
книга / 2016_Kaplan_USMLE_Step_1_Lecture_Notes_Pharmacology
.pdf
Chapter 1 λ Diuretics
Chapter Summary
λDiuretics are used to treat HTN, heart failure, edema, renal dysfunction, hypercalcemia, renal stones, glaucoma, and mountain sickness. In addition to their diuretic action, the loop and thiazide diuretics also cause vasodilation.
λFigure III-1-1 illustrates the water and ion exchange occurring in the various segments of a renal tubule and the site of action of the different classes of diuretics.
λThe positive and negative effects of IV mannitol, an osmotic diuretic, are discussed.
λCarbonic anhydrase inhibitors (e.g., acetazolamide) act in the proximal tubule to decrease absorption of Na+ and bicarbonate. The mechanisms involved are summarized in Figure III-1-2. The clinical uses and adverse affects are listed.
λLoop diuretics (e.g., furosemide) inhibit the Na+/K+/2Cl– cotransporter on the luminal membrane of the thick ascending loop. The mechanisms causing their diuretic actions (Figure III-1-3) and their clinical uses and adverse effects are discussed.
λThe thiazides (e.g., hydrochlorothiazide) inhibit the Na+/Cl– cotransporter on the luminal membrane of the distal convoluted tubule. The mechanisms leading to their diuretic actions (Figure III-1-4) and their clinical uses and adverse effects are discussed.
λSpironolactone, amiloride, and triamterene are K+-sparing, weak diuretics that act at the collecting tubule and duct level. The mechanisms leading to their diuretic actions (Figure III-1-5) and their clinical uses and adverse effects are discussed.
λTable III-1-1 summarizes the mechanisms of action, the urinary electrolyte patterns, and the resultant blood pH associated with administration of the various classes of diuretics.
89

Antihypertensives 2
Learning Objectives
Differentiate between angiotensin-converting enzyme inhibitors and angiotensin-receptor blockers
Explain drug strategy for treating hypertension using calcium-channel blockers, drugs altering sympathetic activity, and direct-acting vasodilators
Answer questions about indications for use of antihypertensive drugs
Describe modifications of hypertension treatment in comorbid conditions
Apply knowledge of treatment of pulmonary hypertension
DRUG STRATEGY
λ↓ TPR
λ↓ CO
λ↓ body fluid volume
λ↓ BP may result in homeostatic regulation:
–Reflex tachycardia (↑ sympathetic activity)
–Edema (↑ renin activity)
THIAZIDE DIURETICS (See Chapter 1)
Thiazide diuretics are commonly used in the management of hypertension.
Clinical Correlate
Current recommendations are to use thiazide diuretics, ACEIs, or long-acting
CCBs as first-line therapy. These drugs are considered equally effective.
