
The Treatment of Stroke
.pdf
The Treatment of Stroke:
Specific Management – Thrombolysis Plus
Prof. Nils Wahlgren
The Treatment of Stroke:
Specific Management – Thrombolysis Plus
Professor Nils Wahlgren, M.D., Ph.D.
Dept of Neurology, Karolinska University Hospital,
Stockholm, Sweden |
1 |
|
Global stroke burden
Annual stroke incidence |
15,000,000 |
Occlusive (ischemic) strokes (87%) |
13,000,000 |
Thrombo-embolic large artery (63%) |
9,500,000 |
WHO: http://www.who.int/cardiovascular_diseases/en/cvd_atlas_15_burden_stroke.pdf
Stroke Brain Attack Reporter’s Handbook,Englewoos, Colo, National Stroke Association, 1997c2
ThromboembolicBloodflow fromlargeadjacentrebarterialarteryterritorieocclusion |
|
with correscompoendingsatebloodpartlyflowt ther ductilossofnbloodwithinflowits territory |
|
maythroughoccurcollateralfor minutesarteriesor aoverfew theourscortexwithofnlythelimitedbrain |
|
ischemic damage |
|
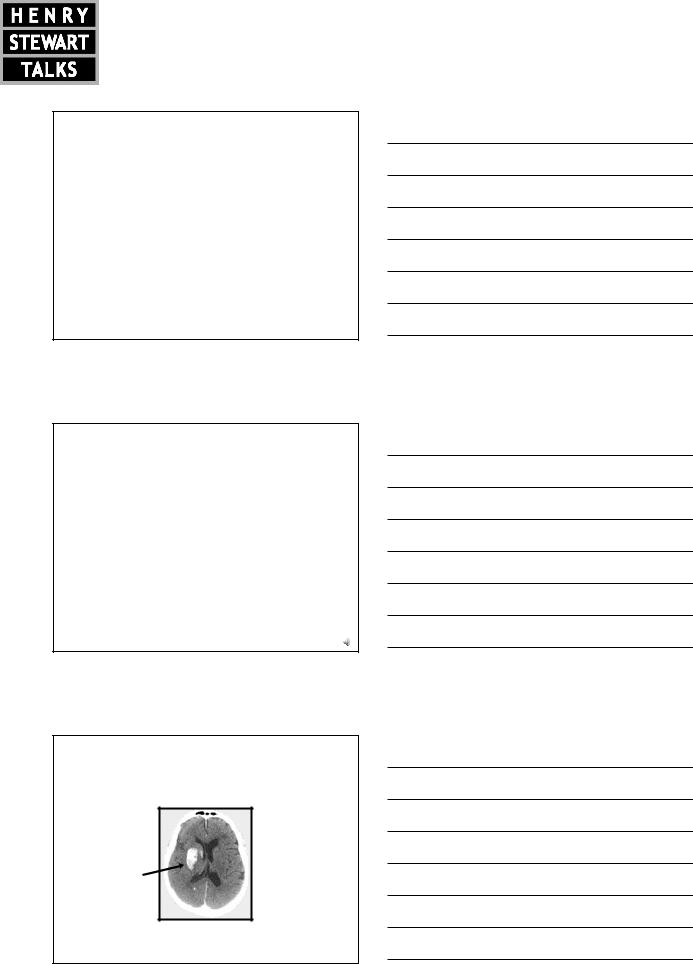
Illustrated by 62year old woman 2h after onset of left-sided hemiparesis, |
|
neglect, NIHSS 10, CT showing MCA occlusion, perfusion deficit |
3 |
The screen versions of these slides have full details of copyright and acknowledgements |
1 |

The Treatment of Stroke:
Specific Management – Thrombolysis Plus
Prof. Nils Wahlgren
Possible interventions |
|||
|
|
• |
Increase O2 transport capacity |
ml/100g |
|
• |
Increase perfusion pressure |
|
|
|
|
/min |
|
• |
Modify genetic regulation |
|
|
||
50 |
|
|
of neovascularisation |
|
|
|
|
40 |
O2 |
• |
Neuroprotection of vulnerable |
|
|
|
neurons subjected |
30 |
|
|
to delayed injury |
20 |
|
|
|
10 |
|
|
|
|
|
|
4 |
ml/100g |
||
/min |
Hyperpolarise (GABA agonists) |
|
50 |
||
X |
||
|
Block voltage-operated calcium channels |
