
новая папка / Apley 938-988
.pdf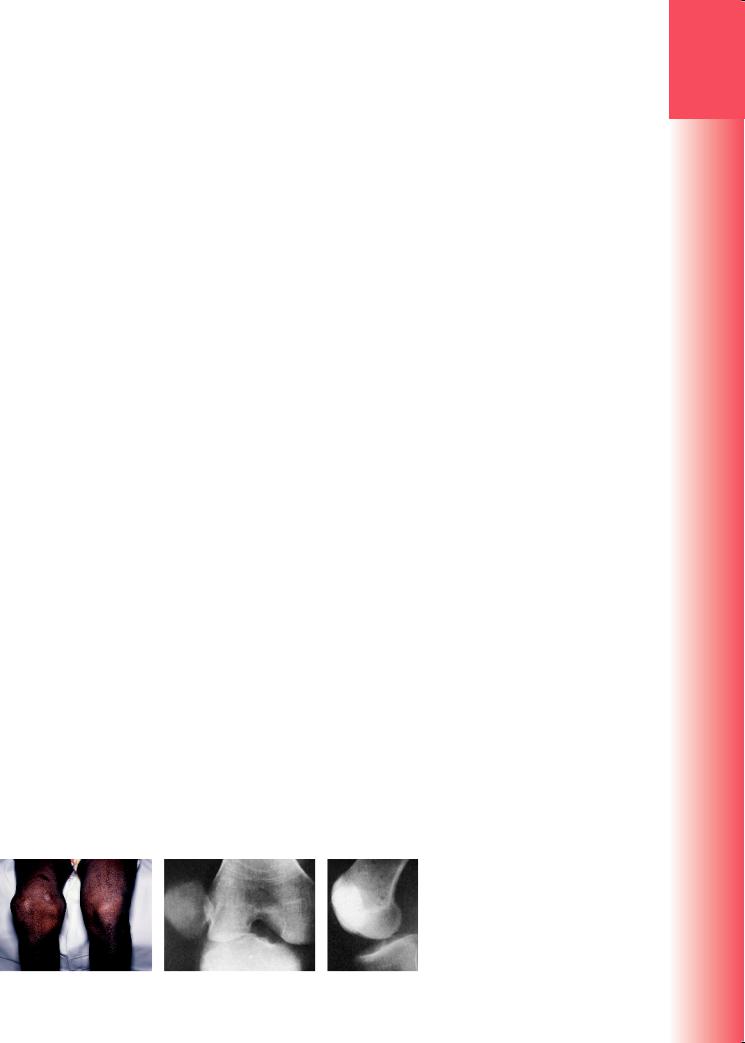
extensor muscle contraction pulls it firmly into the groove; and the extensor retinacula and patellofemoral ligaments guide it centrally as it tracks along the trochlea groove. The most important static checkrein on the medial side is the medial patellofemoral ligament, a more or less distinct structure extending from the superomedial border of the patella towards the medial femoral condyle deep to vastus medialis. Additional restraint is provided by the medial patellomeniscal and patellotibial ligaments and the associated medial retinacular fibres. In a typical knee, considerable force is required to wrench the patella out of its track. However, if the intercondylar groove is unusually shallow (trochlea dysplasia), or the patella is seated higher than usual (patella alta), or the ligaments are abnormally lax (hypermobility), dislocation occurs more easily.
Mechanism of injury
Patella dislocation may be traumatic or atraumatic. The patella dislocates laterally and the medial patellofemoral ligament and retinacular fibres may be torn. Atraumatic dislocations occur in patients with predisposing factors as discussed, such as trochlea dysplasia, patella alta or hypermobility. Traumatic dislocations are rarely caused by direct violence while the knee is flexed and the quadriceps muscle relaxed, although the patella may be forced laterally by direct violence. More often, traumatic dislocation is due to indirect force: sudden, severe contraction of the quadriceps muscle while the knee is stretched in valgus and external rotation. Typically this occurs in field sports when a runner dodges to one side.
The rate of first-time dislocation is highest among female adolescents. Following a first event, 17% of patients will experience subsequent instability. The younger a patient is at the time of first dislocation and the more severe the dislocation, the greater the risk of subsequent dislocation. If the patient has an established history of subluxation or dislocation, the risk of subsequent episodes rises to 50%.
Clinical features
In a ‘first-time’ dislocation the patient may experience a tearing sensation and a feeling that the knee has gone ‘out of joint.’ Often the patella springs back into position spontaneously; however, if it remains unreduced,
there is an obvious (if somewhat misleading) deformity: the displaced patella, seated on the lateral side of the knee, is not easily noticed but the uncovered medial femoral condyle is unduly prominent and may be mistaken for the patella. Neither active nor passive movement is possible (Figure 31.13). If the dislocation has reduced spontaneously, the knee may be swollen and there may be bruising and tenderness on the medial side.
With recurrent dislocation the symptoms and signs are much less marked, though still unpleasant. After spontaneous reduction the knee looks normal, but the apprehension test is positive, i.e. the patient experiences pain and apprehension of attempts to push the patella laterally.
Imaging
Anteroposterior (AP), lateral and tangential (‘patella skyline’) X-rays are needed. In an unreduced dislocation, the patella is seen to be laterally displaced and tilted or rotated. In 5% of cases there is an associated osteochondral fracture. The lateral radiograph enables assessment for patella alta and trochlear dysplasia. A shallow trochlea and a crossing sign are features of dysplasia.
MRI provides invaluable information on the multifactorial aspects of patellofemoral instability and is the investigation of choice for patients being considered for surgical intervention. The cartilage contour in the trochlea typically varies from that of the underlying bone and accentuates the dysplasia. This is not appreciable on conventional radiographs or CT.
Treatment
If unreduced, dislocations can in most cases be pushed back into place without much difficulty. There is no need for immobilization or bracing and it is safe to weight-bear on the knee as soon as it is comfortable to do so.
First-time dislocations are generally managed non-operatively in the first instance. Non-operative therapy initially aims to reducing swelling and increase the range of motion of the knee. This is followed by muscle-strengthening exercises. Physiotherapy is directed towards closed chain exercises and vastus medialis oblique (VMO) strengthening (the main dynamic stabilizer of the patella).
Figure 31.13 Dislocation of the patella (a) The right patella has dislocated laterally; the flattened appearance is typical. (b,c) AP and lateral X-rays of lateral patella dislocation.
