
ECHO 2013 / Acute Coronary Syndromes Echo in the Assessment of Complications
.pdf
Transcatheter Closure of Post-
infarct VSD
Devices:
–Amplatzer Muscular VSD occluder: waist 7 mm
–AMPLATZER™ P.I. Muscular VSD Occluder: waist 10 mm (not available in US)
Patient Selection:
–Exact localization of the VSD within the septum is of paramount importance of the subsequent stability of the device
– Echocardiography prior to device implantation is crucial for optimal patient selection
– Anterior infarction:
Typically in apex, good stability of device
– Inferior infarction:
Typically near base of RV/LV free wall with distortion of the walls or incomplete opening of the device
Close to the tricuspid valve and mitral valve
Kaulfersch C et al Minerva Cardioangiologica 2007;55(5):693-701
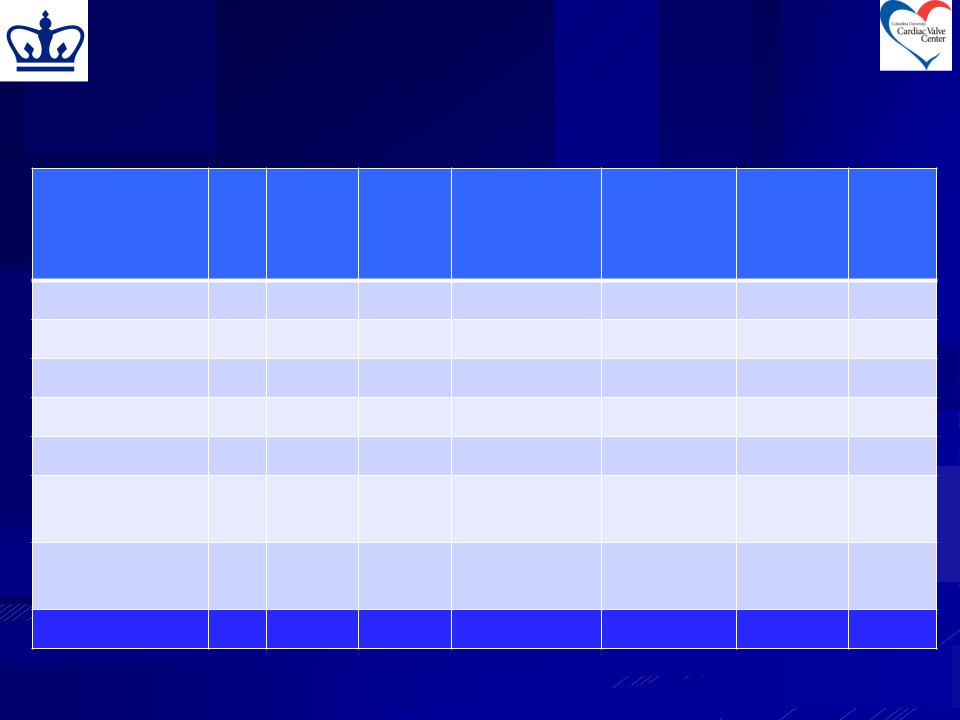
Result of Intervention Post-infarction VSD with
Amplatzer Occluder Registries
|
#Pt |
Acute |
Sub- |
Mean time |
Primary/ |
Success |
Mortal |
|
|
Phase |
acute |
AMI to |
secondary |
rate (%) |
ity (%) |
|
|
|
phase |
closure |
VSD |
|
|
|
|
|
|
(days) |
closure |
|
|
Holzer et al |
18 |
6 |
12 |
25(2-95) |
8/10 |
89 |
39 |
Goklstein et al |
4 |
0 |
4 |
58(15-108) |
0/4 |
75 |
25 |
Szkutnik et al |
7 |
0 |
7 |
54(14-70) |
6/1 |
71 |
20 |
Chessa et al |
12 |
3 |
9 |
___ |
7/5 |
83 |
40 |
Martinez et al |
5 |
3 |
2 |
6(1-16) |
3/2 |
100 |
20 |
Bialkowski et |
19 |
1 |
18 |
62(14-336) |
17/2 |
95 |
31 |
al |
|
|
|
|
|
|
|
Leipzie |
22 |
19 |
3 |
