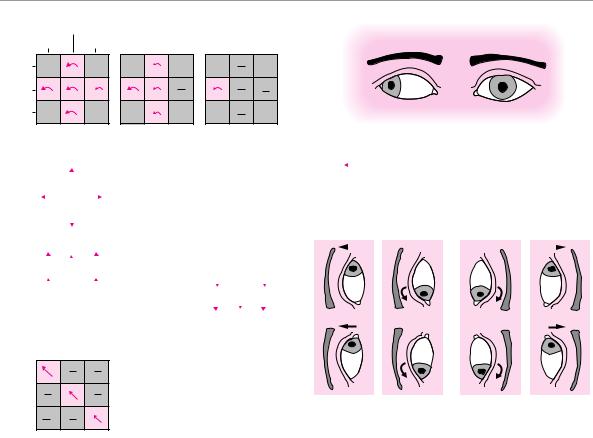
Phenomenological classification of nystagmus. As already discussed to some extent in Chapter 3, nystagmus can be characterized according to various criteria:
Jerk vs. pendular nystagmus: most types of nystagmus are either of the “jerking” type, i. e., with a fast and a slow phase, or pendular (back-and-forth).
Direction of beat in relation to the three major axes of eye movement: one speaks of horizontal, vertical, or rotatory nystagmus.
Direction of beat in relation to the midline of the eye: nystagmus may beat to the left, to the right, upward, downward, or diagonally.
In saltatory nystagmus, the direction of beat is defined, by convention, as that of the rapid phase, even though the slow phase is actually the pathological component and the rapid phase is a physiological correction for it, serving to return the eyes to their original position.
Nystagmus can be spontaneous (p. 185) or else present only in response to specific precipitating stimuli
(e. g., position, change of position, a rotatory or thermal stimulus to the vestibular system, or a particular direction of gaze gaze-evoked nystagmus, p. 185).
The examiner must also determine whether nystagmus is equally severe in both eyes, or whether it is weaker or perhaps nonexistent in one eye. Nystagmus that is unequal in the two eyes is also called dissociated nystagmus.
A mainly phenomenologically oriented listing and illustration of the most important types of nystagmus and their causes, is found in Table 11.1 and Fig. 11.4.
There are a few rarer types of nystagmus whose phenomenology is quite complex and not easily described by the criteria listed above. These types of nystagmus are summarized in Table 11.2.
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme All rights reserved. Usage subject to terms and conditions of license.
Disturbances of Ocular and Pupillary Motility 185
Table 11.1 Important physiological and pathological types of nystagmus (after Henn)
Type of nystagmus |
Physiological |
Pathological |
Remarks |
|
|
|
|
Optokinetic nystagmus |
must be symmetrically |
if asymmetric, |
can be seen and tested by having the patient fixate |
|
present |
dissociated, slowed, or |
on the pattern on a rotating drum |
|
|
absent |
|
Vestibular nystagmus |
must be symmetrically |
if asymmetric, |
elicited by lavage of the external auditory canal with |
|
present |
dissociated, or absent |
cold or warm water (always after otoscopy to ex- |
|
|
|
clude a tympanic defect); also elicitable by rotating |
|
|
|
the patient in a swivel chair, if Frenzel goggles are |
|
|
|
worn to prevent fixation |
Spontaneous nystagmus |
up to 5°/second is |
if present in light |
unidirectional: the nystagmus always beats in the |
|
normal in the dark |
|
same direction, independent of the direction of |
|
|
|
gaze; can be inhibited by visual fixation; may be due |
|
|
|
to a central or peripheral vestibular lesion |
|
|
|
Grade III: present in all directions of gaze |
|
|
|
Grade II: visible with gaze straight ahead or in the |
|
|
|
direction of the nystagmus |
|
|
|
Grade I: visible only with gaze in the direction of |
|
|
|
nystagmus |
|
|
|
Head-shaking nystagmus: occurs only after vigorous |
|
|
|
shaking of the head |
Gaze-evolved |
never |
always pathological |
beats in the direction of gaze; defined as nystagmus |
nystagmus (p. 26) |
|
|
in binocular visual field; lesion always central |
End-gaze nystagmus |
if symmetric |
if asymmetric or |
defined as nystagmus in monocular visual field |
(p. 26) |
|
dissociated |
|
Positional nystagmus |
|
always pathological |
elicited by rapidly placing the patient supine with |
|
|
|
the head hanging down 30° and to one side (Hall- |
|
|
|
pike maneuver); latency of one to several seconds, |
