
книга / 2016_Kaplan_USMLE_Step_1_Lecture_Notes_Pharmacology
.pdf

Section V λ Antimicrobial Agents
Chapter Summary
Basic Principles
λAntibacterial drugs can be either bactericidal or bacteriostatic. The effectiveness of bacteriostatic drugs depends on an intact host immune system. Antimicrobial agents may be administered singly or in combination. Some combinations induce synergy and/or delay emergence of resistance.
λAn antimicrobial agent should have maximal toxicity toward the infecting agent and minimal toxicity for the host. Table V-1-1 summarizes the four basic antibacterial actions demonstrated by antibiotics and the agents working by each of these mechanisms.
λMicrobial resistance can occur by the gradual selection of resistant mutants or more usually by R-factor transmission between bacteria. Table V-1-2 summarizes the common modes of resistance exhibited by microorganisms against the various classes of antimicrobial agents.
Inhibitors of Bacterial Cell-Wall Synthesis
λThe inhibitors of bacterial cell-wall synthesis are the beta-lactam antibiotics (the penicillins and cephalosporins; Figure V-1-1), the carbapenems, vancomycin, and aztreonam.
λThe mechanisms of action of penicillins, the bacterial modes of resistance to penicillins, the penicillin subgroups, their biodisposition, and side effects are provided. The subgroups discussed are the penicillins that are β-lactamase susceptible with a narrow spectrum of activity; β-lactamase–resistant penicillins that have a very narrow spectrum of activity; and β-lactamase–susceptible penicillins that have a wider spectrum of activity. The common penicillins and their susceptible organisms are listed for each subgroup.
λThe same parameters are considered for the cephalosporins. These have the same mode of action as the penicillins and also require an intact β-lactam ring structure for activity. There are four generations of cephalosporins. Each is considered in terms of range of activity, susceptibility to resistance, clinical usage, and specific antibiotics in that class.
λImipenem and meropenem have the same mode of antibacterial action as the penicillins and cephalosporins but structurally are carbapenems that have the β-lactam ring. Their clinical uses, routes of elimination, and side effects are considered.
λAztreonam is a monobactam inhibitor of early cell-wall synthesis. It is used primarily as an intravenous drug against gram-negative rods.
λVancomycin inhibits an early stage of cell-wall synthesis. It has a relatively narrow range of activity, but as yet, resistance is uncommon. Its use, excretion, and side effects are considered.
(Continued )
192

Chapter 1 λ Antibacterial Agents
Chapter Summary (cont’d )
Inhibitors of Bacterial Protein Synthesis
λFigure V-1-2 illustrates the mechanisms of bacterial protein synthesis, and Table V-1-3 summarizes the places in the translatory sequence, as well as the mechanisms by which antibiotics operate to disrupt protein synthesis.
λThe aminoglycosides (e.g., gentamicin and tobramycin) inhibit initiation complex formation. Their uses and properties are discussed. Streptomycin is particularly useful in the treatment of tuberculosis and is the drug of choice for treating bubonic plague and tularemia. Neomycin is toxic and can only be used topically.
λThe tetracyclines block the attachment of aminoacyl tRNA to the acceptor site on the bacterial ribosome. They are broad-spectrum drugs with good activity against chlamydial and mycoplasmal species, as well as against other indicated bacteria. Doxycycline is of particular use in the treatment of
prostatitis, minocycline is useful for treating meningococcal carrier states, and demeclocycline is useful for treating the syndrome of inappropriate secretion of ADH (SIADH). Their biodisposition and side effects are discussed.
λChloramphenicol inhibits the activity of peptidyltransferase and is currently used primarily as a backup drug. Its activity, clinical use, and side effects are considered.
λThe macrolides (e.g., erythromycin, clarithromycin, and azithromycin) are translocation inhibitors. Their spectrums of activity, clinical uses, biodisposition, and side effects are considered. Clindamycin is not a macrolide but shares the same mechanism of action.
λLinezolid inhibits initiation by blocking formation of the N-formyl-methionyl- tRNA-ribosome-mRNA ternary complex. The clinical uses and side effects of this new drug are mentioned.
λQuinupristin and dalfopristin bind to the 50S ribosomal subunit, where they interfere with the interaction of aminoacyl-tRNA and the acceptor site and also stimulate its dissociation from the ternary complex. Their clinical use and side effects are discussed.
Antibiotics That Inhibit Folic Acid Synthesis and Nucleic Acid Metabolism
λThe sulfonamides compete with para-aminobenzoic acid (PABA) as shown in Figure V-1-3. The methods bacteria use to develop resistance to the
sulfonamides, their activity and clinical uses, biodisposition, and side effects are considered.
λTrimethoprim (TMP), a folate analog and inhibitor of dihydrofolate reductase (Figure V-1-3), is usually used together with sulfamethoxazole (SMX). The simultaneous inhibition of the tetrahydrofolate synthesis pathway at two steps has a synergistic effect and prevents the rapid generation of resistance. The clinical uses and side effects of TMP-SMX are discussed.
(Continued )
193

