
новая папка / Apley 938-988
.pdf
The diagnosis in most instances is a clinical one. Severe unremitting pain is the most important symptom. Additional warning symptoms are increasing pain, a feeling of tightness or ‘bursting’ in the leg and numbness in the leg or foot. These complaints should always be taken seriously and followed by careful and repeated examination for pain provoked by passive muscle stretching and loss of sensibility and/or muscle strength. Heightened awareness is all! Compartment pressure measurements can aid in diagnosis. This is particularly useful in patients who are unconscious or uncooperative, and those with multiple injuries. A split-tip 20-gauge catheter is introduced into the anterior compartment of the leg and the pressure is measured close to the level of the fracture. A differential pressure ( P) – the difference between diastolic pressure and compartment pressure – of less than 30 mmHg (4.00 kPA) is regarded as critical and an indication for compartment decompression. Ideally the pressure should be measured in all four compartments.
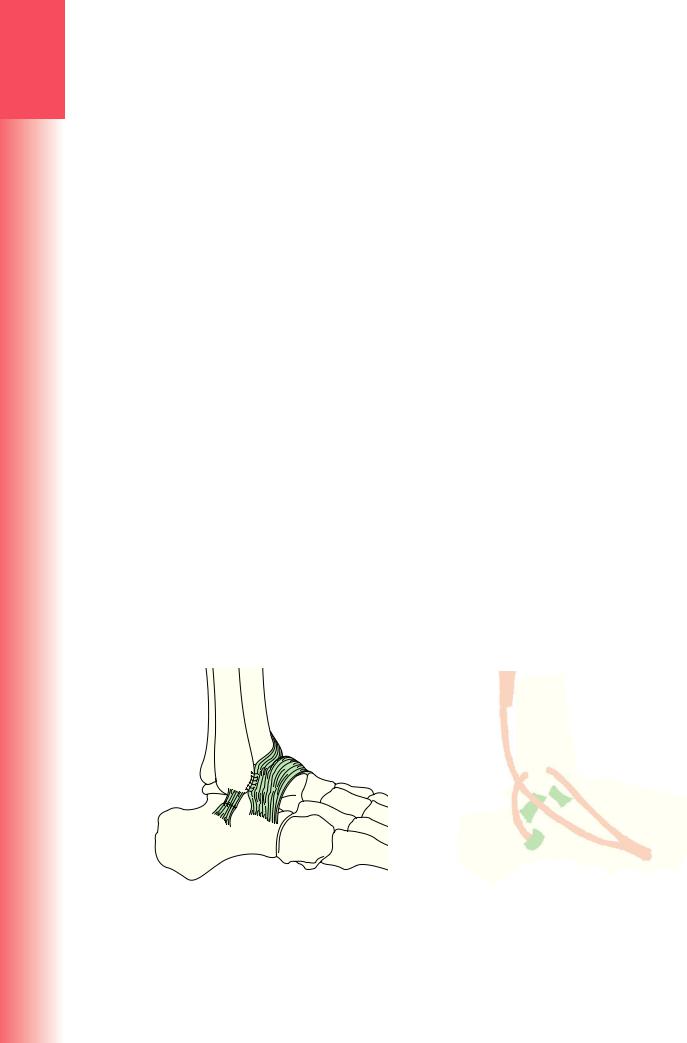
Fasciotomy and decompression Once the diagnosis is made, decompression of all four leg compartments should be carried out with the minimum delay. This is best and most safely accomplished through two incisions, one anterolateral and one posteromedial. The anterolateral incision is made about 2–3 cm lateral to the crest of the tibia and extends from the level of the tibial tuberosity to just above the ankle (Figure 31.23). The fascia is split along the length of the anterior and lateral compartments, taking care not to damage the superficial peroneal nerve. A second, similar incision is made just posterior to the posteromedial border of the tibia; the fascial covering of the superficial posterior compartment is split. The deep posterior compartment is identified just above the ankle and traced proximally; the muscle bulk of the superficial compartment needs to be retracted posteriorly, exposing the fascial envelope of the deep posterior compartment, which is likewise split down its entire length. Segmental arteries that perforate the fascia from the posterior tibial artery should be preserved for possible use in local skin flaps (Figure 31.24). The incisions are left open, a well-padded dressing is applied and the leg is splinted with the ankle in the neutral position. The fracture is treated as a grade III open injury requiring a spanning external fixator and prompt return for wound closure or skin grafting.
Outcome Compartment decompression within 6 hours of the onset of symptoms (or critical pressure measurement) should result in full recovery. Delayed decompression carries the risk of permanent dysfunction, the extent of which varies from mild sensory and motor loss to severe muscle and nerve damage, joint contractures and trophic changes in the foot.
Infection Open fractures are always at risk of infection; even a small perforation should be treated with respect and debridement carried out before the wound is closed.
