
- •Foreword
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1.2 Forehead Augmentation
- •1.2.1 Discussion
- •1.3.1 Discussion
- •1.4 Rhinoplasty
- •1.4.1 Discussion
- •1.5 Lip Augmentation
- •1.5.1 Discussion
- •1.6 Chin and Jaw Augmentation
- •1.6.1 Discussion
- •Further Reading
- •Forehead Augmentation
- •Rhinoplasty
- •Lip Augmentation
- •Jaw Augmentation
- •2: Imaging the Postoperative Orbit
- •2.1 Eyelid Weights
- •2.1.1 Discussion
- •2.2 Palpebral Springs
- •2.2.1 Discussion
- •2.3.1 Discussion
- •2.4.1 Discussion
- •2.5.1 Discussion
- •2.6.1 Discussion
- •2.7 Strabismus Surgery
- •2.7.1 Discussion
- •2.8 Glaucoma Surgery
- •2.8.1 Discussion
- •2.9 Scleral Buckles
- •2.9.1 Discussion
- •2.10 Keratoprostheses
- •2.10.1 Discussion
- •2.11 Intraocular Lens Implants
- •2.11.1 Discussion
- •2.12 Surgical Aphakia
- •2.12.1 Discussion
- •2.13 Pneumatic Retinopexy
- •2.13.1 Discussion
- •2.14 Intraocular Silicone Oil
- •2.14.1 Discussion
- •2.15.1 Discussion
- •2.16 Orbital Tissue Expanders
- •2.16.1 Discussion
- •2.17 Orbital Exenteration
- •2.17.1 Discussion
- •2.18.1 Discussion
- •Further Reading
- •Eyelid Weights
- •Palpebral Spring
- •Frontalis Suspension Ptosis Repair
- •Strabismus Surgery
- •Glaucoma Surgery
- •Scleral Buckles
- •Keratoprostheses
- •Intraocular Lens Implants
- •Surgical Aphakia
- •Pneumatic Retinopexy
- •Intraocular Silicone Oil
- •Orbital Tissue Expanders
- •Orbital Exenteration
- •3.1.1 Discussion
- •3.2 Septoplasty
- •3.2.1 Discussion
- •3.3.1 Discussion
- •3.4.1 Discussion
- •3.5 Nasal Packing Material
- •3.5.1 Discussion
- •3.6 Rhinectomy
- •3.6.1 Discussion
- •3.7 Sinus Lift Procedure
- •3.7.1 Discussion
- •3.8 Caldwell-Luc Procedure
- •3.8.1 Discussion
- •3.9 External Ethmoidectomy
- •3.9.1 Discussion
- •3.10.1 Discussion
- •3.11 FESS Complications
- •3.11.1 Discussion
- •3.11.2 Discussion
- •3.11.3 Discussion
- •3.11.4 Discussion
- •3.11.5 Discussion
- •3.11.6 Discussion
- •3.11.7 Discussion
- •3.11.8 Discussion
- •3.11.9 Discussion
- •3.11.10 Discussion
- •3.11.11 Discussion
- •3.12 Osteoplastic Flap with Frontal Sinus Obliteration
- •3.12.1 Discussion
- •3.13 Frontal Sinus Cranialization
- •3.13.1 Discussion
- •3.14 Paranasal Sinus Stents
- •3.14.1 Discussion
- •3.15 Frontal Sinus Trephination
- •3.15.1 Discussion
- •3.16.1 Discussion
- •3.17.1 Discussion
- •3.18 Maxillary Swing
- •3.18.1 Discussion
- •Further Reading
- •Septoplasty
- •Nasal Septal Button Prosthesis
- •Nasal Packing Material
- •Rhinectomy
- •Sinus Lift
- •Caldwell-Luc Procedure
- •External Ethmoidectomy
- •Functional Endoscopic Sinus Surgery
- •FESS Complications
- •Osteoplastic Flap with Frontal Sinus Obliteration
- •Frontal Sinus Cranialization
- •Paranasal Sinus Stents
- •Frontal Sinus Trephination
- •Maxillectomy and Palatectomy
- •Maxillary Swing
- •4.1 Occipital Nerve Stimulator
- •4.1.1 Discussion
- •4.2 Tissue Expander
- •4.2.1 Discussion
- •4.3 Temporal Fossa Implants
- •4.3.1 Discussion
- •4.4.1 Discussion
- •4.5.1 Discussion
- •4.6.1 Discussion
- •4.7 Scalp Tumor Recurrence
- •4.7.1 Discussion
- •4.8 Burr Holes
- •4.8.1 Discussion
- •4.9 Craniotomy
- •4.9.1 Discussion
- •4.10 Cranioplasty
- •4.10.1 Discussion
- •4.11 Autocranioplasty
- •4.11.1 Discussion
- •4.12.1 Discussion
- •4.14.1 Discussion
- •4.15 Box Osteotomy
- •4.16.1 Discussion
- •4.17.1 Discussion
- •4.18.1 Discussion
- •4.19 Subdural Drainage Catheters
- •4.19.1 Discussion
- •4.20.1 Tension Pneumocephalus
- •4.20.5 Pseudomeningoceles
- •4.20.6 Pseudoaneurysm
- •4.20.7 Postoperative Infection
- •4.20.8 Textiloma
- •4.20.9 Sunken Skin Flap Syndrome
- •4.20.10 External Brain Herniation
- •4.20.11 Bone Flap Resorption
- •Further Reading
- •Occipital Nerve Stimulator
- •Tissue Expander
- •Temporal Fossa Implant
- •Scalp Tumor Recurrence
- •Box Osteotomy
- •Absorbable Hemostatic Agents
- •Duraplasty and Sealant Agents
- •Burr Holes
- •Craniotomy
- •Cranioplasty
- •Autocranioplasty
- •Cranial Vault Reconstruction for Craniosynostosis
- •Cranial Vault Encephalocele Repair
- •Subdural Drainage Catheters
- •Intracranial Pressure Monitor
- •Cranial Surgery Complications
- •5.1 Intraoperative MRI
- •5.1.1 Discussion
- •5.2.1 Stereotactic Biopsy
- •5.2.1.1 Discussion
- •5.2.2 Resection Cavities
- •5.2.2.1 Discussion
- •5.2.3 Ommaya Reservoirs
- •5.2.3.1 Discussion
- •5.2.4 Chemotherapy Wafers
- •5.2.4.1 Discussion
- •5.2.5 Brachytherapy Seeds
