
- •Hematuria II: causes and investigation
- •Hematospermia
- •Lower urinary tract symptoms (LUTS)
- •Nocturia and nocturnal polyuria
- •Flank pain
- •Urinary incontinence in adults
- •Genital symptoms
- •Abdominal examination in urological disease
- •Digital rectal examination (DRE)
- •Lumps in the groin
- •Lumps in the scrotum
- •2 Urological investigations
- •Urine examination
- •Urine cytology
- •Radiological imaging of the urinary tract
- •Uses of plain abdominal radiography (KUB X-ray—kidneys, ureters, bladder)
- •Intravenous pyelography (IVP)
- •Other urological contrast studies
- •Computed tomography (CT) and magnetic resonance imaging (MRI)
- •Radioisotope imaging
- •Post-void residual urine volume measurement
- •3 Bladder outlet obstruction
- •Regulation of prostate growth and development of benign prostatic hyperplasia (BPH)
- •Pathophysiology and causes of bladder outlet obstruction (BOO) and BPH
- •Benign prostatic obstruction (BPO): symptoms and signs
- •Diagnostic tests in men with LUTS thought to be due to BPH
- •Why do men seek treatment for their symptoms?
- •Watchful waiting for uncomplicated BPH
- •Medical management of BPH: combination therapy
- •Medical management of BPH: alternative drug therapy
- •Minimally invasive management of BPH: surgical alternatives to TURP
- •Invasive surgical alternatives to TURP
- •TURP and open prostatectomy
- •Indications for and technique of urethral catheterization
- •Indications for and technique of suprapubic catheterization
- •Management of nocturia and nocturnal polyuria
- •High-pressure chronic retention (HPCR)
- •Bladder outlet obstruction and retention in women
- •Urethral stricture disease
- •4 Incontinence
- •Causes and pathophysiology
- •Evaluation
- •Treatment of sphincter weakness incontinence: injection therapy
- •Treatment of sphincter weakness incontinence: retropubic suspension
- •Treatment of sphincter weakness incontinence: pubovaginal slings
- •Overactive bladder: conventional treatment
- •Overactive bladder: options for failed conventional therapy
- •“Mixed” incontinence
- •Post-prostatectomy incontinence
- •Incontinence in the elderly patient
- •Urinary tract infection: microbiology
- •Lower urinary tract infection
- •Recurrent urinary tract infection
- •Urinary tract infection: treatment
- •Acute pyelonephritis
- •Pyonephrosis and perinephric abscess
- •Other forms of pyelonephritis
- •Chronic pyelonephritis
- •Septicemia and urosepsis
- •Fournier gangrene
- •Epididymitis and orchitis
- •Periurethral abscess
- •Prostatitis: presentation, evaluation, and treatment
- •Other prostate infections
- •Interstitial cystitis
- •Tuberculosis
- •Parasitic infections
- •HIV in urological surgery
- •6 Urological neoplasia
- •Pathology and molecular biology
- •Prostate cancer: epidemiology and etiology
- •Prostate cancer: incidence, prevalence, and mortality
- •Prostate cancer pathology: premalignant lesions
- •Counseling before prostate cancer screening
- •Prostate cancer: clinical presentation
- •PSA and prostate cancer
- •PSA derivatives: free-to-total ratio, density, and velocity
- •Prostate cancer: transrectal ultrasonography and biopsies
- •Prostate cancer staging
- •Prostate cancer grading
- •General principles of management of localized prostate cancer
- •Management of localized prostate cancer: watchful waiting and active surveillance
- •Management of localized prostate cancer: radical prostatectomy
- •Postoperative course after radical prostatectomy
- •Prostate cancer control with radical prostatectomy
- •Management of localized prostate cancer: radical external beam radiotherapy (EBRT)
- •Management of localized prostate cancer: brachytherapy (BT)
- •Management of localized and radiorecurrent prostate cancer: cryotherapy and HIFU
- •Management of locally advanced nonmetastatic prostate cancer (T3–4 N0M0)
- •Management of advanced prostate cancer: hormone therapy I
- •Management of advanced prostate cancer: hormone therapy II
- •Management of advanced prostate cancer: hormone therapy III
- •Management of advanced prostate cancer: androgen-independent/ castration-resistant disease