If the diagnosis is suspected, wound swabs and blood samples should be taken. If debridement is required, deep tissue samples will aid microbiological diagnosis and antibiotic treatment should be withheld until samples have been taken. If not, then antibiotics should be started forthwith, using a ‘best guess’ intravenous preparation. Once the laboratory results are obtained, a more suitable antibiotic may be substituted.
With established infection, skeletal fixation should not be abandoned if the system is stable; infection control and fracture union are more likely if fixation is
(a) |
(b) |
(c)
Figure 31.23 Compartment syndrome (a) X-ray showing a complex proximal tibial fracture. All tibial fractures should be monitored for signs of compartment syndrome. Severe pain is the most important clinical feature. Regular clinical evaluation is important. (b) Swelling, blistering and skin necrosis associated with late, severe compartment syndrome that progressed quickly, unchecked underneath a complete plaster cast. (c) 4 compartment fasciotomies required in the context of lower limb compartment syndrome.
31
leg and knee the of Injuries
933

3
TRAUMA
Anterolateral |
Posterior tibial |
incision |
artery perforatoras |
|
exit on this |
|
line |
Tib. post. |
|
|
Extensors |
|
Medial |
and tib. |
|
incision |
ant. |
|
|
Peroneus |
|
Medial safe |
longus |
|
|
|
|
incision anterior to |
Safe lateral |
|
the posterior tibial |
Gast. |
artery and its |
|
incision |
med. |
perforators |
|
Gast. |
Soleus |
head |
|
|
|
|
|
|
|
lat. |
|
|
|
|
head |
|
|
|
Approximate sites of lateral |
|
|
Approximate |
Posterior tibial |
(peroneal) perforators |
|
|
sites of |
neurovascular |
|
Peroneal artery |
|
perforators |
bundle |
|
Plantaris |
FDL and FHL |
|
|
|
perforators exit |
|
|
|
|
on this line |
|
|
|
(a) |
(b) |
|
(c) |
|
Figure 31.24 Fasciotomies for compartment decompression (a) The first incision is usually anterolateral, giving access to the anterior and lateral compartments. But this is not enough. The superficial and deep posterior compartments also must be opened; their position is shown in (b), a cross-section of the leg. This requires a second incision (b,c), which is made a finger’s breadth behind the posteromedial border of the tibia; care must be taken not to damage the deep perforators of the posterior tibial artery. Note that the two incisions should be placed at least 7 cm apart so as to ensure a sufficient skin bridge without risk of sloughing.
secure. However, if there is a loose implant, it should be removed and replaced by external fixation.
Late complications
Malunion Slight shortening (up to 1.5 cm) is usually of little consequence, but rotation and angulation deformity, apart from being unsightly, can be disabling because the knee and ankle no longer move in the same plane.
Angulation should be prevented at all stages; anything more than 7 degrees in either plane is unacceptable. Angulation in the sagittal plane, especially if accompanied by a stiff equinus ankle, produces a marked increase in sheer forces at the fracture site during walking; this may result in either refracture or non-union.
Varus or valgus angulation will alter the axis of loading through the knee or ankle, causing increased stress in some part of the joint. This is often cited as a cause of secondary osteoarthritis; however, while this may be true for angular deformities close to the joint, long-term studies have failed to show that it applies to moderate deformities in the middle third of the bone.
Rotational alignment should be near-perfect (as compared with the opposite leg). This may be difficult to achieve with closed methods, but it should be possible with locked intramedullary nailing.
Late deformity, if marked, can be corrected by tibial osteotomy.
Delayed union High-energy fractures are slow to unite. If there is insufficient contact at the fracture site, either through bone loss or comminution, early ‘prophylactic’ bone grafting can be considered in high-risk patients. If there is a failure of union to progress on X-ray by 6 months, secondary intervention should be considered. The first nail is removed, the canal reamed and a larger nail inserted. If the fibula has united before the tibia, it should be osteotomized to allow better apposition and compression of the tibial fragments.
Non-union This may follow bone loss or deep infection, but a common cause is faulty treatment. Either the risks and consequences of delayed union have not been recognized, or splintage has been discontinued too soon, or the patient with a recently united fracture has walked with a stiff equinus ankle.
934

Hypertrophic non-union can be treated by intramedullary nailing (or exchange nailing) or compression plating. Atrophic non-union needs bone grafting in addition. If the fibula has united, a small segment should be excised so as to permit compression of the tibial fragments. Intractable cases may require radical Ilizarov techniques (Figure 31.25).
Joint stiffness Prolonged cast immobilization is liable to cause stiffness of the ankle and foot, which may persist for 12 months or longer in spite of active exercises. This can be avoided by changing to a functional brace as soon as it is safe to do so, usually by 4–6 weeks.
