
- •Foreword
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1.2 Forehead Augmentation
- •1.2.1 Discussion
- •1.3.1 Discussion
- •1.4 Rhinoplasty
- •1.4.1 Discussion
- •1.5 Lip Augmentation
- •1.5.1 Discussion
- •1.6 Chin and Jaw Augmentation
- •1.6.1 Discussion
- •Further Reading
- •Forehead Augmentation
- •Rhinoplasty
- •Lip Augmentation
- •Jaw Augmentation
- •2: Imaging the Postoperative Orbit
- •2.1 Eyelid Weights
- •2.1.1 Discussion
- •2.2 Palpebral Springs
- •2.2.1 Discussion
- •2.3.1 Discussion
- •2.4.1 Discussion
- •2.5.1 Discussion
- •2.6.1 Discussion
- •2.7 Strabismus Surgery
- •2.7.1 Discussion
- •2.8 Glaucoma Surgery
- •2.8.1 Discussion
- •2.9 Scleral Buckles
- •2.9.1 Discussion
- •2.10 Keratoprostheses
- •2.10.1 Discussion
- •2.11 Intraocular Lens Implants
- •2.11.1 Discussion
- •2.12 Surgical Aphakia
- •2.12.1 Discussion
- •2.13 Pneumatic Retinopexy
- •2.13.1 Discussion
- •2.14 Intraocular Silicone Oil
- •2.14.1 Discussion
- •2.15.1 Discussion
- •2.16 Orbital Tissue Expanders
- •2.16.1 Discussion
- •2.17 Orbital Exenteration
- •2.17.1 Discussion
- •2.18.1 Discussion
- •Further Reading
- •Eyelid Weights
- •Palpebral Spring
- •Frontalis Suspension Ptosis Repair
- •Strabismus Surgery
- •Glaucoma Surgery
- •Scleral Buckles
- •Keratoprostheses
- •Intraocular Lens Implants
- •Surgical Aphakia
- •Pneumatic Retinopexy
- •Intraocular Silicone Oil
- •Orbital Tissue Expanders
- •Orbital Exenteration
- •3.1.1 Discussion
- •3.2 Septoplasty
- •3.2.1 Discussion
- •3.3.1 Discussion
- •3.4.1 Discussion
- •3.5 Nasal Packing Material
- •3.5.1 Discussion
- •3.6 Rhinectomy
- •3.6.1 Discussion
- •3.7 Sinus Lift Procedure
- •3.7.1 Discussion
- •3.8 Caldwell-Luc Procedure
- •3.8.1 Discussion
- •3.9 External Ethmoidectomy
- •3.9.1 Discussion
- •3.10.1 Discussion
- •3.11 FESS Complications
- •3.11.1 Discussion
- •3.11.2 Discussion
- •3.11.3 Discussion
- •3.11.4 Discussion
- •3.11.5 Discussion
- •3.11.6 Discussion
- •3.11.7 Discussion
- •3.11.8 Discussion
- •3.11.9 Discussion
- •3.11.10 Discussion
- •3.11.11 Discussion
- •3.12 Osteoplastic Flap with Frontal Sinus Obliteration
- •3.12.1 Discussion
- •3.13 Frontal Sinus Cranialization
- •3.13.1 Discussion
- •3.14 Paranasal Sinus Stents
- •3.14.1 Discussion
- •3.15 Frontal Sinus Trephination
- •3.15.1 Discussion
- •3.16.1 Discussion
- •3.17.1 Discussion
- •3.18 Maxillary Swing
- •3.18.1 Discussion
- •Further Reading
- •Septoplasty
- •Nasal Septal Button Prosthesis
- •Nasal Packing Material
- •Rhinectomy
- •Sinus Lift
- •Caldwell-Luc Procedure
- •External Ethmoidectomy
- •Functional Endoscopic Sinus Surgery
- •FESS Complications
- •Osteoplastic Flap with Frontal Sinus Obliteration
- •Frontal Sinus Cranialization
- •Paranasal Sinus Stents
- •Frontal Sinus Trephination
- •Maxillectomy and Palatectomy
- •Maxillary Swing
- •4.1 Occipital Nerve Stimulator
- •4.1.1 Discussion
- •4.2 Tissue Expander
- •4.2.1 Discussion
- •4.3 Temporal Fossa Implants
- •4.3.1 Discussion
- •4.4.1 Discussion
- •4.5.1 Discussion
- •4.6.1 Discussion
- •4.7 Scalp Tumor Recurrence
- •4.7.1 Discussion
- •4.8 Burr Holes
- •4.8.1 Discussion
- •4.9 Craniotomy
- •4.9.1 Discussion
- •4.10 Cranioplasty
- •4.10.1 Discussion
- •4.11 Autocranioplasty
- •4.11.1 Discussion
- •4.12.1 Discussion
- •4.14.1 Discussion
- •4.15 Box Osteotomy
