
Биоинженерия / Биомеханика_микрофлюидные_устройства / статьи / 15342.full
.pdf
Downloaded by guest on November 18, 2019
Fluid forces control endothelial sprouting
Jonathan W. Song and Lance L. Munn1
Edwin L. Steele Laboratory for Tumor Biology, Department of Radiation Oncology, Massachusetts General Hospital and Harvard Medical School, Charlestown, MA 02129
Edited* by Shu Chien, University of California at San Diego, La Jolla, CA, and approved August 1, 2011 (received for review April 5, 2011)
During angiogenesis, endothelial cells (ECs) from intact blood vessels quickly infiltrate avascular regions via vascular sprouting. This process is fundamental to many normal and pathological processes such as wound healing and tumor growth, but its initiation and control are poorly understood. Vascular endothelial cell growth factor (VEGF) can promote vessel dilation and angiogenic sprouting, but given the complex nature of vascular morphogenesis, additional signals are likely necessary to determine, for example, which vessel segments sprout, which dilate, and which remain quiescent. Fluid forces exerted by blood and plasma are prime candidates that might codirect these processes, but it is not known whether VEGF cooperates with mechanical fluid forces to mediate angiogenesis. Using a microfluidic tissue analog of angiogenic sprouting, we found that fluid shear stress, such as exerted by flowing blood, attenuates EC sprouting in a nitric oxide-dependent manner and that interstitial flow, such as produced by extravasating plasma, directs endothelial morphogenesis and sprout formation. Furthermore, positive VEGF gradients initiated sprouting but negative gradients inhibited sprouting, promoting instead sheet-like migration analogous to vessel dilation. These results suggest that ECs integrate signals from fluid forces and local VEGF gradients to achieve such varied goals as vessel dilation and sprouting.
3D angiogenesis on a chip | collagen gel | structural remodeling | alternative to animal model | vessel analog
Angiogenesis, the expansion or extension of existing vasculature, is necessary to deliver oxygen and nutrients to ischemic or avascular regions in wounds and solid tumors (1), and a funda-
mental understanding of the determinants of angiogenesis would accelerate progress in the fields of regenerative medicine, tissue engineering, and oncology. Angiogenesis requires the coordinated growth and migration of endothelial cells (ECs): each EC residing in a vessel wall integrates local signals to determine whether it remains quiescent (2, 3), participates in dilation or contraction (1), undergoes morphogenesis to form an angiogenic sprout (4, 5), or intussusceptive involution (6). Implicit in these processes are endothelial proliferation during expansion of the vasculature and their loss during vessel contraction and pruning (7).
Growth factors have pleiotropic effects on ECs and are undoubtedly key controllers of vascular morphogenesis. The best studied vascular morphogen, vascular endothelial growth factor (VEGF) (8), stimulates EC migration (9), proliferation (10), and matrix degradation (2). VEGF also controls vessel morphogenesis by inducing Delta-like ligand 4 (Dll4)—a membrane-bound ligand for the Notch family of receptors—at the advancing front of sprouts (11), thereby promoting the formation of specialized “tip cells,” which extend protrusions or filopodia that sense growth factor concentrations to guide sprouts (4, 5). However, given the distinct phenotypes exhibited by ECs during sprouting, dilation, contraction, and quiescence—even within the same vessel segment—there are undoubtedly codeterminants that direct EC behavior.
ECs in patent blood vessels are exposed to mechanical forces tangential to the endothelial surface due to blood flow (12–15) and across the vessel wall due to interstitial plasma flow (16, 17). Fluid shear stress imposes signals that mediate EC transcription (18), membrane fluidity (19), VEGF receptor conformational changes (20), tubule formation (21, 22), intraluminal morphol-
ogy (23), barrier function (24), and vessel homeostasis, by maintaining vessel lumens (25, 26) and controlling EC proliferation (27) and turnover (1). In addition, shear stress can induce significant changes in EC morphology (28) and actin cytoskeleton rearrangement (29), whereas flow transverse to the endothelium (16) and/or through the interstitial space (30) can also cause endothelial morphogenesis.
Although there is a wealth of evidence that fluid forces affect endothelial phenotype, no study has simultaneously examined the interplay of tangential shear stress, transverse interstitial flow, and VEGF gradients in mediating sprouting morphogenesis from an intact vessel. Using a microfluidic model of angiogenic sprouting, we found that fluid shear stress inhibits vessel morphogenesis (rearrangement of the vessel wall microanatomy resulting in sprouting or invasion into the matrix) via the nitric oxide (NO) pathway, and interstitial flow increases the rate of morphogenesis. Surprisingly, invading ECs not only detected the direction of VEGF gradients but also showed dramatic differences in morphogenesis, depending on the direction of interstitial fluid flow. Endothelial tip cell filopodia preferentially protruded against the direction of interstitial flow or in the direction of an increasing VEGF gradient. In contrast, a decreasing VEGF gradient promoted migration of an endothelial “sheet” in a process analogous to vessel dilation. These results emphasize the importance of multiple signals during angiogenesis and suggest that fluid forces are important mediators of vascular homeostasis and morphogenesis.