Osteoporosis Osteoporosis of the distal fragment is so common with all forms of treatment as to be regarded as a ‘normal’ consequence of tibial fractures. Axial loading of the tibia is important and weight-bearing should be re-established as soon as possible. After prolonged external fixation, special care should be taken to prevent a distal stress fracture.
Complex regional pain syndrome This is not uncommon in fractures of the distal third of the tibia. Exercises should be encouraged throughout the period of treatment. The management of the established condition is discussed in Chapter 10.
ISOLATED TIBIAL FRACTURES
A direct injury, such as a kick or blow with a club, may cause a transverse or slightly oblique fracture of the tibia alone at the site of impact. In children, the fracture is usually caused by an indirect injury; the fibula is intact or may show plastic deformation.
A fracture of the tibia alone takes just as long to unite as if both bones were broken, so at least 12 weeks is needed for consolidation and sometimes much longer.
Delayed union Isolated tibial fractures, especially in the lower third, may be slow to join and the temptation is to discard splintage too soon. Even slight displacement and loss of contact at the fracture level may delay union, so internal fixation is often preferred as primary treatment. This fracture also has a tendency to drift into varus in the later stages of healing; sometimes a fibular osteotomy is needed to allow correction of the deformity at surgery.
TIBIAL STRESS FRACTURES
Repetitive stress may cause a fatigue fracture of the tibia (usually in the upper half of the bone) or the fibula (most often in the lower third). This injury is seen in army recruits, mountaineers, runners and ballet dancers, who complain of pain in the leg. There is local tenderness and slight swelling. The condition may be mistaken for a chronic compartment syndrome.
X-rays
For the first 4 weeks there may be no visible radiographic signs, but a bone scan shows increased activity at the fracture site. After some weeks periosteal new bone may be seen, with a small transverse defect in the cortex.
There is a danger that these appearances may be mistaken for erosive bone lesion. If the diagnosis of stress fracture is kept in mind, such mistakes are unlikely.
Treatment
The patient is told to avoid the stressful activity. Usually after 8–10 weeks the symptoms settle down. A short leg gaiter can be applied for comfort during weight-bearing.
Figure 31.25 Fractured tibia and tibula –
late complications
(a) Hypertrophic nonunion: the exuberant callus formation and frustrated healing process are typical. (b) Atrophic non-union: there is very little sign of biological activity at the fracture site. (c) Malunion: treated, in this case, by gradual correction in an Ilizarov fixator (d,e).
(a) |
(b) |
(c) |
(d) |
(e) |
31
leg and knee the of Injuries
935

3
TRAUMA
FURTHER READING
Alford JW, Cole BJ. Cartilage restoration: techniques, outcomes and future directions. Am J Sports Med 2005; 33: 443–60.
Bourke HE, Gordon DJ, Salmon LJ, et al. The outcome at 15 years of endoscopic anterior cruciate ligament reconstruction using hamstring tendon autograft for ‘isolated’ anterior cruciate ligament rupture. J Bone Joint Surg Br 2012 May; 94(5): 630–7.
British Orthopaedic Association, British Association of Plastic, Reconstructive and Aesthetic Surgeons Standards for Trauma 2009. The management
of severe open lower limb fractures. J Bone Joint Surg Am 2012 Jun 20; 94: 1057e64. http://dx.doi. org/10.2106/JBJS.K. 00582.
Canadian Orthopaedic Trauma Society. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures: results of a multicenter, prospective, randomized clinical trial.
J Bone Joint Surg 2006; 88A: 2613–23.
Cramer KE, Moed BR. Patellar fractures: contemporary approach to treatment. J Am Acad Orthop Surg 1997; 5: 323–31.
Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am 1976; 58: 453e8.
Howells NR, Barnett A, Ahearn A, et al. Medial patellofemoral ligament reconstruction: prospective outcome assessment of a large single centre series.
J Bone Joint Surg Br 2012 Sep; 94(9).
Howells NR, Brunton LR, Robinson J, et al. Acute knee dislocation: an evidence based approach to the management of the multiligament-injured knee. Injury 2011; 42(2011): 1198–204.
Koval KJ, Helfet DL. Tibial plateau fractures: evaluation and treatment. J Am Acad Orthop Surg 1995; 3: 86–94.
LaPrade RF, Wentorf F. Diagnosis and treatment of posterolateral knee injuries. Clin Orthop Relat Res 2002; 402: 110–21.
Larson E, Lund PM. Ruptures of the extensor mechanism of the knee joint. Clin Orthop Relat Res 1986;
213: 150.
Levy BA, Dajani KA, Whelan DB, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy 2009; 2: 430–8.
Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma 2010 Nov; 24(11): 683–92.
Lyman S, Koulouvaris P, Sherman S, et al.
Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions and subsequent knee surgery.
J Bone Joint Surg Am 2009; 91: 2321.
Oestern H, Tscherne H. Pathophysiology and classification of soft tissue injuries associated with fractures. In: Tscherne H, Gotzen L (eds), Fractures with Soft Tissue Injuries. Berlin: Springer Verlag, 1984.