91

Section III λ Cardiac and Renal Pharmacology
ANGIOTENSIN-CONVERTING ENZYME INHIBITORS (ACEIs)
AND ANGIOTENSIN-RECEPTOR BLOCKERS (ARBs)
|
Inhibited by aliskiren |
|
|
|
|
|||
Angiotensinogen |
|
|
renin (kidney) |
|
|
|
|
|
|
|
|
Angiotensin I |
Bradykinin |
||||
(from liver) |
|
|
|
|||||
|
|
|
||||||
|
|
|
|
|
Angiotensin- |
|
||
|
|
|
|
|
|
|
||
Blocked by |
|
|
|
|
|
converting |
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
enzyme |
|
|
|
ACE inhibitors |
|
|
|
|
|
(plasma) |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
Angiotensin II |
inactivation |
|||
AT-1 receptors |
|
|
Adrenal cortex |
|
Blood vessels |
|||
blocked by |
|
|
|
|||||
losartan |
|
|
|
|
AT-1 |
|
|
|
|
|
|
|
receptors |
|
|
||
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
Aldosterone |
|
Vasoconstriction |
|||
|
|
|
secretion |
|
|
|
|
|
|
|
|
Figure III-2-1. The Angiotensin System |
|
|
|||
λDrugs:
−ACEIs: captopril, lisinopril (and other “−prils”)
ºBlock formation of angiotensin II
ºResulting in prevention of AT1-receptor stimulation
º↓ aldosterone, vasodilation
ºACEIs prevent bradykinin degradation
−ARBs: losartan (and other “−sartans”)
ºBlock AT1 receptors
ºSame results as ACEIs on BP mechanisms
ºARBs do not interfere with bradykinin degradation
−Renin inhibitor: Aliskiren
ºBlocks formation of angiotensin I
ºSame results as ACEIs on BP mechanisms
ºAliskiren does not interfere with bradykinin degradation
λUses:
−Mild-to-moderate hypertension (all)
−Protective of diabetic nephropathy (ACEI/ARBs)
−CHF (ACEI/ARBs)
λSide effects:
−Dry cough (ACEIs)
−Hyperkalemia
−Acute renal failure in renal artery stenosis
−Angioedema
λContraindication: pregnancy
92

CALCIUM-CHANNEL BLOCKERS (CCBs)
λBlock L-type Ca2+ channels in heart and blood vessels
λResults in ↓ intracellular Ca2+
λCauses ↓ CO (verapamil and diltiazem), ↓ TPR (all CCBs)
λDrugs: verapamil, diltiazem, dihydropyridines (−“dipines,” prototype: nifedipine)
|
|
Ca2+-channel blockers |
|
|
|
Heart |
|
|
|
Blood vessel |
|
|
|
|
|
||
|
|
|
|
|
|
VERAPAMIL |
DILTIAZEM |
“—DIPINEs” |
|||
Figure III-2-2. Cardiac or Vascular Selectivity of
Major Ca2+-Channel Blockers
λUses:
−Hypertension (all drugs)
−Angina (all drugs)
−Antiarrhythmics (verapamil, diltiazem)
λSide effects:
−Reflex tachycardia (“−dipines”)
−Gingival hyperplasia (“−dipines”)
−Constipation (verapamil)
DRUGS ALTERING SYMPATHETIC ACTIVITY
λβ blockers
−Mechanism (See ANS section)
– Side effects:
ºCardiovascular depression
ºFatigue
ºSexual dysfunction
º↑ LDLs and TGs
−Cautions in use:
ºAsthma
ºVasospastic disorders
ºDiabetics (alteration of glycemia and masking of tachycardia due to hypoglycemic events)
λα1 blockers
−↓ arteriolar and venous resistance
−Reflex tachycardia
−Drugs: prazosin, doxazosin, terazosin
−Uses:
ºHypertension
ºBPH: ↓ urinary frequency and nocturia by ↓ the tone of urinary sphincters
Chapter 2 λ Antihypertensives
Bridge to Physiology
Vasodilators may have specificity.
λArteriolar: Ca2+-channel blockers, hydralazine, K+-channel openers
λVenular: nitrates
λBoth arteriolar and venular: “the rest”
Orthostatic (postural) hypotension results from venular dilation (not arteriolar) and mainly results from
α1 blockade or decreased sympathetic tone.
93

Section III λ Cardiac and Renal Pharmacology
−Side effects:
º“First-dose” syncope
ºOrthostatic hypotension
ºUrinary incontinence
−Advantage: good effect on lipid profile (↑ HDL, ↓ LDL)
λα2 agonists: clonidine and methyldopa (prodrug)
−α2 stimulation:
º↓ in sympathetic outflow
º↓ TPR but also ↓ HR
−Uses:
ºMild-to-moderate hypertension (both)
ºOpiate withdrawal (clonidine)
ºHypertensive management in pregnancy (methyldopa)
−Side effects:
ºPositive Coombs test (methyldopa)
ºCNS depression (both)
ºEdema (both)
–Drug interactions:
º Tricyclic antidepressants ↓ antihypertensive effects of α2 agonists
Clinical Correlate
Cyanide Poisoning
Sodium nitrite or amyl nitrite can be used in cyanide poisoning. It
promotes formation of methemoglobin (MetHb), which binds CN– ions, forming cyanomethemoglobin. This prevents the inhibitory action of CN– on complex IV of the electron transport chain. Cyanomethemoglobin is then reconverted to methemoglobin by treatment with sodium thiosulfate, forming the less toxic thiocyanate
ion (SCN–). MetHb is converted to oxyhemoglobin with methylene blue.
