
English Lectures / Functional chemistry 2 eng
.pdf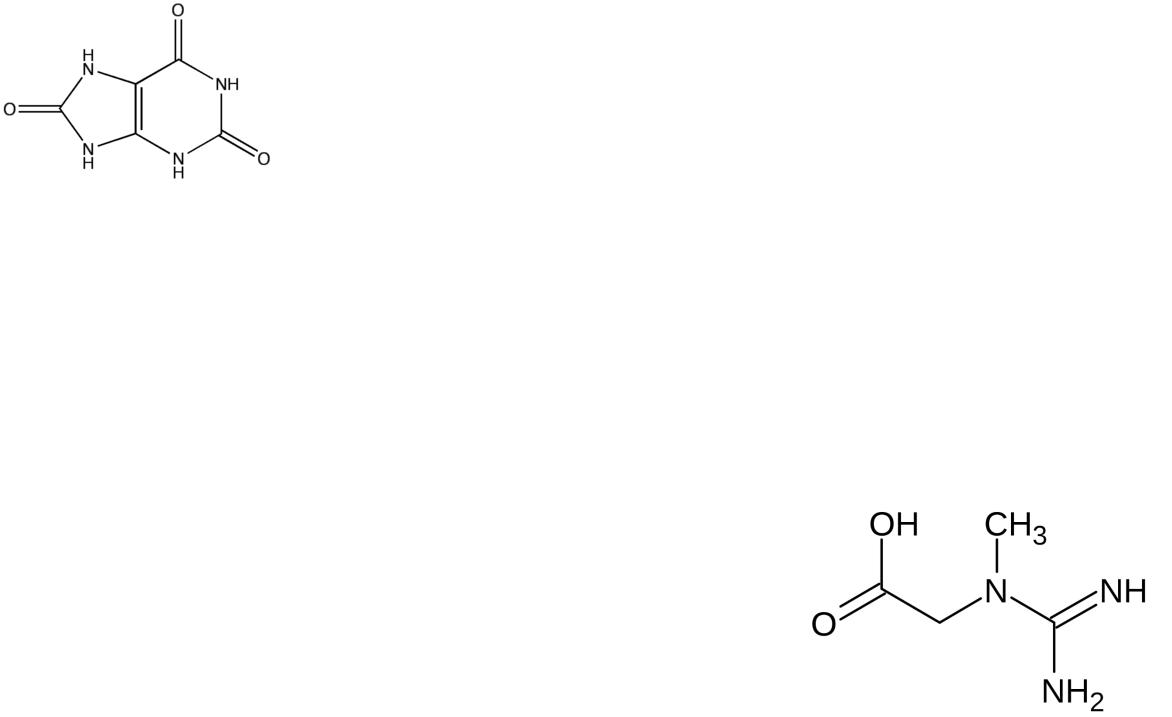
Uric acid and creatine
Uric acid is the end product of catabolism of purine nucleotides. Its content in the blood increases with gout (as a result of increased education) and with impaired renal function (due to insufficient excretion).
Creatine is synthesized in the kidneys and liver, in the muscles it turns into creatine phosphate – a source of energy for muscle contraction processes. With diseases of the muscular system, the creatine content in the blood increases significantly.

Creatinine, indican and bilirubin
Creatinine – the final product of nitrogen metabolism, is formed as a result of dephosphorylation of creatine phosphate in the muscles, excreted from the body by the kidneys. The content of creatinine in the blood decreases with diseases of the muscular system, increases with renal failure.
Indican – a product of the neutralization of indole, is formed in the liver, excreted by the kidneys. Its content in the blood decreases with liver diseases, increases with increased processes of protein decay in the intestine, with kidney diseases.
Bilirubin (direct and indirect) – products of hemoglobin catabolism. The content of bilirubin in the blood increases with jaundice: hemolytic (due to indirect bilirubin), obstructive (due to direct bilirubin), parenchymal (due to both fractions).
