
новая папка / Apley 938-988
.pdf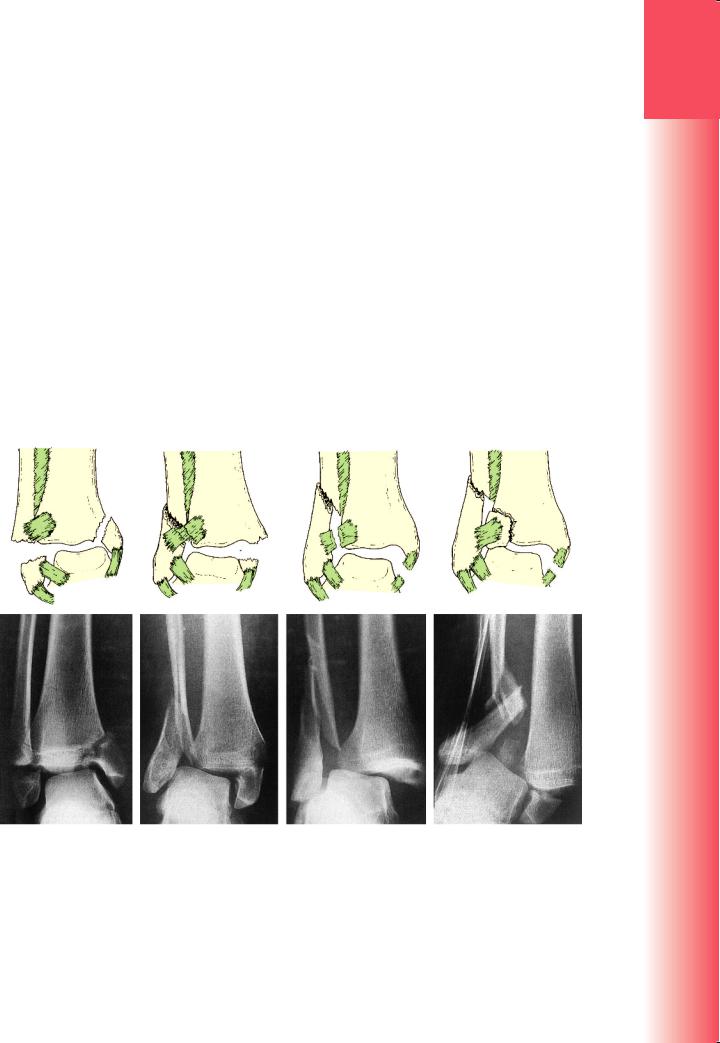
something more serious than a simple sprain. The ankle is swollen and deformity may be obvious. The site of tenderness is important; if both the medial and lateral sides are tender, a double injury (bony or ligamentous) must be suspected.
X-rays
At least three views are needed: anteroposterior, lateral and a 30-degree oblique ‘mortise’ view. The level of the fibular fracture is often best seen in the lateral view; diastasis may not be appreciated without the mortise view. Further X-rays may be needed to exclude a proximal fibular fracture, up as high as the knee.
From a careful study of the X-rays it should be possible to reconstruct the mechanism of injury. The four most common patterns are shown in Figure 32.5.
Treatment
Swelling is usually rapid and severe, particularly in the higher-energy injuries. If the injury is not dealt with
within a few hours, definitive treatment may have to be deferred for several days while the leg is elevated so that the swelling can subside; this can be hastened by using a foot pump (which also reduces the risk of deep-vein thrombosis) and cold compression.
Fractures are visible on X-ray; ligament injuries are not. Always look for clues to the invisible ligament injury – widening of the tibiofibular space, asymmetry of the talotibial space, widening of the medial joint space, or tilting of the talus – before deciding on a course of action.
Like other intra-articular injuries, ankle fractures must be accurately reduced and held if later mechanical dysfunction is to be prevented. Persistent displacement of the talus, or a step in the articular surface, leads to increased stress and predisposes to secondary osteoarthritis.
In assessing the accuracy of reduction, four objectives must be met:
•the fibula must be restored to its full length
•the talus must sit squarely in the mortise, with the talar and tibial articular surfaces parallel
(a) |
(b) |
(c) |
(d) |
Figure 32.5 Ankle fractures – classification The Danis–Weber classification is based on the level of the fibular fracture. (a) Type A: a fibular fracture below the syndesmosis and an oblique fracture of the medial malleolus (caused by forced supination and adduction of the foot). (b) Type B: a fracture at the syndesmosis often associated with disruption of the anterior fibres of the tibiofibular ligament and fracture of the posterior and/ or medial malleolus, or disruption of the medial ligament (caused by forced supination and external rotation).
(c) Type C: a fibular fracture above the syndesmosis; the tibiofibular ligament must be torn, or else (d) the ligament avulses a small piece of the tibia. Here, again, there must also be disruption on the medial side of the joint – either a medial malleolar fracture or rupture of the deltoid ligament.
32
foot and ankle the of Injuries
943
3
TRAUMA
•the medial joint space must be restored to its normal width, i.e. the same width as the tibiotalar space (about 4 mm)
•oblique X-rays must show that there is no tibiofibular diastasis.
Ankle fractures are often unstable. Whatever the method of reduction and fixation, the position must be checked by X-ray during the period of healing.
UNDISPLACED FRACTURES
The first step is to decide whether the injury is stable or unstable (Figure 32.6).
Isolated undisplaced Danis–Weber type A fractures These fractures are stable and will need minimal splintage: a firm bandage or stirrup brace is applied mainly for comfort until the fracture heals.
Undisplaced type B fractures These are potentially unstable only if the tibiofibular ligament is torn or avulsed, or if there is a significant medial-sided injury. X-rays will show if the syndesmosis or mortise is intact; if it is, a below-knee cast is applied with the ankle in the neutral (anatomical) position. The plaster may need to be split and, if so, it must be completed or replaced when swelling has subsided. A check X-ray is taken at 2 weeks to confirm that the fracture remains undisplaced. An overboot is fitted and the patient is taught to walk correctly as soon as possible. The cast can usually be discarded after 6–8 weeks. Ankle and foot movements are regained by active exercises when the plaster is removed. As with any lower limb fracture, the leg must not be allowed to dangle idly – it must be exercised and elevated.