6(1-26) |
22/0 |
78 |
68 |
experience |
|
|
|
|
|
|
|
TOTAL |
87 |
32 |
55 |
35(1-336) |
63/24 |
84 |
35 |
Kaulfersch C et al Minerva Cardioangiologica 2007;55(5):693-701
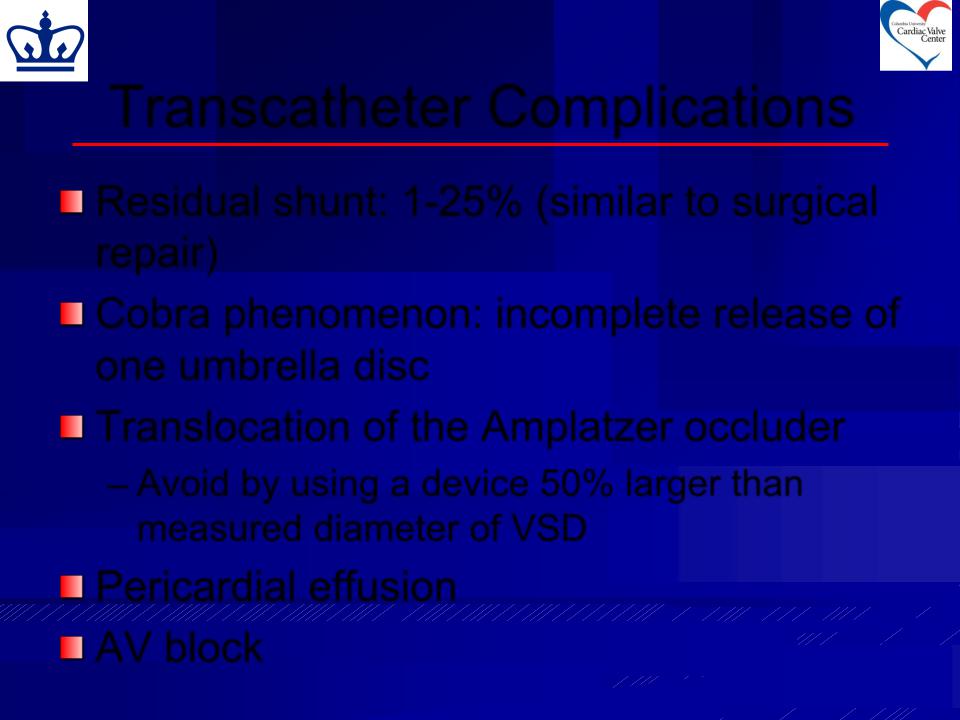
Transcatheter Complications
Residual shunt: 1-25% (similar to surgical repair)
Cobra phenomenon: incomplete release of one umbrella disc
Translocation of the Amplatzer occluder
– Avoid by using a device 50% larger than measured diameter of VSD
Pericardial effusion AV block
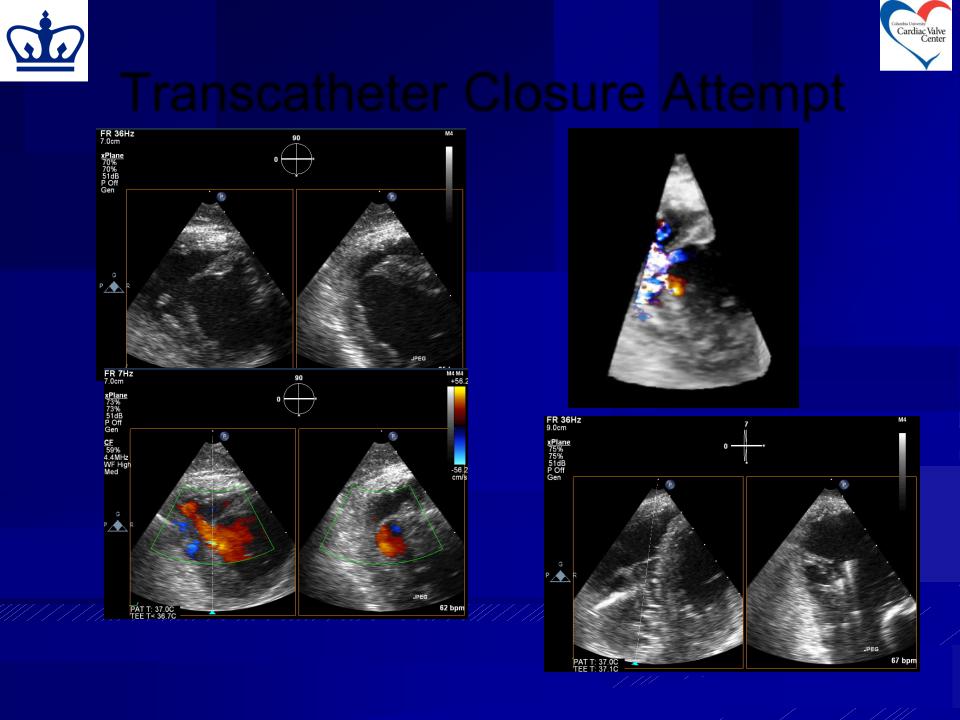
Transcatheter Closure Attempt
85 yo woman, S/P apical MI 5 days
PTA, now with progressive SOB
Direct RV puncture
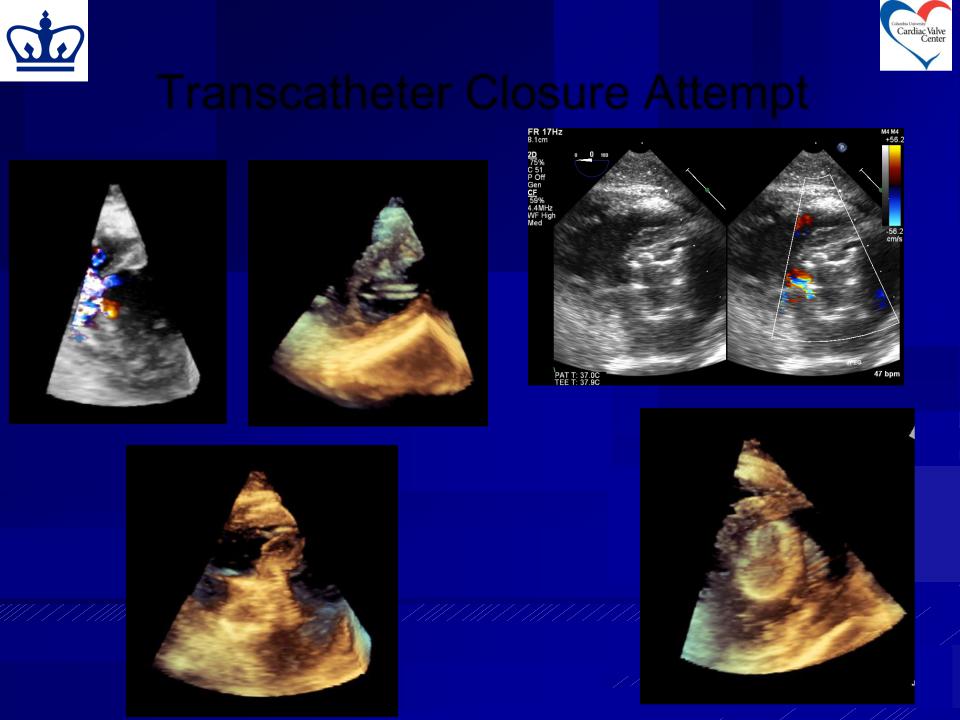
Transcatheter Closure Attempt
Amplatzer post too short
VSD |