31
leg and knee the of Injuries
923
(a) |
(b) |
(c) |

3 |
|
Surgery should not be considered until non-oper- |
|
ative treatments have failed and the recurrent nature |
|
|
|
of the disease has resulted in functional impairment. |
|
|
Surgical strategies involve addressing the underlying |
|
||
|
|
factors predisposing to recurrent dislocation. For |
TRAUMA |
|
patients with minimal or moderate trochlea dyspla- |
|
sia this may involve medial patellofemoral ligament |
|
|
|
|
|
|
reconstruction +/– tibial tubercle osteotomy if there |
|
|
is associated patella alta. For patients with severe dys- |
|
|
plasia this may involve trochleoplasty. (The subjects |
|
|
of recurrent dislocation, subluxation, chronic patellar |
|
|
instability and patellar maltracking are dealt with in |
|
|
more detail in Chapter 20). |
|
|
|
|
|
KNEE INJURIES IN CHILDREN |
|
|
PROXIMAL TIBIAL EPIPHYSEAL INJURIES |
|
|
This uncommon injury is usually caused by a severe |
|
|
hyperextension and valgus strain. It is a rare injury |
|
|
due to the insertion of knee ligaments being distal |
|
|
to the tibial epiphysis, thereby protecting the growth |
|
|
plate and transmitting stresses to the metaphysis. The |
|
|
epiphysis displaces forwards and laterally, often taking |
|
|
a small fragment of the metaphysis with it (a Salter– |
|
|
Harris type 2 injury). There is a risk of popliteal artery |
|
|
damage where the vessel is stretched across the step at |
|
|
the back of the tibia. |
|
|
Imaging |
|
|
Salter–Harris type 1 and 2 injuries may be undis- |
|
|
placed and difficult to define on X-ray; a few small |
|
|
bone fragments near the epiphysis may be the only |
|
|
clue. CT or MRI will more accurately delineate the |
|
|
injury. In the more serious injuries the entire upper |
|
|
tibial epiphysis may be tilted forwards or sideways. |
|
|
The fracture is categorized by the direction of dis- |
|
|
placement, so there are hyperextension, flexion, varus |
|
|
and valgus types. |
|
|
Treatment |
|
|
Under anaesthesia, closed reduction can usually be |
|
|
achieved. The direction of tilt may suggest the mech- |
|
|
anism of injury; the fragment can be reduced by gen- |
|
|
tle traction and manipulation in a direction opposite |
|
|
to that of the fracturing force. Fixation using smooth |
|
|
K-wires or screws may be needed if the fracture is |
|
|
unstable. The rare Salter–Harris type 3 or 4 fractures |
|
|
also may need open reduction and fixation. |
|
|
Complications |
|
|
Epiphyseal fractures in young children sometimes |
924 |
|
result in angular deformity of the proximal tibia. This |
|
may later require operative correction. |
With the higher grades of injury there is a risk of complete growth arrest at the proximal tibia. If the predicted leg length discrepancy is greater than 2.5 cm, tibial lengthening (or epiphysiodesis of the opposite limb) may be needed. Epiphysiodesis is surgical damage to the physis leading to growth arrest.
PROXIMAL TIBIAL METAPHYSEAL
FRACTURES
This rare injury (Cozen’s fracture) usually occurs between the ages of 4 and 8 years, resulting in fracture of the medial cortex with valgus angulation at the fracture site. Most fractures can be managed nonoperatively with reduction and immobilization. It is vital to ensure that any valgus angulation is corrected with careful varus moulding of the cast and this must be monitored while the fracture heals. Open reduction is rarely required, usually due to failed reduction because of interposed soft tissues.
A unique complication seen with this fracture type is a progressive valgus deformity after bony healing and possible tibial overgrowth resulting in leg lengthening.
TIBIAL TUBEROSITY INJURIES
Fracture or avulsion of the tibial tubercle usually occurs as a sports injury in young people. The knee is suddenly forced into flexion while the quadriceps is contracting, and a fragment of the tubercle – or sometimes the entire apophysis – may be wrenched from the bone. The diagnosis is suggested by the history. The area over the tubercle is swollen and tender; active extension causes pain.
The lateral radiograph shows the fracture, although this can be subtle. Patella alta may be present (the patella is abnormally high), having lost part of its distal attachment. CT/MRI may help delineate anatomy of the injury.
An incomplete fracture can be treated by applying a long-leg cast or extension brace with the knee in extension. Complete separation requires open reduction and fixation.
PATELLA SLEEVE FRACTURES
Sleeve fractures occur between the cartilage ‘sleeve’ and main part of the patella and ossific nucleus. The causative mechanism is similar to that of tibial tubercle avulsions, i.e. a forced quadriceps contraction on a flexed knee. These fractures occur most commonly in children aged 8–12 years when patella ossification is nearly complete.
Lateral radiographs may reveal small flecks of bone adjacent to the distal pole of the patella and patella alta. CT/MRI may help delineate anatomy of the injury.
Undisplaced fractures with intact extensor mechanisms may be treated in long-leg casts or extension braces. Displaced fractures require open reduction and internal fixation.
FRACTURES OF THE TIBIA
AND FIBULA
TIBIAL PLATEAU FRACTURES
Mechanism of injury
Fractures of the tibial plateau are caused by a varus or valgus force combined with axial loading (a pure valgus force is more likely to rupture the ligaments). This is sometimes the result of a car striking a pedestrian (hence the term ‘bumper fracture’); more often it is due to a fall from a height in which the knee is forced into valgus or varus. The tibial condyle is crushed or split by the opposing femoral condyle, which remains intact.