Undisplaced type C fractures |
These |
fractures |
are deceivingly innocent-looking |
but |
are often |
accompanied by disruption of the medial joint structures as well as the tibiofibular syndesmosis and interosseous membrane. These defects may become apparent only when the fracture displaces in a cast; arguably, therefore, type C fractures are better fixed from the outset.
DISPLACED FRACTURES
Reduction of these joint disruptions is a prerequisite to all further treatment; knowledge of the causal mechanism (and this is where the Lauge-Hansen classification is useful) helps to guide the method of closed reduction. Although internal fixation is usually performed to stabilize the reduction, not all such fractures require surgery.
Displaced Danis-Weber type A fractures The medial malleolar fracture is nearly vertical and after closed reduction it often remains unstable; internal fixation of the malleolar fragment with one or two screws directed almost parallel to the ankle joint is advisable. A perfect reduction should be aimed for, with accurate restoration of the tibial articular surface. Loose bone fragments are removed. The lateral malleolar fracture, unless it is already perfectly reduced and stable, should be fixed with a plate and screws or tension-band wiring (Figure 32.7). Postoperatively a ‘walking cast’ or removable splintage boot is applied for 6 weeks; the advantage of removable splintage is that early physiotherapy can be commenced.
Displaced Danis-Weber type B fractures The most common fracture pattern is a spiral fracture of the fibula and an oblique fracture of the medial malleolus. The causal mechanism is external rotation of the ankle when the foot is caught in a supinated position.
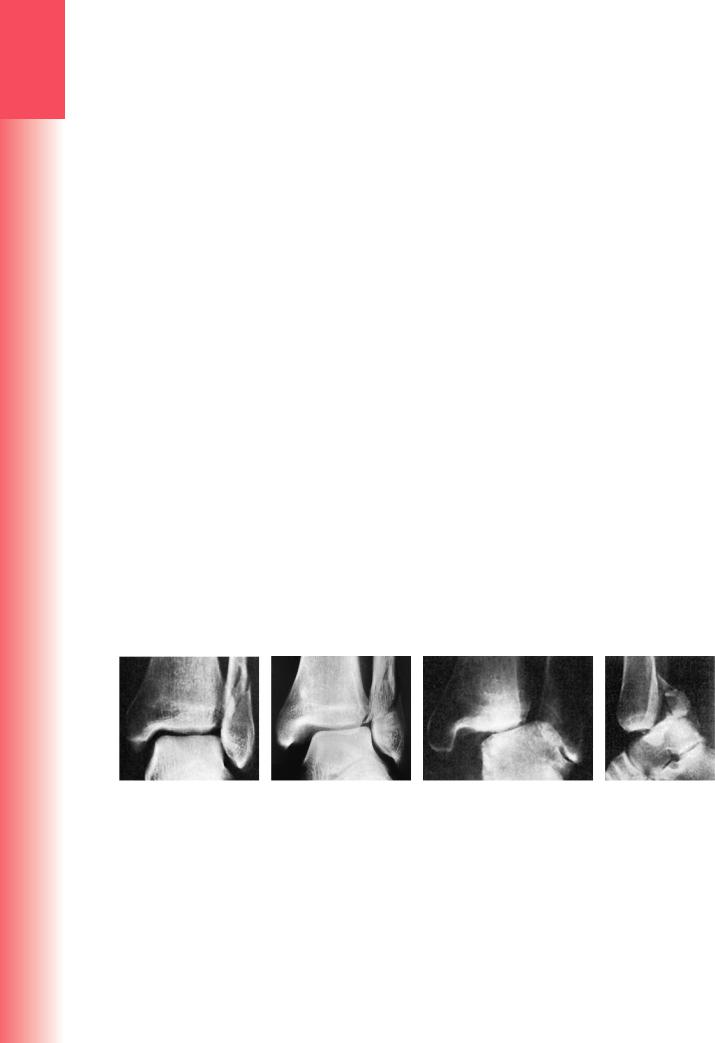
|
(a) |
(b) |
(c) |
(d) |
|
Figure 32.6 Ankle fractures – stable or unstable? (a) Stable fracture: In this Danis–Weber type B fracture the |
|||
|
tibiofibular syndesmosis has held; the surfaces of the tibia and talus are precisely parallel and the width of the |
|||
|
joint space is regular both superiorly and medially. (b) Slight subluxation: The syndesmosis is intact but the talus |
|||
|
has moved laterally with the distal fibular fragment; the medial joint space is too wide, signifying a deltoid |
|||
|
ligament rupture. It is vital, after reduction of the fibular fracture, to check that the medial joint space is nor- |
|||
|
mal; if it is not, the ligament has probably been trapped in the joint and it must be freed so as to allow perfect |
|||
|
repositioning of the talus. (c) Fracture dislocation: In this high fibular fracture the syndesmosis has given way, |
|||
|
the medial collatoral ligament has been torn and the talus is displaced and tilted. The fibula must be fixed to |
|||
|
full length and the tibiofibular joint secured before the ankle can be stabilized. (d) Posterior fracture-disloca- |
|||
944 |
tion: If the posterior margin of the tibia is fractured, the talus may be displaced upwards. The fragment must |
|||
be replaced and fixed securely. |
|
|
||

(e)
(a) |
(b) |
(c) |
(d) |
(f) |
Figure 32.7 Ankle fractures – open treatment (1) (a,b) Danis–Weber type A fractures can often be treated conservatively but, if the medial malleolar fragment involves a large segment of the articular surface, it is best treated by accurate open reduction and internal fixation with one or two screws. (c,d) An unstable fracture-dislocation such as this almost always needs open reduction and internal fixation. The fibula should be restored to full length and fixed securely; in this case the medial malleolus also needed internal fixation; (e) and (f) show the range of ankle movement a few days after operation and before a ‘walking plaster’ was applied.
Closed reduction therefore needs traction (to disimpact the fracture) and then internal rotation of the foot. If closed reduction succeeds, a cast is applied, following the same routine as for undisplaced fractures. Failure of closed reduction (sometimes a torn medial ligament is caught in between the talus and medial malleolus) or late redisplacement calls for operative treatment.