|
40 |
X |
|
|
(nimodipine) |
|
|
Excitatory |
|
30 |
Block calcium flow regulating receptorsattack |
|
|
X |
|
|
(NMDA antagonists) |
|
|
• Depolarisation ofmembranes |
|
20 |
• Calcium flow through |
|
|
Block sodium flow regulating receptors |
|
|
X |
|
|
– V ltage operated channels |
|
|
(AMPA antagonists) |
|
|
– Receptor operated channels |
|
10 |
Block free radicals (scavengers, NXY 059) |
|
|
||
|
X |
|
|
Neurological symptoms |
|
|
Penumbra |
|
|
Irreversible ischemic injury |
|
|
5 |
|
Recanalisation is associated with clinical improvement (same patient as above)
A |
|
|
|
National Institute of Health |
|
|
|
stroke score (NIHSS) |
|
|
|
|
|
Before intravenous |
|
|
|
|
Thrombolysis: |
|
|
|
|
NIHSS score: 10 |
|
|
|
|
After thrombolysis: |
|
|
|
|
|
|
|
|
|
NIHSS: 1 |
B |
|
|
|
(NIHSS score 0 |
|
|
|
|
|
|
|
|
|
represents a normal score) |
6
The screen versions of these slides have full details of copyright and acknowledgements |
2 |
The Treatment of Stroke:
Specific Management – Thrombolysis Plus
Prof. Nils Wahlgren
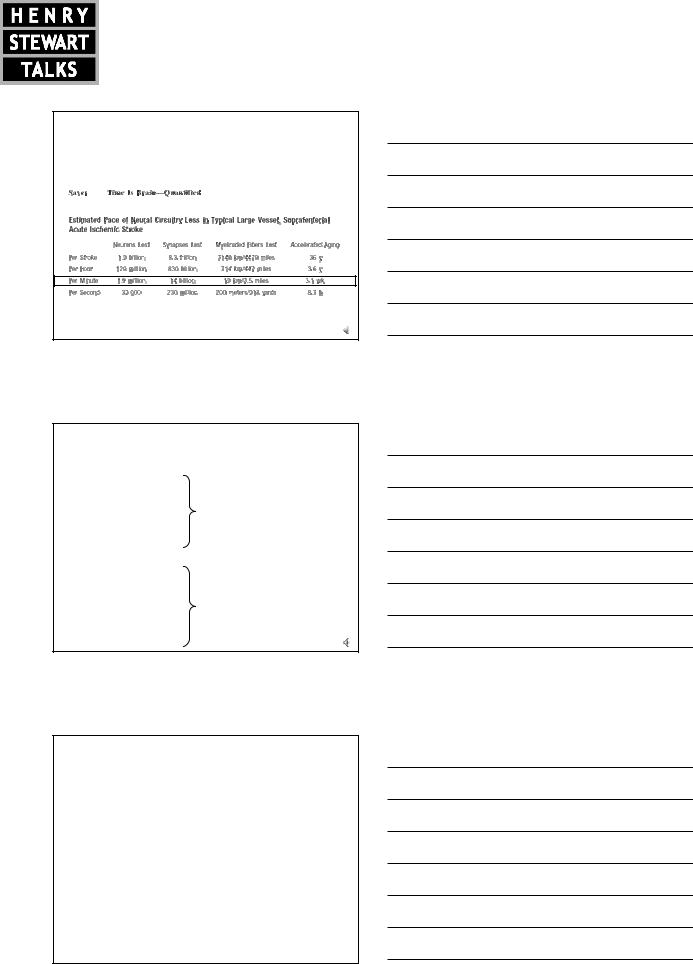
Time is brain –
the delay between occlusion and recanalisation is of critical importance for recovery
Saver J, Stroke 2006; 37(1):263-6 |
7 |
|
Where do thromboembolic occlusions originate?
|
Embolic material |
|
Arterial origin |
Erythrocytefibrin clots |
|
|
|
|
• Local thrombus |
Platelet-fibrin clots |
|
• Artery-to-artery |
Cholesterol crystals |
|
embolism |
Calcified particles |
|
|
Disrupted plaques |
|
|
Erythrocytefibrin clots |
|
|
Platelet-fibrin clots |
|
Cardiac origin |
Cholesterol crystals |
|
|
|
|
• Cardiac embolism |
Calcified particles |
|
|
|
|
|
Bacteria |
|
|
Myxomatous tumours |
8 |
How can recanalisation be achieved?