- •5.2.5.1 Discussion
- •5.2.6.1 Discussion
- •5.3.1 Prefrontal Lobotomy
- •5.3.1.1 Discussion
- •5.3.2 Pallidotomy
- •5.3.2.1 Discussion
- •5.3.3 Cingulotomy
- •5.3.3.1 Discussion
- •5.3.4.1 Discussion
- •5.3.4.2 Thalamotomy
- •5.3.5 Deep Brain Stimulation (DBS)
- •5.3.5.1 Discussion
- •5.3.6.1 Discussion
- •5.3.7.1 Discussion
- •5.3.8.1 Discussion
- •5.3.9.1 Discussion
- •5.3.10 Corticectomy
- •5.3.10.1 Discussion
- •5.3.11.1 Discussion
- •5.3.12.1 Discussion
- •5.3.13 Callosotomy
- •5.3.13.1 Discussion
- •5.3.14 Anterior Temporal Lobectomy
- •5.3.14.1 Discussion
- •5.3.15.1 Discussion
- •5.3.16 Hemispherectomy
- •5.3.16.1 Discussion
- •Further Reading
- •Intraoperative MRI
- •Brain Tumor Surgery
- •Stereotactic Biopsy
- •Resection Cavities
- •Postoperative Hemorrhagic Lesions
- •Ommaya Reservoirs
- •Chemotherapy Wafers
- •Brachytherapy Seeds
- •GliaSite Radiation Therapy System
- •Prefrontal Lobotomy
- •Pallidotomy
- •Cingulotomy
- •Thalamotomy
- •Deep Brain Stimulation (DBS)
- •Epidural Motor Cortex Stimulator
- •Neural Interface System (BrainGate)
- •Corticectomy
- •Selective Disconnection
- •Callosotomy
- •Anterior Temporal Lobectomy
- •Hemispherectomy
- •6.1 Types of Procedures
- •6.1.1 External Ventricular Drainage
- •6.1.1.1 Discussion
- •6.1.2.1 Discussion
- •6.1.3 Atypical Ventricular Shunts
- •6.1.3.1 Discussion
- •6.1.4 Ventriculosubgaleal Shunts
- •6.1.4.1 Discussion
- •6.1.5.1 Discussion
- •6.1.6.1 Discussion
- •6.1.7 Subdural-Peritoneal Shunts
- •6.1.7.1 Discussion
- •6.1.8.1 Discussion
- •6.1.9.1 Discussion
- •6.1.10 Lumboperitoneal Shunts
- •6.1.10.1 Discussion
- •6.1.11 Third Ventriculocisternostomy
- •6.1.11.1 Discussion
- •6.1.12.1 Discussion
- •6.1.13 Aqueductoplasty
- •6.1.13.1 Discussion
- •6.1.14.1 Discussion
- •6.2.1.1 Discussion
- •6.2.2.1 Discussion
- •6.2.3 Intraventricular Fat Migration
- •6.2.3.1 Discussion
- •6.2.4.1 Discussion
- •6.2.5.1 Discussion
- •6.2.6 Slit Ventricle Syndrome
- •6.2.6.1 Discussion
- •6.2.7.1 Discussion
- •6.2.8 Shunt-Associated Infections
- •6.2.8.1 Discussion
- •6.2.9.1 Discussion
- •6.2.10.1 Discussion
- •6.2.11.1 Discussion
- •6.2.12 Peritoneal Pseudocysts
- •6.2.12.1 Discussion
- •6.2.13.1 Discussion
- •6.2.14 Tumor Seeding
- •6.2.14.1 Discussion
- •6.2.15 Shunt Catheter Calcification
- •6.2.15.1 Discussion
- •6.2.16.1 Discussion
- •6.2.17.1 Discussion
- •Further Reading
- •Types of Procedures
- •External Ventricular Drainage
- •Ventriculoperitoneal Shunts
- •Atypical Ventricular Shunts
- •Ventriculosubgaleal Shunts
- •Subdural-Peritoneal Shunts
- •Lumboperitoneal Shunt
- •Third Ventriculostomy
- •Aqueductoplasty
- •Fourth Ventricular Stenting
- •Complications
- •Intraventricular Fat Migration
- •Slit Ventricle Syndrome
- •Shunt-Associated Infections
- •Shunt Malposition and Migration
- •Pseudocysts
- •Cerebrospinal Fluid Leak Syndrome
- •Tumor Seeding
- •Shunt Catheter Calcifications
- •7.1.1 Discussion
- •7.2.1 Discussion
- •7.3.1 Discussion
- •7.4.1 Discussion
- •7.5.1 Discussion
- •7.6.1 Discussion
- •7.7 Radiosurgery for Vestibular Schwannomas
- •7.7.1 Discussion
- •Further Reading
- •Anterior Craniofacial Resection
- •Transsphenoidal Resection
- •Middle Cranial Fossa Reconstruction
- •Surgical Approaches for Vestibular Schwannoma Resection
- •8.1.1 Discussion
- •8.2 Auriculectomy
- •8.2.1 Discussion
- •8.3 Auricular Reconstruction
- •8.3.1 Discussion
- •8.4.1 Discussion
- •8.5 Atresiaplasty
- •8.5.1 Discussion
- •8.6.1 Discussion
- •8.7.1 Discussion
- •8.8 Ossicular Interposition
- •8.8.1 Discussion
- •8.9.1 Discussion
- •8.10.1 Discussion
- •8.11.1 Discussion
- •8.12 Atticotomy
- •8.12.1 Discussion
- •8.13.1 Discussion
- •8.14.1 Discussion
- •8.15.1 Discussion
- •8.16 Temporal Bone Resection
- •8.16.1 Discussion
- •8.17 Cochlear Implants
- •8.17.1 Discussion
- •8.18.1 Discussion
- •8.19.1 Discussion
- •8.20.1 Discussion
- •8.21.1 Discussion
- •8.22 Labyrinthectomy
- •8.22.1 Discussion
- •8.23 Vestibular Nerve Section
- •8.23.1 Discussion
- •8.24.1 Discussion
- •8.25.1 Discussion
- •Further Reading
- •BAHA Device
- •Auriculectomy
- •Auricular Reconstruction
- •Canaloplasty and Meatoplasty
- •Atresiaplasty
- •Myringoplasty and Tympanoplasty
- •Incus Interposition
- •Ossicular Prosthesis Complications
- •Transcanal Atticotomy
- •Mastoidectomy Complications
- •Lateral Temporal Bone Resection
- •Cochlear Implants
- •Cochlear Implant Complications