Type B fractures may also be caused by abduction; often the lateral aspect of the fibula is comminuted and the fracture line more horizontal. Despite accurate reduction (the ankle is adducted and the foot supinated), these injuries are unstable and often poorly controlled in a cast; internal fixation is therefore preferred.
Displaced Danis-Weber type C fractures The fibular fracture is well above the syndesmosis and frequently there are associated medial and posterior malleolar fragments. An isolated type C fibular fracture should raise strong suspicions of major ligament damage to the syndesmosis and medial side of the joint. Almost all type C fractures are unstable and will need open reduction and internal fixation (Figure 32.8). The first step is to reduce the fibula, restoring its length and alignment; the fracture is then stabilized using a plate and screws. If there is a medial fracture, this also is fixed. The syndesmosis is then checked, using a hook to pull the fibula laterally. If the joint opens out, it means that the ligaments are torn; the syndesmosis is stabilized by inserting a
32
foot and ankle the of Injuries
(a) (b) (c) (d) (e) (f)
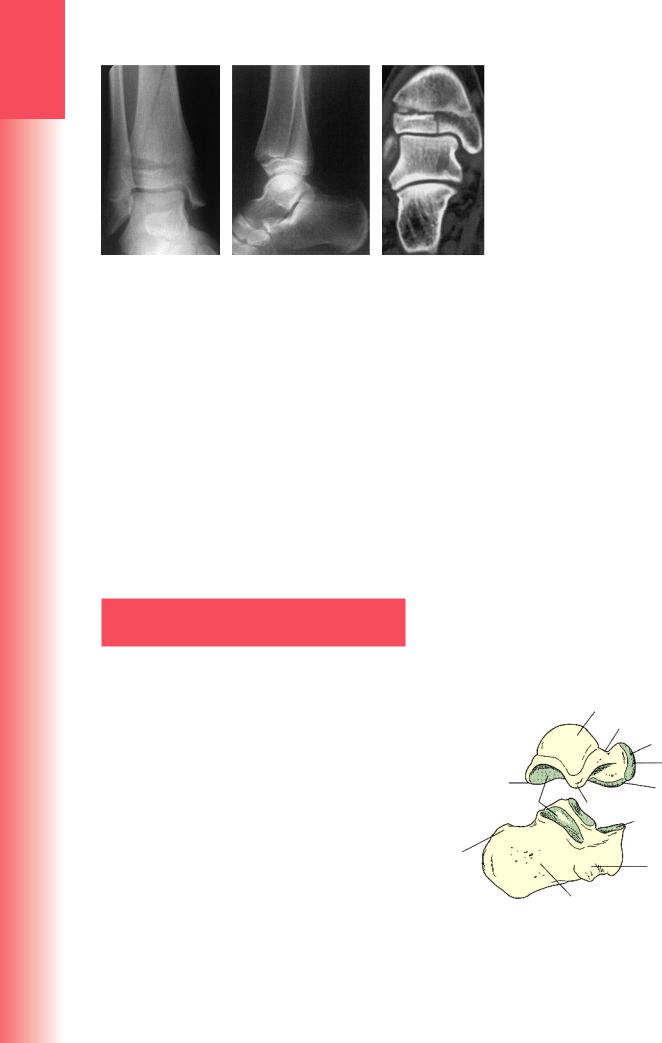
Figure 32.8 Ankle fractures with diastasis – open treatment (2) (a) In this type B fracture there is partial disrup- |
|
tion of the distal tibiofibular syndesmosis. Treatment (b) required medial and lateral fixation as well a tibio- |
|
fibular screw. (c) A type C fracture must, inevitably, disrupt the tibiofibular ligament; in this case the medial |
|
malleolus was intact but the deltoid ligament was torn (look at the wider than normal medial joint space). |
|
(d) By fixing the fibular fracture and using a tibiofibular screw, the ankle was completely reduced and it was |
|
therefore unnecessary to explore the deltoid ligament. (e) This patient presented 5 days after his injury; he, |
|
too, had a diastasis with disruption of the deltoid ligament (f). In this case the tibiofibular joint as well as the |
945 |
deltoid ligament had to be explored before the ankle could be reduced. |

3 |
transverse screw across from the fibula into the tibia |
|
(the ankle should be held in 10 degrees of dorsiflexion |
||
|
when the screw is inserted). |
|
|
Fracture subluxations more than 1–2 weeks old |
|
|
||
|
may prove difficult to reduce because of clot organiza- |
|
TRAUMA |
tion in the syndesmosis. Granulation tissue should be |
|
removed from the syndesmosis and transverse tibio- |
||
|
||
|
fibular fixation secured. |
|
|
Postoperative management After open reduction |
|
|
and fixation of ankle fractures, movements should |
|
|
be regained before applying a below-knee plaster |
|
|
cast or removable support boot. The patient is then |
|
|
allowed partial weight-bearing with crutches; the sup- |
|
|
port is retained until the fractures have consolidated |
|
|
(6–12 weeks). |
|
|
Management of the syndesmosisor diastasis-screw |
|
|
remains controversial. Some advocate removal of the |
|
|
screw when the syndesmosis has healed, and before |
|
|
weight-bearing has commenced (6 weeks is too early; |
|
|
10 weeks is probably more appropriate). Others are |
|
|
happy to allow early weight-bearing with the screw |
|
|
still in place, accepting that the screw may break |
|
|
(especially if four cortices are engaged). |
|
|
OPEN FRACTURES |
|
|
Open fractures of the ankle pose special problems. |
|
|
If the fracture is not reduced and stabilized at an |
|
|
early stage, it may prove impossible to restore the |
|
|
anatomy. For this reason unstable injuries should |
|
|
be treated by internal fixation even in the pres- |
|
|
ence of an open wound, provided the soft tissues |
|
|
are not too severely damaged and the wound is not |
|
|
contaminated. As with all open fractures, atten- |
|
|
tion must be paid to the extent of damage to the |
|
|
soft-tissue envelope and the involvement of other |
|
|
structures, particularly neurovascular or tendinous |
|
|
injuries. If internal fixation seems inappropriate, an |
|
|
external fixator can be used, often as a temporary |
|
|
spanning option. Treatment in other respects fol- |
|
|
lows the principles outlined in Chapter 23. |
|
|
Complications |
|
|
EARLY |
|
|
Vascular injury With a severe fracture-subluxation |
|
|
the pulses may be obliterated. The ankle should be |
|
|
reduced immediately and held in a splint until prompt |
|
|
definitive treatment has been initiated. |
|
|
Wound breakdown and infection Diabetic patients |
|
|
are at greater than usual risk of developing wound- |
|
|
edge necrosis and deep infection. In dealing with |
|
|
displaced fractures, these risks should be carefully |
|
|
weighed against the disadvantages of conservative |
|
|
treatment; casts may also cause skin problems if not |
|
|
well padded and they are less effective in preventing |
|
946 |
malunion. |
LATE
Incomplete reduction Incomplete reduction is common and, unless the talus fits the mortise accurately, degenerative changes may occur. This can sometimes be prevented by a corrective osteotomy.
