
книга / 2016_Kaplan_USMLE_Step_1_Lecture_Notes_Pharmacology
.pdf
Chapter 4 λ Antiarrhythmic Drugs
−Uses: DOC for paroxysmal supraventricular tachycardias and AV nodal arrhythmias
−Administered IV: t1/2 <10 seconds
−Side effects: flushing, sedation, dyspnea
−Adenosine is antagonized by methylxanthines (theophylline and caffeine)
λMagnesium
−Use: torsades
−Drugs causing torsades include:
ºPotassium-channel blockers (class 1A and class III)
ºAntipsychotics (thioridazine)
ºTricyclic antidepressants
Chapter Summary
λThe sequences of ionic events in the action potential of cardiac cells are described.
λDepolarization (phase 0) is due to Na+ influx in fast fibers and due to Ca2+ influx in SA and AV nodal cells. Class I antiarrhythmic drugs block Na+ influx and class IV antiarrhythmics block Ca2+ influx.
λRepolarization (phase 3) in all cardiac cells is due to K+ efflux (delayed rectifier current) and this is blocked by class IA and class III antiarrhythmic drugs. Pacemaker currents (phase 4) are blocked by class II and class IV drugs.
λResponsivity, capacity of a cell for depolarization, depends on resting membrane potential; con-ductance is the rate of potential spread; refractoriness is the inability to respond to excitation.
λFigure III-4-4 depicts the M and h gates of cardiac Na+ channels. Three conformations exist—resting (ready), active (open), and inactive (refractory). Class I drugs are least active when Na+ channels are in the resting state (state-dependent actions).
λActions of class II antiarrhythmics (beta blockers) involve antagonism of
SANS-mediated increases in cAMP, especially at SA and AV nodal cells to slow phase 0 and 4 of the action potential.
λThe class I antiarrhythmic drugs block Na+ channels. Class IA drugs are state-dependent blockers of fast Na+ channels, and they increase the action potential duration (APD). Quinidine, in addition, is an M blocker and can increase the heart rate and AV conduction. Procainamide has less M block than quinidine and no alpha block. The uses and contraindications of quinidine and procainamide are provided.
λClass IB drugs are less state-dependent blockers of fast Na+ channels, and they decrease the APD. The uses for lidocaine, mexiletine, and tocainide are discussed, as are the metabolism and adverse effects of lidocaine.
λThe class IC drug flecainide blocks fast Na+ channels, especially of HisPurkinje cells, and has no effect on the APD and no ANS effects.
109
Section III λ Cardiac and Renal Pharmacology
Chapter Summary (cont’d )
λClass II antiarrhythmic drugs are beta-blockers that decrease SA and AV
nodal activity, decrease the phase 4 slope, and prevent β1 adrenoceptor activation, thereby circumventing the normal increase in cAMP. Propranolol is nonselective; acebutolol and esmolol are selective. Their antiarrhythmic use is discussed.
λClass III antiarrhythmic drugs are K+-channel blockers that increase the APD and effective refractory period (ERP), especially in Purkinje and ventricular tissues. Amiodarone and sotalol are the examples discussed.
λClass IV antiarrhythmic drugs are Ca2+-channel blockers that decrease the SA and AV nodal activity and the slope of phase 4 of the action potential in pacemakers. The uses and adverse effects of verapamil are indicated.
λAdenosine and magnesium are two unclassified antiarrhythmic drugs. Adenosine decreases SA and AV node activity and increases the AV node refractory period. Magnesium has possible use in torsades. Drugs (other than classes Ia and III antiarrhythmics) associated with torsades include thioridazine and tricyclic antidepressants.
110
Antianginal Drugs |
5 |
Learning Objectives
Solve problems concerning the rationale for the use of nitrates, beta blockers, and carvedilol for angina
Use knowledge of calcium channel blockers
Demonstrate understanding of ranolazine
RATIONALE FOR USE
Angina pectoris is the principal syndrome of ischemic heart disease, anginal pain occurring when oxygen delivery to the heart is inadequate for myocardial requirement.
