
книга / 2016_Kaplan_USMLE_Step_1_Lecture_Notes_Pharmacology
.pdf
Antiviral Agents |
3 |
Learning Objectives
Answer questions about anti-herpetics and other antiviral agents
Describe the appropriate treatment of HIV
Solve problems concerning fusion inhibitors
Many antiviral drugs are antimetabolites that resemble the structure of naturally occurring purine and pyrimidine bases or their nucleoside forms. Antimetabolites are usually prodrugs requiring metabolic activation by host-cell or viral enzymes—commonly, such bioactivation involves phosphorylation reactions catalyzed by kinases.
λ Site of action:
Viral |
Enfuvirtide |
|
|
|
|||||
adsorption |
Maraviroc |
Amantadine |
|||||||
|
Penetration |
|
|
|
|||||
|
|
|
|
Uncoating |
|
|
|
||
Viral |
|
|
|
|
|
|
|
|
Polymerase |
|
|
|
Nucleic acid |
|
|
||||
release |
|
HOST |
|
synthesis |
|
|
inhibitors |
||
|
|
CELL |
|
|
|
|
|
Reverse |
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
transcriptase |
|
|
|
|
|
|
Protein |
|
|||
|
Viral |
|
|
|
|
inhibitors |
|||
Neuraminidase |
|
|
synthesis |
|
|
|
|||
assembly |
|
|
|
|
|||||
inhibitors |
and processing |
||||||||
Protease inhibitors
Figure V-3-1. Sites of Antiviral Drug Actions
199

Section V λ Antimicrobial Agents
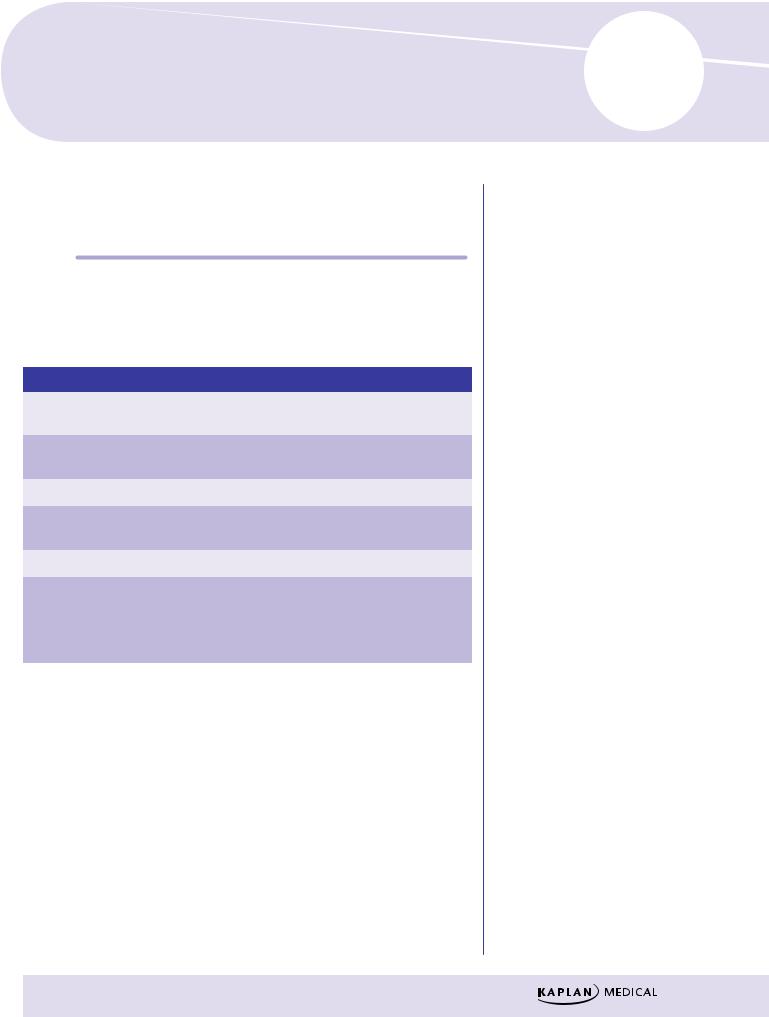
Table V-3-1. Mechanism of Action of Antiviral Drugs
Mechanism of Action |
|
Major Drugs |
Block viral penetration/uncoating |
|
Amantadine, enfuvirtide, maraviroc |
Inhibit viral DNA polymerases |
|
Acyclovir, foscarnet, ganciclovir |
Inhibit viral RNA polymerases |
|
Foscarnet, ribavirin |
Inhibit viral reverse transcriptase |
|
Zidovudine, didanosine, zalcitabine, |
|
|
lamivudine, stavudine, nevirapine, |
|
|
efavirenz |
Inhibit viral aspartate protease |
|
Indinavir, ritonavir, saquinavir, nelfinavir |
Inhibit viral neuraminidase |
|
Zanamivir, oseltamivir |
ANTIHERPETICS
Acyclovir
λMechanisms of action:
–Monophosphorylated by viral thymidine kinase (TK), then further bioactivated by host-cell kinases to the triphosphate
–Acyclovir-triphosphate is both a substrate for and inhibitor of viral DNA polymerase
–When incorporated into the DNA molecule, acts as a chain terminator because it lacks the equivalent of a ribosyl 3′ hydroxyl group
–Resistance possibly due to changes in DNA polymerase or to decreased activity of TK
–>50% of HSV strains resistant to acyclovir completely lack thymidine kinase (TK– strains)
NNRTIs |
|
– |
DNA Polymerase (DNAor RNA-directed) |
|||||||||||
|
|
|
||||||||||||
Foscarnet |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
Host |
|
|
|
|
|
– |
|
|
|||
|
|
|
kinases |
|
|
|
|
|
Lacks |
|
Chain |
|||
|
Drug |
|
|
|
Drug |
|
|
|||||||
|
|
|
|
|
|
|
|
|
3’– OH |
|
termination |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|||
(inactive) |
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
P P |
P |
|
|
|||||||
|
“ovirs” |
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
NRTIs |
|
Viral- |
|
specific |
|
|
|||||||
|
|
|
|
|