- •Auditory Brainstem Stimulator
- •Repair of Perilymphatic Fistula
- •Labyrinthectomy
- •Vestibular Nerve Sectioning
- •Tube Drainage of Cholesterol Cysts
- •9.1 Vertical Ramus Osteotomy
- •9.1.1 Discussion
- •9.2 Sagittal Split Osteotomy
- •9.2.1 Discussion
- •9.3 Genioplasty
- •9.3.1 Discussion
- •9.4.1 Discussion
- •9.5 Mandibular Distraction
- •9.5.1 Discussion
- •9.6 LeFort I Osteotomy
- •9.6.1 Discussion
- •9.7 LeFort III Osteotomy
- •9.7.1 Discussion
- •9.8.1 Discussion
- •9.9 Mandibulotomy
- •9.9.1 Discussion
- •9.10 Enucleation
- •9.10.1 Discussion
- •9.11 Cyst Decompression
- •9.11.1 Discussion
- •9.12 Coronoidectomy
- •9.12.1 Discussion
- •9.13.1 Discussion
- •9.14.1 Discussion
- •9.15.1 Discussion
- •9.16.1 Discussion
- •9.17.1 Discussion
- •9.18.1 Discussion
- •9.19.1 Discussion
- •9.20.1 Discussion
- •Further Reading
- •Vertical Ramus Osteotomy
- •Sagittal Split Osteotomy
- •Genioplasty
- •Mandibular Angle Augmentation
- •Mandibular Distraction
- •Lefort I Surgery
- •Lefort III Surgery
- •Fixation of Mandible Fractures
- •Mandibulotomy
- •Enucleation
- •Cyst Decompression
- •Coronoidectomy
- •Eminectomy and Meniscal Plication
- •10: Imaging the Postoperative Neck
- •10.1 Reconstruction Flaps
- •10.1.1 Discussion
- •10.2 Neck Dissection
- •10.2.1 Discussion
- •10.3 Parotidectomy
- •10.3.1 Discussion
- •10.4.1 Discussion
- •10.5 Facial Reanimation
- •10.5.1 Discussion
- •10.6.1 Discussion
- •10.7.1 Discussion
- •10.8 Transoral Robotic Surgery
- •10.8.1 Discussion
- •10.9 Sistrunk Procedure
- •10.9.1 Discussion
- •10.10 Laryngectomy
- •10.10.1 Discussion
- •10.11.1 Discussion
- •10.12 Montgomery T-Tubes
- •10.12.1 Discussion
- •10.13 Salivary Bypass Stent
- •10.13.1 Discussion
- •10.14 Laryngeal Stents
- •10.14.1 Discussion
- •10.15.1 Discussion
- •10.16 Arytenoid Adduction
- •10.16.1 Discussion
- •10.17 Arytenoidectomy
- •10.17.1 Discussion
- •10.18 Laryngeal Cartilage Remodeling
- •10.18.1 Discussion
- •10.19 Tracheotomy
- •10.19.1 Discussion
- •10.20 Thyroidectomy
- •10.20.1 Discussion
- •10.21.1 Discussion
- •10.22 Brachytherapy
- •10.22.1 Discussion
- •10.23 Vagal Nerve Stimulation
- •10.23.1 Discussion
- •Further Reading
- •Reconstruction Flaps
- •Facial Reanimation
- •Tonsillectomy and Adenoidectomy
- •Transoral Robotic Surgery
- •Neck Dissection
- •Parotidectomy
- •Salivary Duct Stenting
- •Laryngectomy
- •Montgomery T-Tubes
- •Salivary Bypass Stents
- •Laryngeal Stents
- •Arytenoid Adduction
- •Arytenoidectomy
- •Laryngeal Cartilage Remodeling
- •Tracheotomy
- •Thyroidectomy
- •Neck Exploration and Parathyroidectomy
- •Sistrunk Procedure
- •Brachytherapy
- •Vagal Nerve Stimulation
- •11: Imaging of Postoperative Spine
- •11.1 Overview
- •11.2 Spine Decompression
- •11.2.1.1 Discussion
- •11.2.2 Laminectomy
- •11.2.2.1 Discussion
- •11.2.3 Facetectomy
- •11.2.3.1 Discussion
- •11.2.4 Microdiscectomy
- •11.2.4.1 Discussion
- •11.2.5 Laminoplasty
- •11.2.5.1 Discussion
- •11.2.6 Vertebrectomy
- •11.2.6.1 Discussion
- •11.2.7 Cordectomy
- •11.2.7.1 Discussion
- •11.3.1 Halo and Traction Devices
- •11.3.1.1 Discussion
- •11.3.2 Bone Graft Materials
- •11.3.2.1 Discussion
- •11.3.3 Implantable Bone Stimulators
- •11.3.3.1 Discussion
- •11.3.4 Odontoid Screw Fixation
- •11.3.4.1 Discussion
- •11.3.5 Occipitocervical Fusion
- •11.3.5.1 Discussion
- •11.3.6 Anterior Cervical Fusion
- •11.3.6.1 Discussion
- •11.3.7.1 Discussion
- •11.3.8 Posterior Fusion
- •11.3.8.1 Discussion
- •11.3.9 Scoliosis Rods
- •11.3.9.1 Discussion
- •11.3.10 Vertebral Stapling
- •11.3.10.1 Discussion
- •11.3.11 Vertical Expandable Prosthetic Titanium Rib (VEPTR)
- •11.3.11.1 Discussion
- •11.3.12 Interbody Fusion
- •11.3.12.1 Discussion
- •11.4.1 Total Disc Replacement
- •11.4.1.1 Discussion
- •11.4.2.1 Discussion
- •11.4.3.1 Discussion
- •11.4.4 Dynamic Facet Replacement
- •11.4.4.1 Discussion
- •11.4.5 Dynamic Rods
- •11.4.5.1 Discussion
- •11.5.1 Overview
- •11.5.2.1 Discussion
- •11.5.3.1 Discussion
- •11.5.4.1 Discussion
- •11.5.5 Cerebrospinal Fluid Leak
- •11.5.5.1 Discussion
- •11.5.6.1 Discussion
- •11.5.7 Surgical Site Infections
- •11.5.7.1 Discussion
- •11.5.8 Postoperative Neuritis
- •11.5.8.1 Discussion
- •11.5.9 Arachnoiditis
- •11.5.9.1 Discussion
- •11.5.10.1 Discussion
- •11.5.11 Postoperative Synovial Cyst
- •11.5.11.1 Discussion
- •11.5.12 Residual/Recurrent Tumors
- •11.5.12.1 Discussion