Clinical Correlate
A hypertensive emergency occurs when hypertension is severe enough to cause end-organ damage. Most commonly, nitroprusside, labetalol, or the D1 agonist fenoldopam is given intravenously as therapy.
DIRECT-ACTING VASODILATORS
Drugs Acting Through Nitric Oxide
λHydralazine
−↓ TPR via arteriolar dilation
−Use: moderate-to-severe hypertension
−Side effects:
ºSLE-like syndrome and slow acetylators
ºEdema
ºReflex tachycardia
λNitroprusside
−↓ TPR via dilation of both arterioles and venules
−Use: hypertensive emergencies (used IV)
−Side effect: cyanide toxicity (co-administered with nitrites and thiosulfate; see Clinical Correlate)
Drugs Acting to Open Potassium Channels
λDrugs: minoxidil and diazoxide
−Open K+ channel, causing hyperpolarization of smooth muscle
−Results in arteriolar vasodilation
−Uses:
ºInsolinoma (diazoxide)
ºSevere hypertension (minoxidil)
ºBaldness (topical minoxidil)
94
−Side effects:
ºHypertrichosis (minoxidil)
ºHyperglycemia (↓ insulin release [diazoxide])
ºEdema
ºReflex tachycardia
INDICATIONS FOR USE OF ANTIHYPERTENSIVE DRUGS IN COMORBID CONDITIONS
Table III-2-1. Use of Antihypertensive Drugs in Comorbid Conditions
Indication |
|
Suitable Drug(s) |
Angina |
|
Beta blockers, CCBs |
Diabetes |
|
ACEIs, ARBs |
Heart failure |
|
ACEIs, ARBs, beta blockers |
Post-MI |
|
Beta blockers |
BPH |
|
Alpha blockers |
Dyslipidemias |
|
Alpha blockers, CCBs, ACEIs/ARBs |
Chronic kidney disease |
|
ACEI, ARBs |
TREATMENT OF PULMONARY HYPERTENSION
λBosentan
−Endothelin (ET)-1 is a powerful vasoconstrictor through ET-A and -B receptors
−Bosentan is an ETA receptor antagonist
−Administered orally
−Side effects are associated with vasodilation (headache, flushing, hypotension, etc.)
−Contraindication: pregnancy
λProstacyclin (PGI2): epoprostenol
−Administered via infusion pumps
λSildenafil
– Inhibits type V PDE
– ↑ cGMP
– Pulmonary artery relaxation
– ↓ pulmonary hypertension
Chapter 2 λ Antihypertensives
Clinical Correlate
Chronic (preexisting) hypertension in pregnancy is often treated with methyldopa or labetalol, while
preeclampsia (new-onset hypertension in pregnancy) is treated with labetalol or hydralazine.
95

Section III λ Cardiac and Renal Pharmacology
Chapter Summary
λHypertension (HTN) is a major risk factor for stroke, heart failure, renal disease, peripheral vascular disease, and coronary artery disease. Factors inducing HTN include decreased vagal tone, increased sympathetic tone, increased renin-angiotensin activity, and excess water retention.
λTreatments for HTN aim to reduce sympathetic tone and blood volume and/ or relax vascular smooth muscle. However, homeostatic mechanisms may lead to compensatory increases in heart rate and/or salt and water retention.
