
- •Foreword
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1.2 Forehead Augmentation
- •1.2.1 Discussion
- •1.3.1 Discussion
- •1.4 Rhinoplasty
- •1.4.1 Discussion
- •1.5 Lip Augmentation
- •1.5.1 Discussion
- •1.6 Chin and Jaw Augmentation
- •1.6.1 Discussion
- •Further Reading
- •Forehead Augmentation
- •Rhinoplasty
- •Lip Augmentation
- •Jaw Augmentation
- •2: Imaging the Postoperative Orbit
- •2.1 Eyelid Weights
- •2.1.1 Discussion
- •2.2 Palpebral Springs
- •2.2.1 Discussion
- •2.3.1 Discussion
- •2.4.1 Discussion
- •2.5.1 Discussion
- •2.6.1 Discussion
- •2.7 Strabismus Surgery
- •2.7.1 Discussion
- •2.8 Glaucoma Surgery
- •2.8.1 Discussion
- •2.9 Scleral Buckles
- •2.9.1 Discussion
- •2.10 Keratoprostheses
- •2.10.1 Discussion
- •2.11 Intraocular Lens Implants
- •2.11.1 Discussion
- •2.12 Surgical Aphakia
- •2.12.1 Discussion
- •2.13 Pneumatic Retinopexy
- •2.13.1 Discussion
- •2.14 Intraocular Silicone Oil
- •2.14.1 Discussion
- •2.15.1 Discussion
- •2.16 Orbital Tissue Expanders
- •2.16.1 Discussion
- •2.17 Orbital Exenteration
- •2.17.1 Discussion
- •2.18.1 Discussion
- •Further Reading
- •Eyelid Weights
- •Palpebral Spring
- •Frontalis Suspension Ptosis Repair
- •Strabismus Surgery
- •Glaucoma Surgery
- •Scleral Buckles
- •Keratoprostheses
- •Intraocular Lens Implants
- •Surgical Aphakia
- •Pneumatic Retinopexy
- •Intraocular Silicone Oil
- •Orbital Tissue Expanders
- •Orbital Exenteration
- •3.1.1 Discussion
- •3.2 Septoplasty
- •3.2.1 Discussion
- •3.3.1 Discussion
- •3.4.1 Discussion
- •3.5 Nasal Packing Material
- •3.5.1 Discussion
- •3.6 Rhinectomy
- •3.6.1 Discussion
- •3.7 Sinus Lift Procedure
- •3.7.1 Discussion
- •3.8 Caldwell-Luc Procedure
- •3.8.1 Discussion
- •3.9 External Ethmoidectomy
- •3.9.1 Discussion
- •3.10.1 Discussion
- •3.11 FESS Complications
- •3.11.1 Discussion
- •3.11.2 Discussion
- •3.11.3 Discussion
- •3.11.4 Discussion
- •3.11.5 Discussion
- •3.11.6 Discussion
- •3.11.7 Discussion
- •3.11.8 Discussion
- •3.11.9 Discussion
- •3.11.10 Discussion
- •3.11.11 Discussion
- •3.12 Osteoplastic Flap with Frontal Sinus Obliteration
- •3.12.1 Discussion
- •3.13 Frontal Sinus Cranialization
- •3.13.1 Discussion
- •3.14 Paranasal Sinus Stents
- •3.14.1 Discussion
- •3.15 Frontal Sinus Trephination
- •3.15.1 Discussion
- •3.16.1 Discussion
- •3.17.1 Discussion
- •3.18 Maxillary Swing
- •3.18.1 Discussion
- •Further Reading
- •Septoplasty
- •Nasal Septal Button Prosthesis
- •Nasal Packing Material
- •Rhinectomy
- •Sinus Lift
- •Caldwell-Luc Procedure
- •External Ethmoidectomy
- •Functional Endoscopic Sinus Surgery
- •FESS Complications
- •Osteoplastic Flap with Frontal Sinus Obliteration
- •Frontal Sinus Cranialization
- •Paranasal Sinus Stents
- •Frontal Sinus Trephination
- •Maxillectomy and Palatectomy
- •Maxillary Swing
- •4.1 Occipital Nerve Stimulator