- •11.5.13 Inclusion Cysts
- •11.5.13.1 Discussion
- •11.5.14.1 Discussion
- •11.5.15 Retained Surgical Tools
- •11.5.15.1 Discussion
- •11.5.16 Gossypiboma
- •11.5.16.1 Discussion
- •11.5.17.1 Discussion
- •11.5.18 Postoperative Deformity
- •11.5.18.1 Discussion
- •11.6.1 Discussion
- •11.7 Spinal Cord Stimulators
- •11.7.1 Discussion
- •11.8 Filum Terminale Sectioning
- •11.8.1 Discussion
- •11.9.1 Vertebral Augmentation
- •11.9.1.1 Discussion
- •11.9.2 Kiva Device
- •11.9.2.1 Discussion
- •11.9.3 Sacroplasty
- •11.9.3.1 Discussion
- •11.9.4.1 Discussion
- •11.9.5.1 Discussion
- •11.9.6.1 Discussion
- •Further Reading
- •Overview
- •Laminectomy
- •Facetectomy
- •Microdiscectomy
- •Laminoplasty
- •Vertebrectomy
- •Cordectomy
- •Bone Graft Materials
- •Implantable Bone Stimulators
- •Odontoid Screw Fixation
- •Anterior Cervical Fusion
- •Posterior Fusion
- •Occiptiocervical Fusion
- •Scoliosis Rods
- •Vertebral Stapling
- •Interbody Fusion
- •Nucleus Pulposus Replacement
- •Dynamic Facet Replacement
- •Dynamic Rods
- •Cerebrospinal Fluid Leak
- •Seromas and Hematomas
- •Postoperative Infection
- •Postoperative Neuritis
- •Arachnoiditis
- •Postoperative Synovial Cyst
- •Residual/Recurrent Tumors
- •Inclusion Cysts
- •Retained Surgical Tools
- •Gossypiboma
- •Postoperative Deformity
- •Intrathecal Spinal Infusion Pump
- •Spinal Cord Stimulators
- •Filum Terminale Sectioning
- •Kiva Device
- •Sacroplasty
- •Percutaneous Spine Fusion
- •CT-Guided Epidural Blood Patch
- •12.1 Vascular Surgery
- •12.1.1.1 Discussion
- •12.1.2.1 Discussion
- •12.1.3.1 Discussion
- •12.1.4.1 Discussion
- •12.1.6.1 Discussion
- •12.1.7 Carotid Endarterectomy
- •12.1.7.1 Discussion
- •12.1.8 Carotid Body Stimulation
- •12.1.8.1 Discussion
- •12.1.9 Adjustable Vascular Clamp
- •12.1.9.1 Discussion
- •12.1.10.1 Discussion
- •12.2 Endovascular Surgery
- •12.2.7 Endovascular Reconstructive Treatment for Acute Ischemic Stroke Using Intra-arterial Thrombolysis or Embolectomy
- •12.2.10 Endovascular Stent Reconstructive Treatment for Extracranial Cerebrovascular Occlusive Disease
- •12.2.11 Endovascular Reconstructive Treatment for Active Extracranial Hemorrhage or Pseudoaneurysm
- •Further Reading
- •Vascular Surgery
- •Aneurysm and Hemostatic Ligation Clips
- •Intracranial Aneurysm Muscle Wrap
- •Vascular Malformation Surgery
- •Carotid Endarterectomy
- •Carotid Body Stimulation
- •Adjustable Vascular Clamp
- •Reconstruction of the Great Vessels
- •Endovascular Surgery
- •General Imaging Considerations Following Endovascular Cerebrovascular Procedures
- •Endovascular Treatment for Aneurysms
- •Endovascular Stent Reconstructive Treatment for Extracranial Cerebrovascular Occlusive Disease
- •Endovascular Reconstructive Treatment for Active Extracranial Hemorrhage or Pseudoaneurysm
- •Endovascular Treatment for Intracranial Venous Stenosis and Occlusion
- •Index
5 Imaging the Intraoperative and Postoperative Brain |
191 |
|
|
5.2.2\ Resection Cavities
5.2.2.1\ Discussion
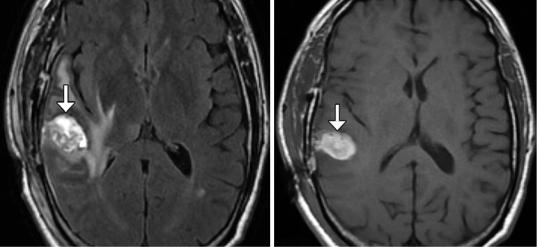
The space that remains after a tumor is surgically removed is known as the resection cavity. The resection cavity is often lined or packed with hemostatic agents (refer to Chap. 4) and contains variable amounts of cerebrospinal fluid and blood products, especially during the early postoperative period (Fig. 5.11). Oftentimes, resection cavities eventually shrink and collapse, becoming nearly imperceptible (Fig. 5.12), although some cavities stay the same size, particularly if they communicate with the ventricular system.
Variable amounts of tumor may remain adjacent to the cavity depending on whether gross total, near-total, or subtotal resection was performed. The extent of tumor resection depends
a
on several factors, including the location and type of tumor. Tumors that involve eloquent parts of the brain, that are in technically difficult areas to reach, or that involve critical structures, such as cranial nerves or major arteries, can limit the extent of tumor resection. Similarly, it is more difficult to achieve complete resection of infiltrative tumors than well-defined tumors. Ultimately, there is often a trade-off between removing as much tumor as possible versus preserving as much normal tissue and avoiding complications. Comparison with preoperative imaging should be performed when possible to help identify residual tumor.
