
Essentials of Orthopedic Surgery, third edition / 08-The Shoulder
.pdf
8
The Shoulder
RAYMOND M. CARROLL
The shoulder joint, as it is commonly called, is not a single joint but a complex arrangement of bones, ligaments, and musculotendinous units that is more aptly called the shoulder girdle. The primary role of the shoulder girdle is to provide a tremendous range of motion for positioning the upper extremity in space. The shoulder girdle also provides power and support for the upper extremity throughout and at the extremes of the range of motion. Many shoulder girdle problems stem from overuse injuries during activities such as pitching a baseball or serving a tennis ball that exploit both the power and range of motion of the shoulder girdle. This chapter reviews the anatomy of the shoulder girdle and provides an approach to evaluating and treating common shoulder problems.
Functional Anatomy
The shoulder girdle includes three bones (scapula, clavicle, and proximal humerus) (Fig. 8-1), three joints (glenohumeral, acromioclavicular, and sternoclavicular), an additional articulation (scapulothoracic), and some 17 musculotendinous units. These individual elements function in a synchronous and interdependent manner to maximize the power and range of motion of the shoulder girdle. The clavicle is the bony strut that links the upper appendicular skeleton to the axial skeleton at the sternum (sternoclavicular joint).
The Glenohumeral Joint
The glenohumeral (GH) joint is the articulation of the proximal humeral epiphysis (ball) with the glenoid fossa (socket) of the scapula. This joint contributes to the majority of motion in the shoulder girdle. As only 20% to 30% of the humeral head is in contact with the glenoid fossa at any point in the shoulder’s arc of motion and the radius of curvature of the glenoid is greater than that of the humeral head, there is little inherent bony stability of the GH joint. As a result, the soft tissues surrounding the joint
333

334 R.M. Carroll
FIGURE 8-1. Anterior view of the shoulder demonstrates the skeletal anatomy and two of the four articulations, the glenohumeral and acromioclavicular joints.
are responsible for maintaining joint stability and congruity while allowing a tremendous range of motion. These soft tissue stabilizers include the joint capsule, glenohumeral ligaments, glenoid labrum, long head of the biceps tendon, and the rotator cuff musculature. The burden placed upon these soft tissues leads to the majority of degenerative and traumatic conditions affecting the shoulder girdle.
The Glenohumeral Ligaments
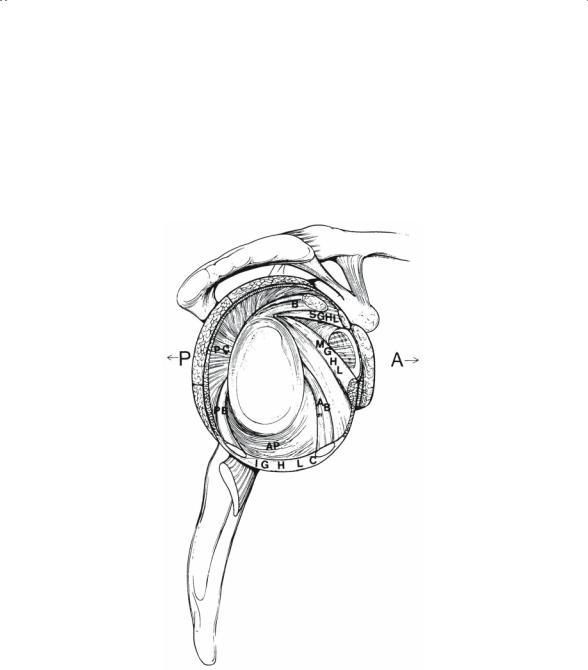
The capsule of the shoulder is a specialized structure that contains distinct thickenings referred to as ligaments (Fig. 8-2). The glenohumeral ligaments are named for their origin from the glenoid rim. This ligamentous complex includes the superior glenohumeral ligament (SGHL), the middle glenohumeral ligament (MGHL), the anterior band of the inferior glenohumeral ligament (AIGHL), and the posterior band of the inferior glenohumeral ligament (PIGHL). These ligaments function as static stabilizers of the glenohumeral joint. The SGHL is the primary restraint to inferior translation and external rotation with the arm in adduction. The MGHL is the primary
8. The Shoulder |
335 |
stabilizer to anterior translation with the arm in 45 degrees of abduction. The inferior glenohumeral ligament complex includes an anterior band, a posterior band, and an intervening sling or pouch. The inferior glenohumeral ligament complex becomes taut when the arm is abducted to 90 degrees. In this position, the anterior band resists anterior translation with external rotation and the posterior band resists posterior translation with internal rotation forces. The sling supports the humeral head.