- •4.1.1 Discussion
- •4.2 Tissue Expander
- •4.2.1 Discussion
- •4.3 Temporal Fossa Implants
- •4.3.1 Discussion
- •4.4.1 Discussion
- •4.5.1 Discussion
- •4.6.1 Discussion
- •4.7 Scalp Tumor Recurrence
- •4.7.1 Discussion
- •4.8 Burr Holes
- •4.8.1 Discussion
- •4.9 Craniotomy
- •4.9.1 Discussion
- •4.10 Cranioplasty
- •4.10.1 Discussion
- •4.11 Autocranioplasty
- •4.11.1 Discussion
- •4.12.1 Discussion
- •4.14.1 Discussion
- •4.15 Box Osteotomy
- •4.16.1 Discussion
- •4.17.1 Discussion
- •4.18.1 Discussion
- •4.19 Subdural Drainage Catheters
- •4.19.1 Discussion
- •4.20.1 Tension Pneumocephalus
- •4.20.5 Pseudomeningoceles
- •4.20.6 Pseudoaneurysm
- •4.20.7 Postoperative Infection
- •4.20.8 Textiloma
- •4.20.9 Sunken Skin Flap Syndrome
- •4.20.10 External Brain Herniation
- •4.20.11 Bone Flap Resorption
- •Further Reading
- •Occipital Nerve Stimulator
- •Tissue Expander
- •Temporal Fossa Implant
- •Scalp Tumor Recurrence
- •Box Osteotomy
- •Absorbable Hemostatic Agents
- •Duraplasty and Sealant Agents
- •Burr Holes
- •Craniotomy
- •Cranioplasty
- •Autocranioplasty
- •Cranial Vault Reconstruction for Craniosynostosis
- •Cranial Vault Encephalocele Repair
- •Subdural Drainage Catheters
- •Intracranial Pressure Monitor
- •Cranial Surgery Complications
- •5.1 Intraoperative MRI
- •5.1.1 Discussion
- •5.2.1 Stereotactic Biopsy
- •5.2.1.1 Discussion
- •5.2.2 Resection Cavities
- •5.2.2.1 Discussion
- •5.2.3 Ommaya Reservoirs
- •5.2.3.1 Discussion
- •5.2.4 Chemotherapy Wafers
- •5.2.4.1 Discussion
- •5.2.5 Brachytherapy Seeds
- •5.2.5.1 Discussion
- •5.2.6.1 Discussion
- •5.3.1 Prefrontal Lobotomy
- •5.3.1.1 Discussion
- •5.3.2 Pallidotomy
- •5.3.2.1 Discussion
- •5.3.3 Cingulotomy
- •5.3.3.1 Discussion
- •5.3.4.1 Discussion
- •5.3.4.2 Thalamotomy
- •5.3.5 Deep Brain Stimulation (DBS)
- •5.3.5.1 Discussion
- •5.3.6.1 Discussion
- •5.3.7.1 Discussion
- •5.3.8.1 Discussion
- •5.3.9.1 Discussion
- •5.3.10 Corticectomy
- •5.3.10.1 Discussion
- •5.3.11.1 Discussion
- •5.3.12.1 Discussion
- •5.3.13 Callosotomy
- •5.3.13.1 Discussion
- •5.3.14 Anterior Temporal Lobectomy
- •5.3.14.1 Discussion
- •5.3.15.1 Discussion
- •5.3.16 Hemispherectomy
- •5.3.16.1 Discussion
- •Further Reading
- •Intraoperative MRI
- •Brain Tumor Surgery
- •Stereotactic Biopsy
- •Resection Cavities
- •Postoperative Hemorrhagic Lesions
- •Ommaya Reservoirs
- •Chemotherapy Wafers
- •Brachytherapy Seeds
- •GliaSite Radiation Therapy System
- •Prefrontal Lobotomy
- •Pallidotomy
- •Cingulotomy
- •Thalamotomy
- •Deep Brain Stimulation (DBS)
- •Epidural Motor Cortex Stimulator
- •Neural Interface System (BrainGate)
- •Corticectomy
- •Selective Disconnection
- •Callosotomy
- •Anterior Temporal Lobectomy
- •Hemispherectomy
- •6.1 Types of Procedures
- •6.1.1 External Ventricular Drainage
- •6.1.1.1 Discussion
