
новая папка / Apley 938-988
.pdf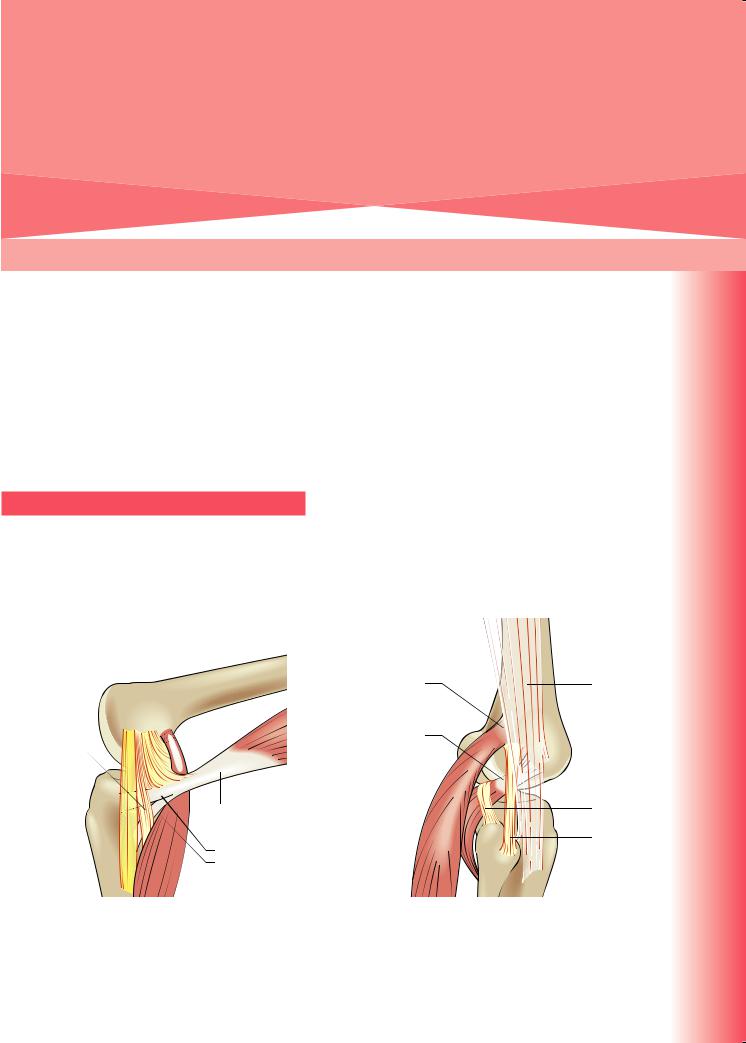
Injuries of the knee |
31 |
and leg |
|
|
|
Nick Howells
The knee is a complex joint which is vulnerable to injury. The bony structure of the knee joint is inherently unstable; were it not for the strong capsule, intraand extra-articular ligaments and controlling muscles, the knee would not be able to function effectively as a mechanism for support, balance and thrust (Figure 31.1, and see below). The tibia is also particularly vulnerable to injury: because of its subcutaneous position, it is more commonly fractured, and more often sustains an open fracture, than any other long bone.
KNEE LIGAMENT INJURIES
Mechanism of injury and pathological anatomy
Most ligament injuries occur while the knee is bent because the capsule and ligaments are relaxed and the
Posterior oblique ligament including the superficial arm
Superficial |
|
|
|
Semimembranosus |
medial |
|
|
|
including |
collateral |
|
|
|
capsular, |
ligament |
|
|
|
anterior and |
|
||||
|
|
|
|
inferior arms |
|
|
|
|
Gastrocnemius |
|
|
|
|
(a)
femur is allowed to rotate on the tibia. The damaging force may be a straight thrust such as a dashboard injury forcing the tibia backwards or, more commonly, a combined rotation and thrust as in a football tackle.
Injuries of the knee ligaments are common, particularly in sporting pursuits but also in road accidents, where they may be associated with fractures or dislocations. They vary in severity from a simple sprain to complete rupture. The direction and nature of the force will directly influence the structure or structures injured. It is important to recognize that these injuries are seldom ‘unidirectional’; they often involve more than one structure and it is therefore useful to refer to them in functional terms (such as ‘anteromedial instability’) as well as anatomical terms (such as ‘torn medial collateral ligament (MCL)’).
The cruciate ligaments provide both anteroposterior and rotary stability. They also help to resist
Lateral gastrocnemius
tendon Iliotibial tract
Popliteus tendon
Popliteofibular ligament
Fibular collateral ligament
(b)
Figure 31.1 Extracapsular restraints to valgus and varus stresses on the knee (a) Restraints on valgus stresses: the deep and superficial parts of the medial collateral ligament, semimembranosus and the posterior oblique ligament. (b) Extracapsular restraints on varus stresses: lateral collateral ligament, popliteus tendon, popliteofibular ligament and the capsule.