Delivery catheter |
|
Translocation |
LV Arm Deployed |
into LV apex |
|
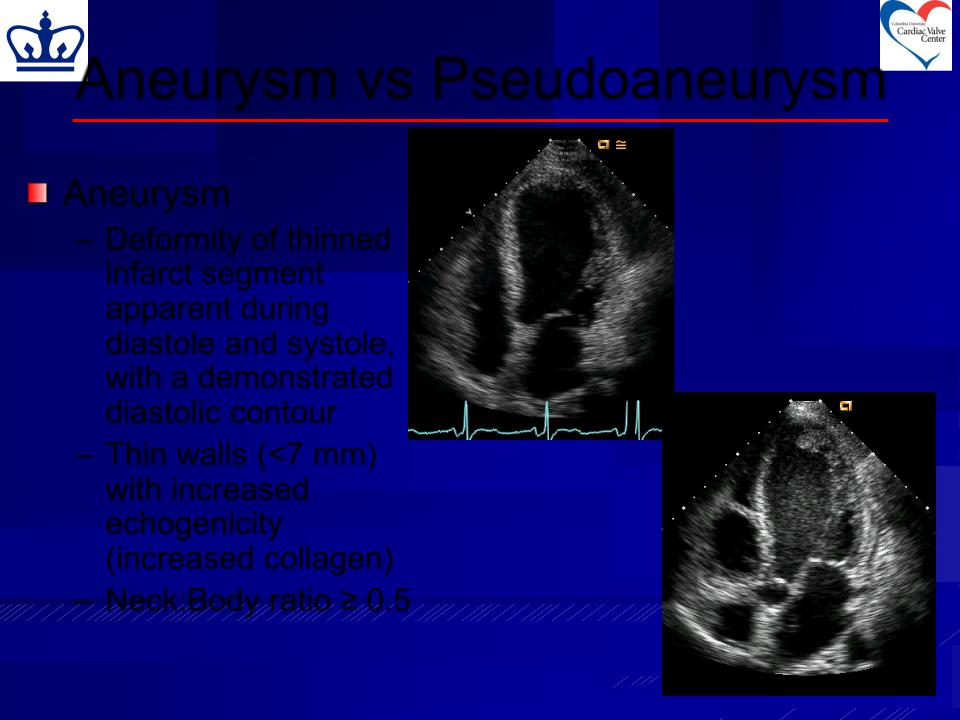
Aneurysm vs Pseudoaneurysm 
Aneurysm
–Deformity of thinned infarct segment apparent during
diastole and systole, with a demonstrated diastolic contour
–Thin walls (<7 mm) with increased echogenicity (increased collagen)
– Neck:Body ratio ≥ 0.5
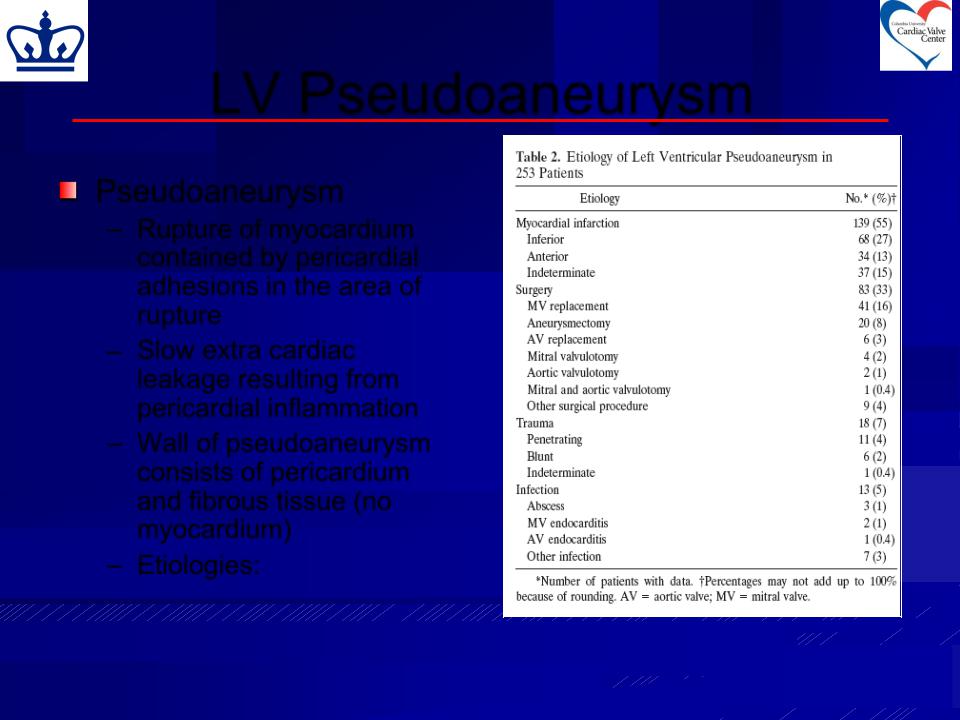
LV Pseudoaneurysm
Pseudoaneurysm
–Rupture of myocardium contained by pericardial adhesions in the area of rupture
–Slow extra cardiac leakage resulting from pericardial inflammation
– Wall of pseudoaneurysm consists of pericardium and fibrous tissue (no myocardium)
– Etiologies:
Yeo TC et al. Ann Intern Med 1998;128:299-305