Pathological anatomy
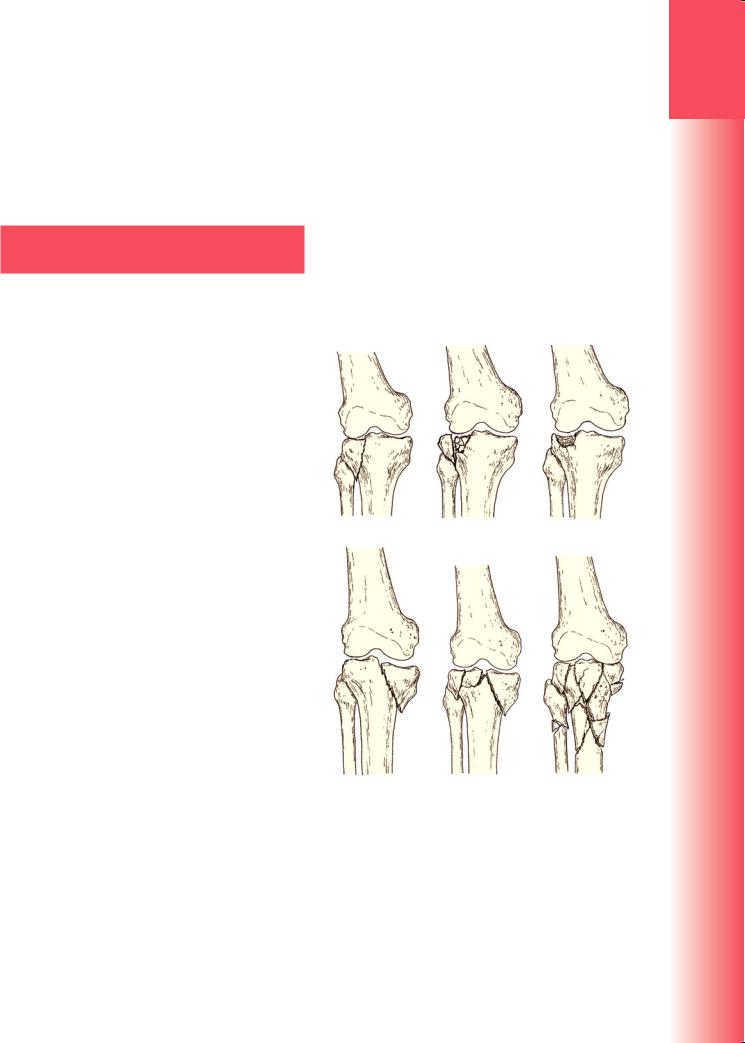
The fracture pattern and degree of displacement depend on the type and direction of force as well as the quality of the bone at the upper end of the tibia. A useful classification is that of Schatzker (Figure 31.14):
•Type 1 – a vertical split of the lateral condyle
This is a fracture through dense bone, usually in younger people. It may be virtually undisplaced, or the condylar fragment may be pushed inferiorly and tilted; the damaged lateral meniscus may be trapped in the crevice.
•Type 2 – a vertical split of the lateral condyle combined with depression of an adjacent load-bearing part of the condyle
The wedge fragment, which varies in size from a portion of the rim to a sizeable part of the lateral condyle, is displaced laterally; the joint is widened and, if the fracture is not reduced, may later develop a valgus deformity.
•Type 3 – depression of the articular surface with an intact condylar rim
Unlike type 2, the split to the edge of the plateau is absent. The depressed fragments may be wedged firmly into the subchondral bone. The joint is usually stable and may tolerate early movement.
•Type 4 – fracture of the medial tibial condyle
Two types of fracture are seen: (1) a depressed, crush fracture of osteoporotic bone in an elderly
person (a low-energy lesion); and (2) a high-energy fracture resulting in a condylar split that runs obliquely from the intercondylar eminence to the medial cortex. The momentary varus angulation may be severe enough to cause a rupture of the lateral collateral ligament and a traction injury of the peroneal nerve. The severity of these injuries should not be underestimated.
•Type 5 – fracture of both condyles
Both condyles are split but there is a column of the metaphysis wedged in between that remains in continuity with the tibial shaft.
•Type 6 – combined condylar and subcondylar fractures
This is a high-energy injury that may result in severe comminution. Unlike type 5 fractures, the tibial shaft is effectively disconnected from the tibial condyles.
(a) |
(b) |
(c) |
(d) |
(e) |
(f) |
Figure 31.14 Tibial plateau fractures - Schatzker classification (a) Type 1: simple split of the lateral condyle. (b) Type 2: a split of the lateral condyle with a more central area of depression. (c) Type 3: depression of the lateral condyle with an intact rim.
(d) Type 4: a fracture of the medial condyle. (e) Type
5:fractures of both condyles, but with the central portion of the metaphysis still connected to the tibial shaft. (f) Type 6: combined condylar and subcondylar fractures; effectively a disconnection of the shaft from the metaphysis.
31
leg and knee the of Injuries
925
3
TRAUMA
Clinical features
The knee is swollen and may be deformed. Bruising is usually extensive and the tissues feel ‘doughy’ because of haemarthrosis. Examining the knee may suggest medial or lateral instability but this is usually painful and adds little to the radiographic diagnosis. More importantly, the leg and foot should be carefully examined for signs of vascular or neurological injury. Traction injury of the peroneal or tibial nerves is not uncommon and it is important to establish the extent of any neurological injury at the time of admission and before surgery.
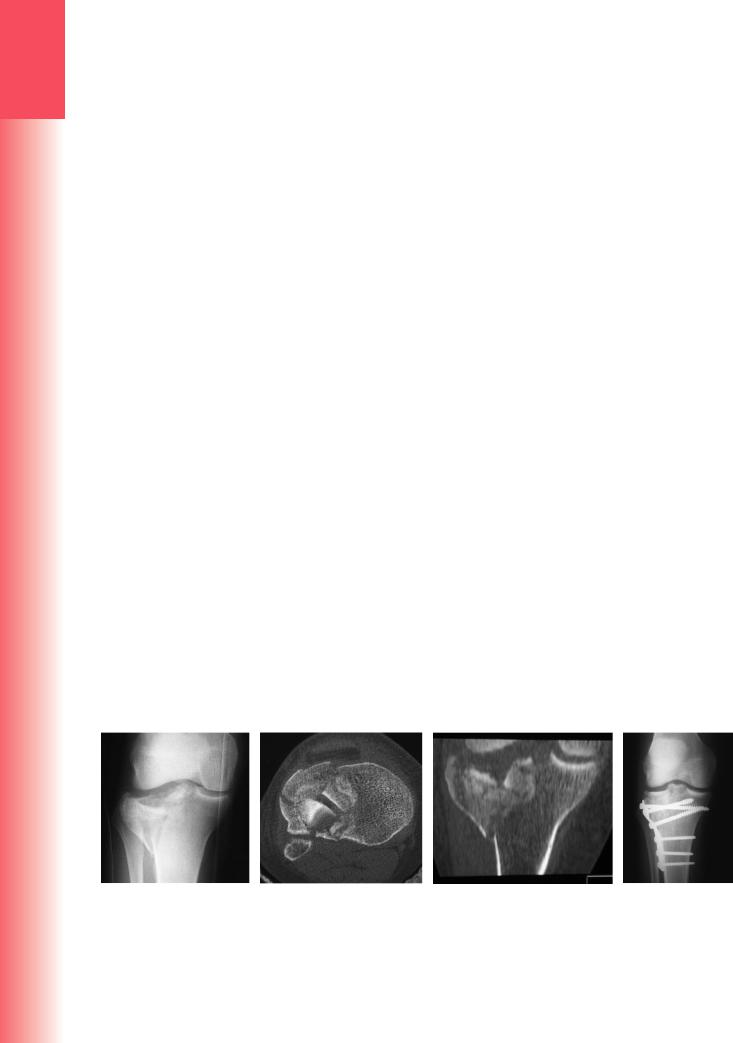
Imaging
Anteroposterior, lateral and oblique X-rays will usually show the fracture, but the amount of comminution or plateau depression may not be appreciated without CT. This provides information on the location of the main fracture lines, the site and size of the portion of condyle that is depressed and the position of major parts of articular surface that have been displaced. Software-generated reassembly of the axial images can provide sagittal and coronal views that aid in surgical planning (Figure 31.15). It is important not to miss a posterior condylar component in high-energy fractures because this may require a separate posteromedial or posterolateral exposure for internal fixation.
