
- •Overview
- •Preface
- •Translator’s Note
- •Contents
- •1. Fundamentals
- •Microscopic Anatomy of the Nervous System
- •Elements of Neurophysiology
- •Elements of Neurogenetics
- •General Genetics
- •Neurogenetics
- •Genetic Counseling
- •2. The Clinical Interview in Neurology
- •General Principles of History Taking
- •Special Aspects of History Taking
- •3. The Neurological Examination
- •Basic Principles of the Neurological Examination
- •Stance and Gait
- •Examination of the Head and Cranial Nerves
- •Head and Cervical Spine
- •Cranial Nerves
- •Examination of the Upper Limbs
- •Motor Function and Coordination
- •Muscle Tone and Strength
- •Reflexes
- •Sensation
- •Examination of the Trunk
- •Examination of the Lower Limbs
- •Coordination and Strength
- •Reflexes
- •Sensation
- •Examination of the Autonomic Nervous System
- •Neurologically Relevant Aspects of the General Physical Examination
- •Neuropsychological and Psychiatric Examination
- •Psychopathological Findings
- •Neuropsychological Examination
- •Special Considerations in the Neurological Examination of Infants and Young Children
- •Reflexes
- •4. Ancillary Tests in Neurology
- •Fundamentals
- •Imaging Studies
- •Conventional Skeletal Radiographs
- •Computed Tomography (CT)
- •Magnetic Resonance Imaging (MRI)
- •Angiography with Radiological Contrast Media
- •Myelography and Radiculography
- •Electrophysiological Studies
- •Fundamentals
- •Electroencephalography (EEG)
- •Evoked potentials
- •Electromyography
- •Electroneurography
- •Other Electrophysiological Studies
- •Ultrasonography
- •Other Ancillary Studies
- •Cerebrospinal Fluid Studies
- •Tissue Biopsies
- •Perimetry
- •5. Topical Diagnosis and Differential Diagnosis of Neurological Syndromes
- •Fundamentals
- •Muscle Weakness and Other Motor Disturbances
- •Sensory Disturbances
- •Anatomical Substrate of Sensation
- •Disturbances of Consciousness
- •Dysfunction of Specific Areas of the Brain
- •Thalamic Syndromes
- •Brainstem Syndromes
- •Cerebellar Syndromes
- •6. Diseases of the Brain and Meninges
- •Congenital and Perinatally Acquired Diseases of the Brain
- •Fundamentals
- •Special Clinical Forms
- •Traumatic Brain injury
- •Fundamentals
- •Traumatic Hematomas
- •Complications of Traumatic Brain Injury
- •Intracranial Pressure and Brain Tumors
- •Intracranial Pressure
- •Brain Tumors
- •Cerebral Ischemia
- •Nontraumatic Intracranial Hemorrhage
- •Infectious Diseases of the Brain and Meninges
- •Infections Mainly Involving the Meninges
- •Infections Mainly Involving the Brain
- •Intracranial Abscesses
- •Congenital Metabolic Disorders
- •Acquired Metabolic Disorders
- •Diseases of the Basal Ganglia
- •Fundamentals
- •Diseases Causing Hyperkinesia
- •Other Types of Involuntary Movement
- •Cerebellar Diseases
- •Dementing Diseases
- •The Dementia Syndrome
- •Vascular Dementia
- •7. Diseases of the Spinal Cord
- •Anatomical Fundamentals
- •The Main Spinal Cord Syndromes and Their Anatomical Localization
- •Spinal Cord Trauma
- •Spinal Cord Compression
- •Spinal Cord Tumors
- •Myelopathy Due to Cervical Spondylosis
- •Circulatory Disorders of the Spinal Cord
- •Blood Supply of the Spinal Cord
- •Arterial Hypoperfusion
- •Impaired Venous Drainage
- •Infectious and Inflammatory Diseases of the Spinal Cord
- •Syringomyelia and Syringobulbia
- •Diseases Mainly Affecting the Long Tracts of the Spinal Cord
- •Diseases of the Anterior Horns
- •8. Multiple Sclerosis and Other Myelinopathies
- •Fundamentals
- •Myelin
- •Multiple Sclerosis
- •Other Demyelinating Diseases of Unknown Pathogenesis
- •9. Epilepsy and Its Differential Diagnosis
- •Types of Epilepsy
- •Classification of the Epilepsies
- •Generalized Seizures
- •Partial (Focal) Seizures
- •Status Epilepticus