FIGURE 8-2. In this cutaway view of the shoulder joint, the humeral head has been removed, allowing visualization of the interior of the normal glenohumeral anatomy. Notice the discrete ligaments that constitute the anterior shoulder capsule, namely the superior (SGHL), middle (MGHL), and anterior inferior glenohumeral ligaments. In this illustration, the most important anterior restraining structure, the inferior glenohumeral ligament complex (IGHLC), is shown further subdivided into having anterior (AB) and posterior (PB) bands and an axillary pouch (AP). (From Rockwood CA Jr, Matsen FA III (eds) The Shoulder, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)

336 R.M. Carroll
The Labrum
The labrum is a fibrous structure of variable anatomy that attaches to the rim of the glenoid cartilage through a fibrocartilaginous zone, increasing the depth of the glenoid concavity by 50%. The labrum functions to increase the surface contact area with the humeral head; to act as a static stabilizer through a buttress effect; and to serve as an attachment site for the shoulder capsule, glenohumeral ligaments, and long head of the biceps tendon. The labrum has a variable cross-sectional anatomy, the superior aspect of the labrum being more triangular shaped and well defined and the inferior aspect of the labrum more rounded and less distinct. Common anatomic variations include a sublabral hole (foramen) or an absent labrum in the anterosuperior quadrant of the glenoid. The combination of a cordlike MGHL and absent anterosuperior labrum has been termed a Buford complex. Additionally, the labrum may attach directly to the rim of the surface of the glenoid cartilage or it may have a reflected, or meniscal-type, attachment.
The Rotator Interval
The rotator interval is the triangular region between the superior aspect of the subscapularis tendon and the anterior aspect of the supraspinatus tendon whose base is the coracoid. The rotator interval includes a number of fibrous structures including the coracohumeral ligament, the SGHL, and the transverse humeral ligament. The coracohumeral ligament (CHL) is the most significant structure in the rotator interval and is extraarticular. It originates from the lateral base of the coracoid, fanning out to envelop the supraspinatus tendon inserting on the greater tuberosity and to envelop the subscapularis tendon inserting on the lesser tuberosity. The CHL is a primary restraint to inferior translation and external rotation in the adducted arm. The transverse humeral ligament forms the apex of the rotator interval and contributes to the superior soft tissue sling that stabilizes the long head of the biceps tendon as it passes through the interval to enter (or exit) the glenohumeral joint.
The Long Head of the Biceps Tendon
The long head of the biceps tendon (LHBT) remains somewhat enigmatic with respect to its function in the shoulder girdle, but it is nonetheless a potential source of pain and disability. The long head of the biceps enters/ exits the glenohumeral joint at the rotator interval by way of the bicipital groove and is an intraarticular structure. The LHBT originates from the superior glenoid tubercle and blends with the fibers of the superior labrum. This intimate relationship of the LGBT with the superior labrum is a significant source of morbidity in the throwing athlete. Although there are

8. The Shoulder |
337 |
conflicting data, the long head of the biceps is thought to be a humeral head depressor and may contribute to glenohumeral instability. Potentially more relevant is the theory of the “peel-back” mechanism of superior labral tears or SLAP (superior labrum anteroposterior) tears. This theory suggests that the LHBT and superior labrum detach from the superior glenoid in the late cocking position of a baseball pitch as the LHBT becomes taut and “peels back” the superior labrum off the glenoid rim. Whether or not this theory is correct, SLAP tears can be a significant problem in the throwing athlete. Tendonitis of the LHBT is also a common source of morbidity in the shoulder and is often a component of the impingement syndrome.