Treatment
TYPE 1 FRACTURES
Undisplaced type 1 fractures can be treated conservatively. As soon as the acute pain and swelling have subsided (usually within 1 week), a hinged cast-brace or ROM brace is fitted to allow early mobilization. Weight-bearing is restricted initially.
Displaced fractures should be treated by open reduction and internal fixation. The condylar surface
is examined (open or arthroscopically) and trapped fragments are released or removed. The aim is for an accurate reduction and fixation; lag screws alone or in combination with a buttress plate are usually sufficient for fixation.
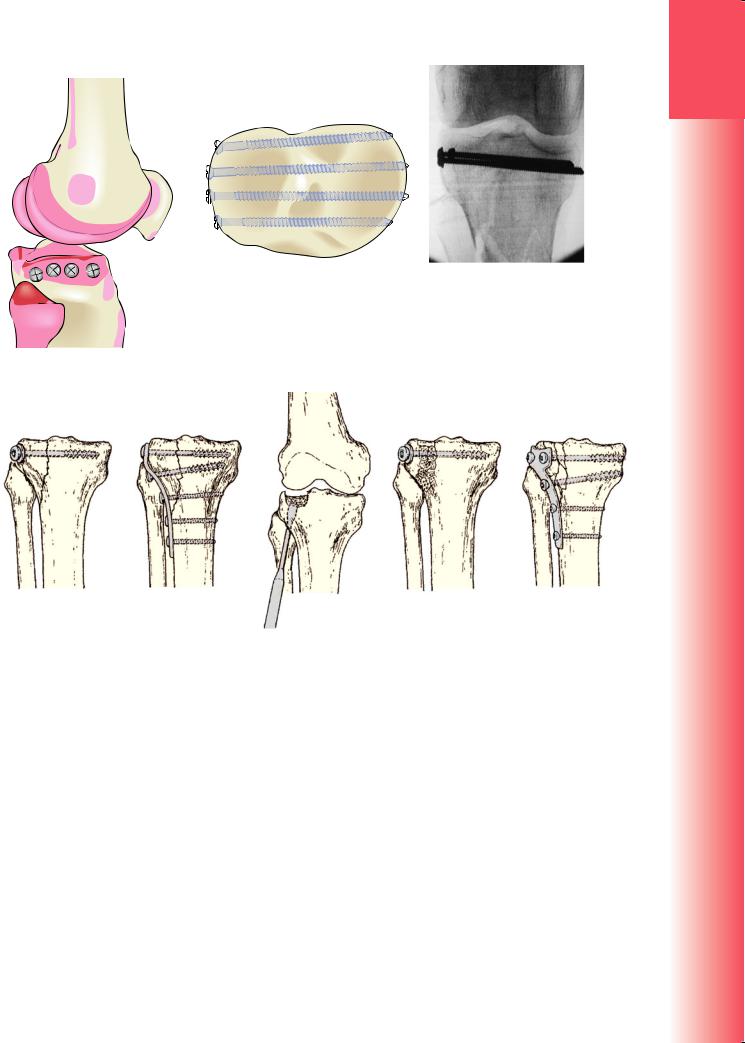
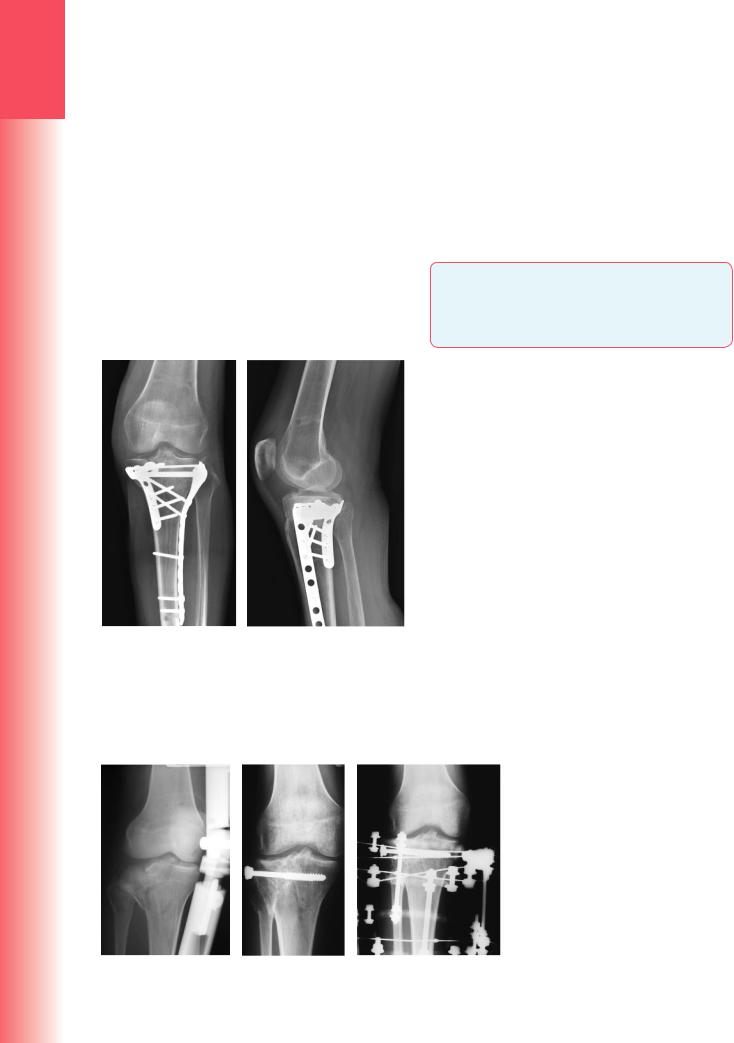
TYPE 2 FRACTURES
If depression is slight (less than 5 mm) and the knee is not unstable, or if the patient is old and frail or osteoporotic, the fracture can be treated non-operatively with the aim of regaining mobility and function rather than anatomical restitution. In younger patients, and more so in those with a central depression of more than 5 mm, open reduction with elevation of the plateau and internal fixation is required. The joint is seen to allow a check on the quality of reduction (either with a submeniscal arthrotomy or arthroscopically). After elevation and restoration of the joint line bone graft may be needed to support the elevated fragments. Screws can be placed in parallel just beneath the subchondral bone to hold up the elevated fragments well. These are sometimes referred to as ‘raft’ screws, describing the arrangement of parallel screws (Figure 31.16). The wedge of lateral condyle is then fixed with a buttress plate (Figure 31.17). Newer designs of anatomically contoured and angle-stable locking plates (using screws that lock into the plate) are available and increasingly used but are not always necessary. Early knee movement is encouraged after surgery to minimize joint stiffness.