•Spontaneous
•Pharmacological – intravenous thrombolysis
•Pharmacological – intraarterial thrombolysis
•Mechanical – thrombectomy
•Sonothrombolysis – by ultrasound
9
The screen versions of these slides have full details of copyright and acknowledgements |
3 |
The Treatment of Stroke:
Specific Management – Thrombolysis Plus
Prof. Nils Wahlgren
Pharmacological treatment
Evaluated in randomised controlled trials
Streptokinase
Ancrod
Recombinant tissue plasminog en activator (rtPA)
•Alteplase
•Duteplase
Desmoteplase
Supported by randomised controlled trials
Alteplase 0.9 mg/kg
(max 90 mg) given as intravenous infusion for 1h, 10% as bolus
Currently approved in many countries, including US and European Union for treatment
of ischaemic stroke within 3 hours of symptoms onset in patients 80 years or young er
10
Pharmacological treatment
StudiesTrials withof implementationalteplase of I.V. alteplase in clinical practice
CanadianNINDS rt-PAAlteplasestudy groupforStroke1995Effectiveness Study (CASES) 2005 SafeEuropeanImplementationCo-operativeof AcuteThrombolysisStroke StudyinStroke(ECASS)Monitoring1995Study
(SITS-MOST) 2007 ECASS II 1998
ATLANTIS 1999
ATLANTIS II 2000
Statistical overviews
Cochrane database systematic review 2003
Pooled ATLANTIS, NINDS and ECASS studies 2004
11
The approvalwas based on results from randomised controlled trials of tPA w ithin 3h of stroke onset
in about 1000 patients
RCT placebo
RCT active rt-PA
10% increase of proportion of ADL independent
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mRS0 |
|
13 |
16 |
11 |
14 |
20 |
|
7 |
|
18 |
|
|
mRS1 |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mRS2 |
|
|
|
|
|
|
+10% |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mRS3 |
|
20 |
|
|
22 |
8 |
|
14 |
12 |
7 |
|
18 |
|
|
mRS4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mRS5 |
0% |
20% |
40% |
|
|
60% |
|
80% |
100% |
mRS6 |
|||||
|
Recovered |
|
|
|
|
|
|
Dead |
|
|||||
Red colours: ADL-independent
Blue colours: ADL-dependent Black colour: Dead
12
The screen versions of these slides have full details of copyright and acknowledgements |
