
ECHO 2013 / Aortic Stenosis Quantitation It’s Not All About the Gradient
.pdf
Measurement Errors: LVOT Velocity
Underestimation of VLVOT
Too far from the valve
Doppler beam not well aligned
Overestimation of VLVOT (>1.5)
Subvalvular flow acceleration
Too far in the valve/aorta

Aortic Stenosis in Community Medical Practice:
Determinants of Outcome and Implications for
Aortic Valve Replacement
“An AVA <1.0 cm2 is the most powerful and sensitive predictor of severe outcomes”
Malouf J. J Thorac Cardiovasc Surg 2012

Case Study #1: Asymptomatic Patient with Severe AS
65 y.o. woman with calcific AS
Asymptomatic (exercise testing)
LVEF: 60%
AS severity on echo:
Peak jet velocity: 5.1 m/s (1 Yr ago: 4.8 m/s)
Peak/mean gradient: 104/64 mmHg
AVA: 0.65 cm2
Indexed AVA: 0.35 cm2/m2
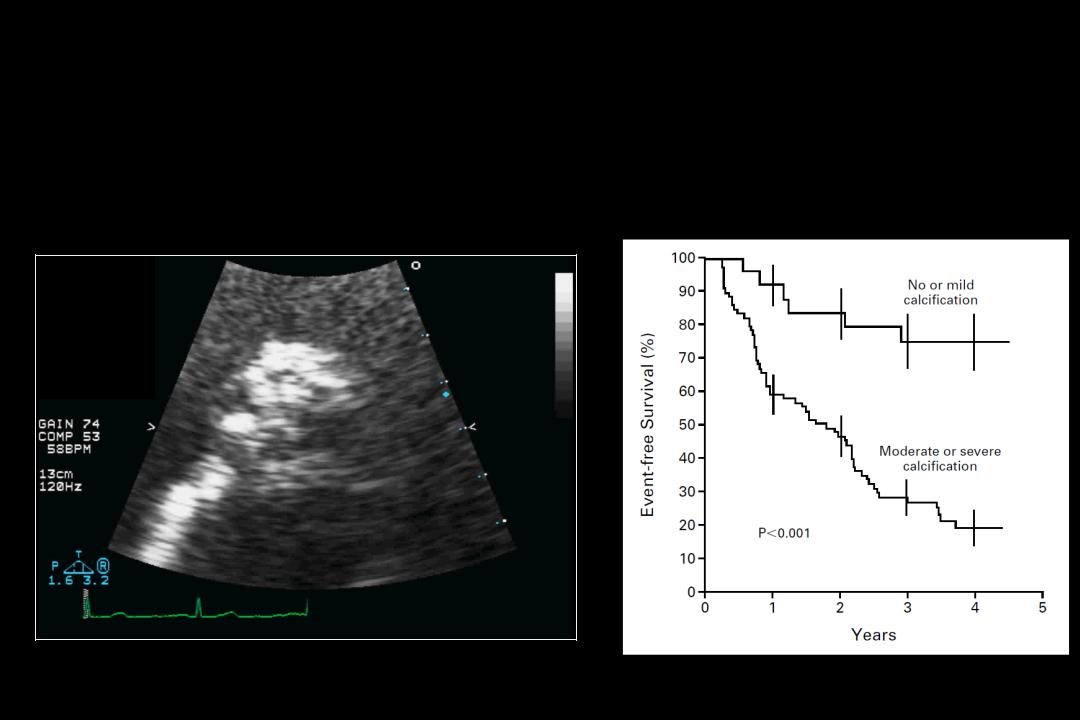
Case Study #1: Look At the Valve!
Severe Aortic Valve Calcification
Valve Calcification
(≥3/4)
Rosenhek et al N Engl J Med
2000; 343:611-7

Severe Aortic Stenosis
VPeak>4 m/s
Mean gradient >40 mm Hg AVA < 1.0 cm²

 Re-evaluation Undergoing CABG or
Re-evaluation Undergoing CABG or
other heart surgery?
Symptoms?
|
|
Yes |
|
|
|
|
|
|
|
|
Equivocal |
|
|
|
|
|
No |
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Normal |
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
Exercise test |
|
|
LV ejection fraction |
|
|
|
|
||||||
|
|
|
|
|
|
Symptoms |
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
BP |
|
|
|
<50% |
|
|
|
|
|
|
Normal |
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
(ESC) |
|
(ACC/AHA) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
|
|
|
Very severe AS (<0.6 cm2) |
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Severe valve calcification (≥3/4) |
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
(ESC) |
(ACC/AHA) |
|
|
Rapid progression (≥0.3 m /s/yr) |
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Class I |
|
Class I |
|
|
Class IIb |
|
|
Class I |
|
Class IIa |
|
Class IIb |
|
|
|
|
No |
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Aortic Valve Replacement |
|
|
|
|
|
|
|
|
Clinical/ echo follow-up, |
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Wait for symptoms |
|
|
|
||
|
Preoperative coronary angiography |
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||

Look at the Aorta And Arteries
►Accounting for Pressure Recovery
►Assessing Vascular Load