- •6.1.2.1 Discussion
- •6.1.3 Atypical Ventricular Shunts
- •6.1.3.1 Discussion
- •6.1.4 Ventriculosubgaleal Shunts
- •6.1.4.1 Discussion
- •6.1.5.1 Discussion
- •6.1.6.1 Discussion
- •6.1.7 Subdural-Peritoneal Shunts
- •6.1.7.1 Discussion
- •6.1.8.1 Discussion
- •6.1.9.1 Discussion
- •6.1.10 Lumboperitoneal Shunts
- •6.1.10.1 Discussion
- •6.1.11 Third Ventriculocisternostomy
- •6.1.11.1 Discussion
- •6.1.12.1 Discussion
- •6.1.13 Aqueductoplasty
- •6.1.13.1 Discussion
- •6.1.14.1 Discussion
- •6.2.1.1 Discussion
- •6.2.2.1 Discussion
- •6.2.3 Intraventricular Fat Migration
- •6.2.3.1 Discussion
- •6.2.4.1 Discussion
- •6.2.5.1 Discussion
- •6.2.6 Slit Ventricle Syndrome
- •6.2.6.1 Discussion
- •6.2.7.1 Discussion
- •6.2.8 Shunt-Associated Infections
- •6.2.8.1 Discussion
- •6.2.9.1 Discussion
- •6.2.10.1 Discussion
- •6.2.11.1 Discussion
- •6.2.12 Peritoneal Pseudocysts
- •6.2.12.1 Discussion
- •6.2.13.1 Discussion
- •6.2.14 Tumor Seeding
- •6.2.14.1 Discussion
- •6.2.15 Shunt Catheter Calcification
- •6.2.15.1 Discussion
- •6.2.16.1 Discussion
- •6.2.17.1 Discussion
- •Further Reading
- •Types of Procedures
- •External Ventricular Drainage
- •Ventriculoperitoneal Shunts
- •Atypical Ventricular Shunts
- •Ventriculosubgaleal Shunts
- •Subdural-Peritoneal Shunts
- •Lumboperitoneal Shunt
- •Third Ventriculostomy
- •Aqueductoplasty
- •Fourth Ventricular Stenting
- •Complications
- •Intraventricular Fat Migration
- •Slit Ventricle Syndrome
- •Shunt-Associated Infections
- •Shunt Malposition and Migration
- •Pseudocysts
- •Cerebrospinal Fluid Leak Syndrome
- •Tumor Seeding
- •Shunt Catheter Calcifications
- •7.1.1 Discussion
- •7.2.1 Discussion
- •7.3.1 Discussion
- •7.4.1 Discussion
- •7.5.1 Discussion
- •7.6.1 Discussion
- •7.7 Radiosurgery for Vestibular Schwannomas
- •7.7.1 Discussion
- •Further Reading
- •Anterior Craniofacial Resection
- •Transsphenoidal Resection
- •Middle Cranial Fossa Reconstruction
- •Surgical Approaches for Vestibular Schwannoma Resection
- •8.1.1 Discussion
- •8.2 Auriculectomy
- •8.2.1 Discussion
- •8.3 Auricular Reconstruction
- •8.3.1 Discussion
- •8.4.1 Discussion
- •8.5 Atresiaplasty
- •8.5.1 Discussion
- •8.6.1 Discussion
- •8.7.1 Discussion
- •8.8 Ossicular Interposition
- •8.8.1 Discussion
- •8.9.1 Discussion
- •8.10.1 Discussion
- •8.11.1 Discussion
- •8.12 Atticotomy
- •8.12.1 Discussion
- •8.13.1 Discussion
- •8.14.1 Discussion
- •8.15.1 Discussion
- •8.16 Temporal Bone Resection
- •8.16.1 Discussion
- •8.17 Cochlear Implants
- •8.17.1 Discussion
- •8.18.1 Discussion
- •8.19.1 Discussion
- •8.20.1 Discussion
- •8.21.1 Discussion
- •8.22 Labyrinthectomy
- •8.22.1 Discussion
- •8.23 Vestibular Nerve Section
- •8.23.1 Discussion
- •8.24.1 Discussion
- •8.25.1 Discussion
- •Further Reading
- •BAHA Device
- •Auriculectomy
- •Auricular Reconstruction