4 |

The Treatment of Stroke:
Specific Management – Thrombolysis Plus
Prof. Nils Wahlgren
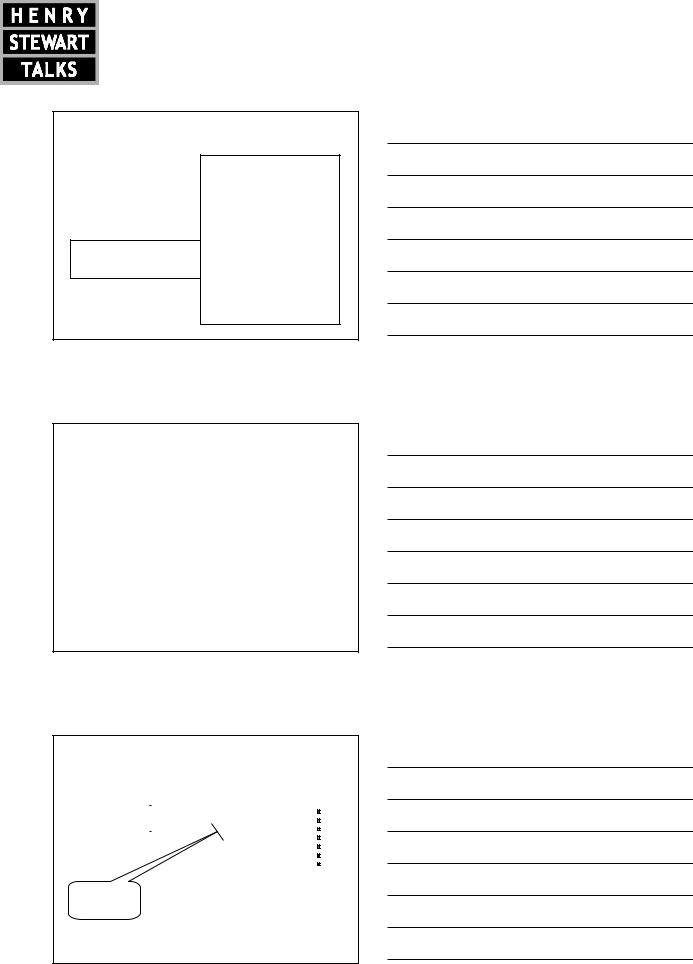
Pooled analysis of all randomised trials: benefit of intravenous thrombolysis decreasedw ith time
betw een stroke onset and start of treatment
|
Usually approved < 3h; |
ECASS3 |
|
||
Thrombolysis better |
SITS-MOST population |
randomised trial |
Regression line |
|
|
|
|
|
|
95% |
Confidence limit |
|
|
|
Control better |
|
|
|
||
Hacke W etal., Lancet 2004,363:768-774
Other trials (E.G. IST-3)
13
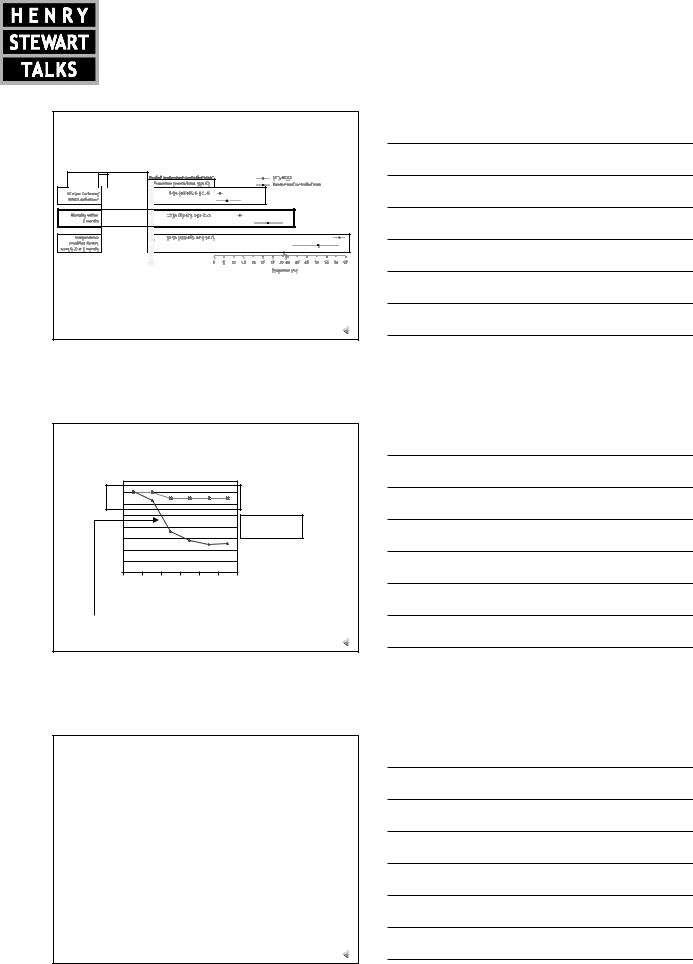
SITS-MOST indicated that the proportion of patients being ADLindependent at three months increased with an additional 3.4% compared to RCT active arm
RCT placebo
+10%
RCT active rt-PA
+3.4%
SITS-MOST
|
Recovered |
Dead |
Further 3.4% |
|
|
increase of |
Red colours: ADL-independent |
|
proportion of ADL |
Blue colours: ADL-dependent |
|
independent |
|
|
|
Black colour: Dead |
|
Wahlgren N et al., Lancet 2007, 369:275-282 |
14 |
|
The main conclusion was that intravenous thrombolysis is safe and effective in routine clinical use
15
The screen versions of these slides have full details of copyright and acknowledgements |
5 |
The Treatment of Stroke:
Specific Management – Thrombolysis Plus
Prof. Nils Wahlgren
AfterSITSadjustment-MOSTforunivariatedifferences inanalysisprognosticallyresultsimportant
baseline variables, the outcomes were almost identical
SITS-MOST
Adjusted proportions (%,95%CI)
9.1%(8.5-9.8)
15.3 (14.6-16.1)
50.3 (49.5-51.1)
SITS main outcomes, SICH, mortality and ADL-independence were compared with RCT;
Trends to better outcome for SITS, but onlysig nificantly for mortality
Lancet2007; 369:275-83 |
16 |
Median door to needle time in SITS thrombolysis register;
Effect of change of local routine
Minutes |
80 |
|
|
|
|
|
|
|
N=18,862 |
|||
|
70 |
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
60 |
|
|
|
|
|
|
|
|
|
|
|
|
50 |
|
|
|
|
|
|
|
|
|
|
|
|
40 |
|
|
|
|
|
|
|
N=782 |
|||
|
|
|
|
|
|
|
|
|
||||
|
30 |
|
|
|
|
|
|
|
|
|
|
|
|
20 |
|
|
|
|
|
|
|
|
|
|
|
|