- •4.16.1 Discussion
- •4.17.1 Discussion
- •4.18.1 Discussion
- •4.19 Subdural Drainage Catheters
- •4.19.1 Discussion
- •4.20.1 Tension Pneumocephalus
- •4.20.5 Pseudomeningoceles
- •4.20.6 Pseudoaneurysm
- •4.20.7 Postoperative Infection
- •4.20.8 Textiloma
- •4.20.9 Sunken Skin Flap Syndrome
- •4.20.10 External Brain Herniation
- •4.20.11 Bone Flap Resorption
- •Further Reading
- •Occipital Nerve Stimulator
- •Tissue Expander
- •Temporal Fossa Implant
- •Scalp Tumor Recurrence
- •Box Osteotomy
- •Absorbable Hemostatic Agents
- •Duraplasty and Sealant Agents
- •Burr Holes
- •Craniotomy
- •Cranioplasty
- •Autocranioplasty
- •Cranial Vault Reconstruction for Craniosynostosis
- •Cranial Vault Encephalocele Repair
- •Subdural Drainage Catheters
- •Intracranial Pressure Monitor
- •Cranial Surgery Complications
- •5.1 Intraoperative MRI
- •5.1.1 Discussion
- •5.2.1 Stereotactic Biopsy
- •5.2.1.1 Discussion
- •5.2.2 Resection Cavities
- •5.2.2.1 Discussion
- •5.2.3 Ommaya Reservoirs
- •5.2.3.1 Discussion
- •5.2.4 Chemotherapy Wafers
- •5.2.4.1 Discussion
- •5.2.5 Brachytherapy Seeds
- •5.2.5.1 Discussion
- •5.2.6.1 Discussion
- •5.3.1 Prefrontal Lobotomy
- •5.3.1.1 Discussion
- •5.3.2 Pallidotomy
- •5.3.2.1 Discussion
- •5.3.3 Cingulotomy
- •5.3.3.1 Discussion
- •5.3.4.1 Discussion
- •5.3.4.2 Thalamotomy
- •5.3.5 Deep Brain Stimulation (DBS)
- •5.3.5.1 Discussion
- •5.3.6.1 Discussion
- •5.3.7.1 Discussion
- •5.3.8.1 Discussion
- •5.3.9.1 Discussion
- •5.3.10 Corticectomy
- •5.3.10.1 Discussion
- •5.3.11.1 Discussion
- •5.3.12.1 Discussion
- •5.3.13 Callosotomy
- •5.3.13.1 Discussion
- •5.3.14 Anterior Temporal Lobectomy
- •5.3.14.1 Discussion
- •5.3.15.1 Discussion
- •5.3.16 Hemispherectomy
- •5.3.16.1 Discussion
- •Further Reading
- •Intraoperative MRI
- •Brain Tumor Surgery
- •Stereotactic Biopsy
- •Resection Cavities
- •Postoperative Hemorrhagic Lesions
- •Ommaya Reservoirs
- •Chemotherapy Wafers
- •Brachytherapy Seeds
- •GliaSite Radiation Therapy System
- •Prefrontal Lobotomy
- •Pallidotomy
- •Cingulotomy
- •Thalamotomy
- •Deep Brain Stimulation (DBS)
- •Epidural Motor Cortex Stimulator
- •Neural Interface System (BrainGate)
- •Corticectomy
- •Selective Disconnection
- •Callosotomy
- •Anterior Temporal Lobectomy
- •Hemispherectomy
- •6.1 Types of Procedures
- •6.1.1 External Ventricular Drainage
- •6.1.1.1 Discussion
- •6.1.2.1 Discussion
- •6.1.3 Atypical Ventricular Shunts
- •6.1.3.1 Discussion
- •6.1.4 Ventriculosubgaleal Shunts
- •6.1.4.1 Discussion
- •6.1.5.1 Discussion
- •6.1.6.1 Discussion
- •6.1.7 Subdural-Peritoneal Shunts
- •6.1.7.1 Discussion
- •6.1.8.1 Discussion
- •6.1.9.1 Discussion
- •6.1.10 Lumboperitoneal Shunts
- •6.1.10.1 Discussion
- •6.1.11 Third Ventriculocisternostomy
- •6.1.11.1 Discussion
- •6.1.12.1 Discussion
- •6.1.13 Aqueductoplasty
- •6.1.13.1 Discussion
- •6.1.14.1 Discussion
- •6.2.1.1 Discussion
- •6.2.2.1 Discussion
- •6.2.3 Intraventricular Fat Migration
- •6.2.3.1 Discussion
- •6.2.4.1 Discussion
- •6.2.5.1 Discussion
- •6.2.6 Slit Ventricle Syndrome
- •6.2.6.1 Discussion
- •6.2.7.1 Discussion
- •6.2.8 Shunt-Associated Infections
- •6.2.8.1 Discussion
- •6.2.9.1 Discussion
- •6.2.10.1 Discussion
- •6.2.11.1 Discussion
- •6.2.12 Peritoneal Pseudocysts
- •6.2.12.1 Discussion
