
5 курс / Пульмонология и фтизиатрия / Clinical_Tuberculosis_Friedman_Lloyd_N_,_Dedicoat
.pdf
300 Tuberculosis and Human Immunodeficiency Virus Coinfection
136.Goosby E, Jamison D, Swaminathan S, Reid M, and Zuccala E. The Lancet Commission on tuberculosis: Building a tuberculosis-free world. Lancet 2018;391(10126):1132–3.
137.Sinha P, Shenoi SV, and Friedland GH. Opportunities for community health workers to contribute to global efforts to end tuberculosis. Global Public Health., 2020, 15:3, 474–84.
138.Moll A, Choi K, Shenoi SV, and Friedland GH Community-based TB case finding and IPT referrals from alcohol venues in rural South Africa. 50th Union World Conference on Lung Health, Hyderbad, India, 2019.
139.Howard AA, and El-Sadr WM. Integration of tuberculosis and HIV services in sub-Saharan Africa: Lessons learned. Clin Infect Dis. 2010;50(Suppl 3):S238–44.
140.Theron G, Jenkins HE, Cobelens F, Abubakar I, Khan AJ, Cohen T, and Dowdy DW. Data for action: Collection and use of local data to end tuberculosis. Lancet 2015;386(10010):2324–33.
141.Naidoo P, Theron G, Rangaka MX, Chihota VN, Vaughan L, Brey ZO, and Pillay Y. The South African Tuberculosis Care Cascade: Estimated Losses and Methodological Challenges. J Infect Dis. 2017;216(Suppl_7):S702–S13.
Книга в списке рекомендаций к покупке и прочтению сайта https://meduniver.com/

16
Drug-Resistant Tuberculosis
KEERTAN DHEDA, ALIASGAR ESMAIL, ANZAAN DIPPENAAR, ROBIN WARREN, JENNIFER FURIN, AND CHRISTOPH LANGE
Introduction |
301 |
Clinical and molecular epidemiology |
302 |
Diagnosis of MDR-TB and resistance beyond MDR-TB |
304 |
Management of MDRand resistance beyond MDR-TB |
307 |
Person-centered care for DR-TB: Human rights, treatment support, and palliative care |
316 |
Research priorities and conclusion |
317 |
References |
317 |
INTRODUCTION
Tuberculosis (TB) is far from eradicated and remains the foremost single infectious disease killer worldwide.1 TB has killed almost a billion people in the last two centuries and remains out of control in Africa and many parts of Asia. Multidrug-resistant TB (MDR-TB: resistance to rifampicin and isoniazid), and resistance beyond MDR-TB (additional resistance to fluoroquinolones, and other second-line drugs [SLIDs], including injectable drugs) is subverting TB control in several parts of the world through increased mortality and diversion of scarce resources, thus marginalizing TB treatment programs. In 2017 the World Health Organization (WHO) reported that the estimated burden of MDR or rifampicin-resistant TB was 560,000 cases.1 Notably, there has been a spike in the detection of TB over the last several years in several high-burden countries including the Russian Federation, South Africa, Congo, India, and China.1–3 Consequently, the estimated burden of MDR-TB had grown dramatically in terms of the absolute number of cases (from 450,000 cases in 2012 to 660,000 cases in 2016).1,3,4 The trend is in keeping with the overall global increase in the burden of antimicrobial resistance (AMR) in general, i.e., to bacteria, fungi, and viruses. Indeed, it is estimated that by 2050 AMR will result in 10 million deaths annually and will cost the global economy up to $100 trillion.5 A major contributor to this estimate is drug-resistant TB (DR-TB). Despite the advent of newer drugs, MDR-TB and resistance beyond MDR-TB have been superseded by programmatically incurable TB.
It is critical to prioritize interventions against DR-TB because of its ability to cripple and undermine current programs. MDRand resistance beyond MDR-TB are associated with considerable morbidity,1,6,7 high mortality (30%–50%, and
thus worse than most cancers),7–9 and have a deleterious impact on health-care worker recruitment in TB-endemic countries,7,10 and are extremely costly to the program and to the country. For example, in South Africa in 2012, DR-TB was already consuming 40% of the total TB resources despite forming less than 5% of the total TB case burden.11 A recent global KPMG report suggested that, in parallel with other African countries, South Africa’s GDP was probably impacted by 2%–3% due to TB, equating to US$10 billion per annum.12 Thus, TB and DR-TB have had a massive impact on economic growth, and any cost-effectiveness or affordability of interventions must be interpreted in context.
Encouragingly, there have been a number of advances in new drugs and diagnostic technologies after a dearth of almost 40 years. The term “XDR-TB” (extensively drug-resistant TB) has become a misnomer as SLIDs are no longer part of the frontline regimen (though they may still be useful in selected situations), and a revision of the nomenclature is required.13 Perhaps, in the future “XDR-TB” will likely be defined by resistance to key sec- ond-line drugs including a combination of fluoroquinolones, linezolid, and bedaquiline.
This chapter adopts a clinical perspective and focuses on the clinical and molecular epidemiology, diagnosis, and clinical management of DR-TB. A patient-centered and human rights approach to treatment is also discussed. There are several other important aspects of DR-TB including disease pathogenesis, drug-specific pharmacokinetic and pharmacodynamic aspects, treatment of MDR-TB in children, transmission of MDR-TB, and major research priorities for MDRand resistance beyond MDR-TB. However, these have recently been covered in detail elsewhere7 and will not be discussed further due to space constraints. Thus, their exclusion here does not undermine their critical importance in the DR-TB landscape.