λStable/classic angina (angina of effort or exercise) is due to coronary atherosclerotic occlusion
λVasospastic or variant angina (Prinzmetal) is due to a reversible decrease in coronary blood flow
Drug Strategies in Stable and Vasospastic Angina
Drug strategies in stable and vasospastic angina involve:
↓ oxygen requirement by ↓ TPR, CO, or both (nitrates, CCBs, and beta blockers).
↑ oxygen delivery by ↓ vasospasm (nitrates and CCBs).
111
Section III λ Cardiac and Renal Pharmacology
Clinical Correlate
Sildenafil (Viagra)
Phosphodiesterase 5 (PDE5) is found in blood vessels supplying the corpora cavernosa. Sildenafil
inhibits PDE 5 |
← |
↑ cGMP |
← |
|
|
||
vasodilation |
← |
↑ blood flow |
← |
↑ |
|||
|
|
|
|||||
erectile response. If used concomitantly with nitrates or other potent vasodilators, the excessive fall in blood pressure may lead to death from cardiovascular causes, including myocardial infarct.
NITRATES
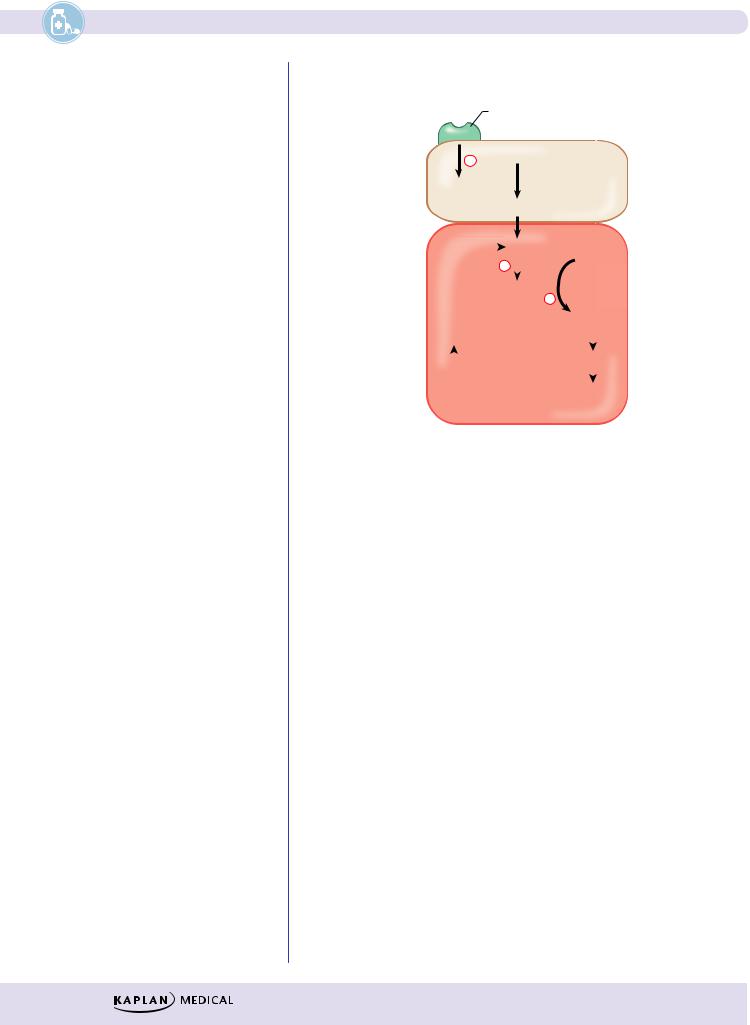
Receptor (ACh, bradykinin, 5HT, etc)
+L-Arg.