Results
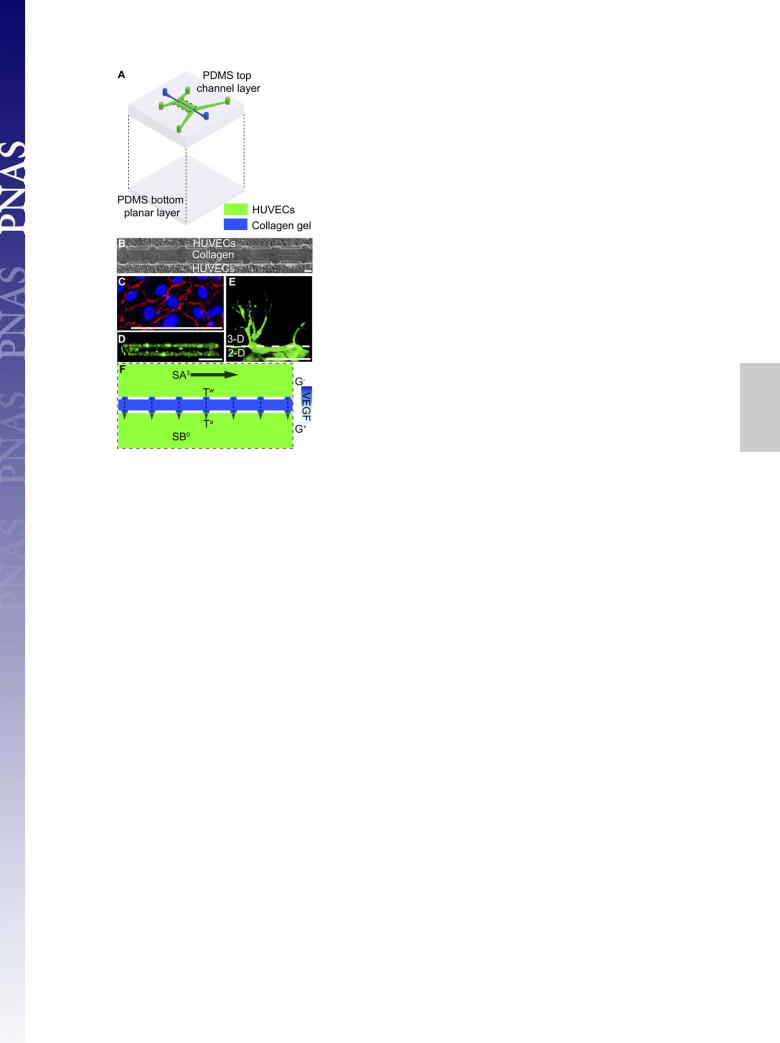
Angiogenic Sprouting in Vitro. To determine how fluid and chemical factors cooperate—or antagonize—to modulate sprouting from realistic vessel analogs in vitro, we developed a microfluidic platform that features (i) fluid flowing through two adjacent, endothelial lined channels, (ii) contact between the vessel wall and a 3D collagen matrix on the abluminal side to allow endothelial sprouting, (iii) controllable fluid convection through the matrix, and (iv) specifiable growth factor gradients (Fig. 1). Two parallel channels (50 μm in height) spaced 300 μm apart and lined with confluent human umbilical vein endothelial cells (HUVECs) traverse the device (Fig. 1 B–D). Along the device, there are seven apertures of 3D collagen I gel matrix (100 μm in width) that allow contact between the vessel walls and the intervessel matrix (Fig. 1B). HUVEC-GFP cells that were stimulated with 50 ng mL−1 VEGF for 3 d migrate into the bulk of the 3D extracellular matrix (ECM) space rather than along the top or bottom surface, adopting morphology distinct from the cells that remain as a 2D monolayer in the main vessel (Fig. 1E). To more easily distinguish the various parameter sets for each experiment, we adopted the naming conventions in Table 1.
Author contributions: J.W.S. and L.L.M. designed research; J.W.S. performed research; J.W.S. and L.L.M. analyzed data; and J.W.S. and L.L.M. wrote the paper.
The authors declare no conflict of interest.
*This Direct Submission article had a prearranged editor.
Freely available online through the PNAS open access option.
1To whom correspondence should be addressed. E-mail: munn@steele.mgh.harvard.edu.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10. 1073/pnas.1105316108/-/DCSupplemental.
15342e15347 | PNAS | September 13, 2011 | vol. 108 | no. 37 |
www.pnas.org/cgi/doi/10.1073/pnas.1105316108 |
Downloaded by guest on November 18, 2019
Fig. 1. Microfluidic device with localized 3D ECM for fluid force-mediated angiogenic sprouting and morphogenesis. (A) Multilayer fabrication of the poly(dimethylsiloxane) PDMS microfluidic device featuring localized region of collagen gel (blue). The top PDMS layer contains the channel features (50 μm in height) and the bottom layer provides a planar surface. (B) HUVECs seeded into two channels separated by multiple collagen gel apertures visualized under phase microscopy. (C) Immunofluorescence staining for VEcadherin expression (red) demonstrates integrity at intercellular junctions of the HUVEC monolayer. Blue depicts nuclei stained with DAPI. (D) Cross-sec- tion view of one of the HUVEC channels. HUVEC-GFP cells seeded on top, bottom, and Side faces mimicking a fully-lined blood vessel. (E) HUVEC-GFP cells sprouting into 3D collagen gel demonstrate clear morphological differences, with HUVECs invading the bulk of the gel rather than along the top or bottom surface. (F) Close-up view of boxed area in A showing seven apertures that allow connection of the two HUVEC channels (green) through the collagen barrier (blue). Each HUVEC channel has independent input and outlet ports, allowing strict control over flow in both channels (SA and SB) and across the collagen matrix (T). As drawn, the nomenclature for this flow configuration is SA3TwG−jSB0TaG+. (Scale bars, 100 μm.)
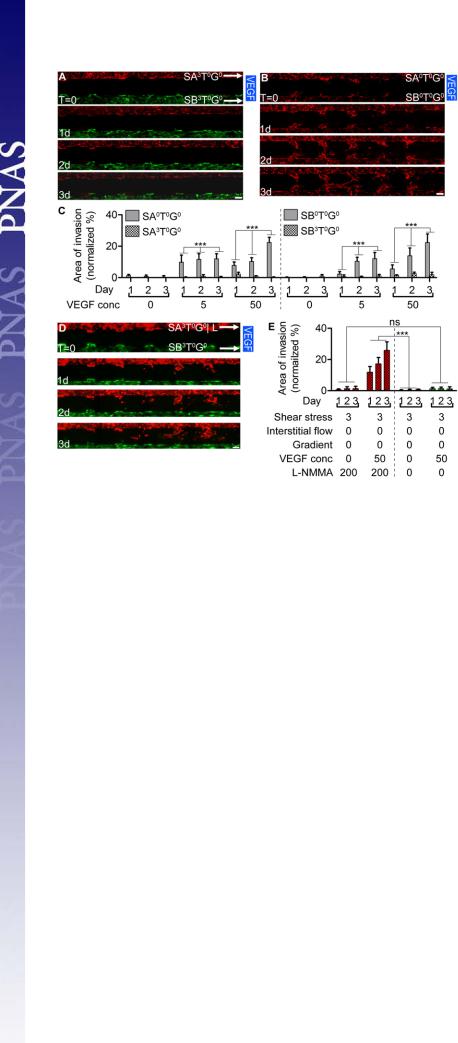
Shear Stress Attenuates VEGF-Induced Morphogenesis. Endothelial morphogenesis and invasion into the gel were prominent from both channels under static conditions (SA0T0G0jSB0T0G0), but minimal when the cells were exposed to shear stress (SA3T0G0jSB3T0G0) at
Table 1. Notation for flow and VEGF conditions
either VEGF concentration (V5 or V50; Fig. 2). With no added VEGF, there was little sprouting under static conditions (SA0T0G0jSB0T0G0jV0; Fig. 2C). Thus, physiological shear stress (3 dyn cm−2; Fig. S1) attenuates VEGF-driven morphogenesis. The attenuation of invasive morphogenesis by shear stress was accompanied by a decrease in EC proliferation (Fig S1C). Inhibition of invasion by shear was not due to proangiogenic factors being washed away in the flow, as shear inhibition was also seen with conditioned medium (Fig. S2).