301

302 Drug-Resistant Tuberculosis
CLINICAL AND MOLECULAR
EPIDEMIOLOGY
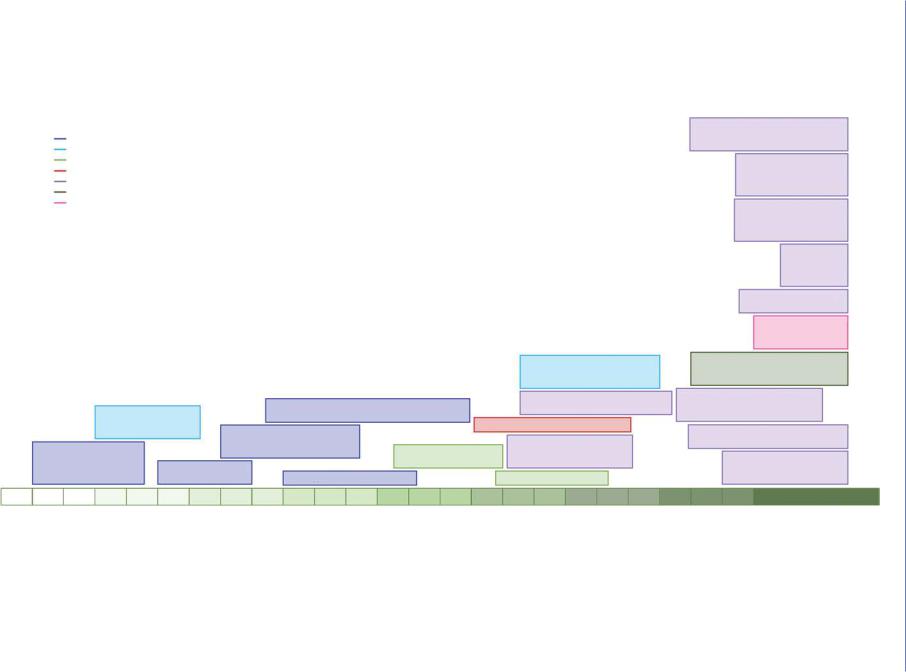
Molecular epidemiology has played an important role in advancing our understanding of DR-TB epidemics (Figure 16.1 and Table 16.1). First, on a population-based level, strain typing provides a means of identifying chains of transmission and providing an indication of how well TB control programs function with respect to transmission control.1,14,15 Second, on a patient level, strain typing may determine the mechanism whereby DR-TB develops in an individual.16–19 Third, DNA sequencing, as a molecular tool, increasingly plays a role in the identification of drug resistance in clinical isolates.20–23
Numerous molecular epidemiologic studies have conclusively demonstrated that DR-TB is transmitted,15,17,24–30 albeit to different degrees.31 On a population level DR-TB develops through:
(i) primary infection with a drug-resistant strain32 (including reinfection with a drug-resistant strain during/after treatment for drug-susceptible TB),16,17,19,33 or mixed infection with a drugsusceptible and drug-resistant strain with unmasking of the drugresistant strain during treatment for drug-susceptible TB,16 or (ii) acquisition of resistance during therapy.34–37 It is estimated that95% of MDR-TB occurring in new TB cases and 60% in previously treated cases are due to transmission.38 This contrasts with previous beliefs that suggested that DR-TB was mainly acquired during antibiotic treatment (secondary resistance) and that acquisition of resistance had a fitness cost that limits transmissibility.39 The restoration of a fitness deficit due to a drug-resistant mutation is thought to occur through epistatic interactions with compensatory mutations in genes encoding in the same or linked pathway(s).40–42 For example, compensatory mutations of rifampicin conferring resistance mutations in rpoB have been described
in rpoA and rpoC.25,28,41,43
Molecular epidemiology is now entering a new era where nextgeneration whole-genome sequencing (WGS) is replacing IS6110 DNA fingerprinting,44 MIRU-VNTR (mycobacterial interspersed repetitive unit-variable number tandem repeat) typing,45,46 and spoligotyping47 due to its superior resolution to study transmission dynamics7,48–52 (Table 16.1). Deciphering DR-TB transmission remains crucial for the optimization of local and global control measures and the early detection of MDR and XDR outbreaks.53–55 Furthermore, the resolution of WGS now provides the opportunity to link genome variants with pathobiology and drug resistance, thereby ensuring a better understanding of factors that drive the DR-TB epidemic as well as providing information to optimize therapy through genetic drug susceptibility testing (DST).53,56,57
WGS-based phylogenetic analysis has also enabled the study of the chronology in which resistance is acquired,25,27,35,58–61 and the factors influencing the emergence of drug resistance.36,62 Analysis of the LAM4 clone (Tugela Ferry, South Africa) from the first XDR-TB outbreak reported in 200615 suggested that development of XDR-TB in KwaZulu-Natal had its roots in drug resistance that arose in the late 1950s, that isoniazid was the first drug resistance acquired, and that MDR-TB emerged in the 1980s, soon after the introduction of rifampicin.27 Drug resistance is thus driven by cycles of de novo drug resistance acquisition, often due
to ineffective treatment regimens,62 diversification, clonal spread, and amplification of resistance.27 Clones of genetically distinct strains have now evolved to become the dominant circulating DR-TB strains in defined geographical regions that may persist for decades, as observed in Eastern Europe,25,63,64 Portugal,65 South Africa,58,66,67 and South America.59 WGS will further provide the opportunity to longitudinally measure the impact of policy changes (shortened treatment regimens68 and implementation of new and repurposed drugs69,70) on the trajectory of current DR-TB epidemics, emergence of drug resistance,35 and past failures of TB control programs. Indeed, it was shown that the mismanagement of even a single TB patient can lead to a public health crisis.71,72
WGS is now being used to measure the contribution of transmission driving DR-TB epidemics and in so doing is questioning whether the high resolution of WGS alters our current understanding, which is based on other traditional genotyping techniques.48 However, interpretation of these early studies is reliant on ill-defined thresholds used to delineate transmission.29,73,74 Importantly, these studies have concluded that determining the direction of transmission is difficult within the context of institutional or household settings where strain diversity is minimal.75 Similarly, defining transmission chains in endemic settings will be dependent on the evolutionary rate, which may be strain dependent.76,77 If the genome of a strain remains stable over many years, this may explain the absence of a direct correlation between clustering (transmission) and epidemiologic links between patients. An alternative explanation is that casual contact is the driver of transmission.78 The slow evolutionary rate and ability of the bacterium to exist in a dormant state for many years in an individual after initial infection before progressing to disease (known as latent TB) further complicates determining the directionality of transmission.