Non-union The medial malleolus occasionally fails to unite because a flap of periosteum or other tissue is interposed between it and the tibia. It should be prevented by operative reduction and screw fixation.
Joint stiffness Swelling and stiffness of the ankle are usually the result of the soft-tissue injury. Optimal treatment can help to mitigate these potential problems. The patient must walk correctly in plaster and, when the plaster is removed, he or she must, until circulatory control is regained, wear a support bandage and elevate the leg whenever it is not being used actively. Physiotherapy is always helpful.
Complex regional pain syndrome (CRPS) This often follows fractures of the ankle. The patient complains of pain in the foot; there may be swelling and diffuse tenderness, with gradual development of trophic changes and severe osteoporosis. Management is discussed in Chapter 10.
Osteoarthritis Malunion and/or incomplete reduction may lead to secondary osteoarthritis of the ankle in later years. Unless the ankle is unstable, symptoms can often be managed by judicious analgesic treatment and the use of firm, comfortable footwear. However, in the longer term, if symptoms become severe, arthrodesis may be necessary.
PILON FRACTURES
Unlike the twisting injuries that cause the common ankle fractures, pilon injury to the ankle joint occurs when a large force drives the talus upwards against the tibial plafond, like a pestle (pilon) being struck into a mortar. There is considerable damage to the articular cartilage and the subchondral bone may be broken into several pieces; in severe cases, the comminution extends some way up the shaft of the tibia.
Clinical features
There may be little swelling initially but this rapidly changes and fracture blisters are common. The ankle may be deformed or even dislocated; prompt approximate reduction is mandatory.
Imaging
This is a comminuted fracture of the distal end of the tibia, extending into the ankle joint. The fracture may be classified according to the amount of displacement and comminution, but in all cases assessment is far better
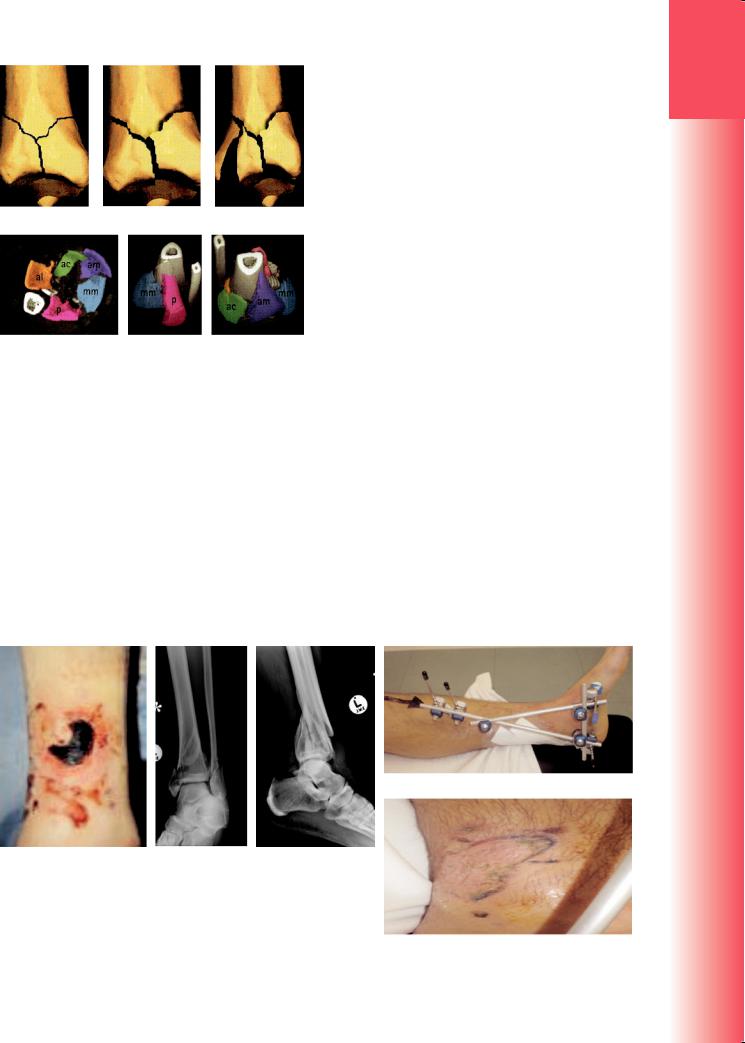
(a) |
(b) |
(c) |
(d) (e) (f)
Figure 32.9 Pilon fractures – imaging These may be (a) undisplaced (type 1), (b) minimally displaced
(type 2); (c) markedly displaced (type 3). CT (d) shows that there are usually five major tibial fragments: anterolateral (al), anterocentral (ac), anterome-
dial (am), the medial malleolus (mm) and the posterior fragment (p). These elements are better defined by 3D CT reconstruction.
with CT scanning (preferably including 3D reconstruction) than with plain X-ray examination (Figure 32.9).
Control of soft-tissue swelling is a priority; this is best achieved by elevation and applying an external fixator across the ankle joint (the spanning external fixator). It may take 2–3 weeks before the soft tissues improve, and fracture blisters can be actively managed rather than hidden under plaster (Figure 32.10). Surgery can be planned, based on the CT scan.