To determine whether VEGF gradients (Fig. S3) drive the invasive morphogenesis, we applied identical flow conditions
to both channels but only added VEGF to channel A (SA0.1T0G−jSB0.1T0G+jV50 or SA3T0G−jSB3T0G+jV50). The slow flow in the SA0.1T0G−jSB0.1T0G+jV50 condition applied
minimal shear stress (w0.1 dyn cm−2), but was sufficient to replenish nutrients and maintain a stable biochemical gradient (Fig. S3 D–F). Morphogenesis and gel invasion occurred in the
slow-flow configuration from both channels, but required VEGF (SA0.1T0G−jSB0.1T0G+jV50; Fig. S4). Again, little invasion oc-
curred at physiological shear stress levels, even with a VEGF gradient (SA3T0G−jSB3T0G+jV50; Fig. S4 C and D).
Attenuation of Morphogenesis by Shear Stress Requires Nitric Oxide Production. To further investigate the attenuation of HUVEC sprouting by shear stress, we next blocked production of nitric oxide (NO), an important shear stress-responsive signaling molecule (31, 32). We infused VEGF-containing medium (50 ng mL−1) into both HUVEC channels at physiological shear stress levels (3 dyn cm−2), but added the pan nitric oxide synthase (NOS) inhibitor NG-monomethyl-L-arginine monoacetate (L-NMMA) (33) (200
μM) into channel A to block NO signaling (32). As expected, with shear flow in both channels (SA3T0G0jSB3T0G0jV50), minimal
sprouting was observed in the channel exposed to VEGF without L-NMMA (Fig. 2E). However, sheared cells exposed to VEGF with L-NMMA sprouted into the collagen gel (SA3T0G0jL; Fig. 2 D and E) at a rate similar to that seen in static channels (Fig. 2C). This effect was not due to direct activity of L-NMMA: when L-NMMA was added to standard media with no VEGF, little sprouting was observed (Fig. 2E), and L-NMMA combined with
VEGF did not enhance sprouting in static cultures, compared with VEGF alone (SA0T0G0jSB0T0G0jV50; Fig. S5). These results show
that the attenuation of VEGF-induced sprouting caused by shear stress requires NO signaling.
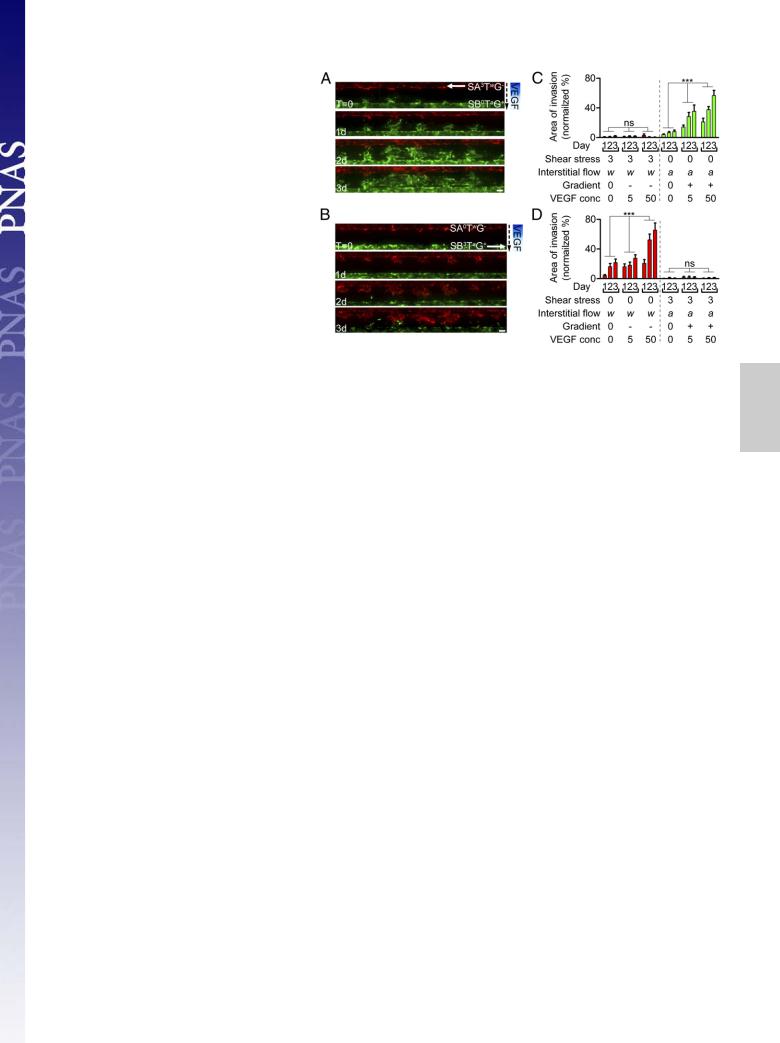
Direction of VEGF Gradient with Interstitial Flow Affects Sprout Morphology. We next evaluated the effect of simultaneous application of physiological levels of shear stress (3 dyn cm−2) and interstitial flow (2.5–35 μm s−1; Fig. S6) (16, 30) on sprouting morphogenesis. Either pushing VEGF-containing medium into channel A (SA3TwG−jSB0TaG+) or pulling non–VEGF-containing medium into channel B (SA0TwG−jSB3TaG+) creates interstitial flow (Fig. S6) and a VEGF gradient (Figs. S7 and S8) from A to B.