λThe metabolic characteristics, clinical uses, and potential adverse effects of various hypertensives are discussed. Examples of each class are provided.
λThiazide diuretics are used to treat HTN. The diuretics are discussed in more detail elsewhere.
λDrugs that act via the renin-angiotensin system are the angiotensinconverting enzyme (ACE) inhibitors (e.g., captopril) and the angiotensin-II (AT-1) blockers (ARBs; e.g., losartan). Figure III-2-1 illustrates the angiotensin system and the pharmacologic effects of these drugs. Their clinical uses and adverse affects are discussed.
λCalcium channel blockers (CCBs) enhance vasodilation by blocking L-type Ca2+ channels in cardiac and vascular tissues. Drugs considered are verapamil, diltiazem, and dihydropyriodines.
λBeta blockers, alpha-1 blockers, and alpha-2 agonists alter sympathetic tone to lower blood pressure.
λDirect-acting vasodilators lower the peripheral vascular resistance mainly by causing arteriolar dilation. Drugs discussed are nitroprusside, hydralazine, minoxidil, and diazoxide.
λTable III-2-1 summarizes the use of antihypertensives in comorbid conditions.
λBosentan, epoprostenol, and sildenafil are used in pulmonary hypertension.
96

Drugs for Heart Failure |
3 |
Learning Objectives
Describe the primary treatments for CHF
Demonstrate understanding of inotropes
Demonstrate understanding of other drugs used in CHF
|
|
|
|
|
|
|
|
|
|
|
|
|
Failing Heart = |
|
CO |
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
Compensation |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
Strength of |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
contraction |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
Decompensation |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
Strength of |
|
|
|
|
|
Contractility |
|
||||||||||||||||||||||||||||
Dilated heart |
|
|
|
|
|||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
contraction |
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
|
Starlings compensation |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
End diastolic |
|
|
|
|
|
End systolic |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Sympathetic |
|
|||||||||||||||||||
|
|
|
|
|
|
CO* |
|
|
|
|
BP |
|
|
|
|
||||||||||||||||||||||||||
volume |
|
|
|
|
|
|
volume |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
activity |
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
HR |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Venous |
|
|
|
|
Renal |
|
|
|
|
|
|
||||||||||||||
Preload |
|
|
|
|
|
BP |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
pressure |
|
|
|
blood flow |
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Vasoconstriction |
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Renin |
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Capillary |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
filtration |
|
|
|
|
|
|
|
|
|
|
|
|
|
Afterload |
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Angiotensin II |
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Pulmonary |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Aldosterone |
|
|
|
|
|
|
|
|||||||||||||
congestion |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Blood |
|
|
|
|
|
|
|
|
|
|
|
|
|
Sodium |
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
volume |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
retention |
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
* = starting point |
|
|
|
|
|
|
|
|
|
Edema |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
Figure III-3-1. The Failing Heart
Clinical Correlate
Left systolic dysfunction secondary to coronary artery disease is the most common cause of heart failure.