Upadhyay N, Wakeley C, Eldridge JD. Patellofemoral instability. Orthopaedics and Trauma Journal 2010;
24(2): 139–48.
936

Injuries of the ankle |
32 |
and foot |
|
|
|
Gavin Bowyer
INTRODUCTION
The foot and ankle act to both support and propel the body and are well adapted for these roles. During running and jumping, loads well in excess of 10 times the body weight are transmitted through the ankle and foot. If this loading is excessive, or excessively repeated, it can lead to foot and ankle injuries.
The ankle is a close-fitting hinge-like joint in which the two parts interlock like a mortise (the box formed by the distal ends of the tibia and fibula) and tenon (the upward projecting talus). The mortise bones are held together as a syndesmosis by the distal (inferior) tibiofibular and interosseous ligaments, and the talus is prevented from slipping out of the mortise by the medial and lateral collateral ligaments and joint capsule. The peroneal tendons provide additional stability, as active resistors of inversion.
The ankle rotates only in one plane (flexion/extension), but with a complex axis of rotation, actually rolling forward as the talus goes into plantar flexion; sideways movement is prevented by the malleolar buttresses and the collateral ligaments, but the bony constraint lessens as the ankle flexes. If the talus is forced to tilt or rotate, something must give: the ligaments, the malleoli or both. Movements of the talus into internal or external rotation come about from a rotatory force upon the foot, or more commonly inversion/supination of the foot, which, through the orientation of the subtalar joint, causes external rotation of the talus. Whenever a fracture of the malleolus is seen, it is important to assess the associated ligament injury.
ANKLE LIGAMENT INJURIES
Ankle sprains are the most common of all sportsrelated injuries, accounting for over 25% of cases. They are probably even more common in pedestrians and country walkers who stumble on stairways, pavements and potholes.
In more than 75% of cases it is the lateral ligament complex that is injured, in particular the anterior talofibular and calcaneofibular ligaments. Medial ligament injuries are usually associated with a fracture or joint injury.
A sudden twist of the ankle momentarily tenses the structures around the joint. This may amount to no more than a painful wrenching of the soft tissues – what is commonly called a sprained ankle. If more severe force is applied, the ligaments may be strained to the point of rupture. With a partial tear, some of the ligament remains intact and, once it has healed, it is able to stabilize the joint. With a complete tear, the ligament may still heal but it might not regain its original form and length; the joint will potentially be unstable (Figure 32.1).
Functional anatomy
The lateral collateral ligaments consist of the anterior talofibular, the posterior talofibular and (between them) the calcaneofibular ligaments. The anterior talofibular ligament (ATFL) runs almost horizontally from the anterior edge of the lateral malleolus to the neck of the talus; it is relaxed in dorsiflexion and tense in plantarflexion. In plantarflexion the ligament essentially changes its orientation from horizontal with respect to the floor to almost vertical. Thus the ligament at greatest stretch, and most vulnerable, with the foot plantar-flexed is the ATFL – hence the propensity for ATFL injury with the plantar-flexed, inverting, foot (e.g. down a pothole, off a kerb). The calcaneofibular ligament runs from the tip of the lateral malleolus to the posterolateral part of the calcaneum, thus it helps also to stabilize the subtalar joint. Maximum tension is produced by inversion and dorsiflexion of the ankle. The posterior talofibular ligament runs from the posterior border of the lateral malleolus to the posterior part of the talus.
The medial collateral (deltoid) ligament consists of superficial and deep portions. The superficial fibres spread like a fan from the medial malleolus as far anteriorly as

3
TRAUMA
Anterior Posterior talofibular talofibular
|
Calcaneofibular |
(a) |
(b) |
(d) |
(e) |
the navicular and inferiorly to the calcaneum and talus. Its chief function is to resist eversion of the hindfoot. The deep portion is intra-articular, running directly from the medial malleolus to the medial surface of the talus. Its principal effect is to prevent external rotation of the talus. The combined action of restraining eversion and external rotation makes the deltoid ligament a major stabilizer of the ankle.