Once the skin has recovered, or using an approach that respects the zone of injury and pattern of vascularity, an open reduction and fixation with plates and screws (usually with bone grafting) may be possible (Figure 32.11). However, the more severe injuries do not readily tolerate large surgical exposures for plating, and significant wound breakdown and infection rates have been reported. Better results have followed wider use of indirect reduction techniques (e.g. applying a bone distractor or utilizing the spanning fixator across the joint to obtain as much reduction as possible through ligamentotaxis) and plating through limited exposures. Recently, these injuries have been successfully treated by using a combination of indirect reduction methods and small screws to hold the articular fragments, coupled with axially stable locking plates. Circular frame and fine-wire fixation has also been successful.
The soft-tissue swelling following these injuries is substantial. After fixation, elevation and early movement help to reduce the oedema; arteriovenous impulse devices applied to the sole of the foot are also helpful.
Treatment |
Outcome |
The three points of early management of these injuries |
Pilon fractures usually take several months to heal. |
are: span, scan, plan. Staged treatment has reduced |
Postoperatively, physiotherapy is focused on joint |
the complication rate in these injuries. |
movement and reduction of swelling. There remains, |
(d)
(a) |
(b) |
(c) |
Figure 32.10 Pilon fracture A 43-year-old man suffered a high-energy comminuted fracture of the distal end of the tibia. (a) Swelling
and fracture blisters around the ankle. (b,c) X-rays showing disruption of the metaphyseal–diaphyseal junction in this pilon fracture.
(d) Fracture held in an external fixator. (e) Fracture blisters were de-roofed and treated with Flamazine (silver sulphadiazine); the skin (e) has re-epithelialized and is free of infection 5 days after injury.
32
foot and ankle the of Injuries
947
3
TRAUMA
(a) |
(b) |
Figure 32.11 Same case as Figure 32.10 – outcome At 3 months after minimal approach reduction and fixation with distal locking plates the fractures have healed and the joint is congruent and normally aligned.
however, a challenging problem with poor functional results in these complex fractures, which represent a significant soft tissue injury as well as bony jigsaw. Although bony union may be achieved, the fate of the joint is decided by the degree of cartilage injury – the ‘invisible’ factor on X-rays. Secondary osteoarthritis, stiffness and pain are still frequent late complications in these injuries.
ANKLE FRACTURES IN CHILDREN
Mechanism of injury
The foot is fixed to the ground or trapped in a crevice and the leg twists to one or the other side. The tibial (or fibular) physis is wrenched apart, usually resulting in a Salter–Harris type 1 or 2 fracture. With severe external rotation or abduction the fibula may also fracture more proximally. The tibial metaphyseal spike may come off posteriorly, laterally or posteromedially; its position is determined by the mechanism of injury and suggests the method of reduction. With adduction injuries the tip of the fibula may be avulsed.
Type 3 and 4 fractures are uncommon. They are due to a supination–adduction force. The epiphysis is split vertically and one piece of the epiphysis (usually the medial part) may be displaced.
Two unusual injuries of the growing ankle are the Tillaux fracture and the notorious triplane fracture. The Tillaux fracture is an avulsion of a fragment of tibia by the anterior tibiofibular ligament (Figure 32.13); in the child or adolescent this fragment is the lateral part of the epiphysis and the injury is therefore a Salter–Harris type 3 fracture.
The triplane fracture occurs on the medial side of the tibia and is a combination of Salter–Harris type 2 and 3 injuries. Fracture lines appear in the coronal, sagittal and transverse planes. Injury to the physis may result in either asymmetrical growth or arrested growth.
Clinical features
Following a sprain the ankle is painful, swollen, bruised and acutely tender. There may be an obvious deformity, but sometimes the injury looks deceptively mild.
Imaging