Despite these limitations, WGS has provided novel insights into mechanisms driving resistance through reinfection,48,79–82 transmission,29,30,54,63,73,77,78,83–85 spread of specific drug-resistant strains,29,30,54,59,74 fatal nosocomial transmission,86 and incorrect classification of the pathogen causing disease87 in various global settings.
The global DR-TB epidemic continues to be exacerbated by the movement of people with infectious DR-TB (Figure 16.2),88–96 which can now be monitored through WGS of the infection-caus- ing Mycobacterium tuberculosis strains. These studies show that refugees fleeing from conflict and poverty in high DR-TB incidence countries, or seeking an education, are introducing DR-TB into low incidence settings.83,88–90,93,96,97 This has prompted the development of assays, based on WGS data, to screen populations at risk of having been exposed to DR-TB in their country of origin, i.e., Russian sex workers in Spain.97
Understanding intra-country/community transmission will be critical for directing resources to identified infectious sources and transmission “hot spots,”88,98 which can now be achieved by combining WGS with geographic information systems (GIS) coordinates.98 Application of this methodology in South Africa has highlighted the large distance between place of residence and the treatment facility, thereby suggesting how DR-TB can spread through public transport networks ultimately leading to endemic resistance beyond MDR-TB.98,99
Книга в списке рекомендаций к покупке и прочтению сайта https://meduniver.com/
IS6110 restriction fragment length polymorphism
Targeted gene sequencing
Spoligotyping
MIRU-VNTR typing
Next-generation whole genome sequencing (WGS)
Targeted next-generation sequencing
Targeted deep next-generation sequencing
|
|
|
|
Heteroresistance explains |
|
|
|
|
|
discordance between genotype |
|
|
|
|
|
and phenotype |
|
|
|
Additional epidemiological mechanisms leading |
Identification of compensatory |
||
Association between |
mutations in rpoA and rpoC |
||||
|
to DR-TB |
|
|||
mutation and drug |
|
XDR-TB in Portugal |
|||
Exogenous reinfection with an |
|
||||
resistance |
|
|
Whole genome sequencing |
||
Exogenous reinfection with |
|
MDR-TB strain in immune- |
|
||
|
competent patients |
XDR-TB outbreak in |
used to erentiatedi |
||
an MDR-TB strain in an |
|
||||
Transmission of |
South Africa |
acquisition from transmission |
|||
immune-compromised |
|||||
|
|
||||
patient |
MDR-TB |
Genotypic classification of DR-TB |
Totally DR TB in Iran |
||
Online next-generation sequencing analysis tools for lineage and DR prediction
Discordance between epidemiological contact and genetically defined contact
Statistical association between chromosomal mutations and resistance phenotype
Regimen dependent acquisition of DR-TB
XDR-TB transmission in South Africa
Cryptic minor drug resistance causing mutations
Detection of mutations conferring resistance by targeted nextgeneration sequencing
Whole genome sequencing identifies transmission of DR-TB in Russia
Rapid detection of drug resistance causing mutations by WGS
Chronology of mutational events leading to the evolution of XDR-TB
1993 |
1994 |
1995 |
1996 |
1997 |
1998 |
1999 |
2000 |
2001 |
2002 |
2003 |
2004 |
2005 |
2006 |
2007 |
2008 |
2009 |
2010 |
2011 |
2012 |
2013 |
2014 |
2015 |
2016 |
2017 |
2018 |
Figure 16.1 Timeline of key molecular epidemiological findings using different genotyping tools. Different colors indicate genotyping tools used for each finding. MDR, multidrug resistant; MIRU-VNTR, mycobacterial interspersed repetitive unit-variable numbers of tandem repeats; XDR, extensively drug-resistant (though this term will likely be redefined soon); DR, drug resistant; TB, tuberculosis. (Adapted from Dheda K et al. Lancet Respir Med. 2017.)