Frances C et al. JACC 1998;32:557-61
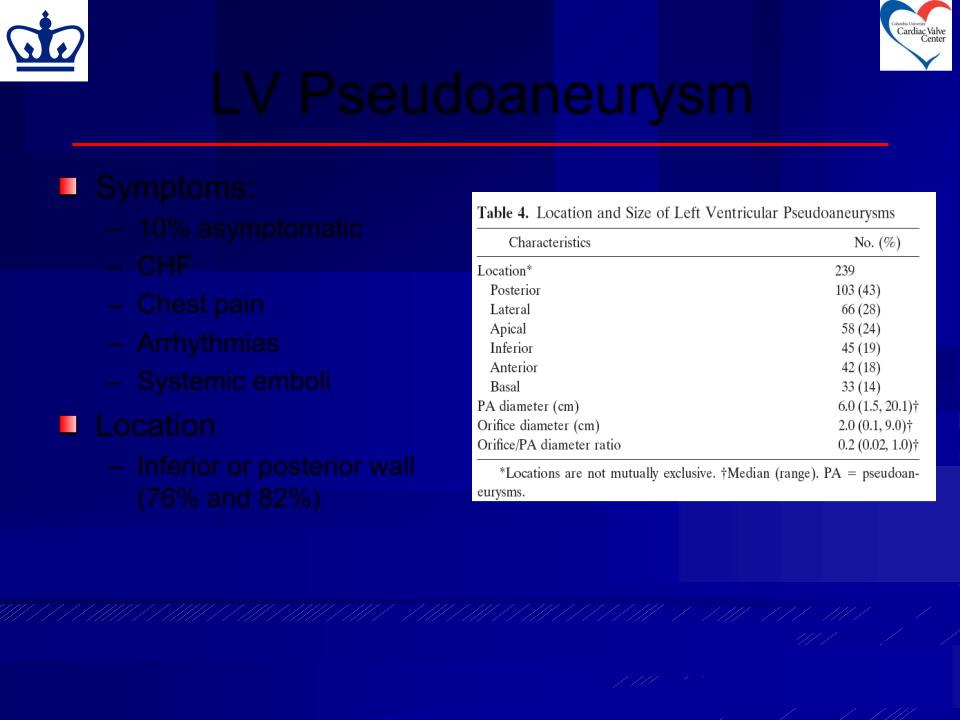
LV Pseudoaneurysm
Symptoms:
–10% asymptomatic
–CHF
–Chest pain
–Arrhythmias
–Systemic emboli
Location
–Inferior or posterior wall (76% and 82%)
Harpaz D et al JASE 2001;14:219-27.
Frances C et al. JACC 1998;32:557-61
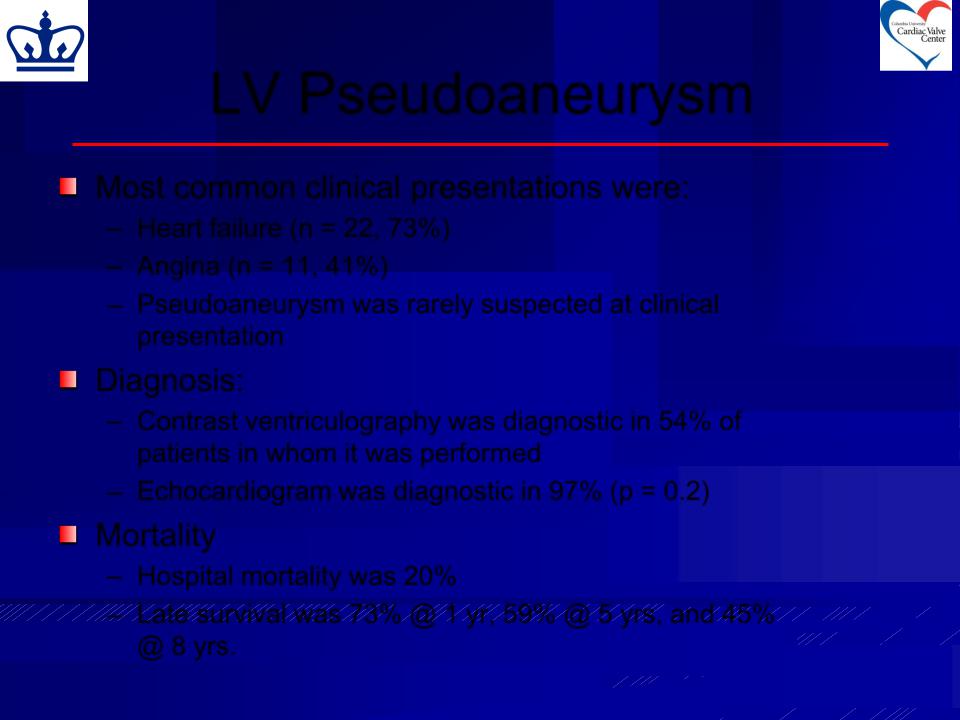
LV Pseudoaneurysm
Most common clinical presentations were:
–Heart failure (n = 22, 73%)
–Angina (n = 11, 41%)
–Pseudoaneurysm was rarely suspected at clinical presentation
Diagnosis:
– Contrast ventriculography was diagnostic in 54% of patients in whom it was performed
– Echocardiogram was diagnostic in 97% (p = 0.2)
Mortality
–Hospital mortality was 20%
–Late survival was 73% @ 1 yr, 59% @ 5 yrs, and 45%
@ 8 yrs.