- •Palliative management of prostate cancer
- •Prostate cancer: prevention; complementary and alternative therapies
- •Bladder cancer: epidemiology and etiology
- •Bladder cancer: pathology and staging
- •Bladder cancer: presentation
- •Bladder cancer: diagnosis and staging
- •Muscle-invasive bladder cancer: surgical management of localized (pT2/3a) disease
- •Muscle-invasive bladder cancer: radical and palliative radiotherapy
- •Muscle-invasive bladder cancer: management of locally advanced and metastatic disease
- •Bladder cancer: urinary diversion after cystectomy
- •Transitional cell carcinoma (UC) of the renal pelvis and ureter
- •Radiological assessment of renal masses
- •Benign renal masses
- •Renal cell carcinoma: epidemiology and etiology
- •Renal cell carcinoma: pathology, staging, and prognosis
- •Renal cell carcinoma: presentation and investigations
- •Renal cell carcinoma: active surveillance
- •Renal cell carcinoma: surgical treatment I
- •Renal cell carcinoma: surgical treatment II
- •Renal cell carcinoma: management of metastatic disease
- •Testicular cancer: epidemiology and etiology
- •Testicular cancer: clinical presentation
- •Testicular cancer: serum markers
- •Testicular cancer: pathology and staging
- •Testicular cancer: prognostic staging system for metastatic germ cell cancer
- •Testicular cancer: management of non-seminomatous germ cell tumors (NSGCT)
- •Testicular cancer: management of seminoma, IGCN, and lymphoma
- •Penile neoplasia: benign, viral-related, and premalignant lesions
- •Penile cancer: epidemiology, risk factors, and pathology
- •Squamous cell carcinoma of the penis: clinical management
- •Carcinoma of the scrotum
- •Tumors of the testicular adnexa
- •Urethral cancer
- •Wilms tumor and neuroblastoma
- •7 Miscellaneous urological diseases of the kidney
- •Cystic renal disease: simple cysts
- •Cystic renal disease: calyceal diverticulum
- •Cystic renal disease: medullary sponge kidney (MSK)
- •Acquired renal cystic disease (ARCD)
- •Autosomal dominant (adult) polycystic kidney disease (ADPKD)
- •Ureteropelvic junction (UPJ) obstruction in adults
- •Anomalies of renal ascent and fusion: horseshoe kidney, pelvic kidney, malrotation
- •Renal duplications
- •8 Stone disease
- •Kidney stones: epidemiology
- •Kidney stones: types and predisposing factors
- •Kidney stones: mechanisms of formation
- •Evaluation of the stone former
- •Kidney stones: presentation and diagnosis
- •Kidney stone treatment options: watchful waiting
- •Stone fragmentation techniques: extracorporeal lithotripsy (ESWL)
- •Intracorporeal techniques of stone fragmentation (fragmentation within the body)
- •Kidney stone treatment: percutaneous nephrolithotomy (PCNL)
- •Kidney stones: open stone surgery
- •Kidney stones: medical therapy (dissolution therapy)
- •Ureteric stones: presentation
- •Ureteric stones: diagnostic radiological imaging
- •Ureteric stones: acute management
- •Ureteric stones: indications for intervention to relieve obstruction and/or remove the stone
- •Ureteric stone treatment
- •Treatment options for ureteric stones
- •Prevention of calcium oxalate stone formation
- •Bladder stones
- •Management of ureteric stones in pregnancy
- •Hydronephrosis
- •Management of ureteric strictures (other than UPJ obstruction)
- •Pathophysiology of urinary tract obstruction
- •Ureter innervation
- •10 Trauma to the urinary tract and other urological emergencies
- •Renal trauma: clinical and radiological assessment
- •Renal trauma: treatment
- •Ureteral injuries: mechanisms and diagnosis
- •Ureteral injuries: management
- •Bladder and urethral injuries associated with pelvic fractures
- •Bladder injuries
- •Posterior urethral injuries in males and urethral injuries in females
- •Anterior urethral injuries
- •Testicular injuries
- •Penile injuries
- •Torsion of the testis and testicular appendages
- •Paraphimosis
- •Malignant ureteral obstruction
- •Spinal cord and cauda equina compression
- •11 Infertility
- •Male reproductive physiology
- •Etiology and evaluation of male infertility