Surgically induced parenchymal injury, postoperative hemorrhage, and enhancing conditions related to brain tumor surgery and adjunctive treatments are discussed in the following sections.
b
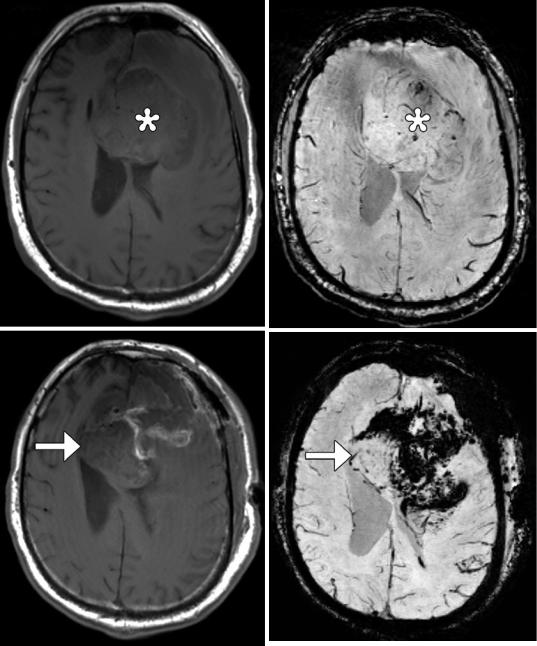
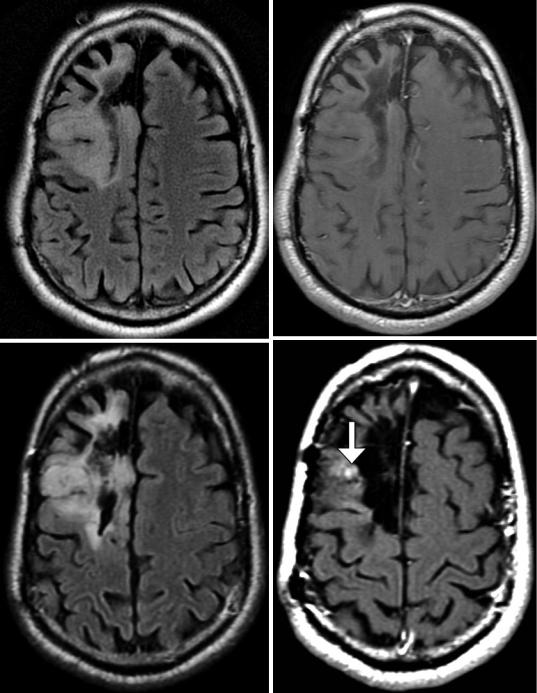
Fig. 5.11 Early surgical cavity with blood products. Axial FLAIR (a), T1-weighted (b), post-contrast T1-weighted (c), and GRE (d) MR images show subacute
blood products within a right temporal resection cavity (arrows). There is no significant mass effect or enhancement
192 |
D.T. Ginat et al. |
|
|
c |
d |
|
Fig. 5.11 (continued)
a
b
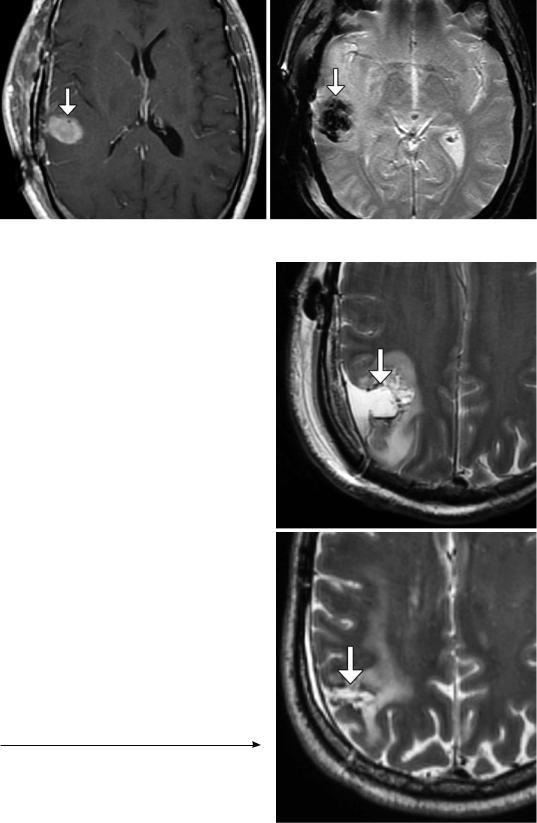
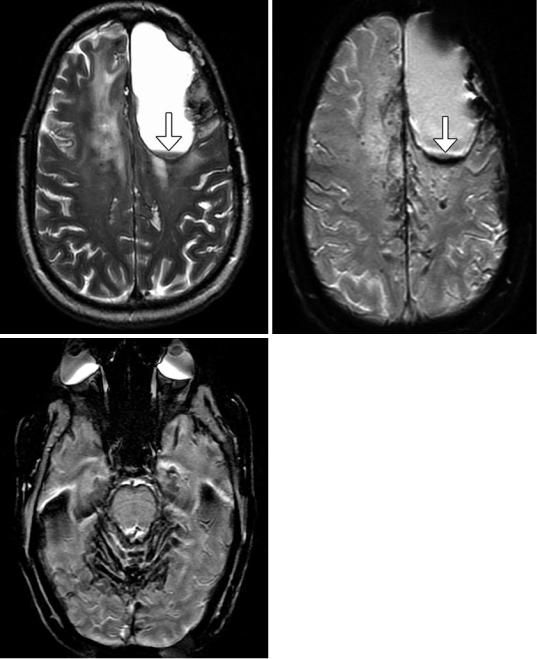
Fig. 5.12 Resection cavity evolution. Initial postoperative axial T2-weighted MRI (a) shows a fluid-filled resection cavity in the right parietal lobe (arrow). Axial T2-weighted MRI obtained 7 months later (b) shows nearcomplete collapse of the resection cavity (arrow)
5 Imaging the Intraoperative and Postoperative Brain |
193 |
|
|
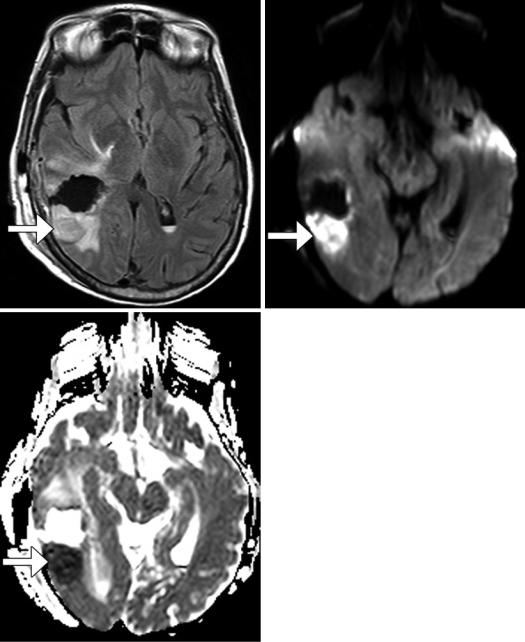
Surgically Induced Parenchymal Injury
Local areas of devitalized brain tissue surrounding the resection cavity are encountered on early postoperative MRI in up to 70% of cases of high- grade glioma resection as well as many other tumor resections. This phenomenon manifests as focal areas of restricted diffusion (Fig. 5.13). Enhancement of the devitalized tissue occurs in over 40% of cases between 1 week and several months. Furthermore, this phenomenon can lead to overestimation of residual non-enhancing tumor volume due to the presence of swelling and high signal on T2-weighted sequences during the early postoperative period. Visible encephalomalacia eventually forms around the surgical cavity in over 90% of cases of resection site infarcts. Larger, territorial infarcts are uncommon complications of tumor resection, but are predisposed by proximity to or encasement of major arterial branches and occasionally venous occlusion.
