
новая папка / Operative Standards for Cancer Surgery Volume I 1st Edition
.pdf
radiographic or clinical features suspicious for persistent atelectasis or pneumonia. In addition, careful assessment of cough and vocal cord function should be performed before the patient transitions to a solid diet, as aspiration of food into the remaining lung can be a devastating postoperative event. Vocal cord dysfunction is more likely after left pneumonectomy given the location of the left recurrent nerve in the left chest near the lung hilum. Placement of a nasoenteric tube for nutrition and/or vocal cord injection should be considered for patients exhibiting signs and symptoms of aspiration.
P.175
Bronchopleural Fistula and Empyema
Postpneumonectomy empyema with or without bronchopleural fistula (BPF) can be a devastating complication
with significant mortality.27 Intraoperative techniques that decrease BPF risk include avoiding excessive dissection and devascularization of the bronchial stump, minimizing the bronchial stump length to prevent secretion pooling and subsequent stump breakdown, and reinforcing the bronchial stump with muscle or a
pleural flap.28,29 BPF should be suspected in patients who have fever, empyema, aspiration pneumonia, an excessively productive cough, or an increasing air leak or amount of pleural air after lung resection. Evaluation for BPF should include bronchoscopy and possibly CT in stable patients. Acute management of BPF focuses on controlling life-threatening conditions and includes postural drainage with the affected lung positioned downward in cases of airway flooding, early pleural drainage to prevent sepsis and aspiration pneumonia, and appropriate antibiotic therapy. Adequate nutrition is critical. Successful BPF treatment ultimately requires closure of the fistula, adequate drainage, and eventual obliteration of the chest cavity.
Postpneumonectomy Pulmonary Edema
Postpneumonectomy pulmonary edema is a syndrome of rapidly progressive dyspnea and hypoxemia requiring mechanical ventilation, with radiologic studies showing diffuse interstitial edema in the remaining lung and no
identifiable cause such as heart failure, pulmonary embolism, pneumonia, or BPF.30 This complication typically develops 2 or 3 days postoperatively, occurs in 1.1% to 4.5% of pneumonectomy patients, and has a mortality
rate of 40% to 100%.25,28,30,31 Some studies have identified perioperative fluid overload and right-sided pneumonectomy as risk factors. Prophylaxis against this complication includes the use of a balanced pleural drainage system, treatment of perioperative hypotension and low urine output with vasopressor or inotropic agents, and diuretic therapy with minimal fluid administration. Treatment is supportive.
REFERENCES
1.Bousamra M II, Presberg KW, Chammas JH, et al. Early and late morbidity in patients undergoing pulmonary resection with low diffusion capacity. Ann Thorac Surg 1996;62(4):968-974; discussion 974-975.
2.Ferguson MK, Little L, Rizzo L, et al. Diffusing capacity predicts morbidity and mortality after pulmonary resection. J Thorac Cardiovasc Surg 1988;96(6):894-900.
3.Morice RC, Peters EJ, Ryan MB, et al. Exercise testing in the evaluation of patients at high risk for complications from lung resection. Chest 1992;101(2):356-361.
4.Walsh GL, Morice RC, Putnam JB Jr, et al. Resection of lung cancer is justified in high-risk patients selected by exercise oxygen consumption. Ann Thorac Surg 1994;58(3):704-710; discussion 711.
5.Berry MF, Worni M, Wang X, et al. Sleeve lobectomy for non-small cell lung cancer with N1 nodal disease
does not compromise survival. Ann Thorac Surg 2014;97(1):230-235.
6.Gaissert HA, Keum DY, Wright CD, et al. POINT: operative risk of pneumonectomy-influence of preoperative induction therapy. J Thorac Cardiovasc Surg 2009;138(2):289-294.
7.Mansour Z, Kochetkova EA, Ducrocq X, et al. Induction chemotherapy does not increase the operative risk of pneumonectomy! Eur J Cardiothorac Surg 2007;31(2):181-185.