Physeal injuries are quite common in children and almost a third of these occur around the ankle (Figure 32.12).
Undisplaced physeal fractures – especially those in the distal fibula – are easily missed. Even a hint of physeal widening should be regarded with great suspicion and
|
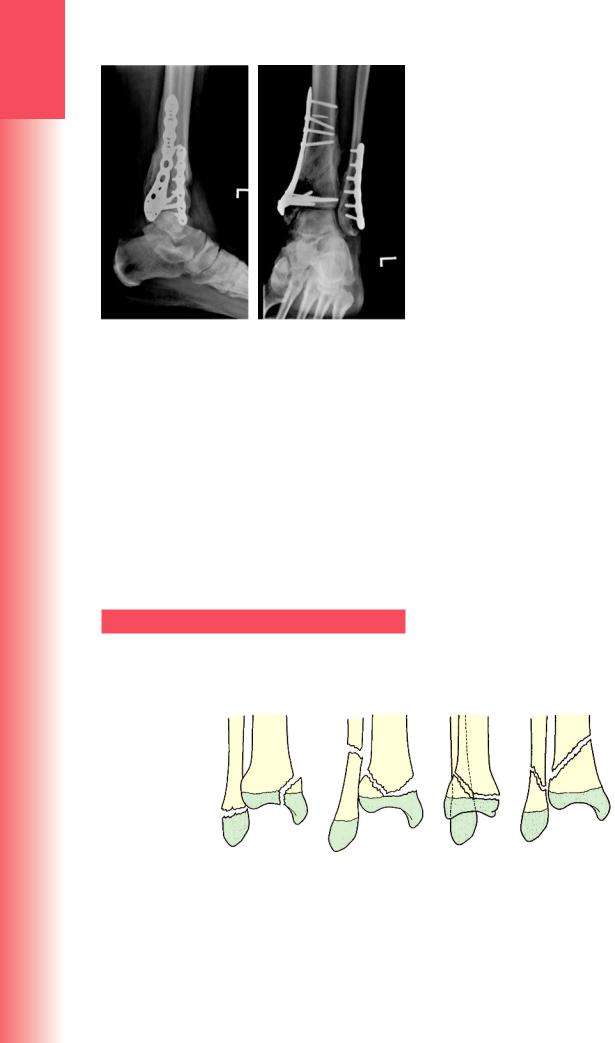
(a) |
(b) |
(c) |
(d) |
|
Figure 32.12 Physeal injuries of the distal tibia The classification suggested by Dias and Tachdjian has the merit of |
|||
|
pointing to the required reduction manoeuvre – the reverse of the causal mechanism. (a) Supination–inversion: the |
|||
|
fibular fracture is usually an avulsion (Salter–Harris type 1) whereas the medial malleolar fracture can be variable. |
|||
|
(b) Pronation–eversion–external rotation: the fibular fracture is often high and transverse. (c) Supination–plantar- |
|||
948 |
flexion: a fracture of the distal tibia only (Salter–Harris type 1 or 2) with posterior displacement. (d) Supination– |
|||
external rotation: an oblique fibular fracture coupled with a fracture of the distal tibia. |
||||
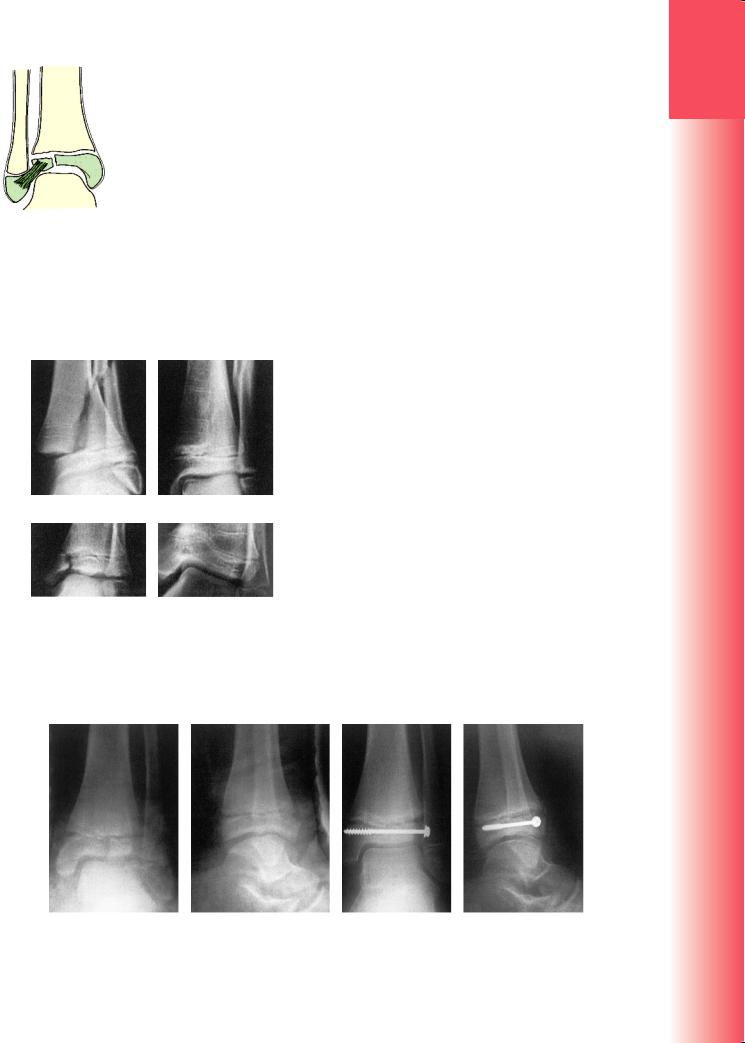
Figure 32.13 Tillaux fracture Diagram illustrating the elements of this unusual injury.
the child X-rayed again after 1 week. In an infant the state of the physis can sometimes only be guessed at, but a few weeks after injury there may be extensive periosteal new bone formation.
In triplane fractures the tibial epiphysis may be split in one plane and the metaphysis in another, thus
(a) |
(b) |
(c) |
(d) |
Figure 32.14 Ankle fractures in children (a) Salter– Harris type 2 injury; after reduction (b) growth has proceeded normally. (c) Salter–Harris type 3 injury;
(d) the medial side of the physis has fused prematurely, resulting in distorted growth.
making it difficult to see both fractures in the same X-ray. CT scans are particularly helpful in these and other type 3 injuries.
Treatment
Salter–Harris types 1 and 2 injuries are treated closed. If it is displaced, the fracture is gently reduced under general anaesthesia; the limb is immobilized in a full length cast for 3 weeks and then in a below-knee walking cast for a further 3 weeks. Occasionally, surgery is needed to extract a periosteal flap, which prevents an adequate reduction (Figure 32.14).
Type 3 or 4 fractures, if undisplaced, can be treated in the same manner, but the ankle must be re-X-rayed after 5 days to ensure that the fragments have not slipped. Displaced fractures can sometimes be reduced closed by reversing the forces that produced the injury. However, unless reduction is near-perfect, the fracture should be reduced open and fixed with interfragmentary screws, which are inserted parallel to the physis. Postoperatively the leg is immobilized in a below-knee cast for 6 weeks.
Tillaux fractures are treated in the same way as type 3 fractures (Figure 32.15). Triplane fractures, if undisplaced, can be managed closed but require vigilant monitoring for late displacement (Figure 32.16). Displaced fractures must be reduced and fixed.
Complications
Malunion Imperfect reduction may result in angular deformity of the ankle – usually valgus. In children under 10 years old, mild deformities may be accommodated by further growth and modelling. In older children the deformity should be corrected by a supramalleolar closing-wedge osteotomy.
Asymmetrical growth Fractures through the epiphysis (Salter–Harris type 3 or 4) may result in localized fusion of the physis. The bony bridge is usually in the
32
foot and ankle the of Injuries
(a) |
(b) |
(c) |
(d) |
Figure 32.15 Tillaux fracture (a,b) This avulsion fracture of the lateral part of the physis was reduced and fixed |
949 |
percutaneously (c,d). |
3
TRAUMA
(a) |
(b) |
(c) |
medial half of the growth plate; the lateral half goes on growing and the distal tibia gradually veers into varus. MRI and CT are helpful in showing precisely where physeal arrest has occurred. If the bony bridge is small (less than 30% of the physeal width), it can be excised and replaced by a pad of fat in the hope that physeal growth may be restored. If more than half of the physis is involved, or the child is near the end of the growth period, a supramalleolar closing-wedge osteotomy is indicated.