303 epidemiology molecular and Clinical

304 Drug-Resistant Tuberculosis
Table 16.1 Molecular epidemiological genotyping methods |
|
|
|
Method/technique |
Advantages |
Disadvantages |
Applications |
Insertion sequence 6110 |
High discriminatory index |
Requires culture and DNA |
Identification of transmission |
restriction fragment length |
|
extraction; cannot differentiate |
chains, and temporal |
polymorphism44 |
|
between drug-sensitive and |
changes in the strain |
|
|
drug-resistant strains; not directly |
population, reinfection, and |
|
|
comparable between labs |
strain migration |
Spacer oligonucleotide typing47 |
Direct genotyping of clinical |
Low discriminatory index; |
Classification of strains |
|
specimens; relatively |
undergoes homoplasy; cannot |
according to lineages, |
|
inexpensive; requires few |
differentiate between drug- |
reinfection, and strain |
|
laboratory resources |
sensitive and drug-resistant strains |
migration |
Mycobacterial interspersed |
Direct genotyping of clinical |
Undergoes homoplasy; cannot |
Identification of transmission |
repetitive unit-variable number |
specimens; high discriminatory |
differentiate between drug- |
chains, and temporal |
tandem repeat |
index; global reference |
sensitive and drug-resistant strains |
changes in the strain |
(MIRU-VNTR)65,68,261 |
database |
|
population, reinfection, and |
|
|
|
strain migration |
Targeted Sanger sequencing20,72 |
Direct genotyping of clinical |
Information limited to nucleotide |
Identification of mutations |
|
specimens; relatively |
variants in a selected set of genes; |
conferring resistance |
|
inexpensive |
limited or no strain typing |
|
|
|
information |
|
Targeted deep |
Direct genotyping of clinical |
Information limited to nucleotide |
Identification of mutations |
sequencing110–112,262,263 |
specimens |
variants in a selected set of genes; |
conferring resistance and |
|
|
no strain type information; more |
heteroresistance |
|
|
expensive; requires high-level |
|
|
|
laboratory infrastructure |
|
Whole-genome |
Comprehensive analysis of the |
Requires culture (or specimen |
Identification of transmission |
sequencing23,49,57,73,101,102,105,264–266 |
genome of the pathogen |
enrichment); more expensive; |
chains, mutations conferring |
|
|
might be computationally |
resistance, heteroresistance |
|
|
demanding or complex |
(low resolution), mixed |
|
|
|
infections, specimen |
|
|
|
heterogeneity, and |
|
|
|
intrapatient evolution |
The phenomenal resolution of WGS also promises to revolutionize the diagnosis of DR-TB.23,100–103 Guidelines are now being developed on how to interpret WGS data to guide drug choices and to individualize treatment.23,101,104 A number of countries have initiated WGS for both diagnosis and epidemiological surveil- lance.23,80,85,101,102,105–108 Furthermore, it is now possible to use WGS to study the natural history of intrapatient evolution of drug resistance by simultaneously monitoring the sequences of multiple genes conferring resistance.62,109 However, numerous limitations still exist for the translation of genotypic data into its phenotypic consequences. To address this, large studies (Comprehensive Resistance Prediction for Tuberculosis: An International Consortium [CRyPTIC] and the Relational Sequencing TB Data Platform [ReSeqTB]) have been initiated to establish associations between genotype and phenotype using WGS and culture-based DST.
An alternative to WGS is targeted next-generation deep sequencing.110,111 This method allows variants to be detected in minor M. tuberculosis populations, termed heteroresistance. This has allowed researchers to find resistance at a frequency below the classical 1% proportion method. It is envisaged that targeted deep sequencing may be a replacement for culture-based DST. It also has the potential to identify resistance earlier, thereby allowing
researchers to get a greater understanding of the biology of the evolution of drug resistance. An added advantage is the potential for clinical decisions to be made earlier and for treatment regimens to be individualized based on the comprehensive drug resistance profile of the M. tuberculosis isolate infecting the patient, but exactly how this should be implemented remains unclear.110,112 However, the limited number of genetic targets being evaluated currently precludes targeted deep sequencing as a method to study the epidemiology of DR-TB.
DIAGNOSIS OF MDR-TB AND
RESISTANCE BEYOND MDR-TB
The emergence and spread of DR-TB is responsible for destabilizing TB control in high-burden countries.1,7 Improving TB diagnostics has the potential to improve patient outcomes,113–116 limit the emergence of resistance,116,117 and restrict the transmission of DR-TB.118 However, only two-thirds of the estimated 10 million cases of TB are diagnosed each year and only one-third of the bacteriologically confirmed TB patients are evaluated with phenotypic DST for first-line drugs.1 The net effect of these “mistreated cases” on transmission is evidenced in countries such as Russia,
Книга в списке рекомендаций к покупке и прочтению сайта https://meduniver.com/

Diagnosis of MDR-TB and resistance beyond MDR-TB 305
(a)
(b)
Figure 16.2 Inter-country and intra-country spread of DR-TB according to M. tuberculosis genotype. (a) Worldwide spread of drug-resis- tant strains of M. tuberculosis. Red = Beijing strain.64,94,97,267–274 Green = LAM9 strain.275 Light blue = Haarlem1 strain.276 Purple = T1 strain.277 Orange = S strain89 Dark blue = untyped strains.96,278–280 (b) Ongoing intra-country spread of XDR-TB strains in South Africa. Red = atypical Beijing strains. Green = LAM4 strain.281,282 Intra-country spread has also been reported in Portugal65 and Spain.283 (Adapted from Dheda K et al. Lancet Respir Med. 2017.)
Ukraine, and Belarus where over 25% of the MDR-TB burden is attributed to person-to-person transmission.1 This phenomenon is partly responsible for the predicted rise in DR-TB rates highburden countries.119
Phenotypic DST
Phenotypic DST involves incubating a bacterial isolate (grown from a clinical specimen) in the presence and absence of a specific drug and comparing its growth. This method is often the benchmark against which other tests are measured as it directly measures growth and is not reliant on proxies of resistance such as genetic mutations. However, discrepancies between methods are not uncommon and it has been suggested that for rifampicin, genotypic analysis may offer a more reliable reference standard in some contexts but not in others.120–122 Furthermore, technical difficulties and inconsistent results are common for some drugs.