3
TRAUMA
excessive valgus and varus angulation. Both cruciate ligaments have a double bundle structure. The fibres within each bundle are arranged in such a way that at any position of knee flexion some of the fibres are taut. The anterior cruciate ligament (ACL) has anteromedial and posterolateral bundles, whereas the posterior cruciate has anterolateral and posteromedial bundles. Anterior displacement of the tibia (as in the anterior drawer test) is resisted by the anteromedial bundle of the ACL, while the posterolateral part tightens as the knee extends. Posterior displacement is prevented by the posterior cruciate ligament (PCL), specifically by the anterolateral bundle when the knee is in near 90 degrees of flexion and by the posteromedial bundle when the knee is straight (Figure 31.2).
Valgus stresses are resisted by the superficial and deep layers of the medial collateral ligament, semimembranosus tendon and its expansions, the tough posteromedial part of the capsule (referred to as the posterior oblique ligament) as well as the cruciate ligaments (Figure 31.1a). Depending on the position of the knee, some will act as primary and others as secondary stabilizers. At 30 degrees of flexion, the MCL is the primary stabilizer.
The main checks to varus angulation are the iliotibial band and the lateral (fibular) collateral ligament (LCL). Structures forming the posterolateral corner of the knee also make an important contribution to stability; they comprise the popliteus tendon and the popliteofibular ligament in addition to the LCL (Figure 31.1b). The iliotibial band and LCL are the primary stabilizers to a varus stress between full extension and 30 degrees of flexion; however, as flexion increases, the LCL relaxes and the posterolateral structures come into play to provide additional stability.
Clinical features
The patient gives a history of a twisting or wrenching injury and may even claim to have heard a ‘pop’ as the tissues snapped. The knee is painful and is usually swollen – and, in contrast to meniscal injury, the swelling appears almost immediately. Tenderness is most acute over the torn ligament, and stressing one or other side of the joint may produce excruciating pain. The knee may be too painful to permit deep palpation or much movement.
Abrasions suggest the site of impact, but bruising is more important and indicates the site of damage. The doughy feel of a haemarthrosis distinguishes ligament injuries from the fluctuant feel of the synovial effusion of a meniscus injury. The entire limb should be examined for other injuries and for vascular or nerve damage.
The most important aspect of the examination is to test for joint stability. Partial tears may permit no abnormal movement, but the attempt can cause pain. Complete tears tend to permit abnormal movement, which sometimes is almost painless.
Anteroposterior stability is assessed first by placing the knees at 90 degrees with the feet resting on the couch and looking from the side for posterior sag of the proximal tibia; when present, this is a reliable sign of posterior cruciate damage (Figure 31.3). Next, the anterior and posterior drawer tests are carried out; a positive drawer sign is diagnostic of a tear, but a negative test does not exclude one. The Lachman test is a more reliable test for AP instability; anteroposterior glide is tested with the knee flexed 15–20 degrees (Figure 31.4). Posterior cruciate ligament insufficiency can be confirmed with a positive quadriceps active test (Figure 31.5b). Rotational stability arising from acute injuries can usually be tested only under anaesthesia. After the
PL
AM
AL
PM
(a) |
(b) |
Figure 31.2 Dual-bundle structure of the anterior and posterior cruciate ligaments (a) The anteromedial (AM) bundle of an anterior cruciate ligament is taut in 90° of knee flexion whereas the posterolateral (PL) bundle tightens in extension. (b) In contrast, it is the anterolateral (AL) bundle of the posterior cruciate ligament that is tight in 90° flexion and the posteromedial (PM) bundle tightens in extension (and therefore resists
914 hyperextension).

Figure 31.3 Posterior cruciate ligament
(a) Viewed from the side, any backwards displacement of the upper tibia is plainly visible and can be confirmed by (b) pushing the tibia backwards.
(a) |
(b) |
(a)
(b) |
(c) |
(a)
Figure 31.5 (a) Testing collateral ligaments. Side-to- side stability of the knee can be checked by holding the foot between the upper arm and body and moving the joint between supporting hands. This method is useful if the leg is large. (b) The quadriceps active test. Note the position of the examiner’s hands in supporting the thigh and resisting knee extension by the ankle. At 90° of knee flexion, a posterior sag caused by a damaged posterior cruciate ligament is corrected when the quadriceps contracts.
acute injury has settled it is possible to perform a pivot shift test for ACL rotatory insufficiency whereby the lateral tibial condyle can be made to sublux forwards as the tibia rotates abnormally around an axis through the medial condyles.
Figure 31.4 Tests for anterior cruciate ligament instability (a) Drawer test: With the knee at 90° and the hamstrings relaxed, grasp the top of the patient’s leg and try to shift it forwards and backwards. (b) Note that there is some anterior shift in this patient when the tibia is pulled forwards - mild anterior cruciate laxity. (c) Lachman test: This is more sensitive than the drawer test. Note the position of the knee and the examiner’s hands. There are modifications to this technique for more cumbersome knees.
Quadriceps contraction
(b)
Sideways tilting (varus/valgus) is examined, first with the knee at 30 degrees of flexion and then with the knee straight (Figure 31.5a). Movement is compared with the normal side. If the knee angulates only in slight flexion, there is probably an isolated tear of
31
leg and knee the of Injuries
915
3
TRAUMA
the collateral ligaments; if it angulates in full extension, there is almost certainly rupture of the capsule and cruciate ligaments as well. See Chapter 20 for more detailed descriptions of knee ligament stability tests.