The distal tibiofibular joint is held by four ligaments: the anterior, posterior, inferior transverse and interosseous ‘ligament’, which is really a thickened part of the interosseous membrane. This strong ligament complex still permits some movement at the tibiofibular joint during flexion and extension of the ankle.
|
Figure 32.1 Ankle ligament |
|
|
injuries (a) Schematic diagram |
|
|
showing the mortise-and-tenon |
|
|
articulation and main ligaments |
|
|
of the ankle. (b) The three com- |
|
|
ponents of the lateral collateral |
|
|
ligament. (c) The commonest |
|
|
injury is a partial tear of one or |
|
|
other component of the lateral |
|
(c) |
ligament. Following a complete |
|
tear, the talus may be displaced |
||
|
||
|
in the ankle mortise; the |
|
|
tibiofibular ligament may have |
|
|
ruptured as well, shown here in |
|
|
somewhat exaggerated form. |
|
|
(d) Stress X-ray showing talar |
|
|
tilt. (e,f) X-rays demonstrating |
|
|
anteroposterior instability. |
|
|
Pulling the foot forward under |
|
|
the tibia causes the talus to |
|
(f) |
shift appreciably at the ankle |
|
joint; this is usually seen after |
||
|
||
|
recurrent sprains. |
is only faint and slow to appear, it is probably a sprain; if bruising is marked and the patient is unable to put any weight on the foot, this suggests a more severe injury. In an ATFL sprain, tenderness is maximal just distal and slightly anterior to the lateral malleolus. The slightest attempt at passive inversion of the ankle is extremely painful. It is impossible to test for abnormal mobility in the acute phase without using local or general anaesthesia.
With all ankle injuries it is essential to examine the entire leg and foot; undisplaced fractures of the fibula or the tarsal bones, or even the fifth metatarsal bone are easily missed and injuries of the distal tibiofibular joint and the peroneal tendon sheath cause features that mimic those of a lateral ligament strain.
|
Pathology |
|
The common ‘twisted ankle’ is due to unbalanced load- |
|
ing with the ankle inverted and plantarflexed. First the |
|
ATFL and then the calcaneofibular ligament is strained; |
|
sometimes the talocalcaneal ligaments are also injured. |
|
If fibres are torn, there is bleeding into the soft tissues. |
|
The tip of the malleolus may be avulsed and in some |
|
cases the peroneal tendons are injured. There may be a |
|
small fracture of an adjacent tarsal bone or (on the lateral |
|
side) the base of the fifth metatarsal. |
|
ACUTE INJURY OF LATERAL LIGAMENTS |
|
Clinical features |
|
A history of a twisting injury followed by pain and |
938 |
swelling could suggest anything from a minor sprain |
to a fracture. If the patient is able to walk and bruising |
Imaging
About 15% of ankle sprains reaching the Emergency Department are associated with an ankle fracture. This complication can be excluded by obtaining an X-ray, but there are doubts as to whether all patients with ankle injuries should be subjected to X-ray examination. More than 20 years ago The Ottawa Ankle Rules were developed to assist in making this decision. X-ray examination is called for if there is: (1) pain around the malleolus; (2) inability to take weight on the ankle immediately after the injury; (3) inability to take four steps in the Emergency Department;
(4) bone tenderness at the posterior edge or tip of the medial or lateral malleolus or the base of the fifth metatarsal bone.
If X-ray examination is considered necessary, anteroposterior, lateral and ‘mortise’ (30-degree oblique) views of the ankle should be obtained.

Localized soft-tissue swelling and, in some cases, a small avulsion fracture of the tip of the lateral malleolus or the anterolateral surface of the talus may be the only corroborative signs of a lateral ligament injury. However, it is important to exclude other injuries, such as an undisplaced fibular fracture or diastasis of the tibiofibular syndesmosis. If tenderness extends onto the foot, or if swelling is so severe that the area cannot be properly examined, additional X-rays of the foot are essential.
Persistent inability to weight-bear over 1 week should call for re-examination and review of all the initial ‘negative’ X-rays. For patients who have had persistent pain, swelling, instability and impaired function over 6 weeks or longer – despite appropriate early treatment – magnetic resonance imaging (MRI) or computed tomography (CT) will be required to assess the extent of soft-tissue injury or subtle bony changes.
Functional treatment, i.e. ‘protected mobilization’, leads to earlier recovery of all grades of injury – without jeopardizing stability – than either rigid immobilization or early operative treatment.
OPERATIVE TREATMENT
If the ankle does not start to settle within 1–2 weeks of starting RICE, further review and investigation are called for. Persistent problems at 12 weeks after injury, despite physiotherapy, may signal the need for operative treatment. Residual complaints of ankle pain and stiffness, a sensation of instability or giving way and intermittent swelling are suggestive of cartilage damage or impinging scar tissue within the ankle. Arthroscopic repair or ligament substitution is now effective in many cases, allowing a return to full function and sports.
Treatment
NON-OPERATIVE TREATEMENT
Initial treatment consists of rest, ice, compression and elevation (RICE), which is continued for 1–3 weeks depending on the severity of the injury and the response to treatment. Cold compresses should be applied for about 20 minutes every 2 hours, and after any activity that exacerbates the symptoms.
More recently the acronym has been extended to ‘PRICE’ by adding protection (crutches, splint or brace) and still further to ‘PRICER’, adding rehabilitation (supported return to function). The principles remain the same – a phased approach, to support the injured part during the first few weeks and then allow early mobilization and a supported return to function. An advice leaflet for patients is probably helpful.