TYPE 3 FRACTURES
The principles of treatment are similar to those applying to type 2 fractures. However, the fact that the lateral rim of the condyle is intact means that the knee is usually stable and a satisfactory outcome is more predictable. The depressed fragments may need to be elevated through a window in the metaphysis; reduction should be checked by X-ray or arthroscopy. The elevated fragments can be supported with
|
(a) |
(b) |
(c) |
(d) |
|
Figure 31.15 Tibial plateau fractures – imaging (a) X-rays provide information about the position of the main |
|||
|
fracture lines and areas of articular surface depression. (b,c) CT reconstructions reveal the extent and direction |
|||
926 |
of displacements, vital information for planning the operation. (d) The postoperative X-ray shows that reduc- |
|||
tion has been achieved. |
|
|
|
|
|
(b) |
(c) |
|
Figure 31.16 Raft screws (a–c) These cortical screws are inserted just beneath the subchondral surface and form a ‘raft’ above which the elevated fragments of the plateau are supported. In types 2, 5 or 6 injuries, they need to be supplemented by a buttress plate or can be performed through holes in a plate.
(a)
(a) |
(b) |
(c) |
(d) |
(e) |
Figure 31.17 Tibial plateau fractures – fixation (a) Two or three lag screws may be sufficient for simple split fractures (type 1), though (b) a buttress plate and screws may be more secure. (c) Depression of more than
5 mm in a type 3 fracture can be treated by elevation from below and (d) supported by bone grafts and fixation. (e) Type 2 fractures require a combination of both techniques – direct reduction, elevation of depressed areas, bone grafting and buttress plate fixation.
bone grafts and the whole segment is held with ‘raft’ screws.
TYPE 4 FRACTURES
Osteoporotic crush fractures of the medial plateau are difficult to reduce; in the long term the patient is likely to be left with some degree of varus deformity. The principles of treatment are the same as for type 2 fractures of the lateral plateau.
Medial condylar split fractures usually occur in younger people and are caused by high-energy trauma. The fracture itself is often more complex than is appreciated at first sight; there may be a second, posterior split in the coronal plane that cannot be
fixed through the standard anterior approach. Good lateral radiographs or CT scans are needed to define the fracture pattern. There may be an associated underlying ligament injury on the lateral side. Stable fixation of the medial side, along the lines described for the type 2 fracture, will then allow an assessment of the ligament injury. If the joint is unstable after fracture fixation, the torn structures on the lateral side may need repair.
TYPE 5 AND 6 FRACTURES
These are severe injuries that carry the added risk of a compartment syndrome. Surgical intervention with the aim of achieving stable internal fixation and early
31
leg and knee the of Injuries
927
3
TRAUMA
joint movement for these injuries is the goal, but surgery is not without significant risk. The danger is that the wide exposure necessary to gain access to both condyles may strip the supporting soft tissues, thus increasing the risk of wound breakdown and delayed union or non-union.
The current approach to management is provisional stabilization with splint, plaster or external fixator, and waiting for the soft-tissue conditions to improve – sometimes as long as 2–3 weeks. Then a double incision approach (anterior and posteromedial usually) is made, which provides access to the main fracture fragments and limits the amount of subperiosteal elevation carried out if both condyles are approached through a single anterior incision only.
The three-column theory for the management of these injuries based on CT fracture pattern has been recently proposed (lateral column, medial column
and posterior column). This provides an excellent strategy for planning surgical approach and fixation methods according to the columns involved and the fragments to be fixed (Figure 31.18). Fixation is most commonly then done using a combination of screws with locking plates and/or buttress plates with bone graft as required.
An alternative method is to perform the articular reduction through a limited surgical exposure (this can often be done percutaneously) and to stabilize the metaphysis to the diaphysis using a circular external fixator (Figure 31.19).
NOTE: Stability is all-important; no matter which method is used, fixation must be secure enough to permit early joint movement. There is little point in ending up with a pleasing X-ray and a stiff knee.
Figure 31.18 Complex tibial plateau fractures – internal fixation AP and lateral X-rays showing use of a lateral locking plate and a postero-medial buttress plate to address all three (anterolateral, anteromedial and posterior) columns involved in this injury. This requires two separate approaches through a lateral and a posteromedial skin incision.
Complications
EARLY
Compartment syndrome With closed type 4 and 5 fractures there is considerable bleeding and swelling of the leg – and a risk of developing a compartment syndrome. The leg and foot should be examined repeatedly for signs such as disproportionate pain on passive stretching of muscles which run through the compartment and distal neurological or vascular compromise.
LATE
Joint stiffness With severely comminuted fractures, and after complex operations, there is a considerable risk of developing a stiff knee. This is prevented by avoiding prolonged immobilization and encouraging movement as early as possible.
Deformity Some residual valgus or varus deformity is quite common – either because the fracture was incompletely reduced or because, although adequately reduced, the fracture became redisplaced during treatment. Fortunately, moderate deformity
Figure 31.19 Complex tibial plateau fractures – external fixation An alternative method. Rather than expose the joint formally in order to reduce the fracture, this can be done percutaneously, albeit with X-ray control, and the articular fragments held with screws and wires (a,b). The tibial metaphysis is then held to the shaft using a circular external fixator (c).
928 |
(a) |
(b) |
(c) |

is compatible with good function, although constant overloading of one compartment may predispose to osteoarthritis in later life.