Atik FA et al. Ann Thorac Surg. 2007;83(2):526-31.
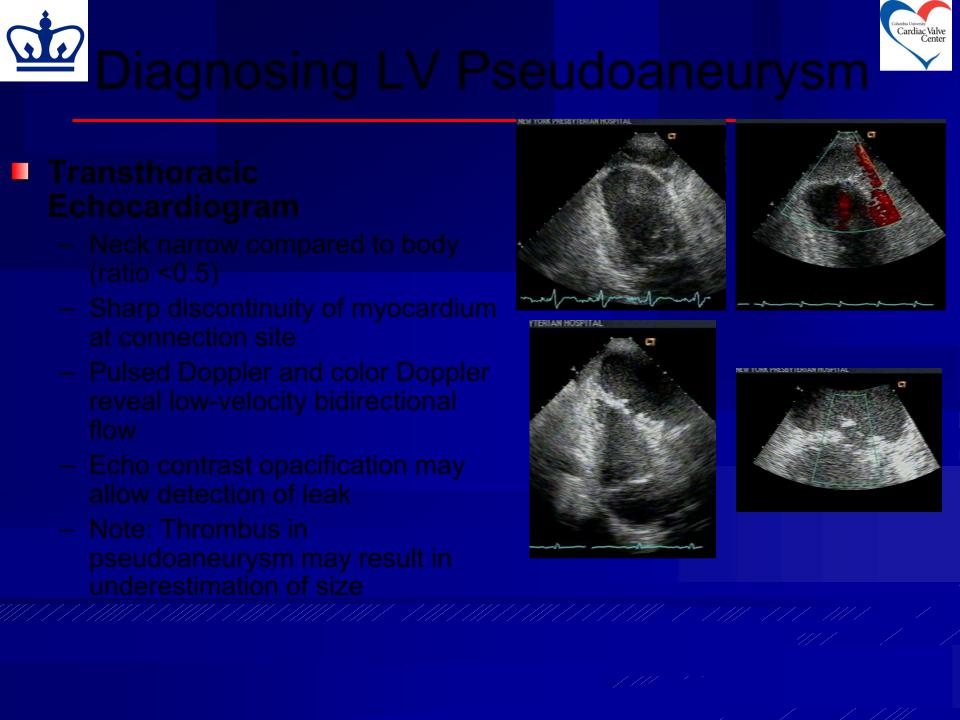
Diagnosing LV Pseudoaneurysm
Transthoracic
Echocardiogram
–Neck narrow compared to body (ratio <0.5)
–Sharp discontinuity of myocardium at connection site
–Pulsed Doppler and color Doppler
reveal low-velocity bidirectional flow
–Echo contrast opacification may allow detection of leak
–Note: Thrombus in pseudoaneurysm may result in
underestimation of size |
Harpaz D et al JASE 2001;14:219-27. |
|
March KL et al Clin Cardiol 1989;12:531-40 |
|
Catherwood E et al Circulation 1980;62:294-302 |
Gatewood RP Jr and Nanda N. Am J Cardiol 1980;46:869-78