Imaging
X-rays Plain X-rays may reveal associated fractures to the femoral condyles or tibial plateau in addition to small bony avulsions that can occur in conjunction with a ligament injury.
Bone may be avulsed from the:
•medial epicondyle of the femur at the origin of the MCL (Pellegrini-Stieda lesion)
•tip of the fibula, probably from the LCL or a posterolateral corner injury
•tibial spine at the insertion of the ACL
•central portion of the posterior tibia at the insertion of the PCL
•near edge of the lateral tibial condyle by the iliotibial tract or capsule – this is called a Segond fracture and is associated with an ACL injury.
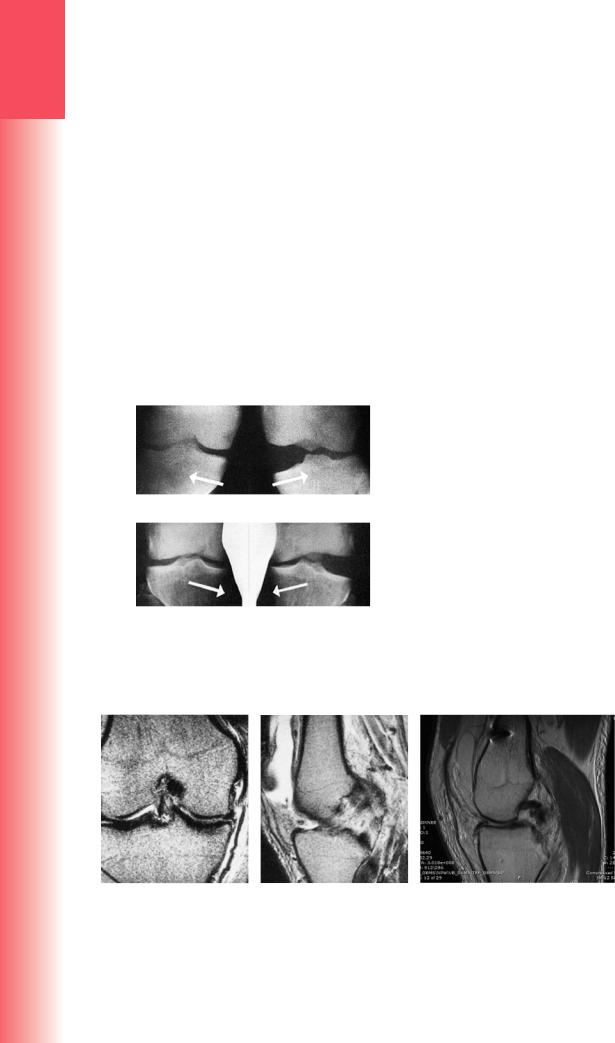
Stress X-rays are useful to document the degree of instability secondary to ligament injury. These can be performed on the table in theatre or in the radiology department. They should be compared to the contralateral limb and are particularly useful in assessing the multiligament-injured knee (Figure 31.6).
Computed tomography CT is useful for the delineation of subtle fractures associated with ligament injuries and to determine exact fracture patterns. This is useful in planning reconstruction. CT is not useful for assessment of ligamentous structures.
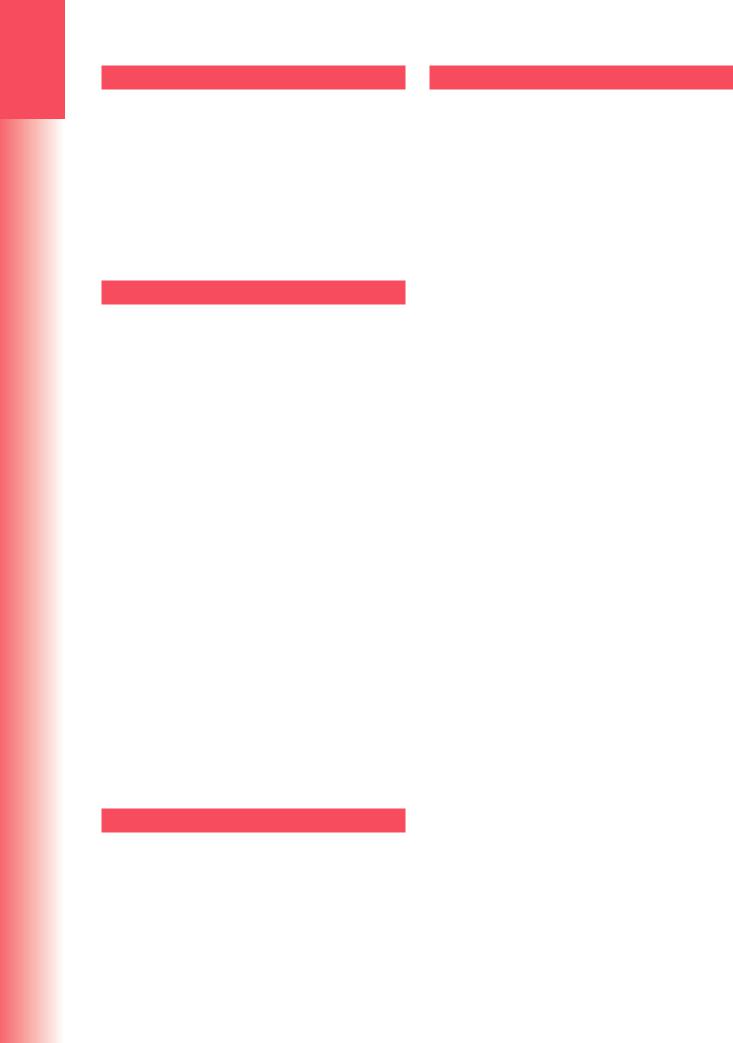
Magnetic resonance imaging MRI is the gold standard imaging tool for the assessment of knee ligament injuries. Increased availability has led to the widespread use of MRI to diagnose ligament, chondral and meniscal injuries, providing almost 100% sensitivity and over 90% accuracy (Figure 31.7).