Vasogenic edema can result from forceful intraoperative retraction, which is sometimes performed in order to access large or deep tumors. The edema may be related to hyperemia of the brain surface after the release of retraction. On imaging obtained during the early postoperative period, retraction-induced vasogenic edema appears as swelling along the path of the retractors (Fig. 5.14). Unlike acute infarction, the vasogenic edema demonstrates elevated diffusivity rather than restricted diffusion.
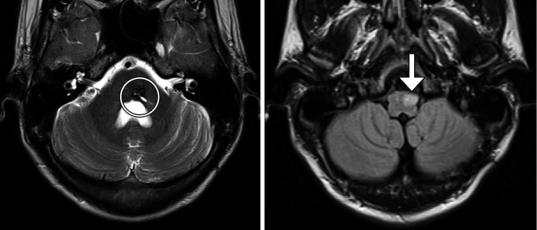
A peculiar complication related to posterior fossa tumor resections is hypertrophic olivary degeneration, which results from disruption of the dentato-rubro-olivary pathway (Guillain- Mollaret triangle). This phenomenon can occur after surgical resection of cerebellar tumors. If the resection site involves the central tegmental tract, the ipsilateral olivary nucleus is affected, while if the superior cerebellar peduncle is involved, the contralateral olivary nucleus is affected. Thus, bilateral hypertrophic olivary degeneration results from disruption of the central tegmental tract and superior cerebellar peduncle. Tongue fasciculations are characteristic of hypertrophic olivary degeneration. On MRI, hypertrophic olivary degeneration manifests as T2 hyperintensity with or without enlargement of the anterolateral medulla (Fig. 5.15). The differential diagnosis includes ischemia, demyelination, tumor spread, and infection. The lack of enhancement with hypertrophic olivary degeneration may help differentiate this entity from the other possibilities, such as some neoplasms. In addition, most cases demonstrate associated atrophy of the contralateral dentate nucleus or cerebellar cortex. Signal changes on MRI develop approximately 1 month after surgery and can persist for many years. Hypertrophy of the olivary nucleus tends to develop after several months and can resolve after 2–3 years.
194 |
D.T. Ginat et al. |
|
|
a |
b |
c
Fig. 5.13 Peri-resection infarction. The patient underwent recent resection of a right posterior temporal lobe glioblastoma. Axial FLAIR (a), DWI (b), and ADC (c)
maps show an area of restricted diffusion posterior to the resection cavity (arrows)

5 Imaging the Intraoperative and Postoperative Brain |
195 |
|
|
a |
b |
c
d
Fig. 5.14 Retraction-induced vasogenic edema. The patient has a history of fourth ventricular medulloblastoma. Preoperative axial FLAIR image (a) shows a large fourth ventricular mass, but no surrounding vasogenic edema. Postoperative FLAIR image (b) shows new areas
of hyperintensity in the bilateral medial cerebellar hemispheres. The diffusion-weighted image (c) and ADC map (d) show corresponding mildly elevated diffusivity (arrows). Small areas of ischemia are also present medially
196 |
D.T. Ginat et al. |
|
|
a |
b |
Fig. 5.15 Hypertrophic olivary degeneration. The patient presented with tongue fasciculations after resection of a right pontine cavernous malformation. Axial T2 MRI (a)
shows the resection site (encircled). Axial FLAIR MRI (b) shows high signal within an enlarged left olivary nucleus (arrow)
5 Imaging the Intraoperative and Postoperative Brain |
197 |
|
|
Postoperative Hemorrhagic Lesions
Hemorrhage is a relatively common occurrence with tumor resection and usually occurs at the craniotomy site. CT or MRI can readily depict these hemorrhages. The lack of contrast enhancement
and susceptibility effects help distinguish hematomas from residual tumor (Fig. 5.16). Hemorrhage that results from incomplete tumor resection is sometimes termed “wounded tumor syndrome” and is more commonly encountered with vascular tumors, such as melanoma, renal cell carcinoma, and glioblastoma (Fig. 5.17). Other risk factors for postoperative hemorrhage include inadequate hemostasis, underlying coagulopathies, and hypertension.
Chronic hemorrhage after surgery can result in superficial siderosis and mainly occurs when there is a cystic cavity that contains friable vessels or residual/recurrent tumor (Fig. 5.18). Hemosiderin deposits can coat remote leptomeningeal surfaces, particularly the cerebellum and brainstem. On CT, superficial siderosis can appear as a mildly hyperattenuating coating of these structures, which may also become atrophic as a result. MRI is more sensitive for depicting hemosiderin deposits, which appear as very low signal intensity on all sequences. Blooming artifact on T2* GRE or SWI sequences accentuates the lesions. The significance of superficial siderosis is that it may cause symptoms such as ataxia and deafness.