- •Episodic Neurological Disturbances of Nonepileptic Origin
- •Episodic Disturbances with Transient Loss of Consciousness and Falling
- •Episodic Loss of Consciousness without Falling
- •Episodic Movement Disorders without Loss of Consciousness
- •10. Polyradiculopathy and Polyneuropathy
- •Fundamentals
- •Polyradiculitis
- •Cranial Polyradiculitis
- •Polyradiculitis of the Cauda Equina
- •Polyneuropathy
- •Fundamentals
- •11. Diseases of the Cranial Nerves
- •Fundamentals
- •Disturbances of Smell (Olfactory Nerve)
- •Neurological Disturbances of Vision (Optic Nerve)
- •Visual Field Defects
- •Impairment of Visual Acuity
- •Pathological Findings of the Optic Disc
- •Disturbances of Ocular and Pupillary Motility
- •Fundamentals of Eye Movements
- •Oculomotor Disturbances
- •Supranuclear Oculomotor Disturbances
- •Lesions of the Nerves to the Eye Muscles and Their Brainstem Nuclei
- •Ptosis
- •Pupillary Disturbances
- •Lesions of the Trigeminal Nerve
- •Lesions of the Facial Nerve
- •Disturbances of Hearing and Balance; Vertigo
- •Neurological Disturbances of Hearing
- •Disequilibrium and Vertigo
- •The Lower Cranial Nerves
- •Accessory Nerve Palsy
- •Hypoglossal Nerve Palsy
- •Multiple Cranial Nerve Deficits
- •12. Diseases of the Spinal Nerve Roots and Peripheral Nerves
- •Fundamentals
- •Spinal Radicular Syndromes
- •Peripheral Nerve Lesions
- •Fundamentals
- •Diseases of the Brachial Plexus
- •Diseases of the Nerves of the Trunk
- •13. Painful Syndromes
- •Fundamentals
- •Painful Syndromes of the Head And Neck
- •IHS Classification of Headache
- •Approach to the Patient with Headache
- •Migraine
- •Cluster Headache
- •Tension-type Headache
- •Rare Varieties of Primary headache
- •Symptomatic Headache
- •Painful Syndromes of the Face
- •Dangerous Types of Headache
- •“Genuine” Neuralgias in the Face
- •Painful Shoulder−Arm Syndromes (SAS)
- •Neurogenic Arm Pain
- •Vasogenic Arm Pain
- •“Arm Pain of Overuse”
- •Other Types of Arm Pain
- •Pain in the Trunk and Back
- •Thoracic and Abdominal Wall Pain
- •Back Pain
- •Groin Pain
- •Leg Pain
- •Pseudoradicular Pain
- •14. Diseases of Muscle (Myopathies)
- •Structure and Function of Muscle
- •General Symptomatology, Evaluation, and Classification of Muscle Diseases
- •Muscular Dystrophies
- •Autosomal Muscular Dystrophies
- •Myotonic Syndromes and Periodic Paralysis Syndromes
- •Rarer Types of Muscular Dystrophy
- •Diseases Mainly Causing Myotonia
- •Metabolic Myopathies
- •Acute Rhabdomyolysis
- •Mitochondrial Encephalomyopathies
- •Myositis
- •Other Diseases Affecting Muscle
- •Myopathies Due to Systemic Disease
- •Congenital Myopathies
- •Disturbances of Neuromuscular Transmission−Myasthenic Syndromes
- •15. Diseases of the Autonomic Nervous System
- •Anatomy
- •Normal and Pathological Function of the Autonomic Nervous System
- •Sweating
- •Bladder, Bowel, and Sexual Function
- •Generalized Autonomic Dysfunction
- •Index
45
4Ancillary Tests in Neurology
Fundamentals . . . |
45 |
Ultrasonography . . . |
61 |
|
Imaging Studies . |
. . 45 |
Other Ancillary Studies . . . |
63 |
|
Electrophysiological Studies . . . |
54 |
|
|
|
Fundamentals
Neurological conditions can often be correctly diagnosed from the history and physical examination alone, but ancillary tests of various kinds are nonetheless vitally important, in many patients, to confirm the diagnosis and identify the etiology precisely. In this section, we will discuss imaging studies including conventional radiographs, CT and MRI, electrophysiological tests (including EEG, EMG, electroneurography, and evoked potentials), and ultrasonography, as well as the laboratory testing of bodily fluids (blood, CSF) and the histopathological or cytological study of biopsy specimens.