10 |
|
|
|
|
|
|
|
|
|
|
|
|
0 |
|
|
|
|
|
|
|
|
|
|
|
|
|
03 |
|
04 |
|
05 |
|
06 |
|
07 |
|
08 |
|
0 |
0 |
0 |
0 |
0 |
0 |
||||||
|
2 |
|
2 |
|
2 |
|
2 |
|
2 |
|
2 |
|

 SITS average
SITS average  One center*
One center*
|
|
CT scan moved to emergency department |
|
|
neurologist available 24/7 at emergency |
|
|
rt-PA bolus given in radiologydept |
* HELSINKI, FINLAND |
immediately after CT scan, and followed byinfusion 17 |
|
Treatment indications for intravenous rt-PA
Indicatio ns
Ischemic stroke
within 3h of symptoms onset
Age 80 years or younger
Contrain dication s
Haemorrhag e on baseline CT/MR
Ong oing anticoagulation treatment
Blood pressure > 185/110
Recent (<3 months) stroke
Previous stroke
(with remaining symptoms) and diabetes mellitus requiring treatment
Verysevere stroke (NIHSS>25)
Blood glucose <50 mg /dl or >400 mg/dl
Recent haemorrhag e,
external heart massag e, or surgery
(study details before treatment) |
18 |
|
The screen versions of these slides have full details of copyright and acknowledgements |
6 |
The Treatment of Stroke:
Specific Management – Thrombolysis Plus
Prof. Nils Wahlgren
Comments on usual misunderstandings
•Seizure is not a contraindication if the neurological deficit is related to acute cerebral ischemia
•Dissection is not a contraindication to thrombolysis
•Some degree of neurological improvement during preparations for intravenous rt-PA is not a reason for interruption
of treatment
•There is usually no reason to wait for laboratory test results unless suspicions of pathological finding
19
Treatment recommendations beyond European labelling
”I.v. rtPA may be of benefit also for acute ischemic stroke beyond 3 hours after onset but is not recommended
for routine clinical practice. The use of multimodal imaging criteria may be useful for patient selection”
”It is recommended that intravenous rtPA may also be administered in selected patients over 80 years of age, although this is outside the current European labelling”
Ringleb P et al.,In press in Cerebrovasc Dis |
20 |