198 |
D.T. Ginat et al. |
|
|
a |
b |
c |
d |
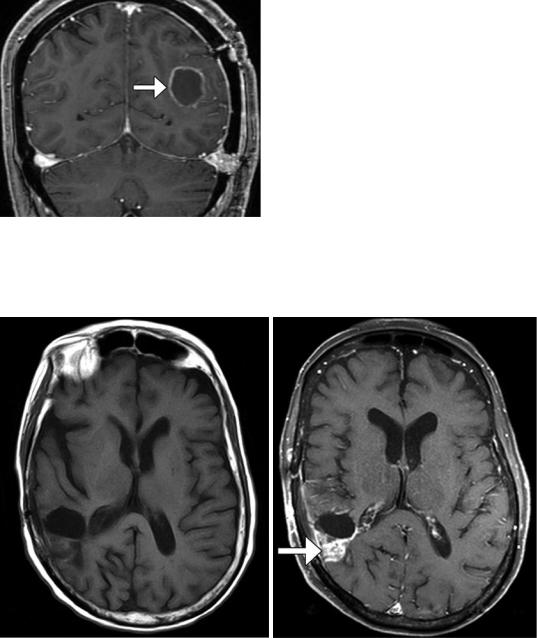
Fig. 5.16 Operative bed hemorrhage. The study was obtained to evaluate for residual tumor following recent meningioma resection. Copious oozing of blood was noted during surgery. Axial T1-weighted (a) and post- contrast T1-weighted (b), T2-weighted (c), and GRE (d)
images show an intrinsically T1 hyperintense and T2 hypointense extradural collection (*) with blooming and mass effect upon the underlying brain. There is also a small amount of hemorrhage within the surgical cavity associated with hemostatic material (arrows)
5 Imaging the Intraoperative and Postoperative Brain |
199 |
|
|
a |
b |
c |
d |
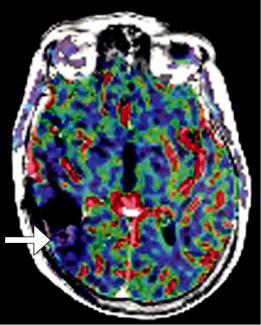
Fig. 5.17 Wounded tumor. The patient underwent subtotal resection of glioblastoma. Preoperative axial T1-weighted (a) and susceptibility-weighted imaging (b) show a large mass (*) in the left frontal lobe with only a few foci of microhemorrhage . Postoperative axial T1-weighted (c)
and susceptibility-weighted imaging (d) show interval appearance of high T1 signal hemorrhage and extensive susceptibility effect within and adjacent to the residual tumor (arrows)
200 |
D.T. Ginat et al. |
|
|
a |
b |
c
Fig. 5.18 Superficial siderosis. Axial T2-weighted MRI (a) and corresponding SWI (b) show a cystic left frontal lobe resection cavity with layering of blood products (arrows). In addition, there is blooming effect along the
margins of the cavity and along the cerebral sulci. SWI at a more inferior level (c) shows extensive susceptibility effect in a leptomeningeal distribution in the brainstem and cerebellum
5 Imaging the Intraoperative and Postoperative Brain |
201 |
|
|
Enhancing Lesions in the Surgical Bed Region and Beyond
Many types of enhancing lesions can be encountered on imaging after surgery, as listed in Table 5.1 and depicted in Figs. 5.19, 5.20, 5.21, 5.22, and 5.23. Indeed, several of these conditions can coexist and make interpretation of the imaging a challenge. Differentiation of these conditions from recurrent enhancing tumor is based on morphology as well as timing. Advanced imaging techniques,
such as perfusion MRI and MR spectroscopy, are often helpful for problem solving. Nevertheless, in some cases, biopsy or serial imaging can help elucidate ambiguous cases. It is also important to systematically evaluate the areas beyond the surgical bed on imaging exams, particularly with aggressive neoplasms, such as glioblastoma, which can undergo spread to remote parts of the brain, seed the scalp and face soft tissues, and undergo cerebrospinal fluid dissemination.
Table 5.1 Differential diagnosis of enhancing lesions on MRI after treatment for malignant glioma (Courtesy John W. Henson, MD and Jennifer Wulff, ARNP)
Condition |
Onset |
Other features |
Granulation tissue |
First postoperative week |
The enhancement is typically linear and smooth, but can |
|
(usually after 2 or 3 days), |
become more nodular by 1 week following surgery. Since |
|
intensifies over the ensuing |
residual enhancing tumor can be obscured or confounded by |
|
weeks, and resolves over |
granulation tissue, baseline imaging is recommended within |
|
3–5 months |
48 h of surgery, before granulation tissue forms. Serial imaging |
|
|
can also help to differentiate granulation tissue from residual |
|
|
tumor in that tumor increases in size over time, while |
|
|
granulation tissue should remain stable and eventually resolves |
Perioperative |
2 weeks after surgery |
Two-thirds of patients have focal infarcts around the resection |
ischemia |
|
cavity, and this can account for new post-op neurological |
|
|
deficits. Look for this on immediate post-op DWI. Can enhance |
|
|
after 10–14 days. Enhancement slowly resolves, leaving an area |
|
|
of encephalomalacia |
|
|
|
Postoperative |
1–3 weeks after surgery |
Clinical deterioration and new enhancement 1–3 weeks after |
infection |
|
surgery should raise a question of infection. Wound breakdown |
|
|
and drainage, markedly tender wound, fever, and elevated ESR |
|
|
can occur. Focal infection may show restricted diffusion |
|
|
|
Pseudoprogression |
Within 3 months following |