- •Lab investigation of male infertility
- •Oligospermia and azoospermia
- •Varicocele
- •Treatment options for male factor infertility
- •12 Disorders of erectile function, ejaculation, and seminal vesicles
- •Physiology of erection and ejaculation
- •Impotence: evaluation
- •Impotence: treatment
- •Retrograde ejaculation
- •Peyronie’s disease
- •Priapism
- •13 Neuropathic bladder
- •Innervation of the lower urinary tract (LUT)
- •Physiology of urine storage and micturition
- •Bladder and sphincter behavior in the patient with neurological disease
- •The neuropathic lower urinary tract: clinical consequences of storage and emptying problems
- •Bladder management techniques for the neuropathic patient
- •Catheters and sheaths and the neuropathic patient
- •Management of incontinence in the neuropathic patient
- •Management of recurrent urinary tract infections (UTIs) in the neuropathic patient
- •Management of hydronephrosis in the neuropathic patient
- •Bladder dysfunction in multiple sclerosis, in Parkinson disease, after stroke, and in other neurological disease
- •Neuromodulation in lower urinary tract dysfunction
- •14 Urological problems in pregnancy
- •Physiological and anatomical changes in the urinary tract
- •Urinary tract infection (UTI)
- •Hydronephrosis
- •15 Pediatric urology
- •Embryology: urinary tract
- •Undescended testes
- •Urinary tract infection (UTI)
- •Ectopic ureter
- •Ureterocele
- •Ureteropelvic junction (UPJ) obstruction
- •Hypospadias
- •Normal sexual differentiation
- •Abnormal sexual differentiation
- •Cystic kidney disease
- •Exstrophy
- •Epispadias
- •Posterior urethral valves
- •Non-neurogenic voiding dysfunction
- •Nocturnal enuresis
- •16 Urological surgery and equipment
- •Preparation of the patient for urological surgery
- •Antibiotic prophylaxis in urological surgery
- •Complications of surgery in general: DVT and PE
- •Fluid balance and management of shock in the surgical patient
- •Patient safety in the operating room
- •Transurethral resection (TUR) syndrome
- •Catheters and drains in urological surgery
- •Guide wires
- •JJ stents
- •Lasers in urological surgery
- •Diathermy
- •Sterilization of urological equipment
- •Telescopes and light sources in urological endoscopy
- •Consent: general principles
- •Cystoscopy
- •Transurethral resection of the prostate (TURP)
- •Transurethral resection of bladder tumor (TURBT)
- •Optical urethrotomy
- •Circumcision
- •Hydrocele and epididymal cyst removal
- •Nesbit procedure
- •Vasectomy and vasovasostomy
- •Orchiectomy
- •Urological incisions
- •JJ stent insertion
- •Nephrectomy and nephroureterectomy
- •Radical prostatectomy
- •Radical cystectomy
- •Ileal conduit
- •Percutaneous nephrolithotomy (PCNL)
- •Ureteroscopes and ureteroscopy
- •Pyeloplasty
- •Laparoscopic surgery
- •Endoscopic cystolitholapaxy and (open) cystolithotomy
- •Scrotal exploration for torsion and orchiopexy
- •17 Basic science of relevance to urological practice
- •Physiology of bladder and urethra
- •Renal anatomy: renal blood flow and renal function
- •Renal physiology: regulation of water balance
- •Renal physiology: regulation of sodium and potassium excretion
- •Renal physiology: acid–base balance
- •18 Urological eponyms
- •Index

470 CHAPTER 11 Infertility
Etiology and evaluation of male infertility
Definition of infertility
Infertility is failure of conception after at least 12 months of unprotected intercourse. The chance of a normal couple conceiving is estimated at 20–25% per month, 75% by 6 months, and 90% at 1 year. Up to 50% of infertility is due to male factors. Up to 25% of couples may be affected at some point in their reproductive years.
Pathophysiology
Failure of fertilization of the normal ovum is due to defective sperm development, function, or inadequate numbers. There may be abnormalities of morphology (teratospermia) or motility (asthenospermia), low sperm numbers (oligospermia), combined disorders (oligoasthenospermia), or absent sperm (azoospermia).
Abnormal epididymal function may result in defective spermatozoa maturation or transport, or induce cell death.