The condition to monitor all patients treated was driven by concern for haemorrhagic complications in routine clinical practice
Haemorrhage following thrombolysis
21
The screen versions of these slides have full details of copyright and acknowledgements |
7 |
The Treatment of Stroke:
Specific Management – Thrombolysis Plus
Prof. Nils Wahlgren
Multivariable analysis:
risk factors for symptomatic intracerebral haemorrhage (SITS-MOST definition) follow ing thrombolysis
SICH by SITS-MOST
OR and 95% CI
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
a b le |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
e n c e |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
V a r i |
|
|
|
|
|
|
|
|
|
|
|
|
R e f e r |
||
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
0-7
0-7
No
0-7
0.51.0 2.0 3.5 6.0
Odds ratio |
22 |
Risk factors for symptomatic intracerebral haemorrhage (SITS-MOST definition) following thrombolysis
•Maintain blood pressure below 180/100 mm Hg
during the whole infusion and after, continuous monitoring throughout first 24h
•Consider if treatment should be avoided in case
of combinations of risk factors, for example very severe neurological deficit at baseline in older patients on aspirin and with high blood sugar
23
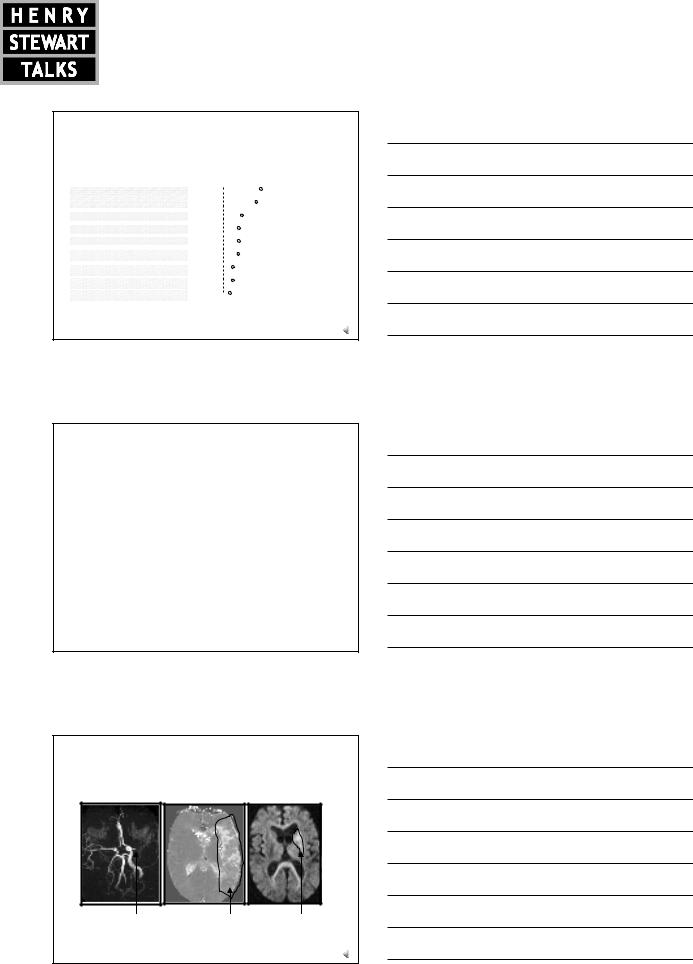
IsIf thereinfarctanisindicationconsiderablyforsmallerrecanalisationthan the are
with reduced blood flow, intravenous and/or intraarterial intervention beyond 3 hours intervention could still be considered
(MR imaging 4h after stroke onset)?
|
Occlusion right |
|
Reduced blood flow |
Small infarct |
|
|
middle cerebral |
|
|
||
|
|
in MCA territory |
within MCA territory |
|
|
|
artery (MCA) |
|
|
||
|
|
|
|
|
|
|
|
|
|||
|
Magnetic Resonance Tomography (MRT), Angiography, Mean Transit Time, |
24 |
|||
|
Diffusion Weighted Imaging; Holtås S, Karolinska Stroke Update 2000 |
||||
The screen versions of these slides have full details of copyright and acknowledgements |
8 |
The Treatment of Stroke:
Specific Management – Thrombolysis Plus
Prof. Nils Wahlgren
Is there a need for additional recanalisation strategies beyond intravenous thrombolysis?