Whenever an ancillary diagnostic test is proposed, the specific indication for the test should be considered carefully and critically:
Only after thorough and meticulous clinical history taking and neurological examination.
Only after the formulation of a clinical differential diagnosis, in which all of the competing diagnoses are ranked by probability.
The study that should be performed is the one whose result is most likely to be important for further diagnostic and therapeutic management,
but only if this will be of clear benefit to the patient,
and only if the risks of performing the study do not outweigh any potential benefit that its findings might bring.
Multiple studies providing the same diagnostic information should not be performed merely for repeated confirmation of the findings.
A study should not be performed if, regardless of its result, another study will have to be performed that is likely to yield at least as much information.
Only very rarely should studies be performed to confirm a diagnosis that is already practically certain.
If a genetic study is contemplated, the potential consequences should be discussed thoroughly with the patient and his or her family before the study is performed.
The costs must not be forgotten.
Because of the high expense of some diagnostic tests—in particular, certain types of imaging study and some of the newer molecular biological studies—the physician is obliged to be cost conscious and order them only when necessary. It is understood, however, that an essential test should not be left out just because of the expense.
Imaging Studies
Conventional Skeletal Radiographs
Even though newer techniques are available, conventional radiograph images can still be of diagnostic use, with or without tomographic (sectional) views. Plain radiograph views of the skull and spine are occasionally indicated for neurological diagnosis.
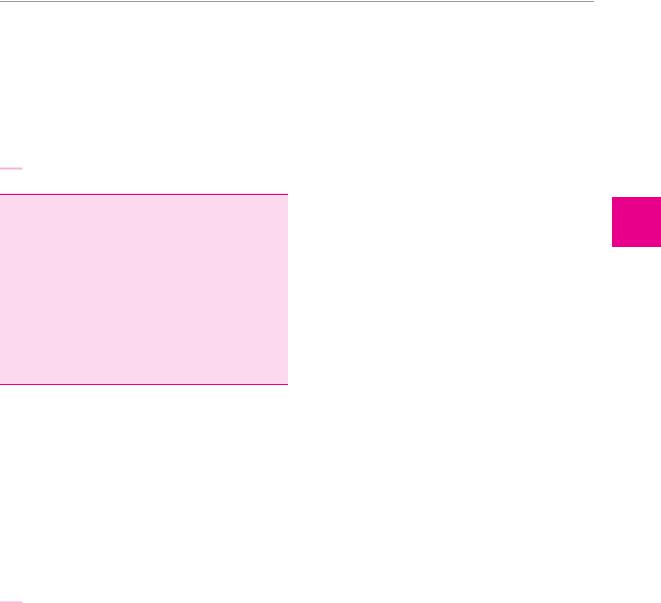
Skull radiographs are performed for very few purposes nowadays and are hardly ever indicated. (They cannot be used as a substitute for CT in head trauma; if a CT is indicated, but unavailable for some reason, then the patient should probably be transported to a center where a CT can be performed.) Plain films of the skull enable visualization of:
fractures (though much less well than on CT, see Fig. 4.1),
congenital malformations of the bony skull, and
various developmental disorders.
Skull radiographs are useless in the diagnostic evaluation of headache or intracranial processes.
Plain radiographs of the spine are sometimes useful for the demonstration of:
fractures,
bony tumors (which, however, are more easily seen by CT or MRI—cf. Fig. 4.2),
degenerative diseases and slippage (olisthesis) of the spine,
infections involving bone,
axial skeletal deformities,
dynamic abnormalities (abnormal mobility or instability of individual spinal segments; their demonstration requires special radiological techniques, socalled “functional studies”).
Most findings of these types, with the notable exception of dynamic spinal abnormalities, can be more readily seen in a CT or MRI scan.
adfsköb
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme
adköb
All rights reserved. Usage subject to terms and conditions of license.