(a)
(b)
Figure 31.6 Stress X-rays Stress films show: (a) complete tear of medial ligament, left knee; (b) complete tear of lateral ligament. In both, the anterior cruciate also was torn.
ANTERIOR CRUCIATE LIGAMENT INJURY
Clinical features
ACL injuries are one of the most common knee injuries, particularly in women. The classic history is of an axial-loading twisting injury on a slightly flexed knee. This commonly occurs when suddenly changing direction or landing and twisting from a jump in pivoting sports such as football, netball and rugby. Risk factors include joint hypermobility, genetic predisposition, elevated BMI and increased tibial slope. The bleeding associated with ligament rupture will cause an acute haemarthrosis and the patient will describe swelling almost immediately.
It is very rare for the ACL to heal satisfactorily as the synovial fluid present around this intra-articular
(a) |
(b) |
(c) |
Figure 31.7 Torn knee ligaments – MRI (a) Coronal T1-weighted image showing a medial collateral ligament tear with surrounding oedema and joint effusion. (b) Sagittal T1-weighted image showing an intra-substance tear of the anterior cruciate ligament with a large joint effusion. (c) Coronal T1-weighted image showing a PCL
916 rupture.

ligament is thought to prevent formation of a consolidated clot that would promote a healing response in the tendon. In some individuals, however, the knee can stabilize symptomatically and clinically after a period of appropriate rehabilitation.
Treatment
ACL deficiency can be overcome with appropriate quadriceps rehabilitation and conscious control of the knee to minimize sagittal instability. This can allow individuals to return to sport. This does pose a risk, however, as unconscious quadriceps control can seldom be achieved. The potential therefore remains for future pivot instability in an ACL-deficient knee causing subsequent irreversible damage to the chondral and meniscal surfaces of the knee.
The majority of patients who sustain an ACL injury will continue to have demonstrable sagittal plane instability despite rehabilitation. In this situation treatment options consist of activity modification to avoid running, jumping, cutting and side-stepping activity, all of which put an ACL-deficient knee at risk, or surgical reconstruction.
ACL reconstruction is a widely performed operation for patients with persistent symptomatic instability in order to provide a functionally stable knee with reduced potential for secondary injury and long-term morbidity. The goals of ACL reconstruction (ACLR) are to stabilize the knee joint, restore normal kinematics and prevent early-onset degenerative arthrosis. Over the last 25–30 years ACLR techniques have evolved and yielded significant improvements in the clinical outcomes following ACL injury. The goal of modern surgical techniques is an intra-articular anatomical reconstruction in order to restore kinematics to as close to normal as possible. Graft options most commonly used are autologous hamstring tendons (semitendinosus + gracilis) or patella tendon. A number of other autologous, allogeneic and synthetic grafts have been trialled and are used with varying success. Graft should be of sufficient diameter to be strong enough to provide an adequate reconstruction. Four-stranded autologous hamstring grafts are the most commonly used worldwide but these sometimes produce too small a graft in smaller patients and therefore other options also need to be considered. Bony tunnels are drilled in the femur and the tibia within the footprint of the native ACL. The graft is pulled through these tunnels into position, tensioned then fixed to maintain this tension. Various fixation techniques are used but commonly include screws, staples and suspensory devices.
A stepwise structured quadriceps rehabilitation programme is important following surgery, focusing on range of movement, strengthening, proprioception and eccentric control. Patients should be counselled
that return to pivoting sports is not advised for a minimum of 9–12 months. Active injury prevention programmes such as the PEP (Prevent injury and Enhance Performance) programme have been shown to dramatically reduce the risk of both primary ACL injury and re-injury following ACL reconstruction in soccer players. This is a focused series of stretches and muscle warm-up exercises that focus on strength, awareness and neuromuscular control. Well-performed, uncomplicated surgery can yield near-normal knee function at 18 months post surgery. At this stage postop rates of re-injury to the reconstructed knee reach equivalence with injury rates to the contralateral uninjured knee.
POSTERIOR CRUCIATE LIGAMENT INJURY
Clinical features
The PCL is most commonly injured by a direct anterior blow or a rapid deceleration injury such as the knee striking the dashboard in a motor vehicle collision. The initial clinical symptoms are very similar to an ACL injury. PCL rupture is much less common than ACL rupture. The PCL is a much stronger ligament with higher load to failure than the ACL.