The first DSTs were developed and validated for solid culture using Lowenstein Jensen slopes or agar plates. However, more rapid commercial versions such as the Bactec MGIT 960 System (Becton Dickinson) are now routinely available, where results may be obtained in 7–12 days.123 Alternative low-cost DST methods have also been developed that utilize titer plates, microscopic observation of colonies or oxidation–reduction dyes to indicate
growth of bacteria.123,124 In some circumstances, the minimal inhibitory concentration (MIC) corresponding to resistance is not confidently known and, in these cases, clinicians may choose to treat patients with a higher dose of a particular drug (e.g., isoniazid and moxifloxacin).123,125,126
The main disadvantage of using phenotypic testing is the time taken to obtain a result which can range from 3 to 6 weeks, depending on the resources available.127 This, coupled with demanding technical and infrastructural requirements, makes phenotypic DSTs less useful for patient management except in situations where determination of MICs is required as is the case for low-level fluoroquinolone resistance.126,128 Another disadvantage of phenotypic DST is that hetero-resistant populations are difficult to quantify using the commonly implemented methods.
Genotypic testing
Mutations in the mycobacterial DNA can render bacilli resistant to the action of specific anti-tuberculous drugs. Small nucleotide polymorphisms (SNPs) in genes encoding for drug targets or enzymes are a frequent cause of resistance, although insertions and deletions can also occur.129,130 The loci implicated in M. tuberculosis resistance have been summarized previously.7 Resistance to rifampicin is mainly is due to alteration in the DNA-dependent

306 Drug-Resistant Tuberculosis
RNA polymerase which is encoded by rpoB.131 Genotypic markers of resistance in the 81 bp rifampicin resistance determining region (RRDR) have a high sensitivity and specificity,132 resulting in the wide-spread implementation of genotypic rifampicin resistance screening in high TB burden countries.
The main advantage of screening for genotypic markers of resistance is that it is rapid since it does not rely on mycobacterial growth and can go from “specimen in” to “result out” in a few hours. Theoretically this means that patients could present to the clinic, be correctly diagnosed, and be started on effective treatment in a single clinical encounter.128
Xpert MTB/RIF is a commercially available quantitative realtime NAAT (nucleic acid amplification test) that diagnoses TB and rifampicin resistance in less than 2 hours.133 It is an automated, cartridge-based system that can be performed in resourced decentralized locations, outside of reference laboratories and by staff with minimal laboratory training.133 It has been widely validated, is endorsed by the WHO134 and the US Federal Drug Administration (FDA)135 for the initial diagnosis of TB and for the diagnosis of MDR-TB (based on rifampicin resistance), and is increasingly being deployed in high-burden countries. A metaanalysis has reported the sensitivity and specificity for rifampicin resistance to be 95% and 98%, respectively.136 A new version of the Xpert MTB/RIF (resistance to rifampin) assay cartridge called the Xpert MTB/RIF Ultra was released in 2016. This assay includes multicopy insertion sequence targets (IS6110 and IS1081) which, together with an improved sample volume, allow improved sensitivity in the detection and the differentiation of the M. tuberculosis complex.137 The new cartridges have decreased run-time and improved chemistry, and use probe-based high-resolution melt to determine drug resistance. Its main added value is in the detection of TB in patients with smear negative disease where an increase in sensitivity of 13% is achieved compared to the Xpert G4 cartridge.137 Furthermore, Xpert Ultra, based on one preliminary study, may be useful in the diagnosis of TB meningitis when including trace results138 though further data are awaited. Data on its use in other pauci-bacillary compartments are lacking. A new, point-of-care, portable, battery-operated Xpert Omni platform will likely become available late 2020. This device will use the Xpert Ultra cartridge and will allow for the detection of M. tuberculosis and determination of rifampicin resistance in remote locations. Xpert Omni may also prove to be a valuable tool for active case finding.139
There are several drawbacks of the Xpert MTB/RIF system. First, it does not detect isoniazid resistance; one in seven TB isolates worldwide is isoniazid mono-resistant (almost a third of TB cases in Eastern Europe).140,141 Thus, many cases could potentially receive a suboptimal regimen (and effective monotherapy in the continuation phase), which may lead to poor patient outcomes and amplification of resistance.140 Second, there is a significant false-positive rate for rifampicin resistance in settings with a low prevalence of MDR-TB. However, data on this is conflicting. For example, empiric evidence from Brazil (MDR-TB prevalence 1%) has suggested the false-positive rates are low when used in programmatic settings (positive predictive value [PPV]90%).142 Last, the assay has a high false-positive rate in patients with a previous history of TB.137 This could potentially lead to the
overtreatment of patients, unnecessarily exposing them to drug toxicity. Collectively, these data suggest that Xpert MTB/RIF may be used as a baseline assay for the diagnosis of TB in most settings. However, clinicians should be aware of the limitations of these assays.