4
Ancillary Tests
46 4 Ancillary Tests in Neurology
a
a |
b |
Fig. 4.2 Chordoma of the T7 vertebral body in a 48-year-old woman. a The spinal cord is posteriorly displaced and compressed. b An image in the frontal plane after the administration of contrast
Computed Tomography (CT)
Technique. CT yields horizontal (axial) sectional images in which the bone and soft tissues are well seen. The images can also be digitally reconstructed in other planes if desired. The technique of CT involves a rotating roentgen ray beam that penetrates the tissue from many different directions. In older CT machines, each plane of section was scanned individually by the rotating beam; in the current generation of scanners, multiple beams travel in a continuous spiral. The beam is attenuated to different degrees by tissues of different radiodensities
Fig. 4.1 Skull fracture seen in a plain skull radiograph. The a−p (a) and p−a (b) images both reveal a fracture line medial to the lambdoid suture on the right (arrow).
b
c
medium shows the tumor compressing the spinal cord from both sides. c At the level of the tumor, the subarachnoid space is completely obliterated by tumor.
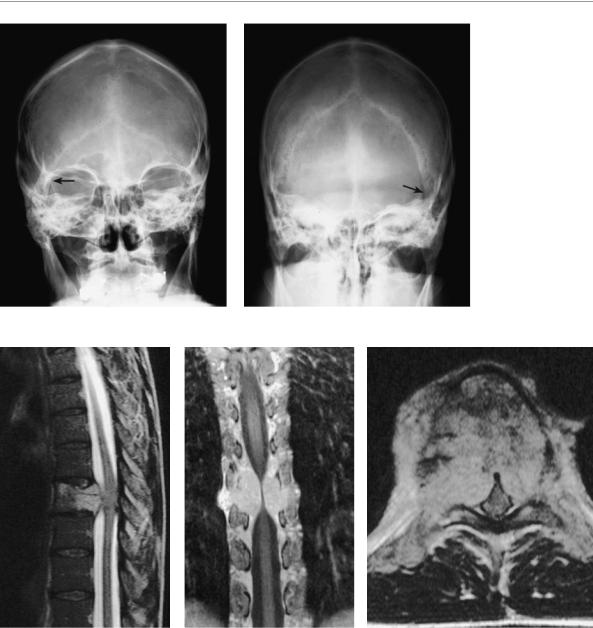
and its amplitude after attenuation is measured by a circular array of detectors and amplifiers. From the resulting pattern of attenuation, the radiodensity at each location in the interior of the brain can be calculated (for example, at each of 512 × 512 pixels; this requires highly specialized computer software). Finally, a visual image is created in which the radiodensity at each location in the tissue is depicted on an analogue gray scale. Different types of tissue have different radiodensities and therefore appear distinct in the CT image (Fig. 4.3). Blood vessels, too, can be visualized.
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme All rights reserved. Usage subject to terms and conditions of license.
Imaging Studies 47
Fig. 4.3 Normal CT scan of the head. a Note the symmetrical, normal-sized frontal and occipital horns of the lateral ventricles. The cerebral cortex and deep white matter can be distinguished from each other, and the falx cerebri can be seen in both the frontal and occipital regions. A number of blood vessels can be seen. Also note the bilateral calcifications of the choroid plexus of the lateral ventricles. b Some of the blood vessels around the base of the brain (arrows) are well seen after the administration of contrast medium.
a |
b |
|
|
|
Spiral CT. As mentioned above, the latest generation of |
Table 4.1 Comparative indications of CT and MRI of the head |
|||
scanners uses one or more roentgen ray beams rotating |
|
|
|
|
Location and type of pathology |
CT |
MRI |
||