- •6.2.13.1 Discussion
- •6.2.14 Tumor Seeding
- •6.2.14.1 Discussion
- •6.2.15 Shunt Catheter Calcification
- •6.2.15.1 Discussion
- •6.2.16.1 Discussion
- •6.2.17.1 Discussion
- •Further Reading
- •Types of Procedures
- •External Ventricular Drainage
- •Ventriculoperitoneal Shunts
- •Atypical Ventricular Shunts
- •Ventriculosubgaleal Shunts
- •Subdural-Peritoneal Shunts
- •Lumboperitoneal Shunt
- •Third Ventriculostomy
- •Aqueductoplasty
- •Fourth Ventricular Stenting
- •Complications
- •Intraventricular Fat Migration
- •Slit Ventricle Syndrome
- •Shunt-Associated Infections
- •Shunt Malposition and Migration
- •Pseudocysts
- •Cerebrospinal Fluid Leak Syndrome
- •Tumor Seeding
- •Shunt Catheter Calcifications
- •7.1.1 Discussion
- •7.2.1 Discussion
- •7.3.1 Discussion
- •7.4.1 Discussion
- •7.5.1 Discussion
- •7.6.1 Discussion
- •7.7 Radiosurgery for Vestibular Schwannomas
- •7.7.1 Discussion
- •Further Reading
- •Anterior Craniofacial Resection
- •Transsphenoidal Resection
- •Middle Cranial Fossa Reconstruction
- •Surgical Approaches for Vestibular Schwannoma Resection
- •8.1.1 Discussion
- •8.2 Auriculectomy
- •8.2.1 Discussion
- •8.3 Auricular Reconstruction
- •8.3.1 Discussion
- •8.4.1 Discussion
- •8.5 Atresiaplasty
- •8.5.1 Discussion
- •8.6.1 Discussion
- •8.7.1 Discussion
- •8.8 Ossicular Interposition
- •8.8.1 Discussion
- •8.9.1 Discussion
- •8.10.1 Discussion
- •8.11.1 Discussion
- •8.12 Atticotomy
- •8.12.1 Discussion
- •8.13.1 Discussion
- •8.14.1 Discussion
- •8.15.1 Discussion
- •8.16 Temporal Bone Resection
- •8.16.1 Discussion
- •8.17 Cochlear Implants
- •8.17.1 Discussion
- •8.18.1 Discussion
- •8.19.1 Discussion
- •8.20.1 Discussion
- •8.21.1 Discussion
- •8.22 Labyrinthectomy
- •8.22.1 Discussion
- •8.23 Vestibular Nerve Section
- •8.23.1 Discussion
- •8.24.1 Discussion
- •8.25.1 Discussion
- •Further Reading
- •BAHA Device
- •Auriculectomy
- •Auricular Reconstruction
- •Canaloplasty and Meatoplasty
- •Atresiaplasty
- •Myringoplasty and Tympanoplasty
- •Incus Interposition
- •Ossicular Prosthesis Complications
- •Transcanal Atticotomy
- •Mastoidectomy Complications
- •Lateral Temporal Bone Resection
- •Cochlear Implants
- •Cochlear Implant Complications
- •Auditory Brainstem Stimulator
- •Repair of Perilymphatic Fistula
- •Labyrinthectomy
- •Vestibular Nerve Sectioning
- •Tube Drainage of Cholesterol Cysts
- •9.1 Vertical Ramus Osteotomy
- •9.1.1 Discussion
- •9.2 Sagittal Split Osteotomy
- •9.2.1 Discussion
- •9.3 Genioplasty
- •9.3.1 Discussion
- •9.4.1 Discussion
- •9.5 Mandibular Distraction
- •9.5.1 Discussion
- •9.6 LeFort I Osteotomy
- •9.6.1 Discussion
- •9.7 LeFort III Osteotomy
- •9.7.1 Discussion
- •9.8.1 Discussion
- •9.9 Mandibulotomy
- •9.9.1 Discussion
- •9.10 Enucleation
- •9.10.1 Discussion
- •9.11 Cyst Decompression
- •9.11.1 Discussion
- •9.12 Coronoidectomy
- •9.12.1 Discussion
- •9.13.1 Discussion
- •9.14.1 Discussion
- •9.15.1 Discussion
- •9.16.1 Discussion
- •9.17.1 Discussion
- •9.18.1 Discussion
- •9.19.1 Discussion
- •9.20.1 Discussion
- •Further Reading
- •Vertical Ramus Osteotomy
- •Sagittal Split Osteotomy
- •Genioplasty
- •Mandibular Angle Augmentation
- •Mandibular Distraction
- •Lefort I Surgery
- •Lefort III Surgery
- •Fixation of Mandible Fractures
- •Mandibulotomy