Endothelial NO cell
synthase NO
|
|
NO |
|
GTP |
|
||
|
|
|
|
||||
|
+ |
|
|
|
|||
|
|
|
|||||
|
Guanylyl |
+ |
|
|
Smooth |
||
|
cyclase |
CGMP |
|||||
|
|
|
|
|
muscle |
||
|
|
|
|
|
|
cell |
|
Nitrosothiol?? |
|
|
|
||||
|
Cysteine |
|
|
|
|
||
|
|
|
|
|
|||
|
|
|
|
|
Relaxation |
|
|
|
|
|
|
|
|
||
Nitroglycerin  R-O-N=O
R-O-N=O
Figure III-5-1. Nitrates and the Nitric Oxide Pathway
λNitrates are prodrugs of nitric oxide
λVenodilation → ↓ preload → ↓ cardiac work → ↓ oxygen requirement
λNitrates ↓ infarct size and post-MI mortality
λDrugs:
−Nitroglycerin: sublingual, transdermal, and IV formulations
−Isosorbide: oral, extended release for chronic use
−Side effects:
ºFlushing, headache, orthostatic hypotension
ºReflex tachycardia and fluid retention
−Cautions and contraindications:
ºTachyphylaxis with repeated use
ºCardiovascular toxicity with sildenafil (see Clinical Correlate, left)
112
BETA BLOCKERS AND CARVEDILOL
λUsed in angina of effort
λβ-blockers are contraindicated in vasospastic angina
λCarvedilol is clinically equivalent to isosorbide in angina of effort
CALCIUM CHANNEL BLOCKERS (CCBs)
λAll CCBs can be used.
λNifedipine is important for vasospastic angina.
λSee Antihypertensive Drugs, chapter 3 in this section.
RANOLAZINE
λIschemia causes increased sodium which prevents calcium exit through Na+/Ca++ exchanger pump
λRanolazine blocks late inward Na+ current in cardiac myocytes, thereby decreasing calcium accumulation
λResults in decreased end diastolic pressure and improvement of diastolic coronary flow
λSide effects include constipation and nausea; increased QT makes the drug contraindicated in patients with long QT syndrome or taking drugs which increase QT (see Magnesium discussion in Chapter 4, Antiarrhythmic Drugs)
Chapter 5 λ Antianginal Drugs
Clinical Correlate
Drugs that decrease mortality in patients with stable angina include aspirin, nitroglycerin, and beta blockers. Nitroglycerin is the preferred drug for acute management of both stable and vasospastic angina.
113
|
Section III λ |
Cardiac and Renal Pharmacology |
|
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
RELAXATION |
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
(↑ cAMP or ↑ cGMP) |
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
Calcium channel blockers |
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
(Nifedipine) |
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Gs coupled receptors (β2) |
|
|
|
|
|
PDE inhibitors |
|
|
|||||||||||||||||
|
|
|
|
|
|
|
(Theophylline, Inamrinone) |
|
||||||||||||||||||||||
|
|
|
|
|
|
|
+ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ATP |
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Adenyl cyclase |
|
|
|
|
|
phospho- |
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
diesterase |
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
cAMP |
|
|
|
AMP |
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
+ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Protein kinase A |
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Myosin light chain kinase P |
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
(inactive) |
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
Myosin light chain |
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(inactive) |
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
Phosphatase |
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
+ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
Protein kinase G |
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
+ |
|
|
|
|
|
phospho- |
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
diesterase |
|
|
|
|||||||
|
|
|
|
+ |
|
|
|
|
|
|
|
|
|
cGMP |
|
|
|
GMP |
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NO |
|
|
|
Guanyl cyclase |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
+ |
|
|
|
|
|
|
|
GTP |
|
|
PDE inhibitors |
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(sildenafil) |
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
Gq-coupled |
|
|
|
• NO-giving drugs |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
receptors |
|
|
|
(nitroprusside, |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
(M3, bradykinin, |
|
|
hydralazine, |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
H1 receptors on |
|
|
nitroglycerin) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
endothelium) |
|
|
|
• Nesiritide |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
CONTRACTION ↑(Ca2+)
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Gq coupled |
||||
|
|
|
|
||||||||
Calcium |
|
|
|
receptors |
|||||||
|
|
(α, M3 receptors |
|||||||||
entry |
|
|
|
||||||||
|
|
|
|
|
|
on smooth muscle) |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
Ca2+ |
|
|
|
|
||
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
Ca2+ calmodulin |
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
Myosin light chain kinase (active)
Myosin light chain |
P |
|
|
|
|
|
|
|
|
|
|
Myosin light chain |
P |
|
plus actin |
|
|
Figure III-5-2. Mechanisms of Smooth Muscle Contraction and
Relaxation and Drugs Affecting Them
114
Chapter 5 λ Antianginal Drugs
Chapter Summary
λAngina is the principal syndrome caused by ischemic heart disease. The forms are classic, stable and vasospastic.