Shortening Early physeal closure occurs in about 2% of children with distal tibial injuries. Fortunately, the resulting limb length discrepancy is usually mild. If it promises to be more than 2 cm and the child is young enough, proximal tibial epiphysiodesis in the opposite limb may restore equality. If the discrepancy is marked, or the child near the end of the growth period, leg lengthening is indicated.
PRINCIPLES IN MANAGING INJURIES
OF THE FOOT
Injuries of the foot are apt to be followed by residual symptoms and loss of function that seem out of proportion to the initial trauma. Severe injuries affect the foot as a whole, whatever the particular bone that might be fractured. A global approach is therefore essential in dealing with these injuries, the objective being a return to full weight-bearing without pain, with an appropriate propulsive gait.
Identification of these injuries is particularly challenging in the patient with multiple trauma, where the more subtle foot injuries might be missed as the life-threatening truncal injuries and limb-threatening long bone injuries distract attention from the more subtle injuries to the foot, which may nonetheless impair eventual function.
Clinical assessment
Figure 32.16 Triplane fracture The three fracture planes may not be seen in a single X-ray, but can be visualized from a combination of images (a,b). In this case the epiphyseal fracture is clearly seen only in the coronal plane CT scan (c).
to one spot. Multiple fractures, or combinations of fractures and dislocations, are easily missed. The circulation and nerve supply must be carefully assessed; a well-reduced fracture is a useless achievement if the foot becomes ischaemic or insensate. Similarly, attention must be paid to the soft tissues and functional movement of the foot; the stiff, painful foot is impaired for propulsion, and maybe even for stance.
Fractures and dislocations may cause tenting of the skin; this is always a bad sign because there is a risk of skin necrosis if reduction is delayed.
Imaging
Imaging routinely begins with anteroposterior, lateral and oblique X-rays of the foot. If a fracture of the talus or calcaneum or fracture-dislocation of the midtarsal joints is suspected, a CT scan of the foot should be obtained.
CT is especially useful for evaluating fractures of the calcaneum, and MRI is helpful in diagnosing osteochondral fractures of the talus. Familiarity with the talocalcaneal anatomy is essential if fractures of the hindfoot are to be diagnosed properly (Figure 32.17).
Body
TALUS |
Neck |
|
|
|
Head |
|
Articulation with |
|
navicular |
Posterior process |
Articulation with |
|
|
Articular surfaces |
Lateral process sustentaculum tali |
|
Facet on sustentaculum |
|
tali |
Tuberosity |
Anterior process |
|
|
CALCANEUS |
Body |
|
950 |
The entire foot should be examined systematically, |
no matter that the injury may appear to be localized |
Figure 32.17 Talus and calcaneum The main features of these two bones, and their relationship to each other, are shown here.

Treatment
Swelling is always a problem. Not only does it make clinical examination difficult, but more importantly it may lead to definitive treatment being delayed; fractures and dislocations are more difficult to reduce in a swollen foot. The principles are:
•realign and splint the foot, keep it elevated and apply Cryo-Cuff or ice-packs and intermittent pneumatic compression foot pumps
•make the diagnosis, defining the extent of injury
•start definitive treatment as soon as the fracture pattern is properly defined and swelling permits.
In the rehabilitation phase, if the foot has to be immobilized, exercise those joints that can be left free. Start weight-bearing as soon as the patient will tolerate it, provided this will not jeopardize the reduction. If a removable splint will fit the purpose, use it so that non-weight-bearing exercises can be started as soon as possible. Prolonged immobilization predisposes to stiffness, impaired function, localized osteoporosis and complex regional pain syndrome.
Mechanism of injury
Fracture of the talar neck is produced by violent hyperextension of the ankle. The neck of the talus is forced against the anterior edge of the tibia, which acts like a cleaver. If the force continues, the fracture is displaced and the surrounding joints may sublux or dislocate.
Fracture of the body is usually a compression injury due to a fall from a height, or an everting force across the body, fracturing the lateral process (the snowboarder’s fracture). Avulsion fractures are associated with ligament strains around the ankle and hindfoot.
Clinical features
The patient has most commonly been involved in a motor vehicle accident or has fallen from a height. The foot and ankle are painful and swollen; if the fracture is displaced, there may be an obvious deformity, or the skin may be tented or split. Tenting is a dangerous sign; if the fracture or dislocation is not promptly reduced, the skin may slough and become infected. The pulses should be checked and compared with those in the opposite foot.
INJURIES OF THE TALUS
Talar fractures and dislocations are relatively uncommon. They usually involve considerable violence, such as car accidents in which the occupants are thrown against the resistant frame of the vehicle, falls from a height, or severe wrenching of the ankle. The injuries include fractures of the neck, body, head or bony processes of the talus, dislocations of the talus or the joints around the talus, osteochondral fractures of the superior articular surface, and a variety of chip or avulsion fractures.
The significance of the more serious injuries is enhanced by two important facts: (1) the talus is a major weight-bearing structure (the superior articular surface carries a greater load per unit area than any other bone in the body); (2) it has a vulnerable blood supply and is a relatively common site for posttraumatic ischaemic necrosis.
Blood vessels enter the bone from the anterior tibial, posterior tibial and peroneal arteries, as well as anastomotic vessels from the surrounding capsule and ligaments. The head of the talus is richly supplied by intraosseous vessels. However, the body of the talus is supplied mainly by vessels that enter the talar neck from the tarsal canal and then run retrograde from distal to proximal. In fractures of the talar neck these vessels are disrupted; if the fracture is displaced, the extraosseous plexus too may be damaged and the body of the talus is at risk of ischaemia.
Imaging
Anteroposterior, lateral and oblique X-ray views are essential (Figure 32.18); CT scanning helps to identify associated injuries of the ankle and foot. Both malleoli, the ankle mortise, the talus and all the adjacent tarsal bones should be carefully assessed. Undisplaced fractures are not always easy to see, and sometimes even severely displaced fractures are missed in the initial assessment because of unfamiliarity with the normal appearance – sad but true.