Etiology
•Idiopathic (25%)
•Varicocele (present in 40%)
•Cryptorchidism (undescended testes)
•Functional sperm disorders: immunological infertility (sperm antibodies); head or tail defects; Kartagener’s syndrome (immotile cilia); dyskinetic cilia syndrome
•Erectile or ejaculatory problems
•Testicular injury: orchitis (postpubertal, bilateral mumps orchitis); testicular torsion; trauma; radiotherapy
•Endocrine disorders: Kallmann’s syndrome (isolated gonadotrophin deficiency causing hypogonadism and anosmia); Prader–Willi syndrome (hypogonadism, short stature, hyperphagia, obesity); pituitary gland adenoma, radiation, or infection
•Hormone excess: excess prolactin (pituitary tumor); excess androgen (adrenal tumor, congenital adrenal hyperplasia, anabolic steroids); excess estrogens
•Genetic disorders: Kleinfelter’s syndrome (47XXY) involves azoospermia, iFSH/LH AND dtestosterone; XX male; XYY syndrome
•Male genital tract obstruction: congenital absence of vas deferens; epididymal obstruction or infection; Müllerian prostatic cysts; groin or scrotal surgery
•Systemic disease: renal failure; liver cirrhosis; cystic fibrosis
•Drugs: chemotherapy; alcohol; marijuana; sulfasalazine; smoking
•Environmental factors: pesticides; heavy metals; hot baths

ETIOLOGY AND EVALUATION OF MALE INFERTILITY 471
History
•Sexual: duration of problem; frequency and timing of intercourse; previous successful conceptions; previous birth control; erectile or ejaculatory dysfunction
•Developmental: age at puberty; history of cryptorchidism; gynecomastia
•Medical and surgical: detailed assessment for risk factors—recent febrile illness; postpubertal mumps orchitis; varicocele; testicular torsion, trauma, or tumor; sexually transmitted diseases; genitourinary surgery; radiotherapy; respiratory diseases associated with ciliary dysfunction; diabetes
•Drugs and environmental: previous chemotherapy; exposure to substances that impair spermatogenesis or erectile function; alcohol consumption; smoking habits; hot baths
•Family: hypogonadism; cryptorchidism
Examination
Perform a full assessment of all systems, with attention to general appearance (evidence of secondary sexual development; signs of hypogonadism; gynecomastia).
Urogenital examination should include assessment of the penis (Peyronie’s plaque, phimosis, hypospadias); measurement of testicular consistency, tenderness, and volume with a Prader orchidometer (normal >20 mL; varies with race); palpation of epididymis (tenderness, swelling) and spermatic cord (vas deferens present or absent, varicocele); and digital rectal examination of the prostate.

472 CHAPTER 11 Infertility
Lab investigation of male infertility
Basic investigations
Semen analysis
Obtain 2 or 3 specimens over several weeks, collected after 2–7 days of sexual abstinence. Deliver specimens to the laboratory within 1 hour. Ejaculate volume, liquefaction time, and pH are noted (Table 11.1).
Microscopy techniques measure sperm concentration, total numbers, morphology, and motility (Table 11.2).
The mixed agglutination reaction (MAR test) is used to detect antiperm antibodies. The presence of leukocytes or round cells in the ejaculate (>1 x 106/mL of semen) suggests infection, and cultures should be requested.
Hormone measurement
Obtain serum FSH, LH, and testosterone (Table 11.3). Elevated serum FSH levels (2 x normal) suggest irreversible testicular failure. In cases of isolated low testosterone level, it is recommended that morning and free testosterone levels be tested.
Elevated prolactin is associated with sexual dysfunction and low serum testosterone levels, and usually indicates the presence of a pituitary adenoma.
Special investigations
•Chromosome analysis is indicated for clinical suspicion of an abnormality (azoospermia or oligospermia, small atrophic testes with iFSH).
•Fructose is produced in the seminal vescle and is a major source of energy for sperm metabolism. If semen fructose is low, an ejaculatory duct obstruction or seminal vesical abnormality should be suspected.
•Testicular biopsy is performed for azoospermic patients with normal FSH levels, to differentiate between idiopathic (e.g., maturation arrest, Sertoli cell only syndrome) and obstructive causes. It may also be used for sperm retrieval.