8.Weder W, Collaud S, Eberhardt WE, et al. Pneumonectomy is a valuable treatment option after neoadjuvant therapy for stage III non-small-cell lung cancer. J Thorac Cardiovasc Surg 2010;139(6):14241430.
P.176
9. Albain KS, Swann RS, Rusch VW, et al. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small-cell lung cancer: a phase III randomised controlled trial. Lancet
2009;374(9687):379-386.
10. van Meerbeeck JP, Kramer GW, Van Schil PE, et al. Randomized controlled trial of resection versus radiotherapy after induction chemotherapy in stage IIIA-N2 non-small-cell lung cancer. J Natl Cancer Inst
2007;99(6):442-450.
11.Qu X, Huang X, Yan W, et al. A meta-analysis of (1)(8)FDG-PET-CT, (1)(8)FDG-PET, MRI and bone scintigraphy for diagnosis of bone metastases in patients with lung cancer. Eur J Radiol 2012;81(5):10071015.
12.Inada K, Kishimoto S. An anomalous tracheal bronchus to the right upper lobe; report of two cases. Dis Chest 1957;31(1):109-112.
13.Ritsema GH. Ectopic right bronchus: indication for bronchography. AJR Am J Roentgenol
1983;140(4):671-674.
14.Ma Z, Dong A, Fan J, et al. Does sleeve lobectomy concomitant with or without pulmonary artery reconstruction (double sleeve) have favorable results for non-small cell lung cancer compared with pneumonectomy? A meta-analysis. Eur J Cardiothorac Surg 2007;32(1):20-28.
15.Ferguson MK, Lehman AG. Sleeve lobectomy or pneumonectomy: optimal management strategy using decision analysis techniques. Ann Thorac Surg 2003;76(6):1782-1728.
16.Shi W, Zhang W, Sun H, et al. Sleeve lobectomy versus pneumonectomy for non-small cell lung cancer: a meta-analysis. World J Surg Oncol 2012;10:265.
17.Deslauriers J, Gregoire J, Jacques LF, et al. Sleeve lobectomy versus pneumonectomy for lung cancer: a comparative analysis of survival and sites or recurrences. Ann Thorac Surg 2004;77(4):1152-1156; discussion 1156.
18.Balduyck B, Hendriks J, Lauwers P, et al. Quality of life after lung cancer surgery: a prospective pilot study comparing bronchial sleeve lobectomy with pneumonectomy. J Thorac Oncol 2008;3(6):604-608.
19.Ilonen IK, Räsänen JV, Sihvo EI, et al. Pneumonectomy: post-operative quality of life and lung function. Lung Cancer 2007;58(3):397-402.
20.Bryant AS, Cerfolio RJ, Minnich DJ. Survival and quality of life at least 1 year after pneumonectomy. J Thorac Cardiovasc Surg 2012;144(5):1139-1145.
21.Cerfolio RJ, Bryant AS, Jones VL, et al. Pulmonary resection after concurrent chemotherapy and high dose (60Gy) radiation for non-small cell lung cancer is safe and may provide increased survival. Eur J Cardiothorac Surg 2009;35(4):718-723; discussion 723.
22.Blank RS, Hucklenbruch C, Gurka KK, et al. Intraoperative factors and the risk of respiratory complications after pneumonectomy. Ann Thorac Surg 2011;92(4):1188-1194.
23.Shapiro M, Swanson SJ, Wright CD, et al. Predictors of major morbidity and mortality after pneumonectomy utilizing the Society for Thoracic Surgeons General Thoracic Surgery Database. Ann Thorac Surg 2010;90(3):927-934; discussion 934-935.
24.Grillo HC, Shepard JA, Mathisen DJ, et al. Postpneumonectomy syndrome: diagnosis, management, and results. Ann Thorac Surg 1992;54(4):638-650; discussion 650-651.
25.Licker M, Spiliopoulos A, Frey JG, et al. Risk factors for early mortality and major complications following pneumonectomy for non-small cell carcinoma of the lung. Chest 2002;121(6): 1890-1897.