Classification
Fractures of the neck of the talus These fractures are classified according to the system devised by Hawkins and modified by Canale:
•Type I – undisplaced
•Type II – displaced (however little) and associated with subluxation or dislocation of the subtalar joint
•Type III – displaced, with dislocation of the body of the talus from the ankle joint
•Type IV – displaced vertical talar neck fracture with associated talonavicular joint disruption.
Fractures of the head of the talus This is a rare injury; the fracture usually involves the talonavicular joint.
Fractures of the body of the talus These are also uncommon. The fracture is often displaced and may cause distortion of the talocalcaneal joint. Rotational malalignment of the fragments is difficult
32
foot and ankle the of Injuries
951
3
TRAUMA
|
|
|
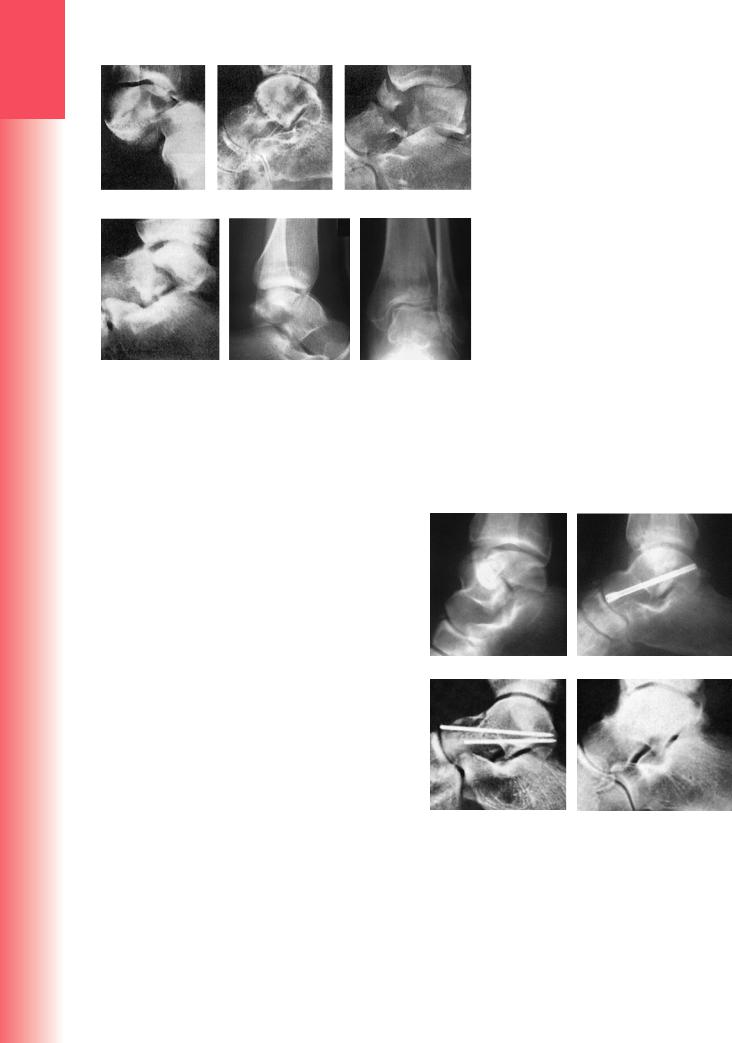
Figure 32.18 Injuries of the talus – X-rays |
|
|
|
(a) Talocalcaneal fracture-dislocation; |
|
|
|
(b) undisplaced fracture of the talar neck; |
|
|
|
(c) type III fracture of the neck; (d) dis- |
|
|
|
placed fracture of the body of the talus. |
|
|
|
(e) This fracture of the body was thought |
|
|
|
to be well reduced; however, in the AP |
|
|
|
view (f) it is possible to see two overlap- |
|
|
|
ping outlines, indicating that the frag- |
(a) |
(b) |
(c) |
ments are malrotated. |
(d) |
(e) |
(f) |
to diagnose on plain X-ray examination; the deformity is best visualized by 3D CT reconstruction.
Fractures of the lateral and posterior processes These are usually associated with ankle ligament strains. It is sometimes difficult to distinguish between a fracture of the posterior process and a normal os trigonum. A simple rule is, ‘If it’s not causing symptoms, it doesn’t really matter.’
Osteochondral fractures Osteochondral fractures following acute trauma usually occur on the lateral part of the dome of the talus. The diagnosis is often missed when the patient is first seen and may come to light only after CT or MRI scan.
|
Treatment |
|
The general principles in managing injuries of the |
|
foot set out above should be observed. |
|
UNDISPLACED FRACTURES |
|
A split below-knee plaster, or a supportive boot, |
|
is applied and, when the swelling has subsided, is |
|
replaced by a complete cast with the foot plantar- |
|
flexed. Weight-bearing is not permitted for the first |
|
4 weeks; thereafter, the plaster is removed, the frac- |
|
ture position is checked by X-ray, a new cast is applied |
|
and weight-bearing is gradually introduced. Further |
|
plaster changes or use of an adjustable splintage boot |
|
will allow the foot to be brought up, slowly, to plan- |
|
tigrade; physiotherapy is commenced. At 8–12 weeks |
|
the splintage is discarded and function is regained by |
|
normal use. |
|
DISPLACED FRACTURES OF THE NECK |
952 |
Even the slightest displacement makes it a type II |
fracture, which needs to be reduced. If the skin is |
tight, reduction becomes urgent because of the risk of skin necrosis (Figure 32.19). Reduction must be perfect: (1) in order to ensure that the subtalar joint is mechanically sound; and (2) to lessen the chance – or at any rate lessen the effects – of avascular necrosis.
With type II fractures, closed manipulation under general anaesthesia can be tried first. Traction is
(a) |
(b) |
(c) (d)
Figure 32.19 Fractures of the talus – treatment
(a) This displaced fracture of the body was reduced and fixed with a countersunk screw (b), giving a perfect radiological result. Fractures of the neck, even if well reduced (c) are still at risk of developing ischaemic necrosis (d). The stabilization with K-wires would probably now be improved upon by using definitive screw fixation, but the risk of avascular necrosis would be the same.