in a spiral, i. e., the roentgen ray tube(s) swivels around |
||||
|
|
|
||
Brain atrophy |
+++ |
+++ |
||
the patient’s head while the table is slowly advanced, at |
||||
constant velocity. The resulting spiral data set is numeri- |
Acute infarct |
++ |
+++ |
|
cally converted into axial sections. This technique short- |
Older infarct |
++ |
+++ |
|
ens the time required for each scan and thereby reduces |
Lacunar state |
+++ |
+++ |
|
the radiation load to the patient. It also enables three-di- |
Intraparenchymal hemorrhage |
++ |
+++ |
|
mensional reconstruction of bony structures, as shown in |
Subarachnoid hemorrhage |
+++ |
+ |
|
Fig. 4.4. The administration of intravenous contrast me- |
||||
Aneurysm |
+ |
++ |
||
dium increases the sensitivity and specificity of CT scan- |
||||
Venous thrombosis |
+ |
+++ |
||
ning: penetration of contrast medium into brain tissue |
||||
Brain tumor (cerebral hemispheres) |
++ |
+++ |
||
(contrast enhancement) indicates disruption of the |
||||
Pituitary tumor |
+ |
+++ |
||
blood−tissue barrier or the blood−CSF barrier. Blood ves- |
||||
sels can also be selectively imaged (CT angiography). |
Brain metastases |
+++ |
+++ |
|
Each CT examination is associated with a radiation |
Carcinomatous meningitis |
− |
++ |
|
load to the patient roughly equaling that of a conven- |
Hydrocephalus |
+++ |
+++ |
|
tional chest radiograph. CT is less expensive than MRI. |
Traumatic brain injury |
+++ |
++ |
|
The comparative indications and advantages of these |
Acute subdural or epidural hematoma |
+++ |
+ |
|
two techniques are presented in Table 4.1. |
Meningoencephalitis |
++ |
+++ |
|
|
||||
|
Abscess |
++ |
+++ |
|
|
Parasitic cyst(s) |
+ |
+++ |
|
|
Arachnoid cyst |
++ |
+++ |
|
|
Posterior fossa |
+ |
+++ |
|
|
Pathology of the white matter |
+ |
+++ |
|
|
Multiple sclerosis |
− |
+++ |
|
|
Atlanto-occipital joint |
+ |
+++ |
|
|
Skull lesions |
+++ |
+ |
|
|
|
|
|
|
Fig. 4.4 Three-dimensional reconstruction of the cervical spine by spiral CT (gyroscan; courtesy of PD Dr. H. Spiess, Neuroradiological Institute, Talstrasse, Zurich, Switzerland).
adfsköb
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme
adköb
All rights reserved. Usage subject to terms and conditions of license.
4
Ancillary Tests
48 4 Ancillary Tests in Neurology
Magnetic Resonance Imaging (MRI) |
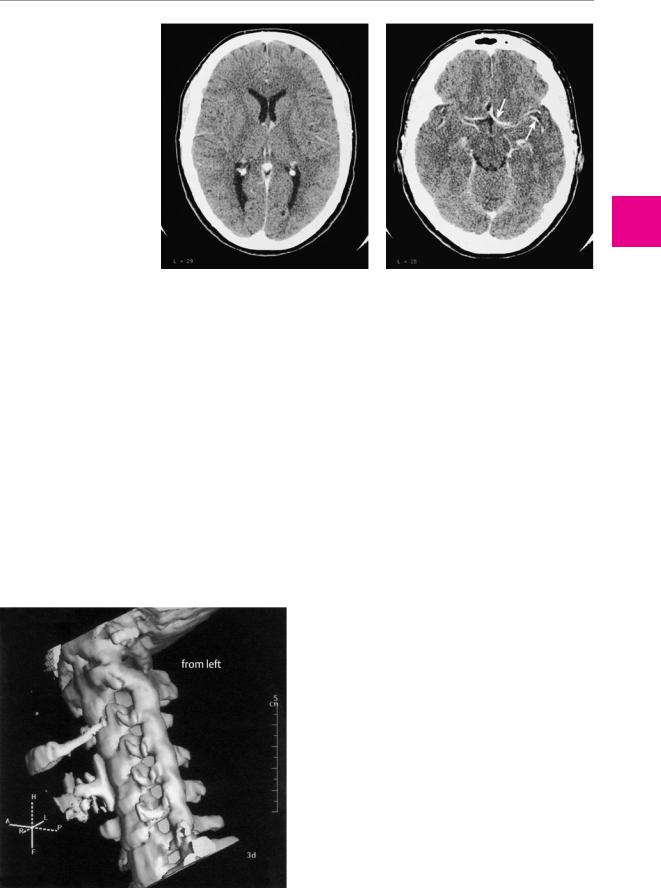
field like a compass needle (Fig. 4.5). When the protons |
MRI is a cross-sectional imaging technique that does not |
in a particularly bodily tissue are oriented in this way, |
and then excited with a radiofrequency pulse at a partic- |
|
rely on the use of ionizing radiation. |
ular frequency (the resonance or Larmor frequency), |
Technique. The underlying physical principles of MRI |