- •Canaloplasty and Meatoplasty
- •Atresiaplasty
- •Myringoplasty and Tympanoplasty
- •Incus Interposition
- •Ossicular Prosthesis Complications
- •Transcanal Atticotomy
- •Mastoidectomy Complications
- •Lateral Temporal Bone Resection
- •Cochlear Implants
- •Cochlear Implant Complications
- •Auditory Brainstem Stimulator
- •Repair of Perilymphatic Fistula
- •Labyrinthectomy
- •Vestibular Nerve Sectioning
- •Tube Drainage of Cholesterol Cysts
- •9.1 Vertical Ramus Osteotomy
- •9.1.1 Discussion
- •9.2 Sagittal Split Osteotomy
- •9.2.1 Discussion
- •9.3 Genioplasty
- •9.3.1 Discussion
- •9.4.1 Discussion
- •9.5 Mandibular Distraction
- •9.5.1 Discussion
- •9.6 LeFort I Osteotomy
- •9.6.1 Discussion
- •9.7 LeFort III Osteotomy
- •9.7.1 Discussion
- •9.8.1 Discussion
- •9.9 Mandibulotomy
- •9.9.1 Discussion
- •9.10 Enucleation
- •9.10.1 Discussion
- •9.11 Cyst Decompression
- •9.11.1 Discussion
- •9.12 Coronoidectomy
- •9.12.1 Discussion
- •9.13.1 Discussion
- •9.14.1 Discussion
- •9.15.1 Discussion
- •9.16.1 Discussion
- •9.17.1 Discussion
- •9.18.1 Discussion
- •9.19.1 Discussion
- •9.20.1 Discussion
- •Further Reading
- •Vertical Ramus Osteotomy
- •Sagittal Split Osteotomy
- •Genioplasty
- •Mandibular Angle Augmentation
- •Mandibular Distraction
- •Lefort I Surgery
- •Lefort III Surgery
- •Fixation of Mandible Fractures
- •Mandibulotomy
- •Enucleation
- •Cyst Decompression
- •Coronoidectomy
- •Eminectomy and Meniscal Plication
- •10: Imaging the Postoperative Neck
- •10.1 Reconstruction Flaps
- •10.1.1 Discussion
- •10.2 Neck Dissection
- •10.2.1 Discussion
- •10.3 Parotidectomy
- •10.3.1 Discussion
- •10.4.1 Discussion
- •10.5 Facial Reanimation
- •10.5.1 Discussion
- •10.6.1 Discussion
- •10.7.1 Discussion
- •10.8 Transoral Robotic Surgery
- •10.8.1 Discussion
- •10.9 Sistrunk Procedure
- •10.9.1 Discussion
- •10.10 Laryngectomy
- •10.10.1 Discussion
- •10.11.1 Discussion
- •10.12 Montgomery T-Tubes
- •10.12.1 Discussion
- •10.13 Salivary Bypass Stent
- •10.13.1 Discussion
- •10.14 Laryngeal Stents
- •10.14.1 Discussion
- •10.15.1 Discussion
- •10.16 Arytenoid Adduction
- •10.16.1 Discussion
- •10.17 Arytenoidectomy
- •10.17.1 Discussion
- •10.18 Laryngeal Cartilage Remodeling
- •10.18.1 Discussion
- •10.19 Tracheotomy
- •10.19.1 Discussion
- •10.20 Thyroidectomy
- •10.20.1 Discussion
- •10.21.1 Discussion
- •10.22 Brachytherapy
- •10.22.1 Discussion
- •10.23 Vagal Nerve Stimulation
- •10.23.1 Discussion
- •Further Reading
- •Reconstruction Flaps
- •Facial Reanimation
- •Tonsillectomy and Adenoidectomy
- •Transoral Robotic Surgery
- •Neck Dissection
- •Parotidectomy
- •Salivary Duct Stenting
- •Laryngectomy
- •Montgomery T-Tubes
- •Salivary Bypass Stents
- •Laryngeal Stents
- •Arytenoid Adduction
- •Arytenoidectomy
- •Laryngeal Cartilage Remodeling
- •Tracheotomy