Osteoarthritis If, at the end of treatment, there is marked depression of the plateau, or deformity of the knee or ligamentous instability, secondary osteoarthritis is likely to develop. This may subsequently require reconstructive/arthroplasty surgery.
TIBIA AND FIBULA SHAFT FRACTURES
Because of its subcutaneous position, the tibia is more commonly fractured, and more often sustains an open fracture (23.5% in one large study), than any other long bone. The commonest mechanisms are falls, sporting and transport accidents, with higher-energy mechanisms seen more commonly in younger patients.
whether the fracture is open or closed. Lowenergy breaks are typically closed or Gustilo I or II, and spiral. High-energy fractures are usually caused by direct trauma and tend to be open (Gustilo III A–C), transverse or comminuted.
•The stability of the fracture – Consider whether it will displace if weight-bearing is allowed. Long oblique fractures tend to shorten; those with a butterfly fragment tend to angulate towards the butterfly. Severely comminuted fractures are the least stable of all.
•The degree of contamination – In open fractures this is an important additional variable.
•Patient factors – Patient comorbidities, frailty, BMI, pre-morbid level of function, smoking status and psychosocial circumstances are also important in prognosis and hence decision making in these injuries.
Mechanism of injury
A twisting force causes a spiral fracture of both leg bones at different levels; an angulatory force produces transverse or short oblique fractures, usually at the same level.
Indirect injury is usually low-energy; with a spiral or long oblique fracture one of the bone fragments may pierce the skin from within.
Direct injury crushes or splits the skin over the fracture; this is usually a high-energy injury and the most common cause is a motorcycle accident.
Clinical features
The limb should be carefully examined for signs of soft-tissue damage: bruising, severe swelling, crushing or tenting of the skin, an open wound, circulatory changes, weak or absent pulses, diminution or loss of sensation and inability to move the toes. Any deformity should be noted before splinting the limb.
Always be on the alert for signs of an impending compartment syndrome.
X-rays
Pathological anatomy
The behaviour of these injuries – and therefore the choice of treatment – depends on the following factors:
•The state of the soft tissues – The risk of complications and the progress to fracture healing are directly related to the amount and type of soft-tissue damage. Closed fractures are best described using Tscherne’s method (Table 31.1); for open injuries, Gustilo’s grading is more useful (Table 31.2). The incidence of tissue breakdown and/or infection ranges from 1% for Gustilo type I to 30% for type IIIC.
•The severity of the bone injury – High-energy fractures are more damaging and take longer to heal than low-energy fractures; this is regardless of
Table 31.2 Gustilo’s classification of open fractures
The entire length of the tibia and fibula, as well as the knee and ankle joints, must be seen. The type of fracture, its level and the degree of angulation and displacement are recorded. Rotational deformity can
Table 31.1 Tscherne’s classification of skin lesions in closed fractures
Grade |
Skin lesion |
|
|
IC1 |
No skin lesion |
|
|
IC2 |
No skin laceration but contusion |
|
|
IC3 |
Circumscribed degloving |
|
|
IC4 |
Extensive, closed degloving |
|
|
IC5 |
Necrosis from contusion |
|
|
Grade |
Wound |
Soft-tissue injury |
Bone injury |
|
|
|
|
I |
<1 cm long |
Minimal |
Simple low-energy fractures |
|
|
|
|
II |
>1 cm long |
Moderate, some muscle damage |
Moderate comminution |
|
|
|
|
IIIA |
Usually >1 cm long |
Severe deep contusion; + compartment syndrome |
High-energy fracture patterns; comminuted |
|
|
|