they will take on energy and reorient themselves op- |
posite the field. Once the exciting pulse is switched off, |
|
are as follows: the most common atomic nuclei in all tis- |
the protons release the energy that they previously ab- |
sues of the body are hydrogen nuclei (protons). They are |
sorbed as they return to their original orientation. The |
positively charged and possess an intrinsic magnetic |
released energy can be detected with a radio antenna or |
property known as “spin,” which can be imagined as a |
coil and is the magnetic resonance signal. The signals |
rotation of the proton around its own axis. Each proton |
from different points in a slab of tissue are distinguished |
thus has its own, small magnetic field. A proton to which |
from one another by means of gradient fields, i. e., |
an external magnetic field is applied orients itself in the |
smaller magnetic fields overlying the main field. The MR |
a |
b |
B0 |
|
|
|
|
|
|
|
|
|
Excitatory radio |
|
|
|
|
|
|
wave pulse |
|
|
|
E |
|
|
|
|
c |
|
|
|
|
|
|
T1 increase |
|
|
|
|
|
|
Signal |
|
|
|
|
|
|
90 ° pulse |
|
|
|
|
|
|
0 |
40 |
80 |
500 |
1000 |
1500 |
2000 |
|
T2 decrease |
|
|
|
ms |
|
|
|
|
|
|
||
Fig. 4.5 Physical principles of magnetic resonance imaging |
two tissue-specific constants called T1 and T2. c After the 90° exci- |
(after Edelmann and Warach). a The magnetic axes of the protons |
tatory pulse is delivered, the protons precess in the transverse |
are randomly distributed over space. b If a magnetic field B0 is ap- |
plane. They are in phase at first, and therefore give off a maximally |
plied to the protons, they align themselves either parallel or anti- |
intense signal. Very small inhomogeneities of the magnetic field |
parallel to the field. A proton aligned parallel to B0 has a lower |
make the protons precess at slightly different speeds, resulting in |
energy than one aligned antiparallel to it; therefore, most protons |
“dephasing” and loss of signal intensity. This process, which takes |
have a parallel alignment at first. If radio waves of a specific |
only a few milliseconds, is called T2 relaxation. The MR signal is usu- |
frequency (the Larmor frequency) are now applied, protons can ab- |
ally measured during T2 relaxation. The restoration of magnetiza- |
sorb the energy they need to “flip” from the lower-energy to the |
tion parallel to B0 is a somewhat slower process, called T1 relaxation. |
higher-energy state, thereby becoming antiparallel to the field B0. |
A number of techniques (e. g., gradient echo, spin echo) are used to |
The flipped protons then gradually return to the parallel, lower- |
generate the largest possible MR signal. |
energy state (relaxation). The speed of relaxation is determined by |