- •Thyroidectomy
- •Neck Exploration and Parathyroidectomy
- •Sistrunk Procedure
- •Brachytherapy
- •Vagal Nerve Stimulation
- •11: Imaging of Postoperative Spine
- •11.1 Overview
- •11.2 Spine Decompression
- •11.2.1.1 Discussion
- •11.2.2 Laminectomy
- •11.2.2.1 Discussion
- •11.2.3 Facetectomy
- •11.2.3.1 Discussion
- •11.2.4 Microdiscectomy
- •11.2.4.1 Discussion
- •11.2.5 Laminoplasty
- •11.2.5.1 Discussion
- •11.2.6 Vertebrectomy
- •11.2.6.1 Discussion
- •11.2.7 Cordectomy
- •11.2.7.1 Discussion
- •11.3.1 Halo and Traction Devices
- •11.3.1.1 Discussion
- •11.3.2 Bone Graft Materials
- •11.3.2.1 Discussion
- •11.3.3 Implantable Bone Stimulators
- •11.3.3.1 Discussion
- •11.3.4 Odontoid Screw Fixation
- •11.3.4.1 Discussion
- •11.3.5 Occipitocervical Fusion
- •11.3.5.1 Discussion
- •11.3.6 Anterior Cervical Fusion
- •11.3.6.1 Discussion
- •11.3.7.1 Discussion
- •11.3.8 Posterior Fusion
- •11.3.8.1 Discussion
- •11.3.9 Scoliosis Rods
- •11.3.9.1 Discussion
- •11.3.10 Vertebral Stapling
- •11.3.10.1 Discussion
- •11.3.11 Vertical Expandable Prosthetic Titanium Rib (VEPTR)
- •11.3.11.1 Discussion
- •11.3.12 Interbody Fusion
- •11.3.12.1 Discussion
- •11.4.1 Total Disc Replacement
- •11.4.1.1 Discussion
- •11.4.2.1 Discussion
- •11.4.3.1 Discussion
- •11.4.4 Dynamic Facet Replacement
- •11.4.4.1 Discussion
- •11.4.5 Dynamic Rods
- •11.4.5.1 Discussion
- •11.5.1 Overview
- •11.5.2.1 Discussion
- •11.5.3.1 Discussion
- •11.5.4.1 Discussion
- •11.5.5 Cerebrospinal Fluid Leak
- •11.5.5.1 Discussion
- •11.5.6.1 Discussion
- •11.5.7 Surgical Site Infections
- •11.5.7.1 Discussion
- •11.5.8 Postoperative Neuritis
- •11.5.8.1 Discussion
- •11.5.9 Arachnoiditis
- •11.5.9.1 Discussion
- •11.5.10.1 Discussion
- •11.5.11 Postoperative Synovial Cyst
- •11.5.11.1 Discussion
- •11.5.12 Residual/Recurrent Tumors
- •11.5.12.1 Discussion
- •11.5.13 Inclusion Cysts
- •11.5.13.1 Discussion
- •11.5.14.1 Discussion
- •11.5.15 Retained Surgical Tools
- •11.5.15.1 Discussion
- •11.5.16 Gossypiboma
- •11.5.16.1 Discussion
- •11.5.17.1 Discussion
- •11.5.18 Postoperative Deformity
- •11.5.18.1 Discussion
- •11.6.1 Discussion
- •11.7 Spinal Cord Stimulators
- •11.7.1 Discussion
- •11.8 Filum Terminale Sectioning
- •11.8.1 Discussion
- •11.9.1 Vertebral Augmentation
- •11.9.1.1 Discussion
- •11.9.2 Kiva Device
- •11.9.2.1 Discussion
- •11.9.3 Sacroplasty
- •11.9.3.1 Discussion
- •11.9.4.1 Discussion
- •11.9.5.1 Discussion
- •11.9.6.1 Discussion
- •Further Reading
- •Overview
- •Laminectomy
- •Facetectomy
- •Microdiscectomy
- •Laminoplasty
- •Vertebrectomy
- •Cordectomy
- •Bone Graft Materials
- •Implantable Bone Stimulators
- •Odontoid Screw Fixation
- •Anterior Cervical Fusion
- •Posterior Fusion
- •Occiptiocervical Fusion
- •Scoliosis Rods
- •Vertebral Stapling
- •Interbody Fusion
- •Nucleus Pulposus Replacement