but soft-tissue cover possible |
|
|
|
|
IIIB |
Usually >10 cm long |
Severe loss of soft-tissue cover |
Requires soft-tissue reconstruction for cover |
|
|
|
|
IIIC |
Usually >10 cm long |
As IIIB, with need for vascular repair |
Requires soft-tissue reconstruction for cover |
|
|
|
|
31
leg and knee the of Injuries
929
3be gauged by comparing the width of the tibiofibular interspace above and below the fracture.
Management
The main objectives are:
TRAUMA |
1 to limit soft-tissue damage and preserve (or restore, |
||
|
in the case of open fractures) skin cover |
||
2 |
to prevent – or at least recognize – a compartment |
||
|
syndrome |
|
|
|
|
|
|
|
3 |
to obtain and hold fracture alignment |
|
|
4 to start early weight-bearing |
(loading promotes |
|
|
|
healing) |
|
|
5 |
to start joint movements as soon as possible. |
|
|
LOW-ENERGY FRACTURES |
|
|
|
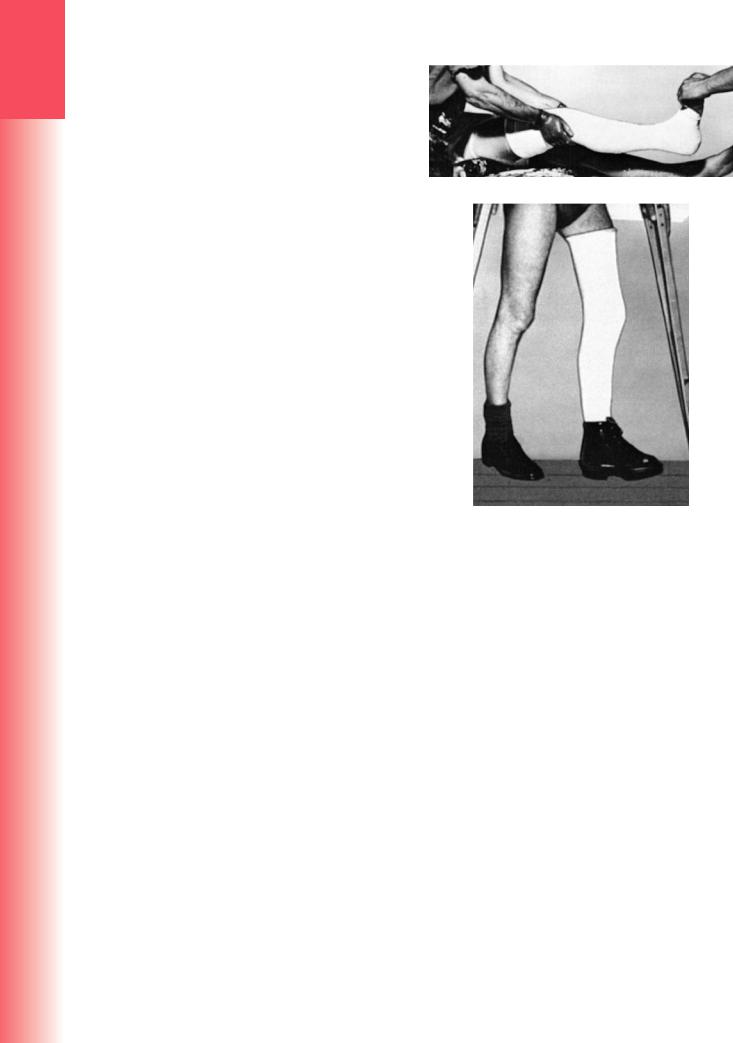
Low-energy fractures can in certain circumstances |
||
|
be treated by non-operative methods. If the fracture |
||
|
is undisplaced or minimally displaced, a full-length |
||
|
cast from upper thigh to metatarsal necks is applied |
||
|
with the knee slightly flexed and the ankle at a right |
||
|
angle (Figure 31.20). Displacement of the fibular |
||
|
fracture, unless it involves the ankle joint, is unim- |
||
|
portant and can be ignored. Apposition need not be |
||
|
complete but alignment must be near-perfect and |
||
|
rotation absolutely perfect. The position is checked by |
||
|
X-ray. Minor degrees of angulation can still be cor- |
||
|
rected by making a transverse cut in the plaster and |
||
|
wedging it into a better position. If there is excessive |
||
|
swelling, the cast is split. After 2 weeks the position |
||
|
is checked by X-ray. A change from an aboveto a |
||
|
below-the-knee cast is possible around 4–6 weeks, |
||
|
when the fracture becomes ‘sticky’. An alternative is |
||
|
a ‘Sarmiento’ cast which allows knee flexion but con- |
||
|
fers some additional stability. The cast is retained (or |
||
|
renewed if it becomes loose) until the fracture unites, |
||
|
which is around 8 weeks in children but seldom under |
||
|
12 weeks in adults. |
|
|
|
SURGICAL FIXATION METHODS |
|
|
|
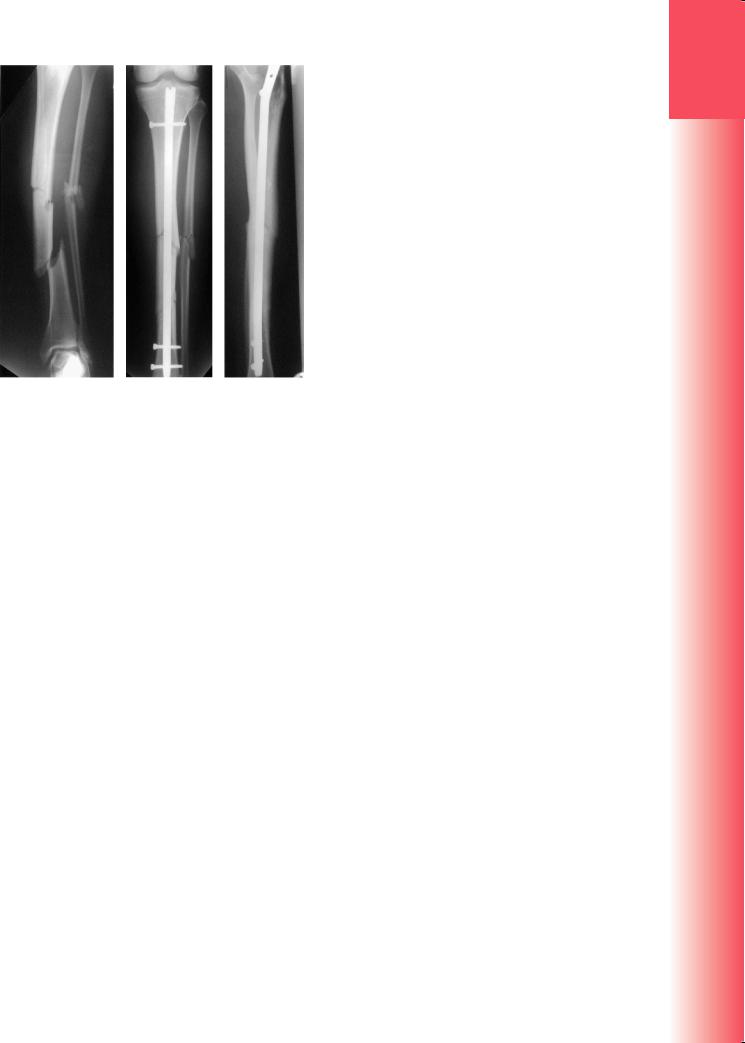
Closed intramedullary nailing |
This is the method |
|
|
of choice for internal fixation in most tibial shaft |
||
|
fractures. The fracture is reduced under X-ray con- |
||
|
trol and image intensification. The proximal end of |
||
|
the tibia is exposed; a guide-wire is passed down the |
||
|
medullary canal and the canal is reamed. A nail of |
||
|
appropriate size and shape is then introduced from |
||
|
the proximal end across the fracture site. Transverse |
||
|
locking screws are inserted at the proximal and distal |
||
|
ends (Figure 31.21). Postoperatively, partial weight- |
||
|
bearing is started as soon as possible, progressing to |
||
|
full weight-bearing when this is comfortable. |
||
|
|
For diaphyseal fractures, union can be expected in |
|
|
over 95% of cases. For metaphyseal fractures near the |
||
|
bone ends, the method is more technically demand- |
||
930 |
ing but, as techniques have evolved, it has become |
||
(a)
(b)
Figure 31.20 Fractured tibia and fibula – closed treatment (a) The position is held while an assistant applies plaster from the knee downwards. When the plaster has set, the leg is lifted and the above-knee plaster completed; note that the foot is plantigrade, the knee slightly bent and the plaster moulded round the patella. A rockered boot can be fitted for walking (b).
commonly performed and is an excellent way of managing these injuries. Care must be taken: there may be existing intra-articular extensions of metaphyseal fracture lines and there is the potential for propagation of a fracture into the joint when the nail is passed.