Notation |
Definition |
Superscripts |
|
|
|
SA, SB |
Shear stress in channel A (Upper channel) |
0 indicates approximately no flow in the channel; 0.1 indicates w0.1 dyn cm−2; |
|
or channel B (Lower channel), |
and 3 is w3 dyn cm−2. For example, SA3 and SB0 indicate that channel A |
|
respectively (Fig. 1) |
was exposed to 3 dyn cm−2, whereas channel B was static. |
T |
Transverse convection or interstitial flow |
0 indicates no convection; a indicates convection against the direction |
|
(2.5–35 mm s−1; Fig. S7) |
of endothelial invasion; and w means convection with the |
|
|
direction of endothelial invasion. |
G |
VEGF gradient |
0 indicates no VEGF gradient; + indicates invasion toward the |
|
|
VEGF source or a positive gradient; and − indicates invasion |
|
|
away from the VEGF source or a negative gradient. |
V |
The concentration of exogenously added VEGF |
0 indicates no VEGF; 5 indicates 5 ng ml−1; and 50 indicates 50 ng ml−1. |
Song and Munn |
PNAS | September 13, 2011 | vol. 108 | no. 37 | 15343 |
|
MEDICAL SCIENCES
Downloaded by guest on November 18, 2019
As before (Fig. 2A), cells in the sheared channels, which were also continually stimulated with VEGF-containing media, exhibited very little invasion (Fig. 3). In contrast, HUVECs in the nonsheared channels invaded into the collagen gel (Movie S1), and the area of invasion increased with VEGF concentration (V0, V5, and V50; Fig. 3, P < 0.0001). However, HUVECs in the two configurations invaded the gel in opposite sense relative to the direction of the VEGF gradient and interstitial flow and exhibited striking differences in sprout morphology (Fig. 4 A and B). Where HUVECs invaded toward the VEGF source (positive VEGF gradient) and against the direction of interstitial flow (SB0TaG+jV50), the number of filopodia or tip cell projections (5, 34) was significantly greater than in the configuration where HUVECs invaded away from the VEGF source (negative VEGF gradient) and with the direction of interstitial flow (SA0TwG−jV50; Fig. 4 A, B, and E, gray vs. orange bar). The prominent filopodia projected by cells moving toward the VEGF source and against flow (SB0TaG+jV50 configuration) were characteristic of sprouting from a preexisting vessel. On the other hand, HUVECs moving down the gradient, with the flow (SA0TwG−jV50 configuration) maintained a relatively smooth boundary as they moved into the gel. This process more closely resembled vessel dilation than sprouting.
Interstitial Flow Enhances Sprouting Morphogenesis. To test whether interstitial flow affects HUVEC invasion and sprout morphology independent of a VEGF gradient, we connected both ports of channel B to the pump and pulled media (28.5 μm s−1) through the intervessel matrix from reservoirs connected to channel A, while exposing both channels to negligible levels of tangential shear (SA0TwG0jSB0TaG0). This configuration also eliminated VEGF gradients (Figs. S8 and S9 A–C). Morphogenic invasion occurred both with and against the direction of flow to the same extent (SA0TwG0jSB0TaG0jV50 condition; Fig. S9 D and E; P > 0.1). Fig. 4 D and E consolidate and compare the data
Fig. 2. Shear stress attenuates VEGF-induced HUVEC invasion. (A) To examine the role of shear stress, identical flow (3 dyn cm−2) and VEGF conditions (50 ng mL−1)
were applied to the Upper and Lower channels (SA3T0G0jSB3T0G0jV50), resulting in no interstitial flow or
VEGF gradient across the collagen gel (see Table 1 for explanation of nomenclature). Invasion was minimal from both channels. (B) Without flow, application of 50 ng mL−1 VEGF-containing media in both HUVEC channels under static conditions results in dramatic invasion (SA0T0G0jSB0T0G0jV50 configuration). Solid blue VEGF bar indicates uniform VEGF concentration in the collagen gel.
(C) Normalized area of invasion in the 3D collagen gel from sheared (SA3T0G0jSB3T0G0) and static (SA0T0G0jSB0T0G0)
channels with various VEGF concentrations. (D) In the SA3T0G0jSB3T0G0jV50 flow configuration, the pan-NOS in-
hibitor L-NMMA was added to the medium in the Upper channel (SA3T0G0jL) resulting in significant invasion. (E) Normalized area of invasion in the 3D collagen gel for the flow configuration in D. Under shear flow, HUVEC invasion requires both VEGF stimulation and NO inhibition by L- NMMA. Duration of all experiments was 3 d. Data points on the graphs represent mean values and error bars depict SEM. Sample populations were compared using two-way ANOVA (row factor was day of treatment; column factor
was treatment condition). Statistical outcome indicated for treatment condition (e.g., SA0T0G0jV50 vs. SA3T0G0jV50). n =
21–28 per condition per day. ***P < 0.0001; ns, P = 0.33. Images represent a mosaic of 4 separate 10× fields acquired along the length of the device, spliced together automatically using the Photomerge command in Adobe Photoshop (SI Materials and Methods, Image Acquisition and Processing). (Scale bars, 100 μm.)
with interstitial flow, without and with VEGF gradients (produced with the previous flow configurations). Interstitial flow alone significantly increased the area of invasion by w75% for both directions (Fig. 4D). Furthermore, the presence of a VEGF gradient (both positive and negative) enhanced interstitial flowguided invasion in an additive manner for both directions (Fig. 4D). However, in the absence of a VEGF gradient, sprouts moving against the direction of interstitial flow still had more filopodia than those moving with the flow (Fig. 4E, yellow vs. purple bar). Considering only the sprouts moving against the interstitial flow from channel B, the presence of the positive VEGF gradient did not result in more filopodia, compared with the uniform VEGF condition (Fig. 4E, purple vs. gray bar). For invading cells moving with the direction of flow from channel A, the negative VEGF gradient inhibited filopodia formation (Fig. 4E, orange vs. yellow bar). These results show that interstitial flow and VEGF both enhance morphogenic invasion, and sprouts moving against the direction of interstitial flow or up a VEGF gradient extend more filopodia.