- •Dynamic Facet Replacement
- •Dynamic Rods
- •Cerebrospinal Fluid Leak
- •Seromas and Hematomas
- •Postoperative Infection
- •Postoperative Neuritis
- •Arachnoiditis
- •Postoperative Synovial Cyst
- •Residual/Recurrent Tumors
- •Inclusion Cysts
- •Retained Surgical Tools
- •Gossypiboma
- •Postoperative Deformity
- •Intrathecal Spinal Infusion Pump
- •Spinal Cord Stimulators
- •Filum Terminale Sectioning
- •Kiva Device
- •Sacroplasty
- •Percutaneous Spine Fusion
- •CT-Guided Epidural Blood Patch
- •12.1 Vascular Surgery
- •12.1.1.1 Discussion
- •12.1.2.1 Discussion
- •12.1.3.1 Discussion
- •12.1.4.1 Discussion
- •12.1.6.1 Discussion
- •12.1.7 Carotid Endarterectomy
- •12.1.7.1 Discussion
- •12.1.8 Carotid Body Stimulation
- •12.1.8.1 Discussion
- •12.1.9 Adjustable Vascular Clamp
- •12.1.9.1 Discussion
- •12.1.10.1 Discussion
- •12.2 Endovascular Surgery
- •12.2.7 Endovascular Reconstructive Treatment for Acute Ischemic Stroke Using Intra-arterial Thrombolysis or Embolectomy
- •12.2.10 Endovascular Stent Reconstructive Treatment for Extracranial Cerebrovascular Occlusive Disease
- •12.2.11 Endovascular Reconstructive Treatment for Active Extracranial Hemorrhage or Pseudoaneurysm
- •Further Reading
- •Vascular Surgery
- •Aneurysm and Hemostatic Ligation Clips
- •Intracranial Aneurysm Muscle Wrap
- •Vascular Malformation Surgery
- •Carotid Endarterectomy
- •Carotid Body Stimulation
- •Adjustable Vascular Clamp
- •Reconstruction of the Great Vessels
- •Endovascular Surgery
- •General Imaging Considerations Following Endovascular Cerebrovascular Procedures
- •Endovascular Treatment for Aneurysms
- •Endovascular Stent Reconstructive Treatment for Extracranial Cerebrovascular Occlusive Disease
- •Endovascular Reconstructive Treatment for Active Extracranial Hemorrhage or Pseudoaneurysm
- •Endovascular Treatment for Intracranial Venous Stenosis and Occlusion
- •Index
2 Imaging the Postoperative Orbit |
33 |
|
|
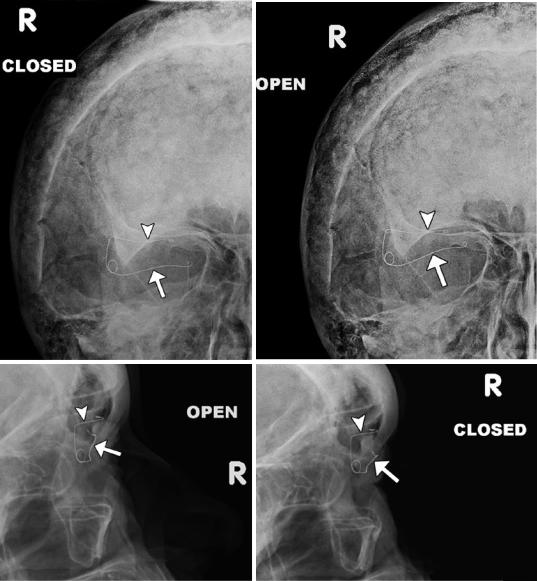
2.2\ Palpebral Springs
2.2.1\ Discussion
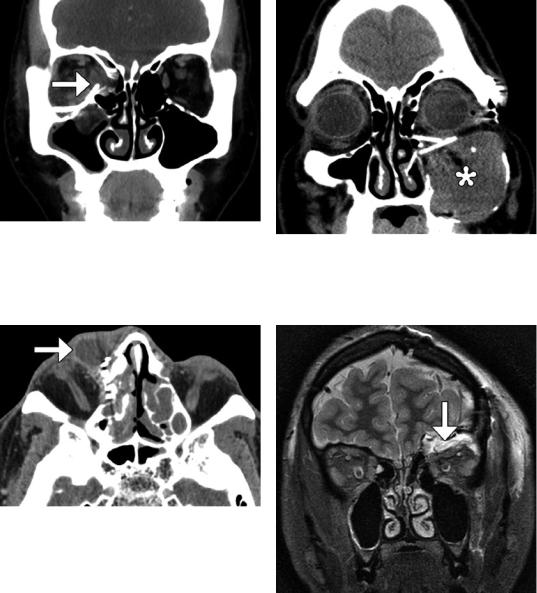
Palpebral springs may rarely be
used to treat patients with lagophthalmos secondary to facial nerve palsy. The device is implanted
a |
b |
c |
d |
via orbitotomy and consists of a palpebral branch and an orbital branch connected by a spring mechanism. The positioning and function of the device can be readily assessed on radiographs obtained in the open and closed lid positions, whereby the palpebral branch is expected to descend with lid closure (Fig. 2.2).
Fig.2.2 Eyelid spring. Open (a) and closed (b) lid frontal and open (c) and closed (d) lid lateral radiographs show the spring device to be well seated and functional. The palpebral branch (arrows) is noted to descend with respect to the orbital branch (arrowheads) during lid closure.