LINE PROBE ASSAYS
Empiric MDR-TB treatment is usually initiated based on an Xpert MTB/RIF result in many high-burden countries like South Africa. However, confirmatory DST for firstand second-line drugs is subsequently performed using phenotypic DST, or often, using a line probe assay (LPA). LPA technology amplifies the target gene of interest followed by the reverse hybridization of the amplicons to a series of oligonucleotide probes immobilized on a membrane.143 Several assays are available but the most widely used is the Hain GenoType MTBDRplus VER 2.0 which detects rifampicin and isoniazid resistance, and the Hain GenoType MTBDRsl VER 2.0 which detects fluoroquinolone and aminoglycoside resistance (Hain Lifescience, Germany).144,145 The Hain MTBDRplus can be performed with reasonably high sensitivity and specificity directly on sputa or on a culture isolate.41,42 It detects rifampicin and isoniazid resistance with a sensitivity of 97.7% and 95.4%, respectively, and a specificity of 91.8% and 89.0%, respectively, using smear positive sputum samples.146,147 However, its accuracy for detecting rifampicin resistance may be lower in smear negative disease, with sensitivity and specificity of only 77.8% and 97.2%, respectively.147
A Cochrane systematic review showed that the Hain MTBDRsl assay (version 1.0) had a sensitivity and specificity of 85.1% (95% CI: 71.9, 92.7) and 98.2% (95% CI: 96.8, 99.0), respectively, for the detection of fluoroquinolone resistance using smear positive sputum. The performance was similar in culture isolates with a sensitivity and specificity of 83.1% (95% CI: 78.7, 86.7) and 97.7% (95% CI: 94.3, 99.1), respectively.148 However, in smear negative samples, the sensitivity was significantly lower at 20.0% for the detection of ofloxacin resistance compared to 85.1% in smear positive samples.146,149 Indeterminate rates for the detection of fluoroquinolone resistance using MTBDRsl is lower when performed on culture isolates than in smear positive sputum and smear negative sputum (0.2% vs. 1.9% vs. 5.1%).146,149
For combined SLID (amikacin, kanamycin, and capreomycin) resistance, the sensitivity and specificity of Hain MTBDRsl is 94.4% (95% CI: 25.2, 99.9) and 98.2% (95% CI: 88.9, 99.7), respectively, when performed on smear positive sputa. However, the sensitivity of MTBDRsl in smear negative sputa was significantly lower at 37.0% for amikacin compared to 94.4% in smear positive samples. The performance of MTBDRsl in detecting SLID resistance on culture isolates is best for amikacin 87.9% (95% CI: 82.1, 92.0) compared to capreomycin 79.5% (95% CI: 58.3, 91.4) or kanamycin 66.9% (95% CI: 44.1, 83.8) but retains high specificity for all three injectable drugs (combined SLID specificity of 99.5% [95% CI: 97.1, 99.9]). Indeterminate results for the detection of SLID resistance are lower when performed on culture isolates than in smear positive sputum and smear negative sputum (0.4% vs. 6.1% vs. 13.5%).146,149,150
In summary, LPAs have the potential to rapidly detect MDR-TB and resistance beyond MDR-TB, enabling clinicians to initiate
Книга в списке рекомендаций к покупке и прочтению сайта https://meduniver.com/

Management of MDRand resistance beyond MDR-TB 307
appropriate treatment timeously. However, the performance of Hain MTBDRsl in smear negative sputum has suboptimal sensitivity for the detection of fluoroquinolone and SLID resistance, which is 20%–30% with indeterminate rates of 5%–10%.146 Thus, a negative LPA test result should prompt the clinician to further confirm susceptibility by phenotypic DST.151
Next-generation WGS
Sequencing has the potential to provide a comprehensive genotypic DST. It facilitates the crafting of individualized treatment regimens, which are more likely to result in cure.152 However, the clinical impact of this strategy in different settings remains to be established. Targeted next-generation sequencing (NGS) (sequencing of specific genes amplified by polymerase chain reaction [PCR]) is more sensitive and allows for the detection of resistance conferring mutations in sputum samples (see Figure 16.3). It also has the additional advantage of detecting, otherwise undetectable, micro-heteroresistance (emerging low-level drug-spe- cific resistant populations) at diagnosis and during the course of treatment.
Patients with rifampicin resistance detected on Xpert MTB/ RIF Ultra usually receive empiric MDR-TB treatment. However, even with regimen modification guided by the LPAs, inadvertent amplification of resistance is promoted due to suboptimal performance of LPA. This would likely be minimized with WGS or targeted NGS, as resistance to multiple drugs are simultaneously detected, thus facilitating precision medicine.129 However, wide-spread clinical implementation of NGS is dubious since the
Bacterial DNA extracted and purified.
M. tuberculosis-specific DNA levels in sputum is below the detection limit of the assay (<1% of sputum DNA from a TB patient’s sputa is mycobacterial in origin) and, currently, this test can only be reliably performed on DNA extracted from cultured isolates. The turnaround time for obtaining NGS results may be reduced by the use of “early positive” cultures (2–7 days), though further data about the utility of this approach are awaited.153 Mutations associated with high confidence drug-specific resistance (including those that portend lowand high-level resistance) have been outlined in detail elsewhere.7
In summary, the main advantage of sequencing is its potential for facilitating individualized, effective treatment for patients with DR-TB. However, to achieve this in a clinically useful way, targeted NGS or WGS would need to be performed “directly” on a sputum sample (rather than DNA extracted from a culture isolate) thus allowing for rapid and precise treatment initiation and minimizing the time of exposure of patients to inappropriate empiric regimens. A comparison of WGS with currently available drug resistance tests is presented in Table 16.2.
MANAGEMENT OF MDRAND
RESISTANCE BEYOND MDR-TB
Medical management of MDR-TB
The management of MDRand resistance beyond MDR-TB is complex, and the type of treatment regimen and package chosen will depend on a number of considerations including HIV status,
Library prepared of |
Sequencing: amplification |
short DNA fragments |
and assembly with multiple |
labeled and tagged. |
reads giving coverage across |
|
the whole genome. |
WGS Result
RIF-R
INH-R
EMB-R
FQL-R
Mtb lineage 2.2.1 seen before
Patient management. |
MTB in silico profile. |
CCATTGCATTGAACCTGA
Alignment to reference genome or de novo assembly to give the genetic code (genome).
Identification of known drug resistance and strain-type mutations in the sample’s genome.
MTB mutations library
Figure 16.3 Next-generation sequencing. With small bacterial genomes such as M. tuberculosis multiple samples can be analyzed within a single run, greatly reducing costs. (Reproduced with permission from Lancet Respir Med 2017.)