Plate fixation Plating can be used for metaphyseal fractures deemed unsuitable for nailing. It is also sometimes used for unstable tibial shaft fractures in children as it avoids the potential damage to the growth plate from passing an intramedullary nail through an open physis. Previously, the disadvantages of plate fixation included the need to expose the fracture site and, in so doing, stripping the soft tissues around the fracture, which could increase the risk of introducing infection and delaying union. Newer techniques of plating overcome these disadvantages. The plate is slid across the fracture through proximal and distal ‘access incisions’ on the anterolateral aspect
(a) |
(b) |
(c) |
Figure 31.21 Fractured tibia and fibula – intramedullary nailing Closed intramedullary nailing is now the preferred treatment for unstable tibial fractures. This series of X-rays shows the fracture before (a) and after (b,c) nailing. Active movements and partial weight-bearing were started soon after operation.
of the tibia and then fixed to the bone only at these levels. This method of ‘submuscular’ plating preserves the soft tissues around the fracture site better than conventional open plating, and it provides a relative stability that appears to hasten union. The soft tissues are still at risk using this technique, however, and considerable care is required in tissue handling to minimize the risk of wound complications.
External fixation This is a more rarely used alternative to closed nailing; it avoids exposure of the fracture site and allows further adjustments to be made if this should be needed. It has a particular role in long, segmental, multifragmentary fractures. Monolateral external fixation is most commonly used as a temporizing method of fixation in the context of an open injury in adults but can be used as a definitive method. It is more commonly used in children. Disadvantages include the need to span joints for sufficient stability, which can cause stiffness and the potential for pinsite infection. Circular external fixators confer greater stability and often negate the need to span joints (Figure 31.22). In both cases the tissues around the fracture are left undisturbed.
HIGH-ENERGY FRACTURES
Initially, the most important consideration is the viability of the damaged soft tissues and underlying
bone. Tissues around the fracture should be disturbed as little as possible.
Comminuted and segmental fractures, those associated with bone loss, and indeed any high-energy fracture that is inherently unstable, require early surgical stabilization. For closed fractures, most commonly this is done by intramedullary nailing hence the tissues around the fracture are left undisturbed.
In cases of bone loss, small defects can be treated by delayed bone grafting as required; limb salvage options for larger defects include either bone transport or compression-distraction (acute shortening to close the defect, with subsequent lengthening at a different level) with a circular external fixator (see Chapter 12).
OPEN FRACTURES
For open fractures, the use of internal fixation has to be accompanied by judicious and expert debridement and prompt cover of the exposed bone and implant; alternatively, initial temporary external (or internal) fixation can be safer if these prerequisites cannot be met and definitive fixation can be delayed until coverage can be achieved. In the UK all high-energy open fractures are managed in Major Trauma Centres where orthopaedic and plastic surgeons can jointly manage these injuries to provide the highest standards of care according to BOA Standards for Trauma (BOAST 4) guidelines.
A suitable mantra for the treatment of open tibial fractures is:
•antibiotics
•debridement
•stabilization
•prompt soft-tissue cover
•rehabilitation.
Antibiotics are started immediately. A firstor secondgeneration cephalosporin or co-amoxiclav is suitable in most cases and should be continued until softtissue closure or for a maximum of 72 hours, whichever is sooner. The evidence for prolonged antibiotic use is lacking. Good debridement of the fracture and prompt cover remain the strongest defence against infection.
The wound should be photographed on first inspection in the Emergency Department by medical photography or using a hospital-registered camera, and then covered with a sterile dressing. The photograph can then be printed for inclusion in the patient’s case notes to serve as a record and prevent further disturbance to the wound.
Adequate debridement is possible only if the original wound is extended. Wounds should be reviewed and discussed with plastic surgeons, especially if there appears to be a need for local or free skin or muscle flaps. Ideally the debridement should be performed
31
leg and knee the of Injuries
931

3
TRAUMA
Figure 31.22 Circular external fixation (a–d) This method of fixation offers the benefit of multilevel stability and can be carried out with little additional damage to the soft tissues around the injury.
(a) |
(b) |
(c) |
(d) |
|
jointly with the plastic surgeon. All dead and for- |
|
eign material is removed; this includes bone without |
|
significant soft-tissue attachments. The wound and |
|
fracture site are then washed out with large quanti- |
|
ties of normal saline. Gustilo grade I injuries can be |
|
closed primarily – being a low-energy injury with a |
|
small wound, closure should be possible without skin |
|
tension – and the fracture is then treated as for closed |
|
injuries. |
|
More severe wounds should, ideally, be closed or |
|
covered at primary surgery as long as the debridement |
|
has been thorough and the skills of a plastic surgeon |
|
are at hand. If there is tissue of doubtful viability that |
|
requires another look, or a local flap cover deemed |
|
to be inappropriate, a second planned operation is |
|
needed. This allows further debridement and, hope- |
|
fully, sufficient time to plan cover by free tissue trans- |
|
fer. Temporary cover of the exposed bone is often |
|
done using vacuum closure devices that can reduce |
|
oedema, improve local blood flow and encourage |
|
granulation tissue formation. |
|
It is important to stabilize the fracture. For |
|
Gustilo I, II and IIIA injuries, locked intramedul- |
|
lary nailing is permissible where definitive wound |
|
cover is possible at the time of debridement. For |
|
more severe grades of open tibial fracture, defini- |
|
tive fixation should be performed only at the time |
|
of definitive soft-tissue cover. If this is not feasible at |
|
the time of primary debridement, the fracture should |
|
be stabilized temporarily with a spanning external |
|
fixator or a temporary plate through the open defect. |
|
Exchange of the temporary fixation for an intramed- |
|
ullary nail can be done at the point when definitive |
932 |
soft-tissue cover is carried out – ideally within 5 days |
of the injury. |
POSTOPERATIVE MANAGEMENT
Swelling is common after tibial fractures; even after skeletal fixation the soft tissues continue to swell for several days. The limb should be elevated and frequent checks made for signs of compartment syndrome.
After intramedullary nailing of a transverse or short oblique fracture, weight-bearing can be started within a few days and increased to full weight when this is comfortable. If the fracture is comminuted or segmental, meaning that almost the entire load will be taken by the nail initially, only partial weightbearing is permitted until some callus is seen on X-ray.
Early complications
VASCULAR INJURY
Fractures of the proximal half of the tibia may damage the popliteal artery. This is an emergency of the first order, requiring exploration and repair. Damage to one of the two major tibial vessels may also occur and go unnoticed if there is no critical ischaemia.
COMPARTMENT SYNDROME
Tibial fractures – both open and closed – are among the commonest causes of compartment syndrome in the leg. The combination of tissue oedema and bleeding (oozing) causes swelling in the muscle compartments and this may precipitate ischaemia. Additional risk factors are proximal tibial fractures, severe crush injury, a long ischaemic period before revascularization (in type IIIC open fractures), a long delay to treatment, haemorrhagic shock, difficult and prolonged operation and a fracture fixed in distraction.