Discussion
The primary role of the vasculature is to deliver blood efficiently. Therefore, it is not surprising that forces exerted by blood and plasma would provide feedback control for formation of that vasculature. It has long been known that blood flow mediates remodeling of immature embryonic networks (35, 36) and helps control vascular tone and collateral formation in muscle tissue (37, 38). However, the role of fluid forces in the initiation of angiogenesis is not well understood, mainly due to a lack of appropriate tools for controlling the relevant parameters. Common approaches either lack intraluminal flow (e.g., the “tube formation” and microbead sprouting assays) or by virtue of plating cells on a solid substrate, prohibit the EC reorganization necessary for vessel dilation or sprouting (e.g., parallel plate flow chambers and poly(dimethylsiloxane), PDMS channels). In vivo analyses,
15344 | www.pnas.org/cgi/doi/10.1073/pnas.1105316108 |
Song and Munn |
Downloaded by guest on November 18, 2019
Fig. 3. Shear stress attenuates HUVEC invasion irrespective
of the direction of interstitial flow and VEGF gradient. (A) In the flow configuration SA3TaG+jSB0TwG−jV50, positive pres-
sure shear flow (3 dyn cm−2) in channel A (Upper) results in interstitial flow of 50 ng mL−1 VEGF-containing medium at a rate of 2.5 μm s−1 and a VEGF gradient from channel
A to channel B (Lower). (B) In the flow configuration SA0TwG−jSB3TaG+jV50, negative pressure shear flow (3 dyn
cm−2) in channel B results in interstitial flow at a rate of 35 μm s-1 and a VEGF gradient from A to B. Solid arrows indicate direction of axial flow in the HUVEC channels; dashed arrows indicate direction of interstitial flow. Blue gradient bar indicates VEGF gradient from A to B in the collagen gel. Images represent a mosaic of four separate 10× fields acquired along the length of the device, spliced together automatically using the Photomerge command in Adobe Photoshop (SI Materials and Methods, Image Acquisition and Processing). (Scale bars, 100 μm.) (C) Normalized area of in-
vasion in the 3D collagen gel for the SA3TaG0jSB0TwG0jV0, SA3TaG+jSB0TwG−jV5, and SA3TaG+jSB0TwG−jV50 flow config-
urations. (D) Normalized area of invasion in 3D collagen space for the SA0TwG0jSB3TaG0jV0, SA0TwG−jSB3TaG+jV5, and
SA0TwG−jSB3TaG+jV50 flow configurations. HUVEC invasion
occurs mainly from the nonsheared channels and irrespective of the direction of interstitial flow and VEGF gradients in channels A and B. Duration of all experiments was 3 d. Data points represent mean + SEM. Statistical outcome indicated for treatment condition (V0 vs. V5 vs. V50). n = 21–35 per day per condition.
***P < 0.0001; ns, P > 0.44.
on the other hand, face the currently insurmountable challenge of quantifying or controlling all of the various growth factors and mechanical forces in the microenvironment of a sprouting vessel segment. Improvements to existing models of vessel development or repair are needed to understand why certain ECs sprout, whereas others are quiescent or are involved in vessel dilation or extension.
By controlled application of VEGF and fluid forces in a microfluidic device that accurately mimics angiogenic sprouting, we found that VEGF gradients and fluid forces cooperate to control endothelial sprouting and morphogenesis. A major finding is that physiological shear stress attenuates VEGF-in- duced sprouting through NO signaling (Fig. 2 C and E). This finding is consistent with the inhibition of EC proliferation by steady laminar shear stress in vitro (27, 39, 40). In vivo, this shear-controlled mechanism would tend to stabilize mature vessels to ensure that sprouting is initiated from vessels with low or no flow, such as damaged or occluded vessels (41), or blindending sprouts (42). The fact that tumor blood vessels have highly abnormal flow patterns (7, 43, 44), characterized by an abundance of segments with stagnant or slow flow, suggests that shear-mediated sprout inhibition may be lacking in many vessels, thereby contributing to tumor angiogenesis. Although eNOS and NO have been implicated in tumor vessel remodeling (33), the link between shear stress and morphogenesis has not been established in tumor vessels. However, there is evidence that eNOS expression is sensitive to temporal or spatial gradients of shear stress profiles in vitro (29, 45). In tissues where angiogenesis is occurring, we would expect temporal changes in shear stress—as vessels dilate, become leaky, or are occluded—and spatial gradients, which would be prominent at new branch points or those leading to occluded segments. It remains to be seen whether shear stress magnitude or spatial gradients of shear stress are more important in determining EC behavior. Further characterization of the stress-sensing mechanisms may provide new targets for controlling sprouting angiogenesis in tumors.