λThe drug strategies are to increase oxygen supply by decreasing vasospasm (nitrates and calcium channel antagonists [CCBs]) and to decrease cardiac oxygen requirements by decreasing peripheral vascular resistance and/or cardiac output (nitrates, CCBs, and beta blockers).
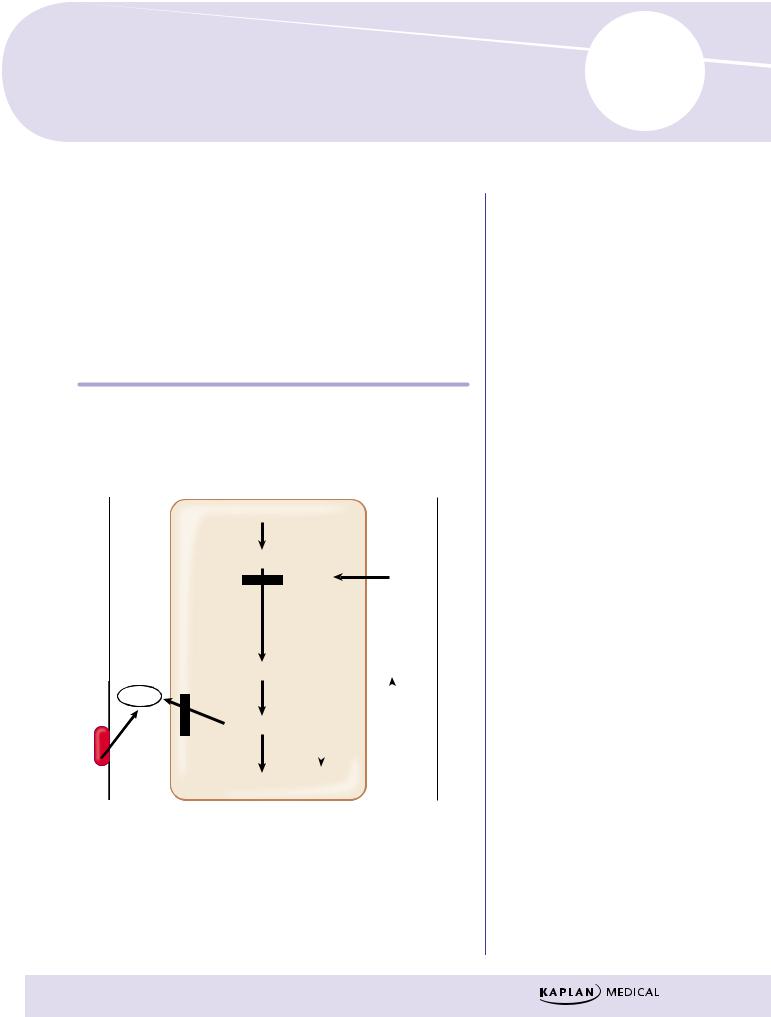
λNitrates increase NO concentrations. Increased NO activates guanylyl cyclase; this increases cGMP levels, which dephosphorylates myosin light chains, decreasing their association with actin and thereby promoting smooth muscle relaxation. These mechanisms are summarized in Figure III-5-1.