97
Section III λ Cardiac and Renal Pharmacology
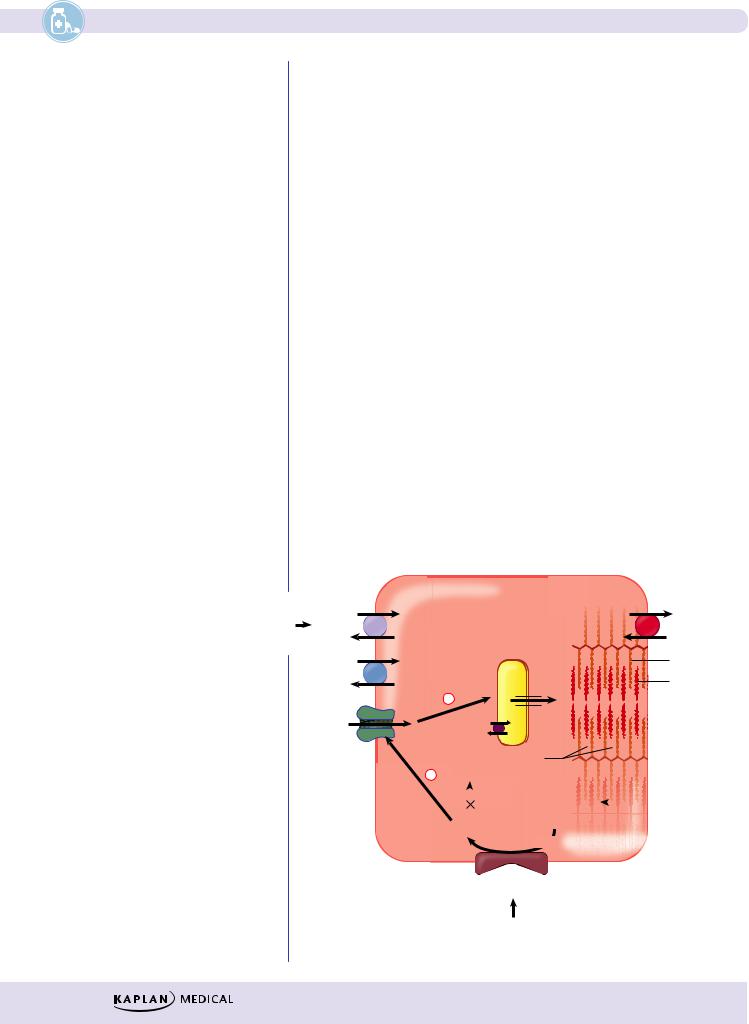
Pharmacotherapy aimed at:
λ↓ preload: diuretics, ACEIs, ARBs, and venodilators
λ↓ afterload: ACEIs, ARBs, and arteriodilators
λ↑ contractility: digoxin, beta agonists, PDE III inhibitors
λ↓ remodeling of cardiac muscle: ACEIs, ARBs, spironolactone, beta blockers
Whereas digoxin does not improve survival, ACEIs, ARBs, beta blockers, and spironolactone have been proven beneficial in CHF. ACEIs and ARBs are currently drugs of choice for the chronic management of CHF. Inotropes are more beneficial in management of acute CHF.
PRIMARY TREATMENTS FOR CHF
λACEI (ARB as an alternative)
λBeta blockers (metoprolol, bisoprolol, carvedilol)
−Provide antiarrhythmic effect and also ↓ remodeling
λDiuretics
−Loop or thiazide diuretics to decrease preload
−Spironolactone or eplerenone to block aldosterone receptors and ↓ remodeling (used in advanced CHF)
λHydralazine + isosorbide dinitrate
−Preferred for chronic therapy in patients who cannot tolerate an ACEI or ARB
|
INOTROPES |
|
|
|
|
|
|
CARDIAC CELL |
H+ |
DIGOXIN |
2 K+ |
|
Sarcoplasmic |
|
3 Na+ |
|
Na+ |
||
|
3 Na+ |
|
reticulum |
Actin |
|
|
|
||
|
Ca2+ |
+ |
Ca2+ |
Myosin |
|
|
Ca2+ |
|
|
|
Ca2+ |
|
|
|
|
channel |
|
2H+ |
|
|
+ |
|
|
Troponin/ |
|
|
|
via |
AMP |
tropomyosin |
|
|
|||
protein |
|
|
|
Phosphodiesterase |
|
INAMRINONE, |
|
kinase A |
|
|
|
||||
|
|
|
|||||
|
|
|
|||||
|
|
|
ATP |
|
MILRINONE |
||
activation |
|
|
|
|
|||
cAMP |
|||||||
|
|
|
Adenylyl |
cyclase (via Gs protein) |
|||
β1 receptor
DOBUTAMINE
Figure III-3-2. Mechanism of Action of Inotropes
98