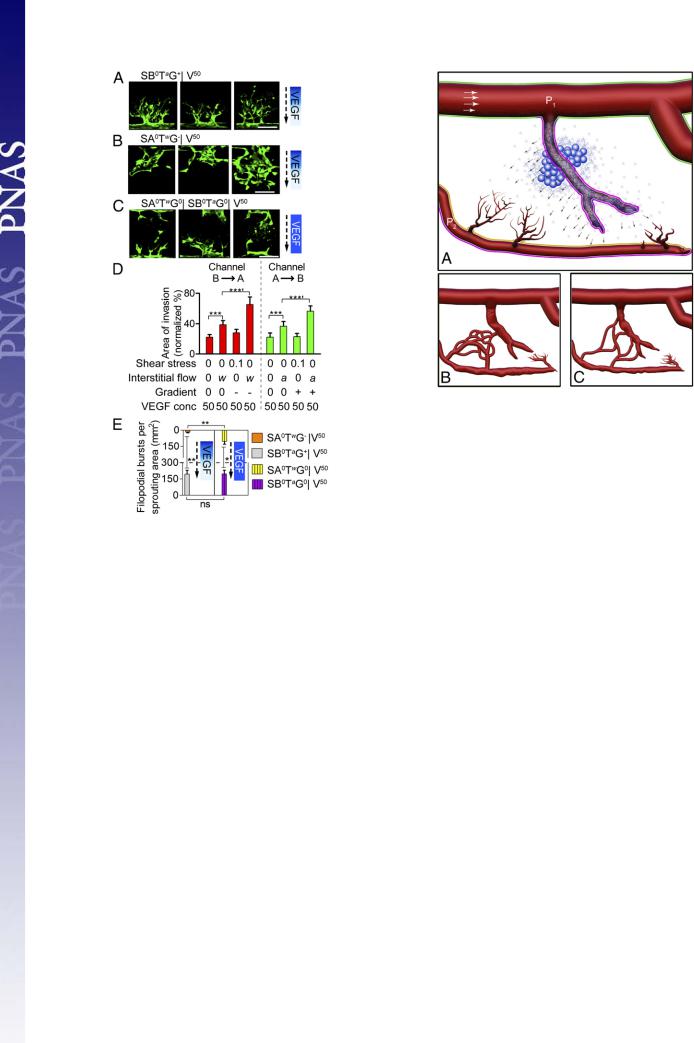
We also demonstrated that VEGF can cause either vessel dilation or sprouting, depending on the nature of its local gradient (Fig. S10). Negative VEGF gradients resulted in a process resembling vessel dilation in our device (although restricted to the regions of the apertures), whereas positive VEGF gradients induced filopodial extensions analogous to tip cell sprouts seen
in vivo (4, 5) (Fig. 4 A and B). This suggests that individual ECs around the vessel circumference can sense their orientation relative to the VEGF source to determine whether they should initiate sprouting or simply participate in vessel dilation to increase overall flow to the tissue.
Even more interesting is the finding that interstitial flow encourages morphogenesis and filopod formation. Interstitial flow alone enhances the rate of EC invasion irrespective of the direction of flow or VEGF gradient (Fig. 4D). The mechanism of the mechanotransduction is not clear, but previous studies have suggested that transverse flow can act on mechanosensors located at cell–cell junctions of endothelial monolayers (46). Other studies have shown that shear stress applied to cells scattered in a 3D matrix can promote morphogenesis by activating membranebound sensors in either ECs (30) or vascular smooth muscle cells (SMCs) (47). The fact that more filopodia were produced by cells moving against the direction of interstitial flow in our study—even in the absence of a VEGF gradient (Fig. 4D)—suggests that filopodia originating from tip cells at the leading edge of sprouts may also be involved in probing the local flow environment. We speculate that, whereas VEGF guides sprouts toward hypoxic regions (1, 5, 9), interstitial flow directs them to other vessels, against the direction of interstitial flow, and consequently, toward vessels that have higher microvascular pressure than their own. The difference in hydrostatic pressure, which drives interstitial flow between the vessels, would also ensure effective perfusion upon connection of those two vessels.
An example of how the various findings in our study would apply during tissue revascularization is depicted in Fig. 5. In ischemic, hypoxic tissue, some stagnant vessels are embedded in the source of VEGF; ECs in these vessels can see a negative VEGF gradient across the vessel wall and initiate dilation. Another vessel farther away (Lower) sees a positive VEGF gradient on one side, but a negative gradient on the other. ECs in this segment sprout or dilate, respectively. Other ECs, far enough away from the VEGF source or with sufficient flow, resist structural changes (Upper). By following both VEGF and interstitial flow cues, the extending sprouts infiltrate the hypoxic region, but also seek the leaky, higher pressure vessels instead of forming self-connections, which are less productive in terms of tissue perfusion.
Song and Munn |
PNAS | September 13, 2011 | vol. 108 | no. 37 | 15345 |
MEDICAL SCIENCES
Downloaded by guest on November 18, 2019
Fig. 4. Sprout morphogenesis is affected by the direction of interstitial flow
and VEGF gradient. (A–C) Filopodia formation in sprouting HUVECs in the (A) SB0TaG+jV50, (B) SA0TwG−jV50, and (C) SA0TwG0jSA0TwG0jV50 flow con-
figurations. Interstitial flow rates were (A) 2.5, (B) 35, and (C) 28.5 μm/s. Each image depicts a single aperture imaged 2–3 d after initiation of experiment. (Scale bars, 100 μm.) (D) Quantification of the number of filopodia per sprouting area produced by sprouting HUVECs. n = 5–21. *P < 0.05; **P < 0.001; ns, P = 0.96. Gradient blue and solid blue VEGF bars indicate VEGF gradient and uniform VEGF concentration, respectively, in the collagen gel. Dashed arrows indicated direction of interstitial flow. (E) Isolated effects of interstitial flow and VEGF gradient on sprouting area, comparing the normalized sprout area at day 3 from each sprouting direction (with interstitial flow and a negative VEGF gradient or against interstitial flow with a positive VEGF gradient). Interstitial flow alone significantly enhances sprout area for both sprouting directions (***). Addition of a VEGF gradient to interstitial flow significantly increases sprout area compared with interstitial flow only, for both sprouting directions (***9). Furthermore, the normalized area of sprouting for interstitial flow only (B/A: 39 ± 5; A/B: 37 ± 6) plus VEGF gradient only (B/A: 28 ± 5; A/B: 23 ± 4) is comparable to the area when both VEGF gradient and interstitial flow are present (B/A: 65 ± 10; A/B: 56 ± 7), suggesting that these components are additive in enhancing sprout area for both sprouting directions. n = 21–49. Data points represent mean + SEM. *** or ***9P < 0.0001.
Thus, by integrating flow and VEGF signals, endothelial cells can more efficiently determine (i) whether they reside in a damaged vessel and are candidates for sprouting (driven by changes in luminal shear stress), (ii) in which direction to extend to revascularize hypoxic regions (driven by VEGF gradients), and (iii) which direction sprouts should extend to reach nearby vessels with different pressure (driven by interstitial flow). A better understanding of how these signals are integrated to coordinate sprouting should lead to therapeutic strategies for modulating pathological angiogenesis.