26.Patel RL, Townsend ER, Fountain SW. Elective pneumonectomy: factors associated with morbidity and operative mortality. Ann Thorac Surg 1992;54(1):84-88.
27.Hollaus PH, Lax F, el-Nashef BB, et al. Natural history of bronchopleural fistula after pneumonectomy: a review of 96 cases. Ann Thorac Surg 1997;63(5):1391-1396; discussion 1396-1397.
28.Bernard A, Deschamps C, Allen MS, et al. Pneumonectomy for malignant disease: factors affecting early morbidity and mortality. J Thorac Cardiovasc Surg 2001;121(6):1076-1082.
29.Deschamps C, Bernard A, Nichols FC III, et al. Empyema and bronchopleural fistula after pneumonectomy: factors affecting incidence. Ann Thorac Surg 2001;72(1):243-247; discussion 248.
30.Deslauriers J, Aucoin A, Gregoire J. Postpneumonectomy pulmonary edema. Chest Surg Clin N Am
1998;8(3):611-631, ix.
31. Turnage WS, Lunn JJ. Postpneumonectomy pulmonary edema. A retrospective analysis of associated variables. Chest 1993;103(6):1646-1650.

Editorial
As the first comprehensive, evidence-based evaluation of standardized surgical practices for several key malignancies, this manual represents a critically important initiative. The lung section, written by expert contributors in our field, describes numerous important principles for the optimal conduct of lung cancer surgery and will serve as a premiere guide to operative management of our lung cancer patients.
As highlighted in the “Introduction” chapter of the “Lung” section, lung cancer remains an enormous public health problem. It is currently the number one cause of cancer-related mortality in the United States for both men and women. Accounting for more predicted deaths than malignancies of the breast, prostate, colon and rectum, and pancreas combined, lung cancer continues to take an enormous toll—in terms of both health care expenses and lives lost. Our ability to provide broad curative therapy for this disease is significantly limited by the preponderance of advanced and inoperable lung cancer at the time of presentation. For this reason, extensive efforts have been put forth in recent years to identify early staged lung cancer through improved screening and to expand our treatment options for those with advanced disease, utilizing novel therapeutic agents and targeted therapy.
For those patients with early staged non-small cell lung cancer (NSCLC), complete surgical resection remains the standard of care. However, despite the efficacy of surgical therapy for early-stage disease, there exists significant variability in overall and disease-free survival following surgical resection. We, as surgeons, should be driven to ensure that those patients who are fortunate enough to receive surgical therapy all undergo optimal oncologic procedures, with minimal variability in postoperative outcome.
There may be a number of reasons contributing to variability in surgical outcomes. From our perspective, there are several key parameters. Although it is not specifically addressed in the chapters that follow, surgeon training and expertise are of critical importance. There is ample evidence that resections for lung cancer performed by fully trained and board-certified thoracic surgeons are associated with better outcomes and reduced cost. Patient selection must be thoughtful, appropriate, and conducted with full consideration of the range of multimodality therapies available and their relative risks and benefits for each patient. Staging must be accurate in the preoperative, operative, and pathologic settings. Resections should be precisely stage-specific and complete. Finally, but of significant importance, in order to minimize variability in outcomes and optimize survival for our patients, regardless of the operating surgeon and institution, a key set of standardized, clearly defined operative procedures must be utilized. In providing a standardized approach to operative management of patients with lung cancer, these chapters serve as an informative guide to the practicing thoracic surgeon, the surgical trainee, and all professionals clinically involved in lung cancer care.
This manual was created utilizing input from some of the most experienced experts in our field, with meticulous attention to evidence-based best practices. Critical elements are presented in great detail, with additional attention directed
P.178 toward addressing areas of controversy that merit further investigation and ongoing evaluation through clinical trials. As a key collaborative effort between the American College of Surgeons and the National Cancer Institute, the value of this publication in standardizing practices cannot be overstated. This manual should serve as a living document as we move into the future, amenable to change as new data and techniques become available. In conjunction with further efforts to standardize cancer care for our patients, these chapters help us, as surgeons, take a huge leap toward providing consistent cancer care.