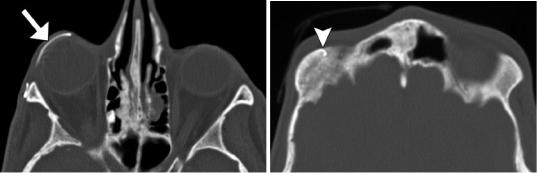
There are also stigmata of Paget’s disease in the skull. Axial CT images (e, f) in a different patient show the lower limb (arrow) of the spring properly positioned along the inner surface of the upper eyelid and the upper limb (arrowhead) implanted in the orbital roof
34 |
D.T. Ginat et al. |
|
|
e |
f |
Fig. 2.2 (continued)
2 Imaging the Postoperative Orbit |
35 |
|
|
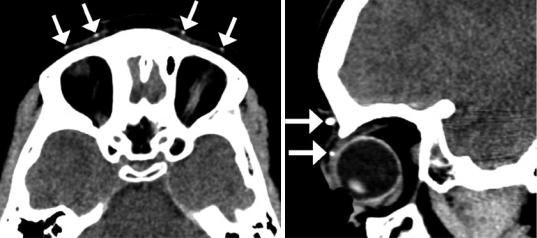
2.3\ Frontalis Suspension Ptosis
Repair
2.3.1\ Discussion
Frontalis suspension may be used to elevate severely drooping eyelids in cases where the levator palpebrae superioris muscle is weak. In this procedure, autologous or alloplastic material
a
is used to create a subcutaneous attachment between the eyelid and the frontalis muscle. Expanded polytetrafluoroethylene (ePTFE) strips are visible on CT as hyperattenuating material configured as a sling in the upper eyelid (Fig. 2.3) in order to suspend the eyelid to the frontalis muscle. Potential complications include infection and granuloma formation.
b
Fig 2.3 Frontalis suspension ptosis repair. The patient is a child with a history of bilateral ptosis due to Marcus Gunn jaw-winking syndrome. Axial (a) and sagittal (b)
CT images show the hyperattenuating sling in the upper eyelids (arrows)
36 |
D.T. Ginat et al. |
|
|
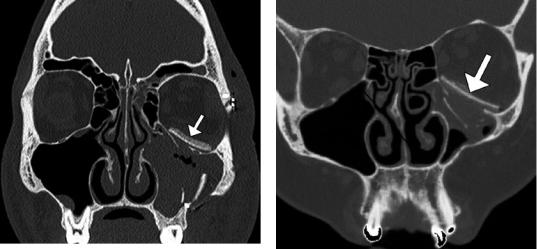
2.4\ Orbital Wall Reconstruction
and Augmentation
2.4.1\ Discussion
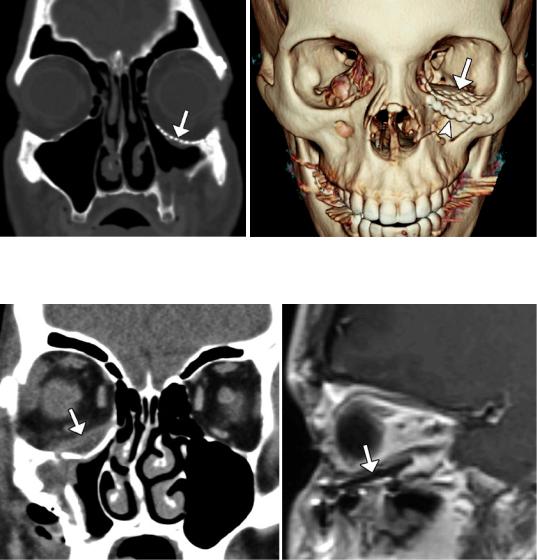
Traditionally, autologous cartilage or bone (Fig. 2.4), silicone sheet implants (Fig. 2.5), and metal plates or mesh (Fig. 2.6) have been used for orbital wall fracture repair. More recent implant technology, including porous polyethylene materials (Fig. 2.7), has resulted in improved biocompatibility. The porous structure enables rapid ingrowth of vascular structures, soft tissues, and bone. Furthermore, endoscopic transantral approaches are increasingly used in order to
avoid eyelid incisions. Wedge implants can be used to augment orbital volume in patients with enophthalmos (Fig. 2.8). Transnasal wires can also be inserted to stabilize the medial canthus in trauma patients (Fig. 2.9). The role of imaging after orbital fracture repair is mainly to asses for complications, which may include infection, hematic cyst formation, implant deformity, and malpositioning, which may be accompanied by mucocele or nasolacrimal duct cyst formation due to obstruction and cerebrospinal fluid (Figs. 2.10, 2.11, 2.12, 2.13, 2.14, 2.15, 2.16, and 2.17). The leaks can be associated with compression of orbital contents, but can resolve spontaneously.