Fig. 5. Putative integration of flow forces and VEGF in damaged tissue. (A) Hypoxic cells (blue) residing in an ischemic region produce VEGF (small blue dots). The damaged, occluded vessel within this region lacks shear stress, but fills with VEGF, and its ECs sense a negative VEGF gradient. This vessel dilates (walls outlined in pink) and becomes leaky in response (arrows; note that P1 > P2). Proximal ECs in the other occluded vessel (Lower) see a positive VEGF gradient across the vessel wall (orange outline), whereas those in the opposite wall see a negative gradient (pink outline). The former sprout, whereas the latter dilate. Morphogenesis of nondamaged, well-perfused vessels is inhibited by shear stress (green outline). (B and C) Interstitial flow supports efficient revascularization. If no fluid forces were involved with mediating revascularization and instead relied solely on VEGF and other chemical factors, then many self-connections would be made between the sprouting vessels, leading to inefficient reperfusion (B). However, interstitial flow originating from the leaky and dilated central vessel serves as an important cue that guides the sprouts toward this higher-pressure vessel to ensure more uniform revascularization of the central region (C).
Materials and Methods
The microfluidic devices were fabricated from PDMS, using standard soft lithography techniques (48). A collagen gel solution (3 mg mL−1 type I collagen, 10 μg mL−1 fibronectin) was localized to defined regions and then polymerized for at least 48 h at 37 °C and hydrated conditions. HUVECs were seeded onto fibronectin-coated regions (10 μg mL−1). Shear stress levels in microfluidic channels were estimated using previously published data for channels of comparable heights and aspect ratios (49, 50). Interstitial flow across the collagen gel was measured experimentally by tracking fluid displacement over time in both the perfused and nonperfused sides of the flow configuration with 1 μm fluorescent beads. The chemical gradient profiles were measured experimentally in HUVEC-lined channels using TRITC-BSA (MW 66 kDa) dissolved in cell culture medium as fluorescent surrogate for VEGF. Filopodia formation was determined by two independent reviewers who blindly analyzed and counted confocal projection images. To systematically investigate whether VEGF and mechanical fluid forces cooperate during the initiation of angiogenesis, we use the nomenclature summarized in Table 1. Additional and more detailed methods are described in SI Materials and Methods.
ACKNOWLEDGMENTS. We are grateful to P. Au, G. Cheng, and J. Tse for performing the retroviral transfections of the HUVECs provided to us by the Center for Vascular Excellence at Brigham and Women’s Hospital. We thank R. Samuel for her assistance with counting filopodia, A. Jain for helpful discussions, and R. Jain for his invaluable insight and suggestions. Funding was provided by the National Cancer Institute (L.L.M).
15346 | www.pnas.org/cgi/doi/10.1073/pnas.1105316108 |
Song and Munn |

Downloaded by guest on November 18, 2019
1.Carmeliet P, Jain RK (2000) Angiogenesis in cancer and other diseases. Nature 407: 249e257.
2.Davis GE, Bayless KJ, Mavila A (2002) Molecular basis of endothelial cell morphogenesis in three-dimensional extracellular matrices. Anat Rec 268:252e275.
3.Ingber DE (2002) Mechanical signaling and the cellular response to extracellular matrix in angiogenesis and cardiovascular physiology. Circ Res 91:877e887.
4.Carmeliet P, De Smet F, Loges S, Mazzone M (2009) Branching morphogenesis and antiangiogenesis candidates: Tip cells lead the way. Nat Rev Clin Oncol 6:315e326.
5.Gerhardt H, et al. (2003) VEGF guides angiogenic sprouting utilizing endothelial tip cell filopodia. J Cell Biol 161:1163e1177.
6.Patan S, Munn LL, Jain RK (1996) Intussusceptive microvascular growth in a human colon adenocarcinoma xenograft: A novel mechanism of tumor angiogenesis. Microvasc Res 51:260e272.
7.Jain RK (2005) Normalization of tumor vasculature: An emerging concept in antiangiogenic therapy. Science 307:58e62.
8.Harris AL (2002) Hypoxia—a key regulatory factor in tumour growth. Nat Rev Cancer 2:38e47.
9.Ferrara N, Gerber H-P, LeCouter J (2003) The biology of VEGF and its receptors. Nat Med 9:669e676.
10.Yancopoulos GD, et al. (2000) Vascular-specific growth factors and blood vessel formation. Nature 407:242e248.
11.Hellström M, et al. (2007) Dll4 signalling through Notch1 regulates formation of tip cells during angiogenesis. Nature 445:776e780.
12.Davies PF (1995) Flow-mediated endothelial mechanotransduction. Physiol Rev 75: 519e560.
13.Frangos JA, Eskin SG, McIntire LV, Ives CL (1985) Flow effects on prostacyclin production by cultured human endothelial cells. Science 227:1477e1479.
14.Shyy JY, Chien S (2002) Role of integrins in endothelial mechanosensing of shear stress. Circ Res 91:769e775.
15.Topper JN, Cai J, Falb D, Gimbrone MA, Jr. (1996) Identification of vascular endothelial genes differentially responsive to fluid mechanical stimuli: Cyclooxygenase-2, manganese superoxide dismutase, and endothelial cell nitric oxide synthase are selectively up-regulated by steady laminar shear stress. Proc Natl Acad Sci USA 93: 10417e10422.
16.Hernández Vera R, et al. (2009) Interstitial fluid flow intensity modulates endothelial sprouting in restricted Src-activated cell clusters during capillary morphogenesis.
Tissue Eng Part A 15:175e185.
17.Tada S, Tarbell JM (2000) Interstitial flow through the internal elastic lamina affects shear stress on arterial smooth muscle cells. Am J Physiol Heart Circ Physiol 278: H1589eH1597.
18.Garcia-Cardeña G, Comander J, Anderson KR, Blackman BR, Gimbrone MA, Jr. (2001) Biomechanical activation of vascular endothelium as a determinant of its functional phenotype. Proc Natl Acad Sci USA 98:4478e4485.
19.White CR, Frangos JA (2007) The shear stress of it all: The cell membrane and mechanochemical transduction. Philos Trans R Soc Lond B Biol Sci 362:1459e1467.
20.Wang Y, et al. (2007) Selective adapter recruitment and differential signaling networks by VEGF vs. shear stress. Proc Natl Acad Sci USA 104:8875e8879.