|
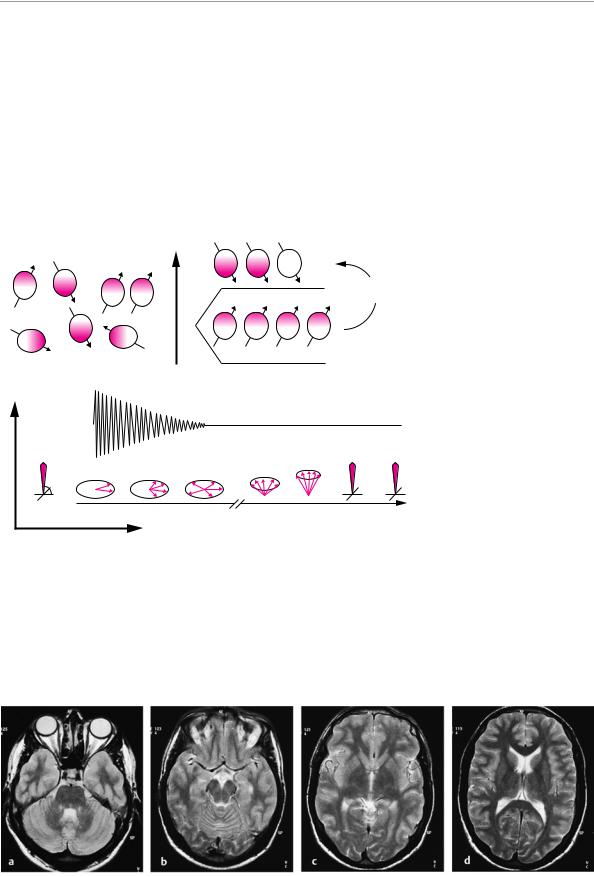
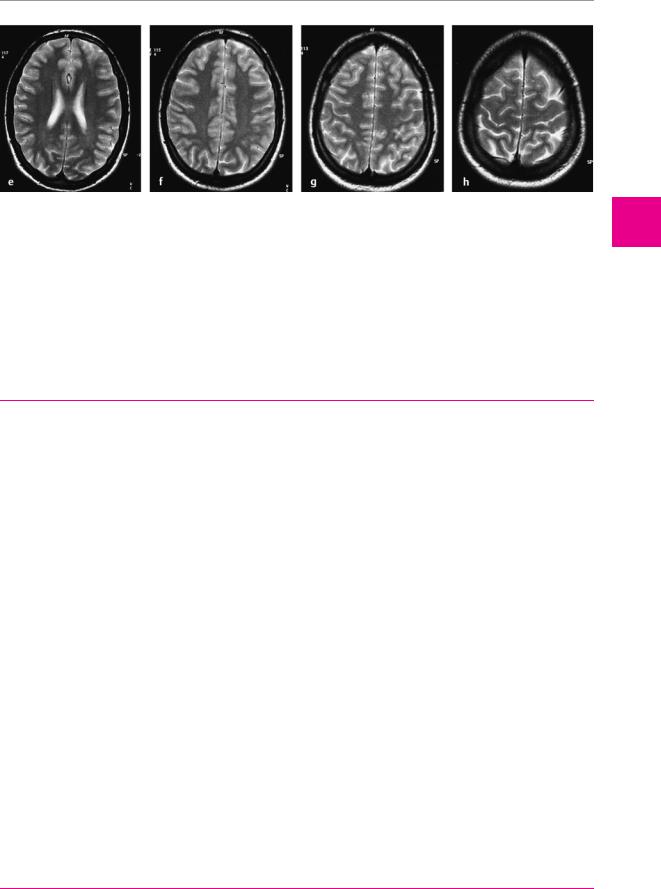
Fig. 4.6 a−h Normal MRI of the brain in 5 mm sections from the base of the brain to the vertex.
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme All rights reserved. Usage subject to terms and conditions of license.
Imaging Studies 49
Fig. 4.6 e−h
image is a gray-scale map of the different intensities of MR signal coming from the tissue (Fig. 4.6) and can be computed in any desired plane of section. Gadolinium− DTPA can be given intravenously as a contrast medium for MRI.
The MR signal intensity of tissue is a function of its local physical and chemical properties, which determine, for example, the length of time that the hydrogen nuclei need to return to their initial orientation (T1 and
T2 relaxation times). The signal intensity is further influenced by the technical parameters of the scanner (e. g., the strength of the applied magnetic field and the frequency of the emitted impulses). The MRI signal characteristics of various normal and pathological tissues in the brain are listed in Table 4.2.
MR angiography. When the spin-echo technique is used in MRI scanning, flowing blood gives rise to a signal
Tabelle 4.2 MRI signal intensities of normal and abnormal structures (after Edelmann)1
Tissue |
T1-weighted image |
T2-weighted image |
Cerebrospinal fluid |
Dark |
Very bright |
Brain |
|
|
White matter |
Bright |
Slightly dark |
Gray matter |
Slightly dark |
Slightly bright |
MS plaque |
Intermediate to dark |
Bright |
Bland infarct |
Dark |
Bright |
Tumor/metastasis |
Dark |
Bright |
Meningioma |
Intermediate |
Intermediate |
Abscess |
Dark |
bright |
Edema |
Dark |
Bright |
Calcification |
Intermediate or bright |
Intermediate or dark |
Fat |
Very bright |
Intermediate to dark |
Cyst |
|
|
Containing mostly water |
Dark |
Very bright |
Containing proteinaceous fluid |
Intermediate to bright |
Very bright |
Containing lipids |
Very bright |
Intermediate to dark |
Bone |
|
|
Cortical bone |
Very dark |
Very dark |
Yellow bone marrow |
Very bright |
Intermediate to dark |
Red bone marrow |
Intermediate |
Slightly dark |
Bone metastasis |
|
|
Lytic |
Dark |
Intermediate to bright |
Sclerotic |
Dark |
Dark |
Cartilage |
|
|
Fibrous |
Very dark |
Very dark |
Hyaline |
Intermediate |
Intermediate |
Intervertebral disk |
|
|
Normal |
Intermediate |
Bright |
Degenerated |
Intermediate to dark |
Dark |
Muscle |
Dark |
Dark |
Tendons and ligaments |
|
|
Normal |
Very dark |
Very dark |
Inflamed |
Intermediate |
Intermediate |
Torn |
Intermediate |
Bright |
Continued
adfsköb
Mumenthaler / Mattle, Fundamentals of Neurology © 2006 Thieme
adköb
All rights reserved. Usage subject to terms and conditions of license.
4
Ancillary Tests