Inflammatory response to treatment. Often symptomatic. |
|
completion of concomitant |
Occurs within the RT port. Cannot be distinguished from true |
|
RT and TMZ |
progression by either routine MRI or advanced* MRI or |
|
|
FDG-PET. More likely in glioblastoma with methylated |
|
|
MGMT promoter. Wanes with time (scans are performed every |
|
|
month until change determines likely diagnosis). Good |
|
|
prognostic factor |
True progression |
Any time following |
Worsens with time. Routine MRI cannot distinguish from |
|
surgery |
pseudoprogression and radiation necrosis, but tumor tends to |
|
|
have elevated blood volume on perfusion MRI. More likely in |
|
|
tumors without methylation of the MGMT promoter. Poor |
|
|
prognostic factor |
|
|
|
Radiation necrosis |
Usually >1 year after |
Routine MRI cannot distinguish from progression; advanced |
|
radiation therapy |
MRI and FDG-PET can be very useful in distinguishing from |
|
|
progression. Can progress or wane over time. SMART |
|
|
(stroke-like migraines after radiation therapy) syndrome is an |
|
|
unusual, late complication of localized radiation therapy for |
|
|
brain tumors, in which patients present with headache and |
|
|
neurological deficits between about 2 and 10 years after |
|
|
treatment, usually greater than 50 Gy of radiation. Treated with |
|
|
observation, steroids, bevacizumab, or surgery |
|
|
|
202 |
D.T. Ginat et al. |
|
|
Fig. 5.19 Granulation tissue. The patient is status post meningioma resection 5 days prior to imaging. Coronal post-contrast T1-weighted MRI shows a thin circumferential rim of enhancement along the resection margin (arrow)
a |
b |
Fig. 5.20 Perioperative infarct. Pre- (a) and post-contrast (b) T1-weighted MR images obtained 1 month after surgery in the same case as in Fig. 5.13 show that the infarcted
tissues enhance (arrow). Furthermore, the CBV map (c) shows corresponding hypoperfusion in the area (arrow)
5 Imaging the Intraoperative and Postoperative Brain |
203 |
|
|
c
Fig. 5.20 (continued)
204 |
D.T. Ginat et al. |
|
|
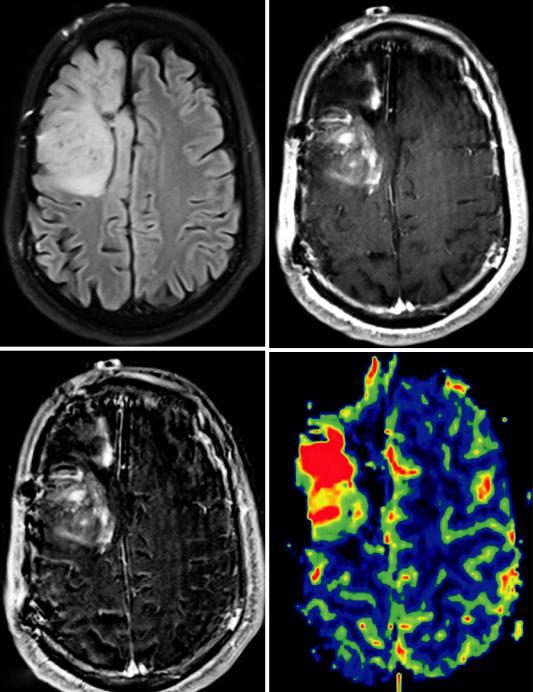
a |
b |
c |
d |
Fig. 5.21 Tumor progression. The patient underwent gross total resection of an oligoastrocytoma (WHO grade II/IV) in the right frontal lobe. Axial FLAIR (a) and post- contrast T1-weighted (b) MR images obtained approximately 10 years after resection show a right frontal resection cavity surrounded by non-enhancing FLAIR signal abnormality. Axial FLAIR (c) and post-contrast T1-weighted (d) MR images obtained approximately
1 year later show a new focus of enhancement adjacent to the resection cavity (arrow), but no obvious change in the FLAIR signal abnormality. Axial FLAIR (e), post-con- trast T1-weighted (f), subtraction image (g), and CBV map (h) obtained approximately 6 months later demonstrate marked interval increase in volume of the FLAIR signal abnormality and enhancing adjacent to the resection cavity and associated elevated CBC (arrows)
5 Imaging the Intraoperative and Postoperative Brain |
205 |
|
|
e |
f |
g |
h |
Fig. 5.21 (continued)
206 |
D.T. Ginat et al. |
|
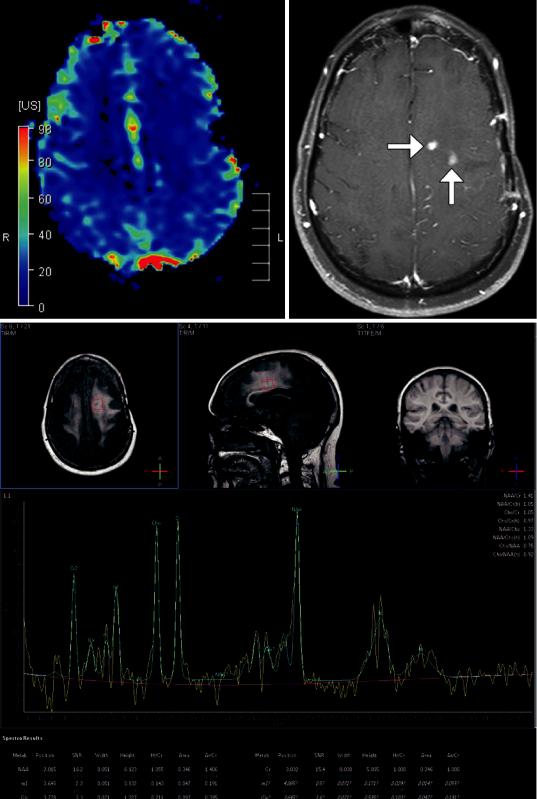
|
a |
c |
b

5 Imaging the Intraoperative and Postoperative Brain |
207 |
|
|
a |
b |
Fig. 5.23 Metastatic glioblastoma in the spinal canal. The patient presented with back and low extremity pain after gross total resection of a left frontal glioblastoma resection with recurrence. Sagittal post-contrast T1-weighted MRI (a) shows irregular enhancement
involving the bilateral frontal lobes, extending to the meningeal surface. Sagittal post-contrast T1-weighted MRI (b) shows an intradural, extramedullary mass with irregular enhancement in the upper lumbar spinal canal (arrow)
Fig. 5.22 Radiation necrosis. The patient has a history of left frontal lobe glioblastoma that was resected and radiated approximately 1 year before. Axial (a) post- contrast T1-weighted MRI shows small areas of enhancement in the treatment bed region (arrows). There is no
corresponding hypermetabolism on the blood volume map (b). MRI spectroscopy (c) over the abnormality shows a lactate peak, mildly reduced NAA peak, and a Cho peak that is not particularly elevated with respect to Cr