21.Kang H, Bayless KJ, Kaunas R (2008) Fluid shear stress modulates endothelial cell invasion into three-dimensional collagen matrices. Am J Physiol Heart Circ Physiol 295: H2087eH2097.
22.Tressel SL, Huang RP, Tomsen N, Jo H (2007) Laminar shear inhibits tubule formation and migration of endothelial cells by an angiopoietin-2 dependent mechanism. Arterioscler Thromb Vasc Biol 27:2150e2156.
23.Hueck IS, Rossiter K, Artmann GM, Schmid-Schönbein GW (2008) Fluid shear attenuates endothelial pseudopodia formation into the capillary lumen. Microcirculation 15:531e542.
24.Price GM, et al. (2010) Effect of mechanical factors on the function of engineered human blood microvessels in microfluidic collagen gels. Biomaterials 31:6182e6189.
25.Hudlicka O, Brown MD, May S, Zakrzewicz A, Pries AR (2006) Changes in capillary shear stress in skeletal muscles exposed to long-term activity: Role of nitric oxide.
Microcirculation 13:249e259.
Song and Munn
26.Jones EAV, le Noble F, Eichmann A (2006) What determines blood vessel structure? Genetic prespecification vs. hemodynamics. Physiology (Bethesda) 21:388e395.
27.Lin K, et al. (2000) Molecular mechanism of endothelial growth arrest by laminar shear stress. Proc Natl Acad Sci USA 97:9385e9389.
28.Helmlinger G, Geiger RV, Schreck S, Nerem RM (1991) Effects of pulsatile flow on cultured vascular endothelial cell morphology. J Biomech Eng 113:123e131.
29.Blackman BR, García-Cardeña G, Gimbrone MA, Jr. (2002) A new in vitro model to evaluate differential responses of endothelial cells to simulated arterial shear stress waveforms. J Biomech Eng 124:397e407.
30.Helm CL, Fleury ME, Zisch AH, Boschetti F, Swartz MA (2005) Synergy between interstitial flow and VEGF directs capillary morphogenesis in vitro through a gradient amplification mechanism. Proc Natl Acad Sci USA 102:15779e15784.
31.Adamo L, et al. (2009) Biomechanical forces promote embryonic haematopoiesis. Nature 459:1131e1135.
32.Sessa WC (2004) eNOS at a glance. J Cell Sci 117:2427e2429.
33.Kashiwagi S, et al. (2008) Perivascular nitric oxide gradients normalize tumor vasculature. Nat Med 14:255e257.
34.Suchting S, et al. (2007) The Notch ligand Delta-like 4 negatively regulates endothelial tip cell formation and vessel branching. Proc Natl Acad Sci USA 104:3225e3230.
35.Djonov V, Schmid M, Tschanz SA, Burri PH (2000) Intussusceptive angiogenesis: Its role in embryonic vascular network formation. Circ Res 86:286e292.
36.Jones EAV, Baron MH, Fraser SE, Dickinson ME (2004) Measuring hemodynamic changes during mammalian development. Am J Physiol Heart Circ Physiol 287: H1561eH1569.
37.Gruionu G, Hoying JB, Gruionu LG, Laughlin MH, Secomb TW (2005) Structural adaptation increases predicted perfusion capacity after vessel obstruction in arteriolar arcade network of pig skeletal muscle. Am J Physiol Heart Circ Physiol 288: H2778eH2784.
38.Skalak TC (2005) Angiogenesis and microvascular remodeling: A brief history and future roadmap. Microcirculation 12:47e58.
39.Akimoto S, Mitsumata M, Sasaguri T, Yoshida Y (2000) Laminar shear stress inhibits vascular endothelial cell proliferation by inducing cyclin-dependent kinase inhibitor p21(Sdi1/Cip1/Waf1). Circ Res 86:185e190.
40.Levesque MJ, Nerem RM, Sprague EA (1990) Vascular endothelial cell proliferation in culture and the influence of flow. Biomaterials 11:702e707.
41.Yamada H, et al. (1999) Hyperoxia causes decreased expression of vascular endothelial growth factor and endothelial cell apoptosis in adult retina. J Cell Physiol 179: 149e156.
42.Anderson CR, Hastings NE, Blackman BR, Price RJ (2008) Capillary sprout endothelial cells exhibit a CD36 low phenotype: Regulation by shear stress and vascular endothelial growth factor-induced mechanism for attenuating anti-proliferative throm- bospondin-1 signaling. Am J Pathol 173:1220e1228.
43.Kamoun WS, et al. (2010) Simultaneous measurement of RBC velocity, flux, hematocrit and shear rate in vascular networks. Nat Methods 7:655e660.
44.Munn LL (2003) Aberrant vascular architecture in tumors and its importance in drugbased therapies. Drug Discov Today 8:396e403.
45.Kuchan MJ, Frangos JA (1994) Role of calcium and calmodulin in flow-induced nitric oxide production in endothelial cells. Am J Physiol 266:C628eC636.
46.Tarbell JM, Demaio L, Zaw MM (1999) Effect of pressure on hydraulic conductivity of endothelial monolayers: Role of endothelial cleft shear stress. J Appl Physiol 87: 261e268.
47.Shi Z-D, Wang H, Tarbell JM (2011) Heparan sulfate proteoglycans mediate interstitial flow mechanotransduction regulating MMP-13 expression and cell motility via FAKERK in 3D collagen. PLoS ONE 6:e15956.
48.Duffy DC, McDonald JC, Schueller OJA, Whitesides GM (1998) Rapid Prototyping of Microfluidic Systems in Poly(dimethylsiloxane). Anal Chem 70:4974e4984.
49.Gaver DP, 3rd, Kute SM (1998) A theoretical model study of the influence of fluid stresses on a cell adhering to a microchannel wall. Biophys J 75:721e733.
50.Zeng Y, Lee TS, Yu P, Roy P, Low HT (2006) Mass transport and shear stress in a microchannel bioreactor: Numerical simulation and dynamic similarity. J Biomech Eng 128:185e193.
PNAS | September 13, 2011 | vol. 108 | no. 37 | 15347
MEDICAL SCIENCES