- •Enucleation
- •Cyst Decompression
- •Coronoidectomy
- •Eminectomy and Meniscal Plication
- •10: Imaging the Postoperative Neck
- •10.1 Reconstruction Flaps
- •10.1.1 Discussion
- •10.2 Neck Dissection
- •10.2.1 Discussion
- •10.3 Parotidectomy
- •10.3.1 Discussion
- •10.4.1 Discussion
- •10.5 Facial Reanimation
- •10.5.1 Discussion
- •10.6.1 Discussion
- •10.7.1 Discussion
- •10.8 Transoral Robotic Surgery
- •10.8.1 Discussion
- •10.9 Sistrunk Procedure
- •10.9.1 Discussion
- •10.10 Laryngectomy
- •10.10.1 Discussion
- •10.11.1 Discussion
- •10.12 Montgomery T-Tubes
- •10.12.1 Discussion
- •10.13 Salivary Bypass Stent
- •10.13.1 Discussion
- •10.14 Laryngeal Stents
- •10.14.1 Discussion
- •10.15.1 Discussion
- •10.16 Arytenoid Adduction
- •10.16.1 Discussion
- •10.17 Arytenoidectomy
- •10.17.1 Discussion
- •10.18 Laryngeal Cartilage Remodeling
- •10.18.1 Discussion
- •10.19 Tracheotomy
- •10.19.1 Discussion
- •10.20 Thyroidectomy
- •10.20.1 Discussion
- •10.21.1 Discussion
- •10.22 Brachytherapy
- •10.22.1 Discussion
- •10.23 Vagal Nerve Stimulation
- •10.23.1 Discussion
- •Further Reading
- •Reconstruction Flaps
- •Facial Reanimation
- •Tonsillectomy and Adenoidectomy
- •Transoral Robotic Surgery
- •Neck Dissection
- •Parotidectomy
- •Salivary Duct Stenting
- •Laryngectomy
- •Montgomery T-Tubes
- •Salivary Bypass Stents
- •Laryngeal Stents
- •Arytenoid Adduction
- •Arytenoidectomy
- •Laryngeal Cartilage Remodeling
- •Tracheotomy
- •Thyroidectomy
- •Neck Exploration and Parathyroidectomy
- •Sistrunk Procedure
- •Brachytherapy
- •Vagal Nerve Stimulation
- •11: Imaging of Postoperative Spine
- •11.1 Overview
- •11.2 Spine Decompression
- •11.2.1.1 Discussion
- •11.2.2 Laminectomy
- •11.2.2.1 Discussion
- •11.2.3 Facetectomy
- •11.2.3.1 Discussion
- •11.2.4 Microdiscectomy
- •11.2.4.1 Discussion
- •11.2.5 Laminoplasty
- •11.2.5.1 Discussion
- •11.2.6 Vertebrectomy
- •11.2.6.1 Discussion
- •11.2.7 Cordectomy
- •11.2.7.1 Discussion
- •11.3.1 Halo and Traction Devices
- •11.3.1.1 Discussion
- •11.3.2 Bone Graft Materials
- •11.3.2.1 Discussion
- •11.3.3 Implantable Bone Stimulators
- •11.3.3.1 Discussion
- •11.3.4 Odontoid Screw Fixation
- •11.3.4.1 Discussion
- •11.3.5 Occipitocervical Fusion
- •11.3.5.1 Discussion
- •11.3.6 Anterior Cervical Fusion
- •11.3.6.1 Discussion
- •11.3.7.1 Discussion
- •11.3.8 Posterior Fusion
- •11.3.8.1 Discussion
- •11.3.9 Scoliosis Rods
- •11.3.9.1 Discussion
- •11.3.10 Vertebral Stapling
- •11.3.10.1 Discussion
- •11.3.11 Vertical Expandable Prosthetic Titanium Rib (VEPTR)
- •11.3.11.1 Discussion
- •11.3.12 Interbody Fusion
- •11.3.12.1 Discussion
- •11.4.1 Total Disc Replacement
- •11.4.1.1 Discussion
- •11.4.2.1 Discussion
- •11.4.3.1 Discussion
- •11.4.4 Dynamic Facet Replacement
- •11.4.4.1 Discussion
- •11.4.5 Dynamic Rods
- •11.4.5.1 Discussion
- •11.5.1 Overview
- •11.5.2.1 Discussion
- •11.5.3.1 Discussion
- •11.5.4.1 Discussion
- •11.5.5 Cerebrospinal Fluid Leak
- •11.5.5.1 Discussion
- •11.5.6.1 Discussion
- •11.5.7 Surgical Site Infections
- •11.5.7.1 Discussion
- •11.5.8 Postoperative Neuritis
- •11.5.8.1 Discussion
- •11.5.9 Arachnoiditis
- •11.5.9.1 Discussion
- •11.5.10.1 Discussion
- •11.5.11 Postoperative Synovial Cyst
- •11.5.11.1 Discussion
- •11.5.12 Residual/Recurrent Tumors