Treatment
With appropriate quadriceps rehabilitation, the majority of patients with an isolated PCL injury will return to a high level of function and avoid surgical intervention. Surgical reconstruction of the PCL is generally reserved for patients with marked and persistent instability despite rehabilitation.
BONY ACL/PCL LIGAMENT AVULSIONS
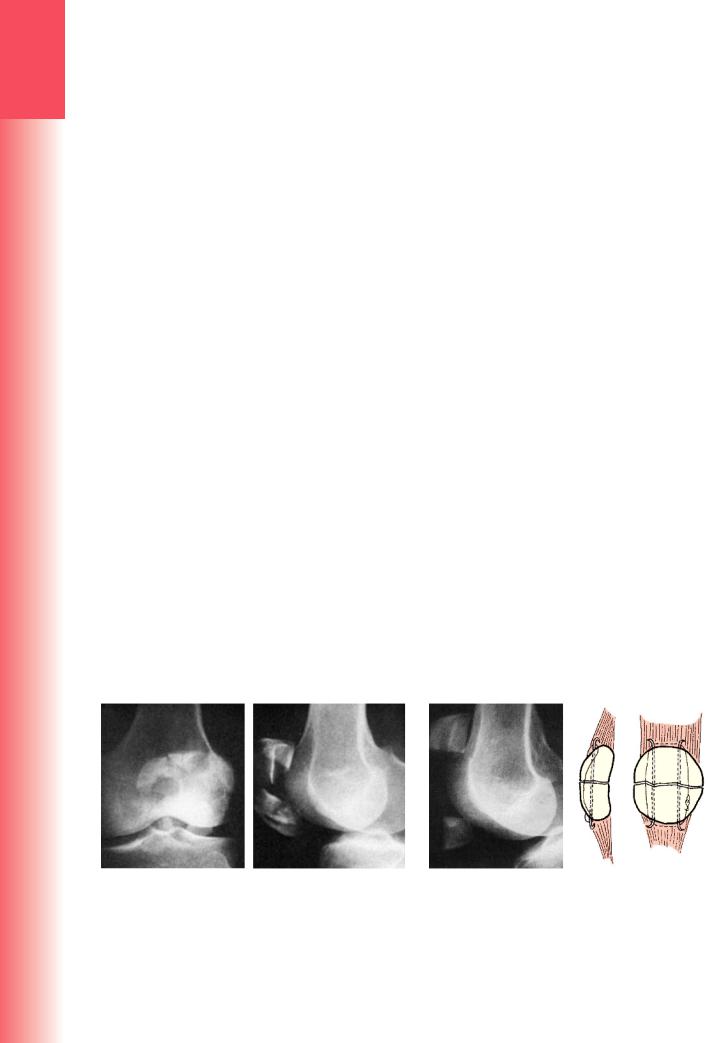
A tibial spine fracture is a bony avulsion of the tibial insertion of the ACL. Often this is a traction type injury and it is seen most commonly in adolescents. The detached bone fragment may remain almost undisplaced, held in position by the soft tissues, it may be partially displaced, the anterior end lifted away on a posterior hinge, or it may be completely detached and displaced. Because the articular surface of the bony fragment is covered with cartilage, which is radiotranslucent, the image seen on radiographs is smaller than the actual fragment (Figure 31.8). CT gives a better impression of fragment displacement and position. MRI identifies any associated ligamentous, chondral or meniscal injuries. PCL bony avulsions are from the central posterior portion of the tibia.
Undisplaced avulsions can be managed nonoperatively in a brace or cast. Displaced ACL and PCL avulsions are best managed with operative reduction and fixation. Both open and arthroscopic techniques
31
leg and knee the of Injuries
917

3
TRAUMA
(a) |
(b) |
(c) |
(d) |
Figure 31.8 Bony avulsion fractures (a,b) AP, lateral X-rays showing a large, displaced avulsion fracture of the tibial spine consistent with a bone ACL injury. This young man injured his knee while playing football. (c,d) AP and lateral X-rays showing a bony avulsion of the PCL.
have been described and are performed depending on fragment size, position and surgeon preference and experience. The fragments are held with screws, anchors or wires. Outcomes are usually good and patients regain good function. However, there is potential for some residual laxity if ligament fibres have been stretched when sustaining the injury.
MEDIAL COLLATERAL LIGAMENT INJURY
Isolated MCL tears are relatively rare. MCL injuries usually occur in conjunction with injuries to other structures, particularly the ACL and medial meniscus. An isolated MCL injury is caused by a purely valgus force. Partial ligament injuries and sprains will tend to stabilize in a brace as the intact fibres splint the torn ones and spontaneous healing will occur. Low-grade fullthickness injuries also have good healing potential with an appropriate bracing regime, which maintains range of motion and full flexion but limits full extension beyond 10 degrees of flexion, as this will prevent undue stress on the healing ligament. Rarely an isolated complete tear will require surgery, most commonly in the form of direct repair. Chronic instability from a missed or inappropriately braced MCL may require surgical reconstruction, although outcomes remain variable.