The Rotator Cuff
The rotator cuff consists of four muscle–tendon units including the subscapularis, supraspinatus, infraspinatus, and teres minor. These muscles originate on the scapula and insert onto the tuberosities of the proximal humerus. The subscapularis originates on the anterior surface of the scapula and inserts onto the lesser tuberosity. The remaining rotator cuff muscles originate from the posterior surface of the scapula and insert along the greater tuberosity. The roles of the rotator cuff are to keep the humeral head centered in the glenoid fossa throughout the range of shoulder motion and to contribute to the rotation and elevation of the extremity. As such, the rotator cuff is the primary dynamic stabilizer of the glenohumeral joint. Traumatic and overuse injuries to the rotator cuff are the most common problems in the shoulder girdle.
The Subacromial Space
The subacromial space is a potential space beneath the acromion and above the rotator cuff. The subacromial bursa outlines the subacromial space and provides frictionless gliding of the rotator cuff beneath the acromion and coracoacromial arch. Bony osteophytes on the undersurface of the anterior acromion have been postulated to narrow the subacromial space, irritate the subacromial bursa, and contribute to rotator cuff tears.
The Acromioclavicular Joint
The acromioclavicular (AC) joint is a true diarthrodial joint containing a fibrocartilaginous disk. The AC joint helps link the appendicular skeleton with the axial skeleton through the clavicle. Because there is little intrinsic bony stability to the AC joint, a number of ligaments and other soft tissues serve to stabilize this articulation (Fig. 8-3). The superior AC ligament is the most important horizontal stabilizer. The coracoclavicular (CC) ligaments, consisting of the conoid ligament (medial) and the trapezoid

338 |
R.M. Carroll |
|
||||
|
|
|
|
|
|
|
|
|
Clavicle |
|
|
|
|
|
|
|
Conoid lig. |
|
|
|
|
|
|
|
|
Coraco- |
|
|
|
|
||||
|
|
|
|
Trapezoid lig. |
|
clavicular |
|
|
|
|
|
ligament |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Acromioclavicular ligament |
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Acromion |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
Coraco- |
||||
|
Coracohumeral ligament |
|
|
|
|
acromial |
||||||||||
|
Coracoid process |
|
|
|
|
ligament |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Opening of sub- |
|
|
|
|
|
|
|
|
|
|
||||
|
|
scapular bursa |
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Capsule |
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Intertubercular |
|
|
|
|
|
|
|
|
|||||
|
|
|
synovial sheath |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Humerus |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Scapula |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FIGURE 8-3. In this anterior view, note the acromioclavicular joint surrounded by the capsule (acromioclavicular ligament), in addition to the supporting coracoclavicular ligaments, the conoid and trapezoid. (From Rockwood CA Jr, Matsen FA III (eds) The Shoulder, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
ligament (lateral), provide the primary restraint to vertical displacement of the clavicle. A significant amount of rotation occurs in the clavicle throughout the arc of elevation of the upper extremity. Approximately 10% of this rotation occurs at the acromioclavicular joint.
The Sternoclavicular Joint
The sternoclavicular (SC) joint is the only bony connection between the upper appendicular skeleton and the axial skeleton and has the least bony stability of any major joint. The majority of clavicular rotation occurs at the sternoclavicular joint, but less than 50% of the bulbous medial clavicle is in contact with the shallow sternal articular fossa. Thus, the soft tissues provide stability to the sternoclavicular joint. The ligamentous anatomy of the SC joint includes the intraarticular disk ligament, the costoclavicular

8. The Shoulder |
339 |
ligament, the interclavicular ligament, and the capsular ligament. Of these, the posterior sternoclavicular joint capsule has been shown to be the most important structure for preventing both anterior and posterior displacement of the medial clavicle.
The Scapulothoracic Articulation
The scapulothoracic articulation includes the scapula, posterior thorax, and interposed bursae, which provide frictionless motion between the scapula and posterior thorax. The scapulothoracic articulation provides a significant percentage of motion to the shoulder girdle. Specifically, the glenohumeral joint and scapulothoracic articulation function in a synchronous fashion to provide full forward elevation of the upper extremity in a 2 : 1 ratio. The scapular stabilizer muscles include the trapezius, levator scapulae, rhomboids, latissimus dorsi, and serratus anterior. Dysfunction of scapulothoracic motion, seen clinically as scapular winging, may be a result of nerve injury or muscle dysfunction. Damage to the spinal accessory nerve results in trapezius dysfunction and lateral scapular winging. Long thoracic nerve injury leads to serratus anterior dysfunction and medial scapular winging. Pain and loss of motion in the glenohumeral joint can lead to overuse and fatigue of the scapular stabilizer muscles, resulting in scapular winging.