- •11.5.12.1 Discussion
- •11.5.13 Inclusion Cysts
- •11.5.13.1 Discussion
- •11.5.14.1 Discussion
- •11.5.15 Retained Surgical Tools
- •11.5.15.1 Discussion
- •11.5.16 Gossypiboma
- •11.5.16.1 Discussion
- •11.5.17.1 Discussion
- •11.5.18 Postoperative Deformity
- •11.5.18.1 Discussion
- •11.6.1 Discussion
- •11.7 Spinal Cord Stimulators
- •11.7.1 Discussion
- •11.8 Filum Terminale Sectioning
- •11.8.1 Discussion
- •11.9.1 Vertebral Augmentation
- •11.9.1.1 Discussion
- •11.9.2 Kiva Device
- •11.9.2.1 Discussion
- •11.9.3 Sacroplasty
- •11.9.3.1 Discussion
- •11.9.4.1 Discussion
- •11.9.5.1 Discussion
- •11.9.6.1 Discussion
- •Further Reading
- •Overview
- •Laminectomy
- •Facetectomy
- •Microdiscectomy
- •Laminoplasty
- •Vertebrectomy
- •Cordectomy
- •Bone Graft Materials
- •Implantable Bone Stimulators
- •Odontoid Screw Fixation
- •Anterior Cervical Fusion
- •Posterior Fusion
- •Occiptiocervical Fusion
- •Scoliosis Rods
- •Vertebral Stapling
- •Interbody Fusion
- •Nucleus Pulposus Replacement
- •Dynamic Facet Replacement
- •Dynamic Rods
- •Cerebrospinal Fluid Leak
- •Seromas and Hematomas
- •Postoperative Infection
- •Postoperative Neuritis
- •Arachnoiditis
- •Postoperative Synovial Cyst
- •Residual/Recurrent Tumors
- •Inclusion Cysts
- •Retained Surgical Tools
- •Gossypiboma
- •Postoperative Deformity
- •Intrathecal Spinal Infusion Pump
- •Spinal Cord Stimulators
- •Filum Terminale Sectioning
- •Kiva Device
- •Sacroplasty
- •Percutaneous Spine Fusion
- •CT-Guided Epidural Blood Patch
- •12.1 Vascular Surgery
- •12.1.1.1 Discussion
- •12.1.2.1 Discussion
- •12.1.3.1 Discussion
- •12.1.4.1 Discussion
- •12.1.6.1 Discussion
- •12.1.7 Carotid Endarterectomy
- •12.1.7.1 Discussion
- •12.1.8 Carotid Body Stimulation
- •12.1.8.1 Discussion
- •12.1.9 Adjustable Vascular Clamp
- •12.1.9.1 Discussion
- •12.1.10.1 Discussion
- •12.2 Endovascular Surgery
- •12.2.7 Endovascular Reconstructive Treatment for Acute Ischemic Stroke Using Intra-arterial Thrombolysis or Embolectomy
- •12.2.10 Endovascular Stent Reconstructive Treatment for Extracranial Cerebrovascular Occlusive Disease
- •12.2.11 Endovascular Reconstructive Treatment for Active Extracranial Hemorrhage or Pseudoaneurysm
- •Further Reading
- •Vascular Surgery
- •Aneurysm and Hemostatic Ligation Clips
- •Intracranial Aneurysm Muscle Wrap
- •Vascular Malformation Surgery
- •Carotid Endarterectomy
- •Carotid Body Stimulation
- •Adjustable Vascular Clamp
- •Reconstruction of the Great Vessels
- •Endovascular Surgery
- •General Imaging Considerations Following Endovascular Cerebrovascular Procedures
- •Endovascular Treatment for Aneurysms
- •Endovascular Stent Reconstructive Treatment for Extracranial Cerebrovascular Occlusive Disease
- •Endovascular Reconstructive Treatment for Active Extracranial Hemorrhage or Pseudoaneurysm
- •Endovascular Treatment for Intracranial Venous Stenosis and Occlusion
- •Index
646 |
D.T. Ginat et al. |
|
|
12.1.7\ Carotid Endarterectomy
12.1.7.1\ Discussion
Carotid endarterectomy (CEA) is considered the treatment of choice for symptomatic and asymptomatic patients with high-grade carotid artery stenosis. In order to appropriately interpret imaging studies obtained following CEA, it is helpful to be familiar with the surgical techniques involved.