The use of non-steroidal anti-inflammatory drugs (NSAIDs) in the acute phase can be helpful, with the usual contraindications and caveats. There is evidence that in acute injuries topical non-steroidal antiinflammatory gels or creams might be as beneficial as oral preparations, probably with a better risk profile.
RECURRENT LATERAL INSTABILITY
Recurrent sprains are potentially associated with cartilage damage, and warrant careful investigation by MRI, arthroscopy and examination under anaesthesia.
Clinical features
The patient gives a history of a ‘sprained ankle’ that never quite seems to recover and is followed by recurrent ‘giving way’ or a feeling of instability when walking on uneven surfaces. This is said to occur in about 20% of cases after acute lateral collateral ligament tears.
The ankle looks normal and passive movements are full, but stress tests for abnormal lateral ligament laxity may show either excessive talar tilting in the sagittal plane or anterior displacement (an anterior drawer sign) in the coronal plane (Figure 32.2). In the chronic phase these tests are painless and can be performed either manually or with the use of special mechanical stress devices. Both ankles are tested, so as to allow comparison of the abnormal with the normal side.
Figure 32.2 Recurrent lateral instability – special tests (a) Anterior drawer test: When the heel is drawn forwards under the tibia, the abnormally lax ligaments allow the talus to displace anteri-
>5 mm orly. (b) Talar tilt test: Forcibly inverting the ankle causes the talus to tilt abnormally in the mortise. For both tests comparison with the normal side is
important.
> 10 degrees
32
foot and ankle the of Injuries
939
(a) |
(b) |
3
TRAUMA
Talar tilt test With the ankle held in the neutral position, the examiner stabilizes the tibia by grasping the leg with one hand above the ankle; the other hand is then used to force the heel into maximum inversion. The range of movement can be estimated clinically and compared with that of the normal ankle. The exact degree of talar tilt can also be measured by X-rays, which should be taken with the ankles in 30 degrees of internal rotation (mortise views); 15 degrees of talar tilt (or 5 degrees more than in the normal ankle) is regarded as abnormal. Inversion laxity suggests injury to both the calcaneofibular and anterior talofibular ligaments.
Anterior drawer test The patient should be sitting with the knee flexed to 90 degrees and the ankle in 10 degrees of plantarflexion. The lower leg is stabilized with one hand while the other hand forces the patient’s heel forward under the tibia. In a positive test the talus can be felt sliding forwards and backwards. The position of the talus is verified by lateral X-rays; anterior displacement of 10 mm (or 5 mm more than on the normal side) indicates abnormal laxity of the ATFL. With an isolated tear of the ATFL, the anterior drawer test may be positive in the absence of abnormal talar tilt. (Note: A positive anterior drawer test can sometimes be obtained in normal, asymptomatic individuals; the finding should always be considered in conjunction with other symptoms and signs).
Treatment
Recurrent ‘giving way’ can sometimes be prevented by modifying footwear, raising the outer side of the heel and extending it laterally. More effectively, the secondary dynamic ankle stabilizers, the peronei, can be strengthened and brought into play by specific
physiotherapy regimes. Ankle exercises to strengthen the peroneal muscles are helpful, and a light brace can be worn during vigorous activities that stress the ankle.
If, in spite of these measures, the patient continues to experience mechanical instability (true giving way) during everyday activities, reconstruction of the lateral ligament should be considered. More commonly the persisting problem will be functional instability, in which the patient does not trust the ankle, and there are recurrent episodes in which the patient has rapidly or suddenly to unload the ankle, probably because of inhibitory feedback from the injured ankle.
Most patients with functional instability can be improved and returned to sport by arthroscopic debridement of the impinging tissue within the ankle joint, followed by physiotherapy.
Various operations for mechanical stabilization are described; they fall mainly into two groups:
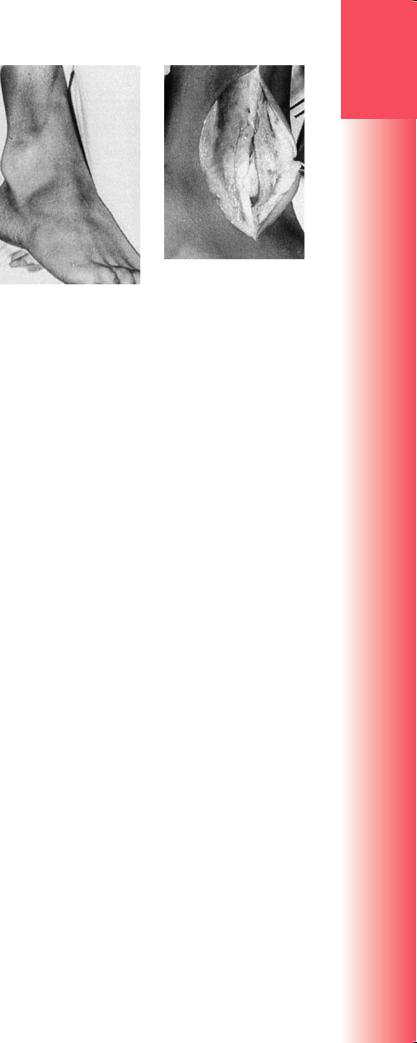
(1) those that aim to repair or tighten the ligaments; and (2) those that are designed to construct a ‘checkrein’ against the unstable movement. The Broström– Karlsson or Gould operation is an example of the first type: the anterior talofibular and calcaneofibular ligaments are exposed and repaired, usually by an overlapping – or ‘double-breasting’ – technique (Figure 32.3a). In the second type of operation a substitute ligament is constructed by using peroneus brevis to act as a tenodesis and prevent sudden movements into varus (the Chrisman operation) (Figure 32.3b). The disadvantages of the non-anatomical reconstructions are that they sacrifice or partially sacrifice the secondary stabilizers, the peroneal tendons.