LATERAL COLLATERAL LIGAMENT INJURY
|
Isolated LCL tears are also rare and result from a |
|
purely varus stress. Careful clinical examination is |
|
required to differentiate an isolated LCL from a more |
|
extensive posterolateral corner (PLC) injury. Isolated |
|
LCL injury can be managed non-operatively with |
|
bracing as for an MCL injury. If there is a bony avul- |
|
sion, this warrants repair and often is an indication of |
918 |
a PLC injury. A PLC injury may benefit from acute |
repair +/– reconstruction. |
KNEE DISLOCATION / MULTILIGAMENT
INJURY
The dislocated knee is an under-diagnosed injury which relies on a high index of clinical suspicion on presentation of any knee injury. Traumatic knee dislocations are uncommon yet serious injuries that historically have had variable prognosis. A knee dislocation describes complete disruption of the integrity of the tibiofemoral articulation (Figure 31.9). Such disruption will result in a multiligament knee injury, defined most commonly as rupture to at least two of the four major knee ligament structures. Half of them are secondary to road traffic accidents (high-velocity dislocations), approximately a third are sports injuries (low-velocity dislocations) and nearly 10% are from simple falls (ultra-low-velocity dislocations).
(a) |
(b) |
Figure 31.9 Knee dislocation X-rays showing an anterior dislocation of the knee.

Clinical features
For an acute dislocation, efficient patient assessment and management according to basic advanced trauma life support (ATLS) principles is the initial priority. A high index of suspicion is required, as a dislocated knee may have reduced spontaneously or may have been reduced before transfer to hospital. Rupture of the joint capsule produces a leak of the haemarthrosis, leading to severe bruising and swelling. The circulation in the foot must be examined because the popliteal artery may be torn or obstructed. Repeated examination is necessary as ischaemia may evolve and compartment syndrome is also a risk.
Acute ischaemia is a surgical emergency and requires in theatre angiography, vascular surgical involvement and revascularization. Subtle suspicion of vascular injury should be investigated with ankle brachial pressure index (ABPI) and vascular imaging such as angiography, CT angiography or MR angiography. ABPI of <0.9 should prompt vascular imaging. Common peroneal nerve injury occurs in nearly 20% of cases; distal sensation and movement should be tested and documented carefully.
Treatment
Should the knee remain dislocated at presentation, it should be reduced under conscious sedation or in the operating theatre as soon as possible and held with brace, plaster or external fixator. This is usually achieved by pulling directly in the line of the leg, but hyperextension must be avoided because of the danger to the popliteal vessels. For the definitive management of the multiligament-injured knee, a non-operative approach was formerly advocated in view of concerns over postoperative stiffness. More recent evidence has, in contrast, shown considerable benefit from surgical treatment in terms of improved functional outcomes, return to work and return to sport. There is increasing consensus that surgical intervention should be
performed early (within 2–3 weeks). A recent systematic review of early versus delayed surgery found significantly better outcomes for early intervention.
A wide variety of surgical techniques have been described in the management of these injuries including primary repair, repair and augmentation, and reconstruction. The important principle is to define the components contributing to the instability and to repair or reconstruct the primary restraints as anatomically and isometrically as possible.
Complications
EARLY
Arterial damage This occurs in 8–14% of patients. Popliteal artery injury causing acute ischaemia needs immediate repair. Delay resulting in an extended warm ischaemic period can result in amputation (Figure 31.10).
Common peroneal nerve injury Nerve injury can result in weak or absent ankle dorsiflexion. Spontaneous recovery is possible if the nerve is not completely disrupted and about 20% of patients with neuropraxia can be expected to improve. If nerve conduction studies or clinical examination show no sign of recovery, a transfer of tibialis posterior tendon through the interosseous membrane to the lateral cuneiform may help restore ankle dorsiflexion.
LATE
Joint instability Mild residual joint instability despite repair and/or reconstruction is common. Appropriately rehabilitated quadriceps muscle can compensate for mild instability and the functional disability is rarely severe.
Stiffness Stiffness due to prolonged immobilization and post-injury scarring is a common problem and it may be more troublesome than instability. Even with early surgical reconstruction, normal knee function is elusive after these severe injuries.
Figure 31.10 Knee dislocation and vascular trauma (a) This patient was admitted with a dislocated knee. After reduction the X-ray looked satisfactory, but the circulation did not. (b,c) An
arteriogram showed vascular cut-off just above the knee; had this not been recognized and treated, amputation might have been necessary.
31
leg and knee the of Injuries
(a) |
(b) |
(c) |
919 |
3MENISCAL INJURIES
|
Meniscal injuries are common occurrences both in |
|
|
isolation and in conjunction with ligament injuries |
|
TRAUMA |
of the knee. The menisci have an important role |
|
in load distribution, stability and articular con- |
||
|
||
|
gruence. Menisci are relatively poorly vascularized |
|
|
structures that receive their blood supply from their |
|
|
periphery. |
|
|
Meniscal injuries are discussed in detail in |
|
|
Chapter 20. |
OSTEOCHONDRAL INJURIES
Patients who have suffered osteochondral injuries give a history of patellar dislocation or a blow to the front of the knee. The joint is swollen and aspiration yields blood-stained fluid mixed with fat globules.