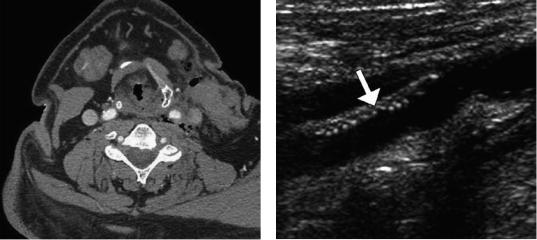
CEA can be performed through an incision made anterior to the sternocleidomastoid and ligation of the facial vein in order to expose the carotid bifurcation and clamping of the carotid artery distal to the endarterectomy. Consequently, a small hematoma within or adjacent to the sternocleidomastoid and mild circumferential narrowing of the carotid artery resulting from clamp placement during surgery can be appreciated on follow-up CT (Fig. 12.25). These findings are usually self-limited.
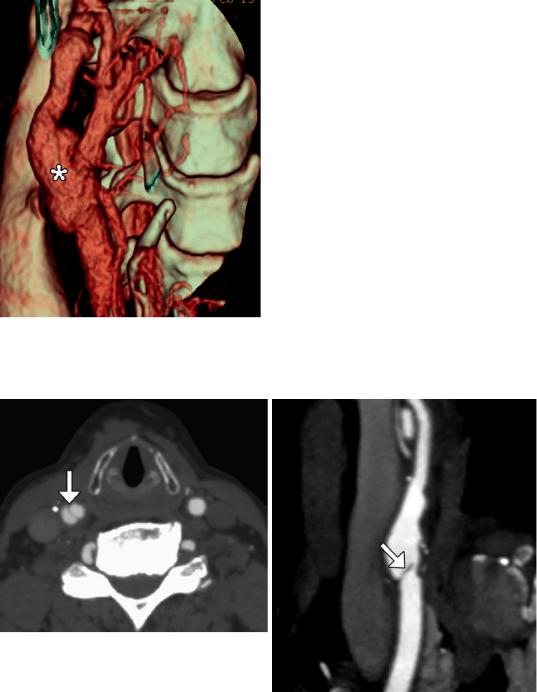
CEA involves opening the carotid artery, removing the plaque and associated endothelium, and suturing the vessel wall closed with or without an enlargement patch. The patch is usually composed of Dacron, which is not readily visible on CT, but can appear as a thin hyperechoic mesh on ultrasound (Fig. 12.26). Alternatively, the section of carotid artery that is resected can be reconstructed using a saphenous vein graft. This has a distinct patulous or bulbous appearance on imaging (Fig. 12.27).