|
|
|
then increasing intensity for a few seconds and |
|
|
|
equally rapid decline; accompanied by a strong feel- |
|
|
|
ing of rotation and dizziness; the nystagmus is |
|
|
|
mainly rotatory, clockwise when the head hangs |
|
|
|
down and to the left, counterclockwise when it |
|
|
|
hangs down and to the right; the response |
|
|
|
diminishes (habituates) on repeated elicitation |
Pendular nystagmus
Nystagmus in the vesti- bulo-ocular suppression test
always pathological, but |
sinusoidal to-and-fro movement increasing with at- |
does not indicate active |
tention or monocular fixation; usually congenital, |
disease |
rarely acquired |
always pathological |
when the patient is passively rotated en bloc while |
|
keeping the arms in forward extension and staring |
|
at the thumbs, visual fixation normally completely |
|
suppresses vestibular nystagmus; if nystagmus does |
|
appear, this indicates a lesion of the vestibulocere- |
|
bellum or of its afferent or efferent connections; |
|
the test can be falsely positive with inadequate fixa- |
|
tion |
Diseases of the Cranial Nerves
11
Topical classification of pathological nystagmus.
Often, the type of nystagmus that is present already provides a clue to the site of the lesion:
Gaze-paretic nystagmus. This type of nystagmus may be due to disease of the eye muscles themselves, or to a lesion of the cranial nerves innervating the eye muscles or of the corresponding brainstem nuclei.
Gaze-paretic nystagmus is usually slow, coarse, and in the direction of the impairment of gaze.
Vestibular nystagmus is due to a lesion of the vestibular organ itself or of the vestibular n. or its nuclei in the brainstem. It typically appears as a spontaneous nystagmus beating away from the side of the lesion, regardless of the direction of gaze (nystagmus in a fixed direction, cf. Table 11.1). Vestibular nystagmus
is typically inhibited by fixation; it is sometimes observable only if fixation is abolished by having the patient wear Frenzel goggles or shake the head rapidly.
Gaze-evoked nystagmus beats in the direction of gaze and indicates a lesion in the brainstem or its afferent or efferent connections with the cerebellum. If caused by a unilateral cerebellar lesion, it can be highly asymmetrical or even beat only to the side of the lesion. In such patients, gaze-evoked nystagmus can be difficult to distinguish from vestibular nystagmus.
Nystagmus due to brainstem lesions. Vestibular spontaneous nystagmus, gaze-evoked nystagmus, upbeat or downbeat vertical nystagmus and posi-
Thieme Argo OneArgo bold
ArgoOneBold
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme All rights reserved. Usage subject to terms and conditions of license.
186 11 Diseases of the Cranial Nerves
direction |
|
central |
of gaze: |
right |
left |
|
||
upward |
|
|
central |
|
|
down- |
|
|
ward |
|
|
|
|
|
grade III |
grade II |
|
grade I |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
spontaneous nystagmus |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
gaze-evoked nystagmus |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
dissociated |
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
nystagmus in INO |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
upbeat |
downbeat |
|
|
nystagmus |
nystagmus |
|
|
|
obliquely beating |
|
|
|
nystagmus |
positional nystagmus |
|
|
|
||
|
|
right side of head down |
left side of head down |
Fig. 11.4 The most important types of nystagmus. For each type of nystagmus, the figure shows the intensity and direction of beating, depending on the direction of gaze.
tional and/or positioning nystagmus can all indicate the presence of a brainstem lesion. These types of nystagmus are often rotatory or dissociated (as in internuclear ophthalmoplegia).