Section V λ Antimicrobial Agents
Chapter Summary (cont’d )
λThe fluoroquinones (e.g., ciprofloxacin) are nalidixic acid analogs that inhibit topoisomerase II (DNA gyrase) and topoisomerase IV. Their clinical use,
the relevant drugs in this class, their biodisposition, and side effects are reported.
λThe exact mode of metronidazole action is unknown. Its use as an antiprotozoal and antibacterial drug is discussed, as are its side effects.
Antitubercular Drugs
λInfections caused by Mycobacterium tuberculosis are treated with combination therapy. The primary drugs used are isoniazid, rifampin, ethambutol, and pyrazinamide. Highly resistant organisms may require the use of additional agents. Backup drugs include streptomycin, fluoroquinolones, capreomycin, and cycloserine.
λTable V-1-4 summarizes the actions, resistance, and side effects of the antitubercular drugs.
194

Antifungal Agents |
2 |
Learning Objectives
Demonstrate understanding of the use and side effects of polyenes (amphotericin B, nystatin), azoles (ketoconazole, fluconazole, itraconazole, voriconazole), and other antifungals
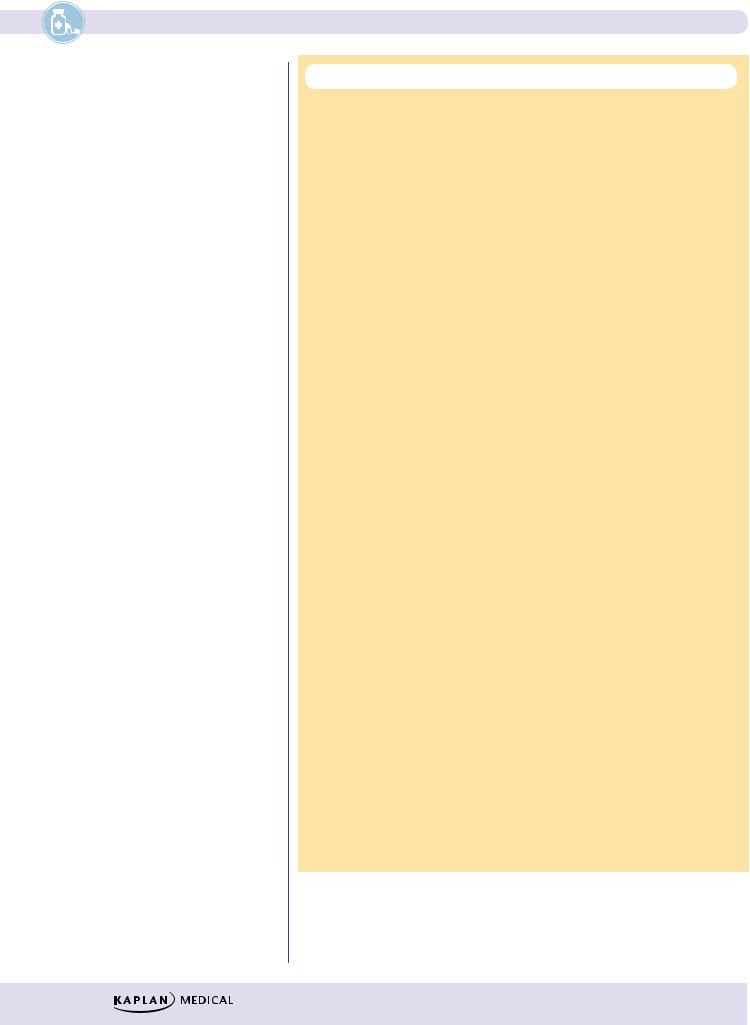
Caspo “fungin”
inhibits  Beta-glucan Cell wall synthesis
Beta-glucan Cell wall synthesis
|
|
|
|
|
|
|
|
|
|
Cell membrane |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
= lipid-bilayer |
|
|
|
|
|
|
|
|
|
|
Amphotericin B |
||
“Azoles” |
|
|
|
|
|
|
|
|
|
binds |
|||
|
|
|
14-α-demethylase |
|
|||||||||
|
|
|
|
|
|
|
|
||||||
|
inhibit |
|
|
|
|
|
|
|
|
|
|
|
|
= ergosterol |
|
|
|
|
|
|
|
|
Terbinafine |
|
|||
|
|
|
Lanosterol |
inhibits |
|
||||||||
|
|
|
|
|
|
|
Squalene |
|
|
Squalene |
|||
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
epoxide |
|
Squalene |
||||
|
|
|
|
|
|
|
|||||||
epoxidase
Figure V-2-1. Mechanism of Action of Antifungal Drugs
POLYENES (AMPHOTERICIN B [AMP B], NYSTATIN)
λMechanisms:
–Amphoteric compounds with both polar and nonpolar structural components—interact with ergosterol in fungal membranes to form artificial “pores,” which disrupt membrane permeability
–Resistant fungal strains appear to have low ergosterol content in their cell membranes
λActivity and clinical uses:
− Amphotericin B has wide fungicidal spectrum; remains the DOC (or co-DOC) for severe infections caused by Cryptococcus and Mucor
− Amphotericin B—synergistic with flucytosine in cryptococcoses − Nystatin (too toxic for systemic use)—used topically for localized
infections (e.g., candidiasis)
195