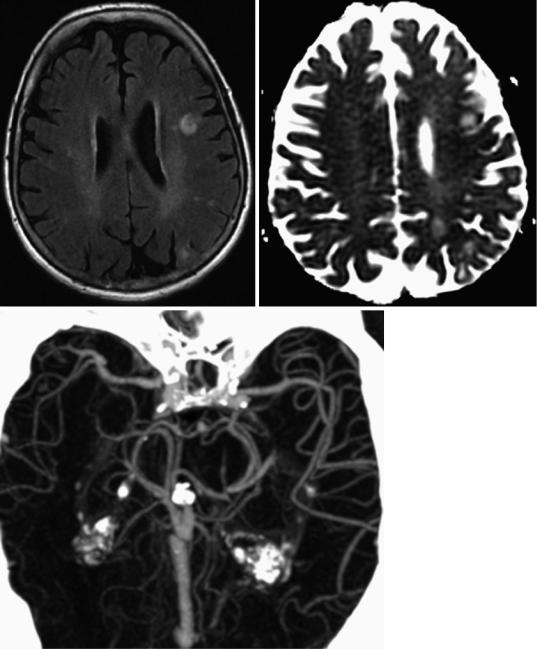
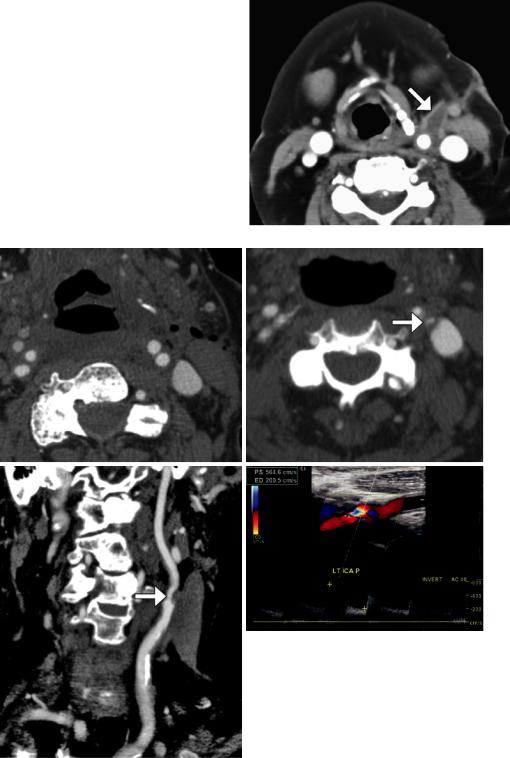
Complications related to CEA include localized intimal flap or dissection, reperfusion syndrome, patch infection, restenosis, cerebral infarction, and cranial nerve injury, usually facial and hypoglossal (Figs. 12.28, 12.29, 12.30, 12.31, 12.32, and 12.33).
Wound infection following carotid endarterectomy occurs in about 2% of cases. Staphylococcus
species are the most common causative organisms. Patients typically present with wound swelling, drainage, and fever. On imaging, abscess appears as a fluid collection that abuts the surgical site. Characteristic rim enhancement and cellulitis are often present. There may also be debris, septations, and draining sinus that extends from the operative bed to the incision. Wound abscesses usually resolve with antibiotics and debridement. However, periarterial abscess or patch infection may predispose to dehiscence of the suture line, resulting in pseudoaneurysm formation.
Hyperperfusion or reperfusion syndrome is an unusual complication of carotid endarterectomy or carotid artery stenting, occurring in 0.3–1.2% of cases. A possible etiology for this condition is impaired cerebrovascular autoregulation. Predisposing factors include severe underlying cerebrovascular disease, diabetes mellitus, long- standing hypertension, prolonged cross clamping during endarterectomy, and a greater than 100% increase in the degree of reestablished cerebral blood flow, which is usually associated with greater than 90% carotid artery stenosis. Patients may present with headaches, seizures, focal neurological deficits, or confusion within several days after surgery. Patients may recover completely if the diagnosis is made promptly. However, in some series, there is a mortality rate of up to 50%. The diagnosis of cerebral hyperperfusion syndrome can be suggested on CT in the proper setting by noting the presence of edema, often in the watershed zones ipsilateral to the side of surgery. On MRI, focal ipsilateral vasogenic edema is apparent. Diffusion-weighted imaging and apparent diffusion coefficient maps help confirm the presence of vasogenic edema. On MRA, prominent vessels on the affected side may be apparent. Similarly, perfusion-weighted imaging
12 Imaging of Vascular and Endovascular Surgery |
647 |
|
|
can depict the relative increased flow to the affected side. The finding of hemorrhage portends a poor prognosis. Imaging can help identify hyperperfusion syndrome before serious sequelae result. Differential considerations for the imaging appearance of cerebral hyperperfusion syndrome include hypertensive encephalopathy, cyclosporine toxicity, and eclampsia. The lack of restricted diffusion helps exclude cerebral ischemia.