|
|
||||||||
|
|
|
kinase (herpes) |
|
|
|||||||||
Figure V-3-2. Common Mechanism for “ovirs” and NRTIs
λActivity and clinical uses:
−Activity includes herpes simplex virus (HSV) and varicella-zoster virus (VZV)
−There are topical, oral, and IV forms; has a short half-life
200
Chapter 3 λ Antiviral Agents
−Reduces viral shedding in genital herpes; ↓ acute neuritis in shingles but has no effect on postherpetic neuralgia
−Reduces symptoms if used early in chickenpox; prophylactic in immunocompromised patients
λSide effects:
−Minor with oral use, more obvious with IV
−Crystalluria (maintain full hydration) and neurotoxicity (agitation, headache, confusion—seizures in OD)
−Is not hematotoxic
λNewer drugs—famciclovir and valacyclovir are approved for HSV infec-
tion and are similar to acyclovir in mechanism. They may have activity against strains resistant to acyclovir, but not TK– strains. They have a longer t1/2 than acyclovir.
Ganciclovir
λMechanisms of action:
−Similar to that of acyclovir
−First phosphorylation step is viral-specific; involves thymidine kinase in HSV and a phosphotransferase (UL97) in cytomegalovirus (CMV)
−Triphosphate form inhibits viral DNA polymerase and causes chain termination
−Resistance mechanisms similar to acyclovir
λActivity and clinical uses:
−HSV, VZV, and CMV
−Mostly used in prophylaxis and treatment of CMV infections, including retinitis, in AIDS and transplant patients—relapses and retinal detachment occur
λSide effects:
−Dose-limiting hematotoxicity (leukopenia, thrombocytopenia), mucositis, fever, rash, and crystalluria (maintain hydration)
−Seizures in overdose
Foscarnet
λMechanisms and clinical uses:
–Not an antimetabolite, but still inhibits viral DNA and RNA polymerases
–Uses identical to ganciclovir, plus > activity versus acyclovir-resistant strains of HSV
λSide effects:
–Dose-limiting nephrotoxicity with acute tubular necrosis, electrolyte imbalance with hypocalcemia (tremors and seizures)
–Avoid pentamidine IV (→↑ nephrotoxicity and hypocalcemia)
201




Chapter 3 λ Antiviral Agents
Chapter Summary
General Principles
λAntiviral drugs are often antimetabolites that are structural analogs of purine or pyrimidine bases or their nucleoside forms. Many are prodrugs to be activated by host or viral enzymes. The steps in viral replication and the main sites of action of such antiviral drugs are illustrated in Figure V-3-1.
λTable V-3-1 summarizes the mechanisms of action of the major antiviral drugs.
Antiherpetics
λThe antiherpes drugs include acyclovir, ganciclovir, and foscarnet. Famciclovir and valacyclovir are newer drugs very similar to acyclovir. All inhibit viral DNA polymerase. Acyclovir and ganciclovir do so by first being phosphorylated by viral enzymes. As well as acting as a polymerase inhibitor, acyclovir triphosphate is incorporated into the viral DNA, where it acts as a chain terminator. The mechanisms of action, activities, clinical uses, and adverse effects are discussed.