There are various post-operative regimes that aim to protect the repair but allow an early, supported, return to activity. These might involve a plaster cast
|
(a) |
(b) |
|
Figure 32.3 Recurrent lateral instability – operative treatment (a) The lax anterior talofibular and calcaneofibu- |
|
|
lar ligaments can be reinforced by a double-breasting technique (the Boström–Karlsson operation). (b) Another |
|
940 |
way of augmenting the lateral ligament is to re-route part of the peroneus brevis tendon so that is acts as a |
|
check-rein (tenodesis) (the Chrisman operation). |
|
|
but more commonly now use a special supportive boot (the ‘moon boot’). Sometimes a removable brace is worn as the patient returns to active exercise and sports. The brace can usually be discarded after 3 months but it may need to be used from time to time for sports activities.
DELTOID LIGAMENT TEARS
Rupture of the deltoid ligament is usually associated with either a fracture of the distal end of the fibula or tearing of the distal tibiofibular ligaments (or both). The effect is to destabilize the talus and allow it to move into eversion and external rotation. The diagnosis is made by imaging: there is widening of the medial joint space in the mortise view; sometimes the talus is tilted, and diastasis of the tibiofibular joint may be obvious.
When there is a deltoid ligament or medial malleolar injury but no apparent lateral disruption at the ankle, it is important to look for a fracture or dislocation of the proximal fibula – the highly unstable
Maisoneuve injury.
Treatment
Provided the medial joint space is completely reduced, the ligament will heal. The fibular fracture or diastasis must be accurately reduced, if necessary by open reduction and internal fixation. Occasionally the medial joint space cannot be reduced; it should then be explored in order to free any soft tissue trapped in the joint. A below-knee cast or support boot is applied with the foot plantigrade and is retained for 8 weeks.
DISLOCATION OF PERONEAL TENDONS
Acute dislocation of the peroneal tendons may accompany – or may be mistaken for – a lateral ligament strain. Telltale signs on X-ray are an oblique fracture of the lateral malleolus (the so-called ‘rim fracture’) or a small flake of bone lying lateral to the lateral malleolus (avulsion of the retinaculum). Treatment in a below-knee cast, or similar support/immobilization in a brace or boot, for 6 weeks will help in a proportion of cases; the majority will complain of residual symptoms.
Recurrent subluxation or dislocation is unmistakable; the patient can demonstrate that the peroneal tendons dislocate forwards over the fibula during dorsiflexion and eversion (Figure 32.4). Treatment is operative and is based on the observation that the attachment of the retinaculum to the periosteum on the front of the fibula has come adrift, creating a pouch into which the tendons displace. Using nonabsorbable sutures through drill holes in the bone,
(b)
(a)
Figure 32.4 Dislocation of peroneal tendons (a) On movement of the ankle, the peroneal tendons slip forwards over the lateral malleolus. (b) The anterior part of the retinaculum is being reconstructed.
the normal anatomy is recreated. An alternative approach is to modify the morphology of the distal fibula, posteriorly translating a shelf of bone to constrain the tendons mechanically in a deepened posterior channel. Whichever method of stabilization is used, it is important also to assess the state of the tendons themselves, as an associated longitudinal split tear is commonly found, and this will lead to continuing pain and dysfunction around the lateral border of the ankle if it is not repaired.
TEARS OF INFERIOR TIBIOFIBULAR
LIGAMENTS
The inferior tibiofibular ligaments may be torn, allowing partial or complete separation of the tibiofibular joint (diastasis). Complete diastasis, with tearing of both the anterior and posterior fibres, follows a severe abduction strain. Partial diastasis, with tearing of only the anterior fibres, is due to an external rotation force. These injuries may occur in isolation, but they are usually associated with fractures of the malleoli or rupture of the collateral ligaments.