λNO-enhancing drugs used to treat angina include nitroglycerin and isosorbide.
λThe adverse effects of the nitrates are also considered.
λCCBs decrease contractility and increase vasodilation by preventing the influx of Ca2+ required for muscle contraction. The sequence of reactions involved is summarized in Figure III-5-2. The CCBs considered are the dihydropyridines (e.g., nifedipine), verapamil, and diltiazem.
λBeta blockers act directly on the heart by decreasing the heart rate, the force of contraction, and cardiac output, thereby decreasing the work performed.
115
Antihyperlipidemics 6
Learning Objectives
Solve problems concerning HMG-CoA reductase inhibitors
Demonstrate understanding of bile acid sequestrants
Use knowledge of nicotinic acid (niacin, vitamin B3)
Solve problems concerning gemfibrozil, fenofibrate (fibrates)
Explain information related to ezetimibe
Answer questions related to orlistat
λ↑ risk of atherosclerosis is associated with hypercholesterolemia
λ↑ risk of cardiovascular and cerebrovascular diseases
λTreatment goal is to ↓ LDL cholesterol and atheroma plaque formation
Lipoprotein Lipase
Gemfibrozil
Blood |
AcCoA |
GI |
|
|
Niacin, Statins
VLDL
HMG CoA
Statins
Mevalonic acid
Cholesterol
Bile acids
|
|
|
|
Cholesterol |
Ezetimibe |
|
|
|
|||
|
|
|
|||
|
|
out |
Cholestyramine |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Colestipol |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Figure III-6-1. Site of Action of Statins, Niacin, and Gemfibrozil on the Synthesis of Lipids
117
Section III λ Cardiac and Renal Pharmacology
Clinical Correlate
Nonstatin drugs have not been shown to improve cardiovascular outcomes when added to statin therapy. These drugs are most often used in patients who cannot tolerate a statin.
HMG-CoA REDUCTASE INHIBITORS
λDrugs: atorvastatin, rosuvastatin, and other “–statins”
−At their highest therapeutic doses, atorvastatin and rosuvastatin are considered “high-intensity” statins and can lower LDL-C by ≥ 50%
−Lower doses of statins are classified as “low” or “moderate” intensity
λMechanisms:
−HMG-CoA reductase inhibition, results in:
º↓ liver cholesterol
º↑ LDL-receptor expression
º↓ plasma LDL
−↓ VLDL synthesis results in: ↓ triglyceridemia
λSide effects:
−Myalgia, myopathy (check creatine kinase)
−Rhabdomyolysis
−Hepatotoxicity (check liver function tests)
λDrug interaction:
−Gemfibrozil (↑ rhabdomyolysis)
−Cytochrome P450 inhibitors enhance toxicity of statins
BILE ACID SEQUESTRANTS
λDrugs: cholestyramine and colestipol
λMechanism: complexation of bile salts in the gut, results in:
−↓ enterohepatic recirculation of bile salts
−↑ synthesis of new bile salts by the liver
−↓ liver cholesterol
−↑ LDL-receptor expression
−↓ blood LDL
λSide effects:
−↑ VLDL and triglycerides
−Gastrointestinal disturbances
−Malabsorption of lipid-soluble vitamins
−Hyperglycemia
λDrug interactions with orally administered drugs (warfarin, thiazides, digoxin, etc.)
λContraindication: hypertriglyceridemia
NICOTINIC ACID (NIACIN, VITAMIN B3)
λMechanism: inhibition of VLDL synthesis, results in:
−↓ plasma VLDL
−↓ plasma LDL
−↑ plasma HDL
118