Sperm function tests
Postcoital test
Cervical mucus is taken just before ovulation and within 8 hours of intercourse, and microscopy is performed. Normal results shows >10 sperm per high-powered field, the majority demonstrating progressive motility. Abnormal results indicate inappropriate timing of the test; cervical mucus antisperm antibodies; abnormal semen; or inappropriately performed coitus.
Sperm penetration test
A sample of semen is placed directly onto preovulatory cervical mucus on a slide and the penetrative ability of spermatozoa is observed.
Sperm-cervical mucus test
A specimen of semen (control) and one mixed with cervical mucus are placed separately on a slide and observed for 30 minutes. More than 25% exhibiting jerking movements in the mixed sample (but not the control) is a positive test for antisperm antibodies.
|
|
LAB INVESTIGATION OF MALE INFERTILITY |
473 |
|
|
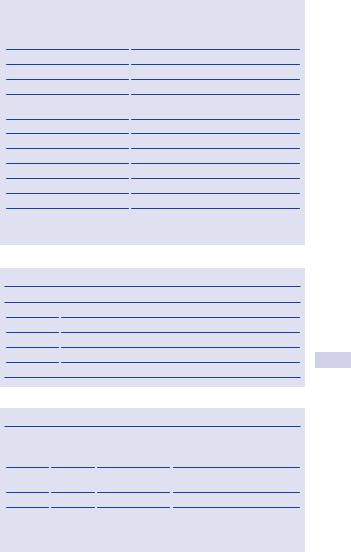
Table 11.1 Semen analysis: normal parameters* |
|||
|
|
|
|
|
|
Semen analysis |
Normal values |
||
|
|
|
|
|
|
Semen volume |
>2.0 mL |
||
|
pH |
7.2–7.8 |
||
|
Total sperm count |
>40 x106/ejaculate |
||
|
Sperm concentration |
>20 x106/mL |
||
|
Sperm motility |
>50% with progressive motility (grades >2); |
||
|
|
or >25% grade 4 |
||
|
Sperm morphology |
>15% normal forms |
||
|
Viability |
>75% viable sperm |
||
|
Time to liquefy |
5–25 minutes |
||
|
White blood cells |
<1 x106 WBC/mL |
||
|
MAR test (for antisperm Ab) |
Negative (<10% with adherent particles) |
||
|
Zinc |
>2.4 mol/ejaculate |
||
|
Semen fructose |
120–145 mg/dL |
||
|
|
|
|
|
*Adapted from World Health Organization (WHO) reference values for semen analysis.
Table 11.2 Grading of sperm motility
Grade |
Type of sperm motility |
0No motility
1Sluggish; no progressive movement
2Slow, meandering forward progression
3Moving in a straight line with moderate speed
4Moving in a straight line at high speed
Table 11.3 Clinical diagnosis on hormone assay
FSH* |
LH** |
Testosterone |
Diagnosis |
i |
Normal |
Normal |
Seminiferous tubule damage |
|
|
|
(defective spermatogenesis) |
Normal |
Normal |
Normal |
Normal; or bilateral genital tract |
|
|
|
obstruction |
i |
i |
Normal/d |
Testicular failure |
d |
d |
d |
Hypogonadotrophism |
|
|
|
|
* Follicle stimulation hormone. ** Luteinizing hormone.

474 CHAPTER 11 Infertility
Imaging
Scrotal ultrasound
This is used to confirm a varicocele and assess testicular abnormalities.
Transrectal ultrasound
TRUS is indicated for low ejaculate volumes, to investigate seminal vesicle obstruction (>1.5 cm width) or absence and ejaculatory duct obstruction (>2 .3 mm).
Vasography
Vas deferens is punctured at the level of the scrotum and injected with contrast toward the prostate, never toward the epdidymis. Vasography is performed at the time of planned reconstruction.
A normal test shows the passage of contrast along the vas deferens, seminal vesicles, ejaculatory duct, and into the bladder, which rules out obstruction—indigo carmine is commonly used to confirm patency.
Formal radiographic vasography is only indicated to localize obstructions proximal to the inguinal ring.
Venography
This is used to diagnose and treat varicoceles (embolization).
This page intentionally left blank