The Brachial Plexus
The brachial plexus is composed of the ventral rami of cervical roots C5, C6, C7, and C8 and ventral thoracic root T1. With the exception of the spinal accessory nerve (XI), which innervates the trapezius, all the muscles contributing to the function of the shoulder girdle and upper extremity are innervated by nerves originating from the brachial plexus. The brachial plexus includes five nerve roots, three trunks (superior, middle, and inferior), six divisions (three anterior, three posterior), three cords (lateral, medial, and posterior), and six terminal branches (musculocutaneous, ulnar, medial cord branch to median nerve, lateral cord branch to median nerve, axillary, and radial). With the exception of the divisions, nerves originate from each level of the brachial plexus to innervate muscles of the shoulder girdle. Brachial plexus injuries are relatively common with traumatic shoulder girdle injuries such as proximal humerus fractures, glenohumeral dislocations, and fracture-dislocations.
Clinical Examination of the Shoulder Girdle
The history of present illness is critical in evaluation of shoulder girdle pathology and should be used to develop a reasonable differential diagnosis based on the patient’s story and the epidemiology of shoulder pathology.

340 R.M. Carroll
For example, a high-school athlete with activity-related shoulder pain is more likely to have instability or labral pathology than a rotator cuff tear. Conversely, a 65-year-old who has shoulder pain with activities of daily living is more likely to have rotator cuff disease than a labral tear or instability. The physical examination is used to narrow the differential diagnosis and make the definitive diagnosis. Most of the time an accurate diagnosis can be made using only the history and physical examination. Indiscriminate use of imaging studies and additional testing is not recommended.
Before ordering additional studies, the examiner must have a clear understanding of how the study will contribute to the evaluation and treatment of the patient.
History
Patients with shoulder pathology most often complain of pain, stiffness, instability, and weakness. When pain is the chief complaint, the examiner must characterize the pain, with particular attention to location. Pain from the glenohumeral joint and its surrounding soft tissues typically is localized to the anterosuperior aspect of the shoulder. Localization of the pain to the deltoid insertion in the arm is common in rotator cuff or subacromial pathology. Pain emanating from the neck or to the posterior scapular region is often due to cervical spine disease. Pain and crepitation in the periscapular region, however, may be related to scapulothoracic bursitis.
The timing and frequency of shoulder pain must also be given careful consideration. Activity-related pain can provide valuable clues as to the underlying diagnosis. Pain with overhead activities of daily living is common in rotator cuff pathology. Pain with sporting activities such as swimming, throwing, or serving is often related to the labrum or glenohumeral ligaments. Night pain is often reported with shoulder girdle pathology, especially in the setting of rotator cuff tears. Patients often report the inability to sleep on the affected side. Rest pain is uncommon but may occur with severe arthropathy or radicular pain from the cervical spine. If rest pain is the predominant complaint, the examiner should consider infection or malignancy as a possible source of pain.
The relationship of pain to injury is important to establish. Pain that begins with a traumatic event such as a fall on an outstretched hand, direct blow to the shoulder, or shoulder dislocation may represent significant damage to the rotator cuff, ligaments, or bony structures. Pain that begins days or weeks after a seemingly innocuous event such as shoveling snow; trimming hedges, or painting may represent tendonitis or early capsulitis.
Pain that begins more insidiously or over time is more likely to be related to degenerative lesions of the shoulder girdle such as rotator cuff tears or osteoarthritis.