Mara B. Antonoff, MD
G. Alexander Patterson, MD

Department of Thoracic and Cardiovascular Surgery
University of Texas MD Anderson Cancer Center
Houston, TX
Division of Cardiothoracic Surgery
Washington University School of Medicine
St. Louis, MO
P.179
Lung Cancer Critical Elements of Synoptic
Preresection Staging
None
EBUS
EUS
Cervical mediastinoscopy
VATS/thoracotomy
Chamberlain
Preresection Nodal Staging (with Diagnostic Lymphoid Tissue)
N/A
Right nodal stations |
Left nodal stations |
2 |
2 |
4 |
4 |
7 |
5 |
8 |
6 |
9 |
7 |
10 |
8 |
Other N1 |
9 |
|
10 |
Other N1
Nodal Evaluation at Time of Resection
Systematic sampling |
Nodal dissection |
|
|
Nodal Stations Examined at Time of Resection
N/A
Right nodal stations |
Left nodal stations |
2 |
2 |
4 |
4 |
7 |
5 |
8 |
6 |
9 |
7 |
10 |
8 |
Other N1 |
9 |
|
10 |
|
Other N1 |
Method of Lung Resection
VATS |
Thoracotomy Robot assisted |
|
|
Extent of Lung Resection
|
|
|
|
Wedge |
Segmentectomy |
Lobectomy |
Pneumonectomy |
resection |
|
|
Component of non-anatomic resection as part of anatomic |
yes |
no |
|
|
resection |
|
||
|
|
|
|
|
|
|
|
|
|

Introduction
Localized pancreatic ductal adenocarcinoma (PDAC) was once considered a uniquely surgical problem. Staging of PDAC was routinely accomplished in the operating room; patients found to have technically removable tumors upon exploration underwent pancreatectomy, and those who were not found to have removable tumors underwent palliative bypass operations. Radical resections involving wide clearance of soft tissues and the
mesenteric vasculature1 and/or total pancreatectomy2 were often advocated as a means to control local
recurrence and distant progression. Perioperative mortality was common,3 and adjuvant therapy was not
routine.4 Although longterm survival was distinctly rare, it was never observed in the absence of a potentially
curative pancreatectomy.5 Therefore, despite generally discouraging results, surgery became accepted as the only potentially curative therapy for patients with an otherwise uniformly fatal disease.
Although PDAC remains a considerable clinical problem, the perioperative management of patients with localized disease has changed significantly over the past 35 years. Advances in multidisciplinary treatment programs that emphasize highquality pretreatment staging, meticulous surgical care, and perioperative adjuvant therapies have collectively provided a basis for optimism; now, as many as one-quarter of patients who receive combination therapy with chemotherapy with or without chemoradiation and pancreatectomy can expect to live 5 years or
longer.6 However, among the treatments administered as part of these multimodality programs, surgery remains the only one that is potentially curative on its own. Therefore, although localized PDAC is no longer considered a uniquely surgical condition, resection of the primary pancreatic tumor and regional lymph nodes remains as important today as it was 35 years ago.
Staging
In the 1970s and 1980s, accurate pretreatment staging of PDAC was impossible because only low-resolution cross-sectional imaging technologies were available at that time. Discrimination between localized and disseminated disease and between resectable and nonresectable primary tumors was therefore largely made in the operating room at exploratory surgery. Cross-sectional imaging has now improved to the point at which the primary tumor’s anatomy and relationship to the mesenteric vasculature can be determined radiographically with great precision, and metastatic disease can be safely ruled out in the majority of patients. Furthermore, studies correlating radiographic findings to surgical outcomes have led to the establishment of objective staging designations that reflect the surgeon’s likelihood of achieving a margin-negative resection.