Standard anteroposterior and lateral radiographs seldom show the bony part of the fragment and the deficit from which it arises. MRI imaging is required to delineate the lesion accurately.
Treatment
Small fragments should be removed because they may cause symptoms. Larger osteochondral fragments, and especially those from load-bearing areas, can be reattached with counter-sunk or ‘headless’ small fragment screws if the patient presents early.
Sometimes an area of purely chondral damage is identified on the articular surface that is not amenable to reattachment. For areas less than 15 mm in diameter the current gold standard treatment is arthroscopic trimming of any ragged parts and ‘micro-fracturing’. Micro-fracturing consists of drilling through the crater to stimulate an inflammatory response and produce fibrocartilage. For larger lesions treatment remains more experimental. Techniques available that are associated with successful outcomes include cartilage transplantation techniques, collagen scaffold implantation, autologous chondral transfer, and resurfacing implants.
OSTEOCHONDRITIS DISSECANS
|
Teenagers and young adults who complain of inter- |
|
mittent pain in the knee are sometimes found to have |
|
developed a small segment of osteochondral necro- |
|
sis, usually on the lateral aspect of the medial femoral |
|
condyle. This is probably a traumatic lesion, caused |
|
by repetitive contact with the overlying patella or an |
920 |
adjacent ridge on the tibial plateau. The condition is |
described in Chapter 20. |
PATELLOFEMORAL INJURIES
EXTENSOR MECHANISM INJURIES
Disruption of the extensor apparatus may occur in the quadriceps tendon, at the attachment of the quadriceps tendon to the proximal surface of the patella, through the patella and retinacular expansions, at the junction of the patella and the patellar tendon, in the patellar tendon, or at the insertion of the patellar tendon to the tibial tubercle.
In all but direct fractures of the patella, the mechanism of injury is the same: sudden resisted extension of the knee or (essentially the same thing) sudden passive flexion of the knee while the quadriceps is contracting. The patient gives a history of stumbling on a stair, catching the foot while running, or kicking hard at a muddy football.
The lesion tends to occur at progressively higher levels with increasing age: adolescents suffer avulsion fractures of the tibial tubercle; young adult sportspeople tear the patellar tendon, middle-aged adults fracture their patellae; and older people (as well as those whose tissues are weakened by chronic illness or steroid medication) suffer acute tears of the quadriceps tendon.
QUADRICEPS TENDON RUPTURE
The patient is usually elderly, may have a history of diabetes or rheumatoid disease, or may have been treated with corticosteroids. Occasionally acute rupture is seen in a young athlete. The typical injury is followed by tearing pain and giving way of the knee. There is bruising and local tenderness; sometimes a gap can be felt proximal to the patella. Active knee extension is either impossible (suggesting a complete rupture) or weak (partial rupture). Diagnosis can be confirmed by ultrasound or MRI.
Treatment
PARTIAL TEARS
Non-operative treatment will usually restore function: an extension brace or plaster cylinder is applied, followed by physiotherapy that concentrates on restoring knee flexion and quadriceps strength.
COMPLETE TEARS
Early operation is needed, or else the ruptured fibres will retract and repair will be more difficult. End-to- end suturing can be reinforced by proximal turndown techniques as required. If the tendon has been avulsed from the proximal pole of the patella, it should be reattached to a trough created at that site using longitudinal pull-through sutures through bone tunnels in

the patella. Postoperatively the knee is held in extension in a hinged brace. Early supervised movement through the brace is important to prevent adhesions; limits to the amount of flexion can be controlled through the brace and increased as the repair heals.
‘Chronic’ ruptures (usually the result of delayed presentations or missed diagnoses) are difficult to repair because the ends have retracted. The gap can be closed and residual defects covered with turndown techniques, or augmentation techniques can be used, most commonly using autologous hamstring tendons or synthetic meshes.
The results of acute repairs are good, with most patients regaining full power, a good range of movement and little or no extensor lag. Late repairs are less predictable.
PATELLA TENDON RUPTURE
This is an uncommon injury; it is usually seen in young athletes and the tear is almost always at the proximal or distal attachment of the ligament. There may be a previous history of ‘tendinitis’ and local injection of corticosteroid.
The patient gives a history of sudden pain on forced extension of the knee, followed by bruising, swelling and tenderness at the lower edge of the patella or more distally.
X-rays may show a high-riding patella and a telltale flake of bone torn from the proximal or distal attachment of the ligament.
Ultrasound or MRI will help to distinguish a partial from a complete tear.
Treatment
ACUTE TEARS
Partial tears can be treated by applying an extension brace or plaster cylinder. Complete tears need operative repair or reattachment to bone. Tension on the suture line can be lessened by inserting a temporary pull-out wire or a protective figure-of- eight strong suture to keep the distance between the inferior pole and attachment to the tibial tuberosity constant. Immobilization in full extension may precipitate stiffness – it is, after all, a joint injury – and it may be better to support the knee in a hinged brace with limits to the amount of flexion permitted. This range can be gradually increased incrementally with time.