Fig. 2.4 Bone graft. Coronal CT image shows graft (arrow) harvested from the iliac bone used to reconstruct the left orbital floor (Courtesy of Gregory Katzman MD, MBA)
Fig. 2.5 Silicone implant. Coronal CT image shows left orbital floor fracture reconstruction with silicone implant (arrow)
2 Imaging the Postoperative Orbit |
37 |
|
|
a |
b |
Fig. 2.6 Titanium mesh. Coronal (a) and 3D CT (b) images show left orbital floor fracture repair with titanium mesh (arrow) and inferior orbital rim fracture with malleable titanium plate (arrowhead)
a |
b |
Fig.2.7 Porous polyethylene implant. Coronal CT image (a) shows the intermediate-attenuation sheet implant (arrow) positioned along the right orbital floor beneath the
inferior rectus muscle. The implant (arrow) appears as low signal intensity on the sagittal T1-weighted MRI (b)
38 |
D.T. Ginat et al. |
|
|
a
Fig. 2.9 Medial canthus stabilization. Axial CT image shows numerous healed left orbital fractures that involved the medial canthus, which is secured by a transnasal metal wire (arrow)
b
Fig. 2.8 Wedge implants. Sagittal T1-weighted (a) and coronal T2-weighted (b) MR images show the two lowintensity nearly parallel lines of the implant in the floor of the left orbit (arrows)
Fig. 2.10 Infection. Coronal post-contrast CT image shows diffuse right preand postseptal orbital cellulitis following recent medial and inferior orbital floor fracture repair with titanium mesh

2 Imaging the Postoperative Orbit |
39 |
|
|
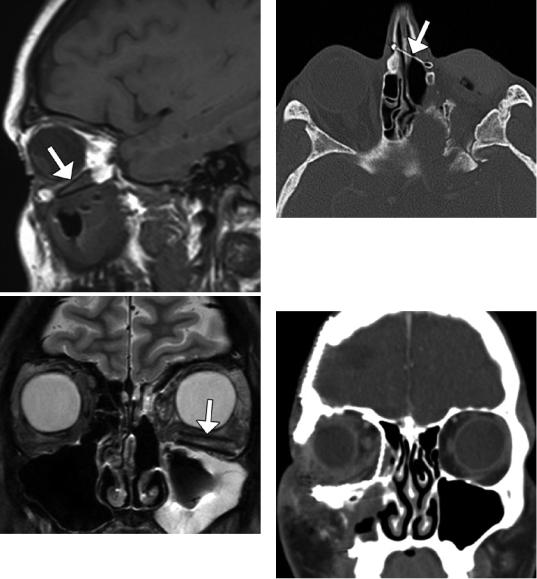
Fig. 2.11 Hematic cyst. Coronal CT image shows a right inferior intraorbital lenticular-shaped fluid collection (arrow) along the surface of a silastic plate
Fig. 2.12 Mesh deformity. Coronal CT image shows deformity of the orbital floor titanium mesh implant (arrow)
a |
b |
Fig. 2.13 Inferiorly positioned mesh. The patient presented with enophthalmos after left inferior orbital wall repair with titanium mesh. Coronal (a) and sagittal (b) CT images show inferior displacement of the left orbital mesh (arrows)
40 |
D.T. Ginat et al. |
|
|
Fig. 2.14 Rectus muscle impingement. Coronal CT image shows lateral right medial orbital wall titanium mesh impinging upon the swollen medial rectus muscle (arrow). There is also persistent herniation of right orbital contents
Fig. 2.15 Nasolacrimal duct obstruction. Axial CT image shows dilation of the right lacrimal sac (arrow) secondary to obstruction by titanium mesh
Fig. 2.16 Mucocele secondary to malpositioned implants. Coronal CT image shows an expansile left maxillary opacity (*) and obstruction of the infundibulum by the orbital floor reconstruction plates
Fig. 2.17 Cerebrospinal fluid leak. The patient underwent biopsy of a suspect orbital roof lesion with mesh reconstruction of the orbital roof. Coronal STIR MR image shows a fluid collection in the superior left orbit (arrow), with compression of the orbital contents