Positioning nystagmus is a predominantly rotatory nystagmus lasting several seconds after changes of position of a particular type; it is found in benign paroxysmal positioning vertigo, a disorder of the peripheral portion of the vestibular system (p. 202).
Congenital pendular nystagmus is characterized by conjugate, pendular eye movements that increase with attention or monocular fixation. It is normally well compensated. There is no underlying, pathological structural lesion.
Physiological nystagmus. The most important example is optokinetic nystagmus. This normal phenomenon serves to stabilize the visual image of a moving object on the retina and thus has the same purpose as the vestibulo-ocular reflex.
Optokinetic nystagmus consists of slow pursuit movements alternating with rapid return movements (saccades). The return movements occur whenever the moving object “threatens” to leave the visual field. If the object is moving very rapidly, optokinetic nystagmus can be voluntarily suppressed. Absent, asymmetrical, or dissociated optokinetic nystagmus is pathological.
Vestibulo-ocular reflex (VOR) is a function of the labyrinth that serves to stabilize gaze fixation on rapid movement of the head: it produces a compensatory eye movement in the direction opposite the head movement. Slower head movements do not need to be compensated for by the vestibular system, as the ocular pursuit system suffices to keep gaze fixated in this case (see above, p. 183). Vestibular nystagmus can be suppressed by fixation on an object moving in tandem with the head (nystagmus or VOR suppression test, see below). An inability to suppress the VOR by fixation is pathological.
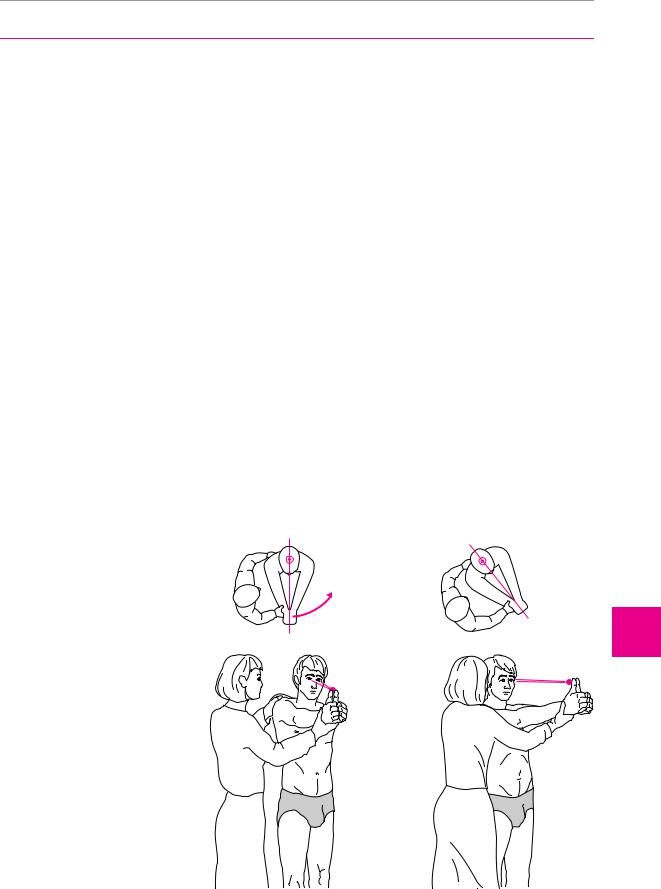
Nystagmus suppression test (= VOR suppression test).
In this test, the subject stretches both arms forward, holds his or her thumbs up, and fixates gaze on them. When the subject is then rapidly rotated around the long axis of the body, there is normally no nystagmus, because vestibular nystagmus can be suppressed by visual fixation (Fig. 11.5). If nystagmus does appear, this indicates a lesion in the cerebellum or its connections with the vestibular apparatus of the brainstem.
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme All rights reserved. Usage subject to terms and conditions of license.