LATE CASES
Late cases are difficult to manage because of proximal retraction of the patella. A two-stage operation may be needed: first to release the contracted tissues and apply traction directly to the patella, then at a
later stage to repair the patellar tendon and augment it with autologous hamstrings.
Early repair of acute ruptures gives excellent results. Late repairs are less successful and the patient may be left with a permanent extension lag.
PATELLA FRACTURES
The patella is a sesamoid bone in continuity with the quadriceps tendon and the patellar tendon. There are additional insertions from the vastus medialis and lateralis into the medial and lateral edges of the patella. The extensor ‘strap’ is completed by the medial and lateral extensor retinacula (or quadriceps expansions), which bypass the patella and insert into the proximal tibia.
The mechanical function of the patella is to hold the entire extensor ‘strap’ away from the centre of rotation of the knee, thereby lengthening the anterior lever arm and increasing the efficiency of the quadriceps muscles.
The key to the management of patellar fractures is assessment of the state of the entire extensor mechanism.
It is important to remember that if the extensor retinacula are intact, active knee extension is still possible, even if the patella itself is fractured.
Mechanism of injury and pathological anatomy
The patella may be fractured, either by a direct force or by an indirect traction force that pulls the bone apart (and often tears the extensor expansions as well).
Direct injury – usually a fall onto the knee or a blow against the dashboard of a car – causes either an undisplaced crack or a comminuted (‘stellate’) fracture without severe damage to the extensor expansions.
Indirect injury occurs, typically, when someone catches the foot against a solid obstacle and, to avoid falling, contracts the quadriceps muscle forcefully. This is a transverse fracture with a gap between the fragments.
Clinical features
Following one of the typical injuries, the knee becomes swollen and painful. There may be an abrasion or bruising over the front of the joint. The patella is tender and sometimes a gap can be felt. There is an associated haemarthrosis.
X-rays
The X-rays may show one or more fine fracture lines without displacement, multiple fracture lines with irregular displacement or a transverse fracture with a gap between the fragments (Figure 31.11).
31
leg and knee the of Injuries
921
3
TRAUMA
922
Patella fractures are classified as transverse, longitudinal, polar or comminuted (stellate). Any of these may be either undisplaced or displaced. Separation of the fragments is significant if it is sufficient to create a step on the articular surface of the patella or, in the case of a transverse fracture, if the gap is more than 3 mm wide.
A fracture line running obliquely across the superolateral corner of the patella should not be confused with the smooth, regular line of a (normal) bipartite patella. Check the opposite knee; bipartite patella is often bilateral.
Treatment
UNDISPLACED OR MINIMALLY DISPLACED FRACTURES
The extensor mechanism is generally intact and treatment is mainly protective. A plaster cylinder or an extension brace holding the knee straight should be worn for 3–4 weeks, and during this time quadriceps exercises are to be practised every day.
LONGITUDINAL FRACTURES
The extensor mechanism is nearly always intact and the fracture is inherently more stable to early movement. Extension brace or cylinder plaster can be converted to a range of movement brace with incremental increases in movement range usually after 2 weeks.
COMMINUTED (STELLATE) FRACTURES
The extensor expansions are intact and the patient may be able to lift the leg. However, the undersurface of the patella is irregular and there is a serious risk of damage to the patellofemoral joint. Open reduction and fixation is generally advocated. Some small fragments that obviously distort the articular surface may
(a) |
(b) |
be removed but the principle is to restore and hold the articular surface as much as possible. A combination of K-wires, mini fragment screws, cerclage wires or sutures are most commonly employed. A hinged brace is used in extension but can be unlocked for exercises to mould the fragments into position and to maintain mobility (see Figure 31.11).
DISPLACED TRANSVERSE FRACTURES
The lateral expansions are torn and the entire extensor mechanism is disrupted. Operative treatment is essential. Through a longitudinal incision the fracture is exposed and the patella repaired by the tension-band principle. The fragments are reduced and transfixed with two stiff K-wires; flexible wire is then looped tightly around the protruding K-wires and over the front of the patella (Figure 31.12). The tears in the extensor expansions are then repaired. A plaster backslab or hinged brace is worn until active extension of the knee is regained; either may be removed every day to permit active knee-flexion exercises.
Outcome
Patients usually regain good function but, depending on the severity of the injury, there is a significant incidence of late patellofemoral osteoarthritis.
PATELLA DISLOCATION
Because of the offset created by the femoral neck, the knee is normally angled in slight valgus that creates a natural tendency for the patella to pull towards the lateral side when the quadriceps muscle contracts. Lateral deviation of the patella during knee extension is prevented by a number of factors: the patella is seated in the intercondylar groove or trochlea, which has a high lateral ‘embankment’; the force of
(a) |
(b) |
Figure 31.11 Displaced comminuted patella |
Figure 31.12 Fractured patella – transverse The sepa- |
fracture Displacement to the joint surface and |
rated fragments (a) are transfixed by K-wires; (b) mal- |
disruption of the extensor mechanism. |
leable wire is then looped around the protruding |
|
ends of the K-wires and tightened over the front of |
|
the patella. |