Pretreatment staging with computed tomography or magnetic resonance imaging is now used to help optimize
and individualize the treatment of patients with localized PDAC (Table I-1 and Fig. I-1).7,8,9,10 Locally advanced disease is represented radiographically as the cancer’s extensive involvement of the mesenteric vasculature. Complete resection of the primary cancer to microscopically clear margins (R0 resection) is rarely feasible for patients with this stage of disease, and attempts to use neoadjuvant therapy to reduce the size or anatomic
extent of such cancers and thus improve the surgeon’s ability to remove them have been unsuccessful.11
Therefore, patients with locally advanced cancers are typically treated with chemotherapy
P.183
and/or chemoradiation. At the other end of the spectrum, potentially resectable cancers on computed tomography scans appear to be separate from the mesenteric vasculature or approximate the vessels only minimally, and such tumors can routinely be resected safely to negative margins, so surgery is generally
recommended as the initial therapeutic approach.12 Finally, borderline resectable tumors radiographically appear to approximate the mesenteric vasculature to a limited degree. Patients with these tumors are at high risk for at
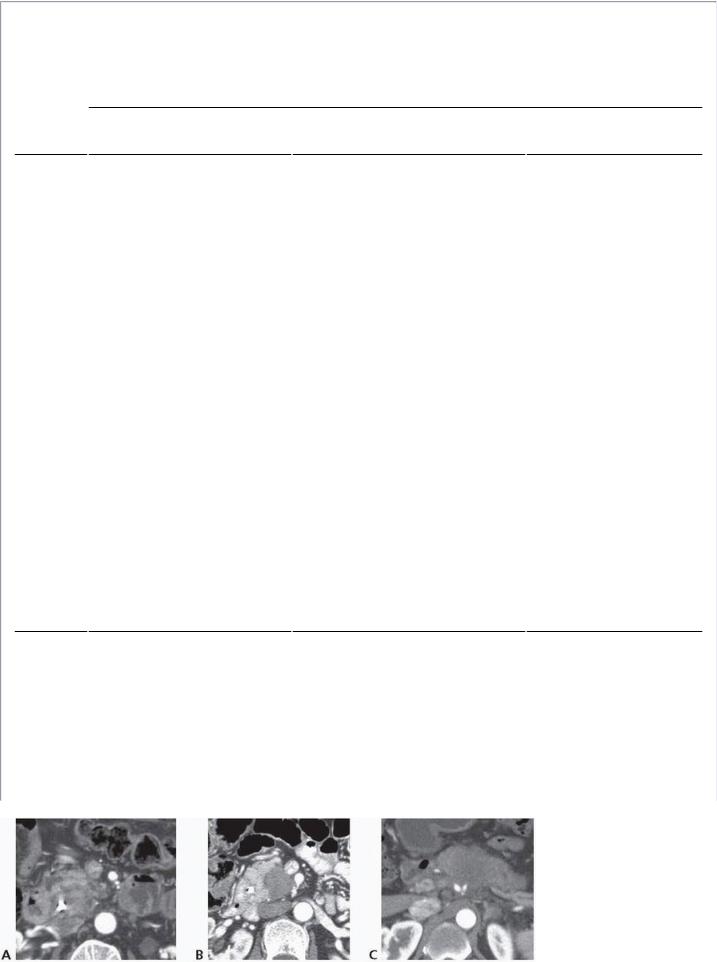
least microscopically incomplete (R1) resection.10
TABLE I-1 Staging Designations Used for Patients with Localized Pancreatic Cancer
Staging Designation
Vessel |
Potentially Resectable |
Borderline Resectable |
Locally Advanced |
SMV- |
No interface or interface |
Interface between the tumor and |
Unreconstructable |
PV |
between the tumor and |
vessel measuring ≥180° of the |
occlusion of the vessel |
|
vessel measuring <180° of |
circumference of the vessel wall |
by the tumor |
|
the circumference of the |
and/or reconstructible occlusion |
|
|
vessel wall |
|
|
SMA |
No interface |
Interface between the tumor and |
Interface between the |
|
|
vessel measuring <180° of the |
tumor and vessel |
|
|
circumference of the vessel wall |
measuring ≥180° of the |
|
|
|
circumference of the |
|
|
|
vessel wall |
CHA |
No interface |
Reconstructible, short-segment |
Unreconstructable |
|
|
interface between the tumor and |
interface between the |
|
|
vessel of any degree |
tumor and vessel |
Celiac |
No interface |
Interface between the tumor and |
trunk |
|
vessel measuring <180° of the |
|
|
circumference of the vessel wall |
Interface between the tumor and vessel measuring ≥180° of the circumference of the vessel wall
CHA, common hepatic artery; SMA, superior mesenteric artery; SMV-PV, superior mesenteric vein-portal vein.