Disturbances of Ocular and Pupillary Motility 187
Table 11.2 Rare types of nystagmus
Type |
Characteristics |
Localization |
Cause (examples) |
||||
|
|
|
|
|
|
|
|
Seesaw nystagmus |
alternating movement of one eye upward and the |
oral brainstem and dien- |
tumor, multiple sclerosis, |
||||
|
other eye downward, with simultaneous rotation; |
cephalon |
vascular, syringobulbia |
||||
|
various other kinds of eye movement can resemble this |
|
|
|
|
||
|
type of nystagmus |
|
|
|
|
||
Downbeat nystagmus |
vertical nystagmus with downward rapid component |
caudal medullary lesion, |
as above; phenytoin in- |
||||
|
|
|
|
vitamin B12 deficiency |
toxication, drugs of |
||
|
|
|
|
|
|
abuse |
|
Convergence |
slow abduction followed by rapid adduction of both |
(rostral) midbrain |
as above |
||||
nystagmus |
eyes |
tegmentum |
|
|
|||
Retractory nystagmus |
jerking movements of both eyes back into their sock- |
midbrain tegmentum |
rare: tumor, multiple |
||||
|
ets, usually accompanied by other oculomotor distur- |
|
|
sclerosis, vascular |
|||
|
bances |
|
|
|
|
||
Nystagmus with |
vertical nystagmus with upward rapid component ac- |
pons and periaqueductal |
often vascular |
||||
eyelid response |
companied by simultaneous rapid raising of upper lid |
region |
|
|
|||
Monocular nystagmus |
in internuclear ophthalmoplegia; as an ictal phenome- |
medial longitudinal |
very rarely ictal |
||||
|
non in epilepsy |
fasciculus |
|
|
|||
Opsoclonus |
spontaneous, grouped, variably rapid, nonrhythmic |
brainstem and |
paraneoplastic, neuro- |
||||
(gaze myoclonus, |
conjugate eye movements, irregularly “dancing” back |
cerebellum |
blastoma, multiple |
||||
dancing eyes) |
and forth |
|
|
sclerosis, encephalitis |
|||
Ocular bobbing |
rapid, nonrhythmic downward beating of the eyes, |
pons, compression by |
tumor, ischemia, hemor- |
||||
|
which stay down for a few seconds, then slowly return |
cerebellar hemorrhage |
rhage |
||||
|
to the original position; when it appears unilaterally, |
(lesion of central |
|
|
|||
|
the other side is usually blocked by a paresis of the |
tegmental tract) |
|
|
|||
|
extraocular muscles (usually oculomotor nerve palsy); |
|
|
|
|
||
|
may also be accompanied by simultaneous palatal |
|
|
|
|
||
|
nystagmus |
|
|
|
|
||
Gaze dysmetria |
overshooting movements when redirecting gaze to a |
cerebellar |
e. g., multiple sclerosis |
||||
|
new target, followed by compensatory corrections |
|
|
|
|
||
|
(ocular apraxia) |
|
|
|
|
||
Ocular flutter (ocular |
rapid, irregular back-and-forth movements around the |
as for opsoclonus and |
|
|
|||
myoclonus) |
point of fixation |
gaze dysmetria |
|
|
|||
|
|
|
|
|
|
|
|
Fig. 11.5 Nystagmus suppression test. |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
The patient extends the arms, fixates gaze |
|
|
|
|
|
|
|
on his or her own thumbs, and is then |
|
|
|
|
|
|
|
rapidly rotated “en bloc” by the examiner. |
|
|
|
|
|
|
|
In a normal individual, gaze fixation on the |
|
|
|
|
|
|
|
thumbs prevents the appearance of nystag- |
|
|
|
|
|
|
|
mus. Failure to suppress nystagmus indi- |
|
|
|
|
|
|
|
cates a central lesion, usually in the cere- |
|
|
|
|
|
|
|
bellum. |
|
|
|
|
|
|
|
Diseases of the Cranial Nerves
11
Thieme Argo OneArgo bold
ArgoOneBold
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme All rights reserved. Usage subject to terms and conditions of license.