308 Drug-Resistant Tuberculosis
Table 16.2 Summary comparison of WGS with current drug resistance tests |
|
|
||
Test characteristic |
Phenotypic tests |
Xpert MTB/RIF |
Line probe assays |
Whole-genome sequencing |
Time to result |
Slow (weeks/months) |
Less than 2 hours |
Rapid (hours/days) |
Rapid (hours/days) if |
|
|
|
when performed |
performed directly from |
|
|
|
directly from samples |
samples |
Sensitivity for detecting |
Sensitivity high |
High for rifampicin, |
Sensitivity limited |
Sensitivity dependent on |
resistance |
|
zero for other drugs |
|
knowledge of polymorphisms |
Resistance levels |
Ability to determine MICs |
Does not assess MIC |
Limited ability to |
Ability to predict some MICs |
|
|
|
predict MICs |
|
Safety |
High safety concerns |
Low safety concerns |
Reduced safety |
Reduced safety concerns |
|
|
|
concerns |
|
EQA |
Quality assurance via WHO/ |
Limited quality |
Limited quality |
Quality assurance schemes |
|
IUATLD reference lab |
assurance schemes |
assurance schemes |
not available |
|
network |
|
|
|
Efficiency |
Separate tests for each drug |
Detects resistance |
2–3 drugs per test |
Single analysis for all drugs |
|
|
to one drug only |
|
|
Source: Reproduced with permission from Dheda K et al. Lancet Respir Med. 2017;5:291–360.
CD4 count, degree of organ dysfunction (e.g., renal, liver, etc.), presence of comorbidities, history of previous TB, age, disease severity, the local drug susceptibility profile, resource availability, and access to supportive care, amongst others. Optimal regimen selection for MDRand resistance beyond MDR-TB is a rapidly changing landscape with the emergence of newer drugs; there are many ongoing clinical trials evaluating new drug combinations and these have been outlined in detail elsewhere.7 Regimens will also evolve with changing resistance patterns. Thus, clinicians need to be aware of local resistance patterns and the status of access to newer and repurposed drugs. While the focus here is on regimen selection, there are other quintessential aspects of management that include well-functioning laboratories for bacteriological studies and DST, infection control in health-care facilities to minimize transmission, availability, and access to adherence promoting mechanisms, attention to psychosocial factors and financial/resource assistance to patients, access to quality drugs and distribution systems, appropriate training of healthcare workers, good systems processes and information systems (to track patients, communicate results, and audit data), and a robust and well-functioning TB program (NTP).
While there are different perspectives about the merits of an empiric PAN TB regimen without the need for prior susceptibility testing, we take the view that this approach is not sustainable nor in the best interests of patients; rather, we subscribe to and support a concept of individualized therapy and precision medicine. Thus, as much information as possible should be obtained through rapid molecular testing in order to, at the least, quasiindividualize regimens. Thus, rifampicin-resistant readouts (typically from Xpert MTB/RIF Ultra in many TB-endemic countries) should be confirmed and clarified with molecular readouts (e.g., LPAs) and extended phenotypic DSTs. Typically, such readouts are obtained within 3–7 days of using LPA (e.g., the Hain MTBDRplus and sl assay, though other platforms are available). Using such an approach it is feasible to rule-in resistance beyond MDR-TB in a substantial majority of cases within 7–10 days.132,154–158 Indeed, this approach is the standard of care in South Africa where sputum from patients with rifampicin-resistant TB is subjected to
Hain MTBDRplus and sl assays. The reality, however, is that in some parts of the country the LPA results are only available in 2–4 weeks, and yield in smear negative patients is lower, limiting the usefulness of the assay. Nevertheless, using this approach ensures that susceptibility to rifampicin, isoniazid, fluoroquinolones, and SLIDs will be ascertained fairly rapidly, as will readouts for ethionamide and high-dose isoniazid (based on the inhA and katG mutations). Phenotypic DST will still be required given the suboptimal sensitivity and indeterminate rates when using sputumbased LPA testing (discussed in the diagnostics section). Using this approach, resistance profiles for drugs like pyrazinamide, ethambutol, and bedaquiline will still remain unknown (at least given the current format of the LPAs). Although next-generation WGS readouts may address these deficiencies to some extent, the major challenge (as already discussed) is that the results are only available after 6–8 weeks making this a user-unfriendly tool at present, as the lack of a rapid readout fails to prevent resistance amplification. Technology is evolving, but it will take another 5–10 years before WGS directly from the sputum will likely be optimized. However, even with comprehensive WGS readouts, phenotypic susceptibility testing will still be required for drugs such as clofazimine, cycloserine, PAS (para-aminosalicylic acid), and carbapenems. Thus, for the foreseeable future, we will need to rely on a combination of genotypic and phenotypic DST to construct optimal regimens.
The principles to medically managing MDRand resistance beyond MDR-TB are outlined in Table 16.3. Essentially, a partindividualized and part-empiric MDR-TB regimen should be constructed based on the initial molecular readouts (as outlined earlier) that should comprise a backbone of bedaquiline, fluoroquinolone, and linezolid (group A drugs; see Table 16.4 for the WHO classification of second-line drugs).159 Other drugs that should likely be added to the regimen after this first step, depending on the DST readouts, would include clofazimine and cycloserine (group B drugs) that will likely make up the five-drug regimen. In the patient meta-analysis, the group A drugs were all associated with substantial mortality reduction (>50%) and treatment success benefit, while the group B drugs showed similar effects but
Книга в списке рекомендаций к покупке и прочтению сайта https://meduniver.com/

Management of MDRand resistance beyond MDR-TB 309
Table 16.3 Recommended principles to be used when designing a regimen for the medical management of MDR-TB and resistance beyond MDR-TB including in those with pulmonary TB, extra-pulmonary TB, and in children
•Route of administration: Use an all oral regimen (asee note later on WHO-recommended Bangladesh-like shorter course regimen).