Reverse Transcriptase Inhibitors
λNucleoside reverse transcriptase inhibitors (NRTIs) are used in most drug regimes to treat HIV infections. Commonly two NRTIs are used together with a protease inhibitor.
λThe mechanisms, biodisposition, and adverse effects associated with zidovudine (AZT) use are described. The other nucleotide RTIs act almost identically. The NRTIs and their adverse effects are summarized in Table V-3-2.
λNonnucleoside inhibitors of reverse transcriptase (NNRTIs) and a nucleotide RTI are also used in combinations for treatment in an HIV-positive patient.
Protease Inhibitors (PIs)
λHIV aspartate protease has a unique dipeptide structure that has been used as a target for protease inhibitory drugs.
λRitonavir is the most commonly used protease inhibitor. Adverse effects of this group are discussed.
Fusion Inhibitors
λ Enfuvirtide and maraviroc block the entry of HIV into cells.
Integrase Inhibitors
λRaltegravir inhibits HIV integrase and prevents integration of the viral genome into host DNA.
(Continued )
205

Section V λ Antimicrobial Agents
Chapter Summary (cont’d )
Other Antivirals
λZanamivir and oseltamivir inhibit influenza viruses A and B neuraminidase, promoting viral clumping and decreasing the chance of penetration. Ribavirin becomes phosphorylated and inhibits IMP dehydrogenase and RNA polymerase. It is used to treat respiratory syncytial virus, influenza A and B,
Lassa fever, Hantavirus, and as an adjunct to alpha-interferons in hepatitis C. The mechanisms, clinical uses, and side effects of these drugs are considered. Hepatitis C therapies are rapidly changing, however. Sofosbuvir is popular in many regimens while simepravir is also being used.
206
Antiprotozoal Agents |
4 |
Learning Objectives
Demonstrate understanding of drugs for malaria and helminthic infections
OVERVIEW
Table V-4-1. Major Protozoal Infections and the Drugs of Choice
Infection |
|
Drug of Choice |
|
Comments |
Amebiasis |
|
Metronidazole |
|
Diloxanide for noninvasive intestinal |
|
|
|
|
amebiasis |
Giardiasis |
|
Metronidazole |
|
“Backpacker’s diarrhea” from con- |
|
|
|
|
taminated water or food |
Trichomoniasis |
|
Metronidazole |
|
Treat both partners |
Toxoplasmosis |
|
Pyrimethamine + |
|
|
|
|
sulfadiazine |
|
|
Leishmaniasis |
|
Stibogluconate |
|
|
Trypanosomiasis |
|
Nifurtimox |
|
|
|
|
(Chagas disease) |
|
|
|
|
Arsenicals |
|
|
|
|
(African) |
|
|
ANTIMALARIAL DRUGS
λClinical uses:
−Chloroquine-sensitive regions
ºProphylaxis: chloroquine +/– primaquine
ºBackup drugs: hydroxychloroquine, primaquine, pyrimethaminesulfadoxine
207

Section V λ Antimicrobial Agents
λ Specific treatment:
Table V-4-2. Treatment of Chloroquine-Sensitive Malaria
P. falciparum |
Chloroquine |
P. malariae |
Chloroquine |
P. vivax |
Chloroquine + primaquine |
P. ovale |
Chloroquine + primaquine |
−Chloroquine-resistant regions
ºProphylaxis: mefloquine; backup drugs: doxycycline, atovaquoneproguanil
ºTreatment: quinine +/– either doxycycline or clindamycin or pyrimethamine
λSide effects:
−Hemolytic anemia in G6PD deficiency (primaquine, quinine)
−Cinchonism (quinine)
DRUGS FOR HELMINTHIC INFECTIONS
λMost intestinal nematodes (worms)
−Albendazole (↓ glucose uptake and ↓ microtubular structure)
−Pyrantel pamoate (NM agonist → spastic paralysis)
λMost cestodes (tapeworms) and trematodes (flukes)
−Praziquantel (↑ Ca2+ influx, ↑ vacuolization)
Chapter Summary
λTable V-4-1 lists the major types of protozoal infections and the drugs of choice for their treatment, with various relevant comments.
λTable V-4-2 lists the drugs of choice used against the various forms of malaria, and information is given about treatment and prophylaxis of malaria. Chloroquine-sensitive or -resistant areas are listed separately.
λThe drugs used to treat helminthic infections are listed, and their mechanisms of action are noted.
208