Pressure Recovery
EOA

Determinants of Pressure Recovery
LVOT
EOA
AA
AORTA
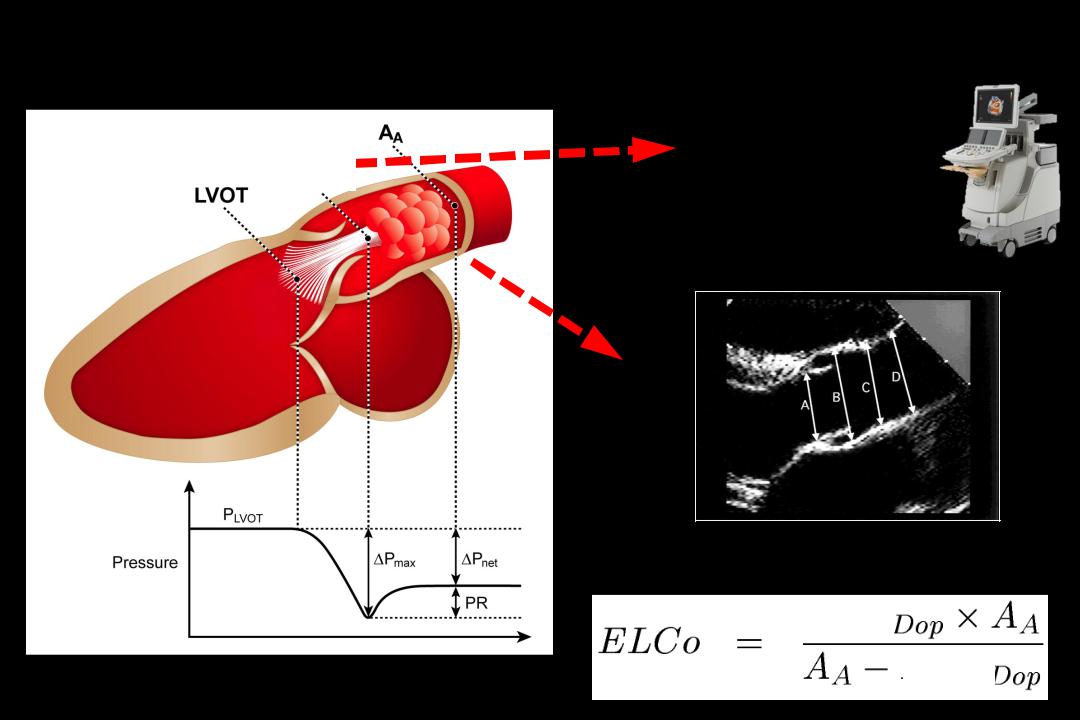
A New Doppler-Echo Parameter of AS Severity that Accounts for Pressure Recovery
EOA
EOA
AA
Garcia et al, Circulation 2000 ; 101 : 765-771
Garcia et al., JACC 2003; 41:435-42
Energy loss coefficient
EOA
EOA

Pressure Recovery: Reclassification of AS Severity
Case #1
Severe
AS
Doppler |
|
|
Aorta Diameter (mm) |
|
|
|||
AVA |
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(cm2) |
20 |
25 |
30 |
35 |
|
40 |
45 |
|
0.4 |
0.5 |
0.4 |
0.4 |
0.4 |
|
0.4 |
0.4 |
|
|
|
|
|
|
|
|
|
|
0.5 |
0.6 |
0.6 |
|
0.5 |
0.5 |
|
0.5 |
0.5 |
|
|
|
|
|
|
|
|
|
0.6 |
0.7 |
0.7 |
|
0.7 |
0.6 |
|
0.6 |
0.6 |
|
|
|
|
|
|
|
|
|
0.7 |
0.9 |
0.8 |
|
0.8 |
0.8 |
|
0.7 |
0.7 |
|
|
|
|
|
|
|
|
|
0.8 |
1.1 |
1.0 |
|
0.9 |
0.9 |
|
0.9 |
0.8 |
|
|
|
|
|
|
|
|
|
0.9 |
1.3 |
1.1 |
|
1.0 |
1.0 |
|
1.0 |
1.0 |
|
|
|
|
|
|
|
|
|
1.0 |
1.5 |
1.3 |
|
1.2 |
1.1 |
|
1.1 |
1.1 |
|
|
|
|
|
|
|
|
|
1.1 |
1.7 |
1.4 |
|
1.3 |
1.2 |
|
1.2 |
1.2 |
1.2 |
1.9 |
1.6 |
|
1.4 |
1.4 |
|
1.3 |
1.3 |
1.3 |
2.2 |
1.8 |
|
1.6 |
1.5 |
|
1.5 |
1.4 |
1.4 |
2.5 |
2.0 |
|
1.7 |
1.6 |
|
1.6 |
1.5 |
1.5 |
2.9 |
2.2 |
|
1.9 |
1.8 |
|
1.7 |
1.7 |
|
|
|
|
|
|
|
|
|
Garcia et al., JACC 2003; 41:435-42