Clinical features
Following a twisting injury, the patient complains of pain in the front of the ankle. There is swelling and marked tenderness directly over the inferior tibiofibular joint. A ‘squeeze test’ has been described by Hopkinson and colleagues: when the leg is firmly compressed some way above the ankle, the patient experiences pain over the syndesmosis. Be sure, though, to exclude a fracture before carrying out the test.
32
foot and ankle the of Injuries
941

3X-rays
|
With a partial tear the fibula usually lies in its normal |
|
|
position and the X-ray looks normal. With a complete |
|
|
tear the tibiofibular joint is separated and the ankle |
|
TRAUMA |
mortise is widened; sometimes this becomes apparent |
|
only when the ankle is stressed in abduction. There |
||
|
||
|
may be associated fractures of the distal tibia or fibula, |
|
|
or an isolated fracture more proximally in the fibula. |
|
|
Treatment |
|
|
Partial tears can be treated by strapping the ankle |
|
|
firmly or bracing for 2–3 weeks. Thereafter exercises |
|
|
are encouraged. |
|
|
Complete tears are best managed by internal fixa- |
|
|
tion with a transverse screw just above the joint. This |
|
|
must be done as soon as possible so that the tibiofib- |
|
|
ular space does not become clogged with organizing |
|
|
haematoma and fibrous tissue. If the patient is seen |
|
|
late and the ankle is painful and unstable, open clear- |
|
|
ance of the syndesmosis and transverse screw fixa- |
|
|
tion may be warranted. The ankle is immobilized in |
|
|
plaster for 8 weeks or similar support and off-loading |
|
|
is used, after which the screw is removed. However, |
|
|
some degree of instability usually persists. |
MALLEOLAR FRACTURES OF
THE ANKLE
Fractures and fracture – dislocations of the ankle are common. Most are low-energy fractures of one or both malleoli, usually caused by a twisting mechanism. Less common are the more severe fractures involving the tibial plafond, the pilon fractures, which are high-energy injuries, often caused by a fall from a height.
In malleolar injuries, the patient usually presents with a history of a twisting injury, usually with the ankle going into inversion, followed by immediate pain, swelling and difficulty weight-bearing. Bruising often comes out soon after injury.
One such injury was described by Percival Pott in 1768, and the group as a whole was for a long time referred to as Pott’s fracture – although, as with many eponyms, he was not the first to notice or describe it, and what became known by this eponym was not what he described anyway!
|
The most obvious injury is a fracture of one or |
|
both malleoli; often, though, the ‘invisible’ part of |
|
the injury – rupture of one or more ligaments – is just |
|
as serious. |
|
Mechanism of injury |
|
The patient stumbles and falls. Usually the foot is |
942 |
anchored to the ground while the body lunges for- |
ward. The ankle is twisted and the talus tilts and/or |
rotates forcibly in the mortise, causing a low-energy fracture of one or both malleoli, with or without associated injuries of the ligaments. If a malleolus is pushed off, it usually fractures obliquely; if it is pulled off, it fractures transversely. The precise fracture pattern is determined by: (1) the position of the foot;
(2) the direction of force at the moment of injury. The foot may be either pronated or supinated and the force upon the talus is towards adduction, abduction or external rotation, or a combination of these.
Pathological anatomy
There is no completely satisfactory classification of ankle fractures. Lauge-Hansen in the 1950s grouped these injuries according to the likely position of the foot and the direction of force at the moment of fracture. This is useful as a guide to the method of reduction (reverse the pathological force); it also gives a pointer to the associated ligament injuries. However, some people find this classification overly complicated. (For a detailed description the reader is referred to the original 1950 paper by Lauge-Hansen).
A simpler classification is that of Danis and Weber, which focuses on the fibular fracture.
•Type A – is a transverse fracture of the fibula below the tibiofibular syndesmosis, perhaps associated with an oblique or vertical fracture of the medial malleolus. This is almost certainly an adduction (or adduction and internal rotation) injury.
•Type B – is an oblique fracture of the fibula in the sagittal plane (and therefore better seen in the lateral X-ray) at the level of the syndesmosis; often there is also an avulsion injury on the medial side (a torn deltoid ligament or fracture of the medial malleolus). This is probably an external rotation injury and it may be associated with a tear of the ATFL.
•Type C – is a more severe injury, above the level of the syndesmosis, which means that the tibiofibular ligament and part of the interosseous membrane must have been torn. This is due to severe abduction or a combination of abduction and external rotation. Associated injuries are an avulsion fracture of the medial malleolus (or rupture of the medial collateral ligament), a posterior malleolar fracture and diastasis of the tibiofibular joint.
Clinical features
Ankle fractures are seen in sportsmen and sportswomen, as well as those who catch their foot, twist and fall in day-to-day activities; an older group includes women with postmenopausal osteoporosis who trip and fall.
A history of a twisting injury, followed by intense pain and inability to stand on the leg suggests