From Katz MH, Marsh R, Herman JM, et al. Borderline resectable pancreatic cancer: need for standard ization and methods for optimal clinical trial design. Ann Surg Oncol 2013;20(8):2787-2795, with permission.
FIGURE I-1 Radiographic examples of resectable (A), borderline resectable (B), and locally advanced (C)

primary tumors. A: The primary tumor (T) is separated from the superior mesenteric vein, superior mesenteric artery, and aorta by a plane of fat. B: The primary tumor has an interface with the superior mesenteric artery measuring < 180° of the circumference of the vessel wall. C: The primary tumor has interfaces with the splenic artery, common hepatic artery, and celiac trunk that each measure ≥180° of the circumferences of the respective vessels’ walls.
P.184 Preoperative therapy is therefore recommended for patients with borderline resectable cancers prior to planned
surgical resection.7 Because the initial treatment recommended to each patient with localized PDAC depends on the radiographic stage of the primary tumor, precise preoperative imaging and its accurate clinical interpretation by the surgeon, preferably in the context of a multidisciplinary conference or clinic, now represents the primary
objective of the pretreatment workup.13
Operative Management and Outcomes
The fundamental technical elements of pancreatoduodenectomy and distal pancreatectomy for cancer are
essentially identical to those employed in operations performed in the first part of the 20th century.14,15
Nonetheless, patients who undergo pancreatic resection today benefit from improvements in perioperative
management that have occurred in high-volume centers over the past 3 decades.16 The bases for these improvements are many and include, but certainly are not limited to, better patient selection for surgery, better surgical training, centralization of care to highvolume surgeons and hospitals, improvements in the ability to
rescue from perioperative complications, and advances in perioperative anesthesia and medicine.17,18,19 The reduction in perioperative morbidity and mortality is all the more notable as surgeons attempt increasingly complex operations requiring venous and even arterial resection and reconstruction, thereby expanding the role of potentially curative therapy to patients previously considered to have unresectable—and therefore incurable—
disease.20 Furthermore, recent major advances in minimally invasive surgical techniques and equipment now facilitate the complex surgical maneuvers required as part of pancreatoduodenectomy and distal pancreatectomy to be performed without the morbidity of a major abdominal incision, which may translate into further reductions
in surgical morbidity and mortality and increases in quality and quantity of life.21
Adjuvant and Neoadjuvant Therapy
Although the propensity for PDAC to recur both locally and systemically—even following R0 resection of a nodenegative tumor—has been recognized as long as operations for PDAC have been performed, the results of the
first major trial of postoperative therapy for pancreatic cancer were only published in 1985.22 Systemic chemotherapy following potentially curative resection, which offers better progression-free and overall survival relative to surgery alone, now represents the standard of care, and rates of its administration are increasing
nationwide.23,24 Favorable anecdotal reports that the administration of chemotherapy and/or chemoradiation prior to surgery may improve selection for surgery, reduce rates of margin-positive and node-positive resection, and prolong overall survival following resection have led to increasing interest in administering chemotherapy
and/or chemoradiation prior to, instead of following, pancreatectomy.25 Although many remain resistant to using this approach for patients with resectable tumors owing to a fear of preoperative disease progression that would eliminate the possibility for potentially curative surgery, neoadjuvant treatment strategies are now the preferred
approach for patients with borderline resectable cancers.26 Furthermore, the recent approval of two novel
chemotherapeutic regimens, FOLFIRINOX (folinic acid, fluorouracil, irinotecan, oxaliplatin)27 and gemcitabine-
nab-paclitaxel,28 have given hope that the relatively favorable results observed with