Recurrent stenosis after carotid endarterectomy occurs at the rate of about 1% per year. This complication is the main limitation of carotid endarterectomy and predisposes to cerebrovascular ischemia. Acute thrombotic occlusion is much less common and is a potentially devastating complication that can result in cerebral infection. Conventional carotid end-
arterectomy with patch angioplasty and the use of lipid-lowering pharmaceuticals are associated with lower rates of restenosis. Risk factors for restenosis include female gender and renal failure. CTA, MRA, and Doppler ultrasound are all appropriate for evaluation of suspected restenosis or occlusion after carotid endarterectomy. Each of these modalities has advantages and disadvantages. CTA with reformats, especially the curved planar reformats, is useful for studying stenoses. In the setting of carotid endarterectomy with patching, the internal carotid artery velocities on Doppler ultrasound must be interpreted with caution, since these are normally higher than in the nonoperated counterparts. MRA is best suited for identifying pseudo-occlusions.
Fig. 12.25 Expected carotid endarterectomy early postoperative changes. Axial contrast CT after recent CEA demonstrates several foci of air scattered within and adjacent to the surgical bed, left sternocleidomastoid swelling, and edema in the fat planes
Fig. 12.26 Patch endarterectomy ultrasound image shows the echogenic Dacron patch (arrow) in the proximal internal carotid artery
648 |
D.T. Ginat et al. |
|
|
Fig. 12.27 Endarterectomy with saphenous vein graft. 3D CT image shows a patulous reconstructed right carotid bifurcation (*)
a |
b |
Fig. 12.28 Localized intimal flap. Axial (a) and curved planar reformatted (b) CT images show a linear filling defect (arrows) at the junction of the endarterectomy patch and native carotid artery
12 Imaging of Vascular and Endovascular Surgery |
649 |
|
|
a |
b |
c
Fig. 12.29 Reperfusion syndrome. The patient presented with acute onset of seizures 1 week status post left carotid endarterectomy . Axial FLAIR MRI (a) and ADC map (b) show areas of high T2 signal with elevated diffusivity in
the left cerebral hemisphere watershed zones. CTA MIP image (c) shows asymmetrically prominent left middle cerebral artery branches diffusely
650 |
D.T. Ginat et al. |
|
|
Fig. 12.30 Patch infection. The patient presented with fever, swelling, and purulent drainage from the left carotid endarterectomy incision site. Axial CT image shows a rim-enhancing fluid collection (arrow) surrounding the left carotid artery surgical bed
a |
b |
c |
d |
Fig. 12.31 Carotid artery restenosis. Initial postoperative axial CTA image (a) shows a patent proximal left internal carotid artery. Axial (b) and curved planar reformatted (c) CTA images obtained 6 months later now show focal high-grade stenosis at the origin of the left internal
carotid artery due to low-density plaque at the site of reanastomosis (arrows). Doppler ultrasound (d) confirms the presence of high-grade stenosis of the proximal internal carotid artery with turbulent flow and velocities surpassing 500 cm/s
12 Imaging of Vascular and Endovascular Surgery |
651 |
|
|
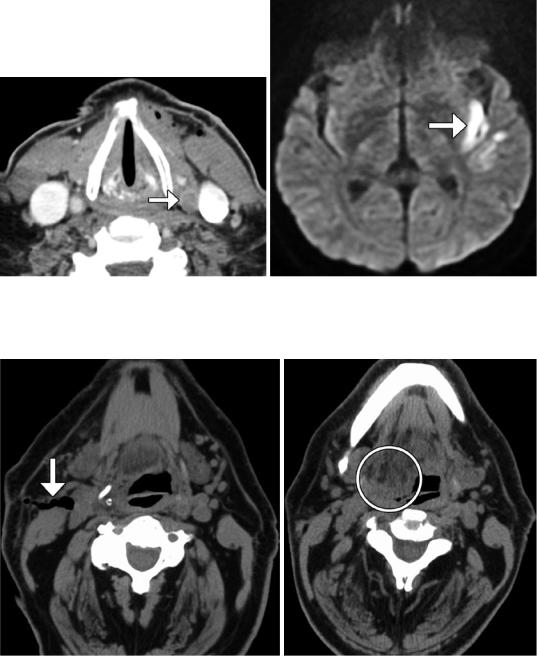
b
a
Fig. 12.32 Post-endarterectomy carotid artery occlusion and cerebral infarction. Delayed phase axial CTA image (a) shows occlusion of the CCA at the site of recent CEA
(arrow). The diffusion-weighted image (b) shows an associated left internal capsule/insula infarction (arrow)
a |
b |
Fig. 12.33 Cranial nerve injury. The patient presented with right cranial nerve XII deficit after right internal carotid endarterectomy. Initial postoperative axial CT image (a) shows that the endarterectomy was performed
at the expected level of the right hypoglossal nerve (arrow). A subsequent axial CT image (b) shows prolapse and fatty infiltration of the right hemi-tongue (encircled)