•Number of drugs: Ideally use five drugs (minimum four) to which the strain has proven or likely susceptibility (drugs previously taken for
≥1 month are generally avoided); use at least three (preferably four) likely effective drugs in the continuation phaseb.288
•Individual components of the regimen:
i.Use a backbone of the three Group A drugs, i.e., a later-generation fluoroquinolone, e.g., levofloxacin (less QT prolongation), linezolid, and bedaquiline.288 Actively monitor for toxicity especially to linezolid ( 30% reduce the dose or stop the drug).289–291 The optimal duration of individual drugs like linezolid and bedaquiline remains unclear but they are generally used for at least 6 months (in practice extension of bedaquiline to ≥ 9 months may be undertaken, particularly late culture converters and those with poor prognostic features).
ii.Add additional Group B drugs (e.g., cycloserine/terizidone, and/or clofazimine).
iii.Add additional Group C drugs, if necessary (based on toxicity and resistance profiles), so that five likely effective drugs make up the regimen.
•Duration of treatment: The optimal duration of the multidrug regimen remains unclear. Current practice when treating MDR-TB (using a Group A backbone) varies from 9 to 11 months (e.g., in South Africa) to the WHO-recommended 18–20 months. The optimal duration of treatment will depend on several factors including mycobacterial burden (and time of culture conversion), disease extent, comorbidities (e.g., HIV and diabetes), previous treatment, country setting, local resistance profiles, and patient preference.292
•Empiric versus individualized: To optimize outcomes and prevent resistance amplification, and loss of newer drugs, drug susceptibilityguided treatment for individual drugs is preferred over empiric treatment regimens. To minimize resistance amplification sputum-based genotypic testing for second-line resistance, particularly FQs, is recommended. Regimens should be further optimized based on drug susceptibility results when they become available.
•Delamanid (Group C) can be used together with bedaquiline, if required, to make up the five-drug regimen (monitor QT interval).293,294
•Meropenem or imipenem/cilastin should be administered with clavulanic acid (generally given as oral Augmentin).
•A second-line injectable drug (amikacin or streptomycin; Group C drugs) may be used if an appropriate regimen of four to five likely effective drugs cannot be constructed, provided baseline and follow-up screening for hearing loss and renal toxicity is accessible. We recommend that an intravenous catheter be used for the administration of amikacin and/or a carbapenem. If inaccessible we recommend that amikacin be given intramuscularly together with a local anesthetic agent.295
•Psychosocial, adherence, and financial support are critical elements of the treatment package.
•Patients should be actively monitored for adverse drug reactions, which are common.296
•A single drug should not be added to a failing regimen.
•The HIV status should be determined, and ART initiated in all HIV-infected patients (within 8 weeks; 2 weeks in advanced HIV).
•Surgical intervention may be offered in appropriate patients who have failed treatment or are at high risk of relapse.
•Children: Use the same principles as outlined previously. Bedaquiline can be used from 6 years of age. Delamanid is safe and effective from 3 years of age and prioritized in children. Lack of optimal diagnostics, and child-friendly formulations remain a major challenge.297
•aWHO-recommended shorter course regimen (9–11 month Bangladesh-like regimen containing amikacin but not containing bedaquiline or linezolid): While scale up of newer drugs and diagnostics continues, as an interim option, this regimen can be used on a discretionary basis provided there is no proven or likely resistance to any component of the regimen (except isoniazid), there is access to baseline and longitudinal monitoring for hearing loss, and FQ and SLID resistance have been excluded.159,165 There should be clear plans to transitioning to an oral Group A-based regimen.
Source: Adapted with permission from Dheda K. Lancet, 2016; Dheda K. Lancet Resp Med, 2017.
Abbreviations: FQ, fluoroquinolone; MDR-TB, multidrug-resistant TB.
aSee main text for the composition of WHO-recommended shorter course regimen.
bContinuation phase: Some Group A drugs like bedaquiline and/or linezolid may only be given for a limited period (e.g., 6 months) and thus the period beyond this point may only contain a limited number of drugs. Depending on the length of the regimen and how long each drug is used, in specific instances, there may not be a continuation phase.
reduced in magnitude. Group C drugs did not demonstrate a mortality benefit or data were unavailable.
The optimal duration of linezolid (2–3 vs. ≥6 months) remains unclear. Several other drugs are generally not counted as representing part of the five likely effective drugs. Indeed, in countries like South Africa, there is a 50% rate of isolate-specific resistance to pyrazinamide and ethambutol in patients with MDR-TB. The rates of isoniazid resistance are region-dependent; for example, in South Africa 40% have inhA promoter mutations, and 60% of isolates harbor katG mutations, while in Eastern Europe the KatG mutation accounts for over 90%, thus conferring high-level
resistance to isoniazid.160,161 Thus, ethionamide resistance levels in these, and several other settings, is high (50%–90%); high-dose isoniazid is often used at 10 mg/kg to limit toxicity (resulting in suboptimal drug levels and doubtful effectiveness) and levels are further marginalized in those with high acetylator status. Thus, molecular readouts like the LPA are only a guide and may have limited PPV in the clinical setting. Although the shorter course WHO regimen recommends that both high-dose INH and ethionamide be used concurrently, we recommend that only one of the drugs be used depending on the inhA or katG mutation available from molecular testing. When using high-dose INH, a dose of