Complaints of shoulder instability are relatively common. The patient may describe the shoulder “slipping out of place” or “getting stuck” in

8. The Shoulder |
341 |
extreme positions. It is important to establish whether a frank shoulder dislocation was ever documented. True traumatic shoulder dislocations are the result of significant trauma and require a manipulative reduction. Unfortunately, subsequent dislocations may occur with less trauma. Patients who have shoulders that “slip out of place” and “slide back in” on their own are more likely to have multidirectional instability as opposed to traumatic instability.
Weakness or loss of shoulder function is an infrequent complaint. In the absence of pain, a neurologic origin of the deteriorating function should be considered. Insidious onset of pain with deteriorating function may represent a degenerative condition of the shoulder or adhesive capsulitis.
A careful review of systems is important to document as there are a number of disease processes remote from the shoulder girdle that can result in shoulder pain. Cervical spine pathology, cardiac disease, gallbladder disease, and lung disease (pancoast tumor) can present with shoulder pain. A history of cancer is also important to document because metastatic cancer can present with shoulder pain and lesions in the shoulder girdle.
Functional Assessment
In addition to establishing the history of present illness, it is imperative to establish the functional status of the patient. Important patient factors to note include the handedness (right, left, or ambidextrous) of the patient; the vocation of the patient; extracurricular/sporting activities enjoyed by the patient, and, most importantly, the expectations of the patient with regard to the shoulder problem. Understanding the patient’s functional demands and expectations allows the clinician to prescribe appropriate treatment regimens and to provide reasonable expectations for functional recovery.
Inspection
The physical examination begins with inspection of the shoulder girdle. The region must be adequately exposed for the examination. The inspection begins with assessment of symmetry between the involved and uninvolved shoulder girdles. Gross deformity such as distal clavicle prominence in an AC separation, prior surgical incisions, skin discoloration, or open wounds are readily appreciated. A more subtle finding is muscle atrophy, which may be the result of disuse or injury. Patients with long-standing rotator cuff tears often have atrophy of the supraspinatus and infraspinatus fossae, resulting in prominence of the spine of the scapula. Traumatic injuries can produce subtle deformities. In the setting of an anterior dislocation, the anterior aspect of the shoulder may appear “full” and the posterior aspect may lose its normal contour, making the posterior acromion

342 R.M. Carroll
appear more prominent. Inspection should continue through the entire exam as some deformities such as scapular winging may only be revealed during provocative testing.
Palpation
The primary importance of palpation is to localize the source of pain. Palpation of bony prominences and superficial joints yields the most information. In the absence of trauma, palpation includes the SC joint, AC joint, the greater and lesser tuberosities, and the intertubercular or bicipital groove. Tenderness on palpation at any of these sites can be a valuable clue in making a diagnosis. When the presenting complaint is neck or periscapular pain, palpation of the posterior elements of the cervical spine and bony elements of the scapula is warranted. In the setting of trauma, palpation of all bony structures and areas of deformity is critical to localize the zone of injury.
Range of Motion
The evaluation of range of motion is straightforward. The examiner directs the motions and observes for symmetry. The standard motions include forward elevation, external rotation, internal rotation, and abduction. Forward elevation occurs in the plane of the scapula and is a combination of scapulothoracic and glenohumeral motion. Loss of glenohumeral motion can lead to scapulothoracic substitution and scapular winging. External rotation is evaluated with the arms at the side to prevent scapulothoracic contribution to rotation. Internal rotation is evaluated by having the patient place his hands as high as possible along the midline of the back. Internal rotation is graded by the approximate vertebral level the patient is able to reach. Assessment of abduction, including internal and external rotation in abduction, is critical for unmasking subtle losses of motion. Baseball pitchers often lose some internal rotation in abduction while gaining external rotation in abduction in their throwing arm. There is no net loss of motion, only a resetting of the range of motion relative to the nonthrowing shoulder.
When loss of active motion is identified, the examiner must assess the passive range of motion. If there is loss of active and passive motion, there is likely a soft tissue contracture or a physical block to motion (dislocation, loose body, or osteophyte). In the absence of trauma, loss of both active and passive motion usually represents adhesive capsulitis (frozen shoulder) or arthropathy. If there is loss of active motion with preserved passive motion, the examiner must consider tendon (rotator cuff) rupture or, potentially, nerve damage. When examining the rotator cuff muscles, the examiner must appreciate lag signs.