•Are large artery stenoses, as for example those appearing as hyperdense middle cerebral artery signs (HMCAS) on CT scans, responding to intravenous thrombolysis?
25
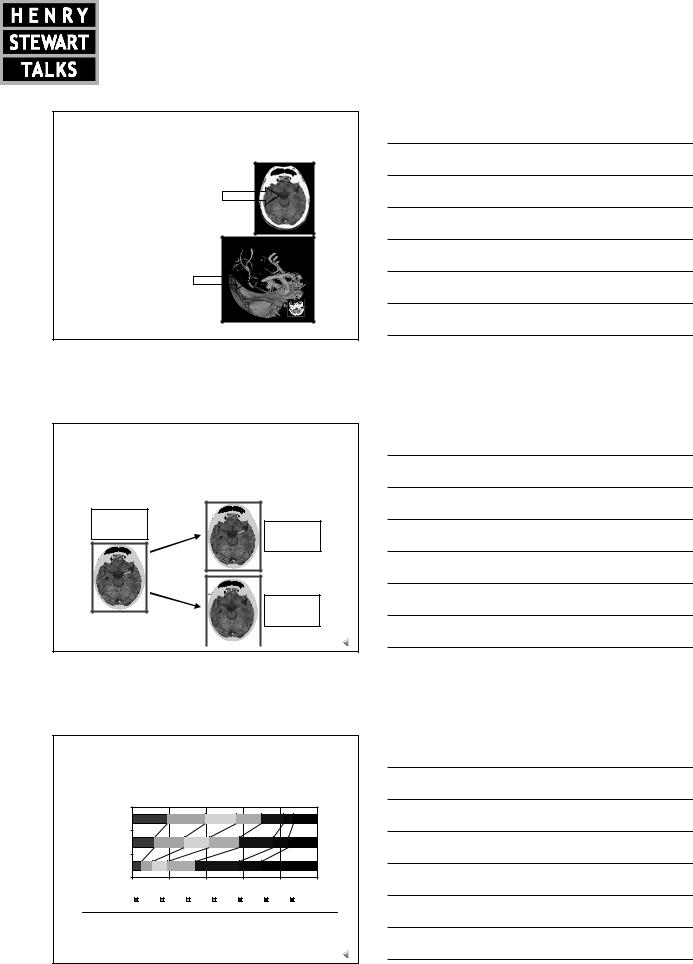
Results from SITS – rate of disappearance of HMCAS after I.V. thrombolysis
CT 1 |
CT 2 |
HMCAS
1905 HMCAS-P Persistent
788 (45%)
HMCAS-D Disappeared 831 (48%)
Kharitonova et al.,Cerebrovasc Dis 2007 |
26 |
|
|
|
|
Results: functional outcome modified Rankin score at 3 months
Outcome (mRS at day90)
SITS Non-HMCAS |
|
|
|
|
|
|
HDMCAS-D |
|
|
|
|
|
|
HMCAS-P |
|
|
|
|
|
|
0% |
20% |
40% |
|
60% |
80% |
100% |
mRS=0 |
mRS=1 |
mRS=2 |
mRS=3 |
mRS=4 |
mRS=5 |
mRS=6 |
|
|
HMCAS-D |
HMCAS-P |
P |
|
|
|
|
|
|
Independency (mRS0-2 atday 90) |
296 (41.5%) |
134 (19.0%) |
< 0.001 |
|
Mortality |
111 (15.3%) |
214 (30.2%) |
< 0.001 |
Kharitonova et al.,Cerebrovasc Dis 2007 |
|
|
27 |
|
The screen versions of these slides have full details of copyright and acknowledgements |
9 |

The Treatment of Stroke:
Specific Management – Thrombolysis Plus
Prof. Nils Wahlgren
Thrombectomy using the MERCI device has been evaluated in the MERCI trial and the Multi-MERCI trial
X6
Smith W,AJNR 2006 27(6): 1177-1182 |
28 |
Smith W et al.,Stroke 2008 39(4): 1205-1212 |
29
30 |
The screen versions of these slides have full details of copyright and acknowledgements |
10 |