Section V λ Antimicrobial Agents
λPharmacokinetics:
−Amphotericin B given by slow IV infusion—poor penetration into the CNS (intrathecal possible)
−Slow clearance (half-life >2 weeks) via both metabolism and renal elimination
λSide effects:
−Infusion-related
ºFever, chills, muscle rigor, hypotension (histamine release) occur during IV infusion (a test dose is advisable)
ºCan be alleviated partly by pretreatment with NSAIDs, antihistamines, meperidine, and adrenal steroids
−Dose-dependent
ºNephrotoxicity includes ↓ GFR, tubular acidosis, ↓ K+ and Mg2+, and anemia through ↓ erythropoietin
ºProtect by Na+ loading, use of liposomal amphotericin B, or by drug combinations (e.g., + flucytosine), permitting ↓ in amphotericin B dose
AZOLES (KETOCONAZOLE, FLUCONAZOLE,
ITRACONAZOLE, VORICONAZOLE)
λMechanism:
−“Azoles” are fungicidal and interfere with the synthesis of ergosterol by inhibiting 14-α-demethylase, a fungal P450 enzyme, which converts lanosterol to ergosterol
−Resistance occurs via decreased intracellular accumulation of azoles
λActivity and clinical uses:
−Ketoconazole
ºCo-DOC for Paracoccidioides and backup for Blastomyces and Histoplasma
ºOral use in mucocutaneous candidiasis or dermatophytoses
−Fluconazole
ºDOC for esophageal and invasive candidiasis and coccidioidomycoses
ºProphylaxis and suppression in cryptococcal meningitis
−Itraconazole and Voriconazole
ºDOC in blastomycoses, sporotrichoses, aspergillosis
ºBackup for several other mycoses and candidiasis
−Clotrimazole and miconazole
ºUsed topically for candidal and dermatophytic infections
λPharmacokinetics:
−Effective orally
−Absorption of ketoconazole ↓ by antacids
−Absorption of itraconazole ↑ by food
196

Chapter 2 λ Antifungal Agents
−Only fluconazole penetrates into the CSF and can be used in meningeal infection. Fluconazole is eliminated in the urine, largely in unchanged form.
−Ketoconazole and itraconazole are metabolized by liver enzymes.
−Inhibition of hepatic P450s
λSide effects:
−↓ synthesis of steroids, including cortisol and testosterone → ↓ libido, gynecomastia, menstrual irregularities
−↑ liver function tests and rare hepatotoxicity
OTHER ANTIFUNGALS
λFlucytosine
−Activated by fungal cytosine deaminase to 5-fluorouracil (5-FU), which after triphosphorylation is incorporated into fungal RNA
−5-FU also forms 5-fluorodeoxyuridine monophosphate (5-Fd-UMP), which inhibits thymidylate synthase → ↓ thymine.
−Resistance emerges rapidly if flucytosine is used alone.
−Use in combination with amphotericin B in severe candidal and cryptococcal infections—enters CSF
–Toxic to bone marrow (see Anticancer Drugs, Section IX).
λGriseofulvin
− Active only against dermatophytes (orally, not topically) by depositing in newly formed keratin and disrupting microtubule structure
− Side effects:
º Disulfiram-like reaction
λTerbinafine
− Active only against dermatophytes by inhibiting squalene epoxidase → ↓ ergosterol
− Possibly superior to griseofulvin in onychomycoses
–Side effects: GI distress, rash, headache, ↑ liver function tests → possible hepatotoxicity
λEchinocandins (caspofungin and other “fungins”)
− Inhibit the synthesis of beta-1,2 glucan, a critical component of fungal cell walls
− Back-up drugs given IV for disseminated and mucocutaneous Candida infections or invasive aspergillosis
− Monitor liver function
197
Section V λ Antimicrobial Agents
Chapter Summary
λIn eukaryotes, fungal metabolism is somewhat similar to that in humans. Thus, most bacterial antibiotics are ineffective, and many otherwise potentially effective drugs are also toxic to their human hosts. A difference between fungi and humans susceptible to exploitation by antibiotics is the high concentration of ergosterol in their membranes.
λThe polyenes amphotericin (amp B) are amphoteric compounds that bind to ergosterol, forming pores, which results in the leakage of intracellular contents. The activity, clinical uses, biodisposition, and side effects of these polyenes are discussed.
λThe azoles (ketoconazole, fluconazole, clotrimazole, miconazole, and itraconazole) kill fungi by interfering with ergosterol synthesis. The mechanisms of action, clinical uses, biodisposition, and side effects are considered.
λFlucytosine is activated by fungal cytosine deaminase to form 5-fluorouracil
(5-FU). It is sometimes used in combination with amp-B. Insomuch as 5-FU is a classic anticancer agent, it is not surprising that flucytosine is also toxic to bone marrow.
λGriseofulvin and terbinafine are active against dermatophytes. Griseofulvin interferes with microtubule function; terbinafine blocks ergosterol synthesis.
198