Blood coagulation system |
Let’s write! |
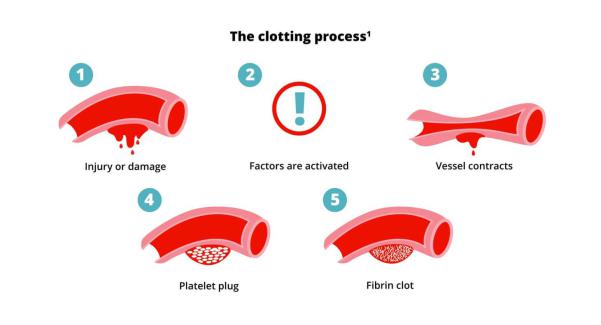
In case of accidental damage to small blood vessels, the resulting bleeding stops after some time. This is due to the formation of a blood clot or clot at the site of damage to the vessel. This process is called blood coagulation.
Blood coagulation phases Let’s write!
The process of blood coagulation proceeds in two phases.
In the first phase, prothrombin passes into the active enzyme thrombin under the influence of thrombokinase contained in platelets and released from them during the destruction of blood plates and calcium ions.
In the second phase, under the influence of the formed thrombin, fibrinogen turns into fibrin, which is deposited in a platelet plug and a thrombus forms on its surface.
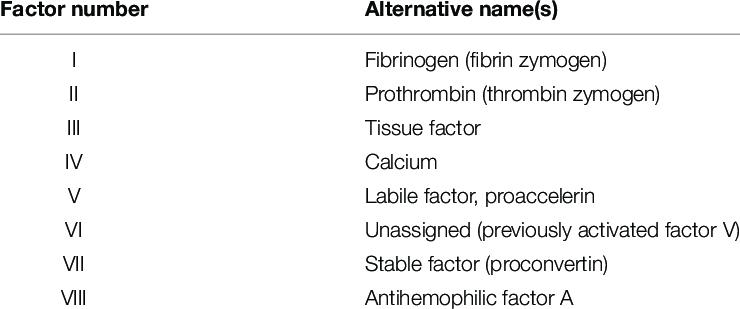
Clotting factors
In the process of blood coagulation, coagulation factors are involved. Coagulation factors associated with platelets are usually denoted by Arabic numerals (1, 2, 3, etc.), and coagulation factors found in blood plasma are indicated by Roman numerals.
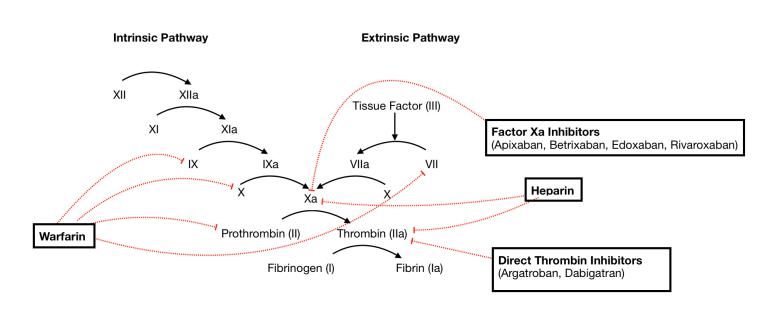
Extrinsic coagulation pathway Let’s write!
•Trace amounts of factor VIIa are constantly contained in the blood plasma.
•When tissue and vessel walls are damaged, factor III, a potent activator of factor VIIa, is released; the activity of the latter increases by more than 15,000 times.
•Factor VIIa cleaves a part of the peptide chain of factor X, turning it into an enzyme - factor Xa.
•Similarly, Xa activates prothrombin;
•the resulting thrombin catalyzes the conversion of fibrinogen to fibrin, as well as the conversion of the transglutaminase precursor to the active enzyme (factor XIIIa).
•This cascade of reactions has positive feedbacks that enhance the final result.
Intrinsic coagulation pathway
Let’s write!
•It is much slower and takes 10-15 minutes.
•This mechanism is called internal, because it does not require thromboplastin (tissue factor) and all the necessary factors are contained in the blood.
•Starting from the stage of conversion of factor X into Xa, the external and internal paths are the same. Like the external pathway, the internal coagulation pathway has positive feedbacks: thrombin catalyzes the conversion of the precursors V and VIII into activators V 'and VIII', which ultimately increase the rate of formation of thrombin itself.
External and internal blood coagulation mechanisms interact with each other. Factor VII specific to the external coagulation pathway can be activated by factor XIIa, which is involved in the internal coagulation pathway. This turns both paths into a single blood coagulation system.
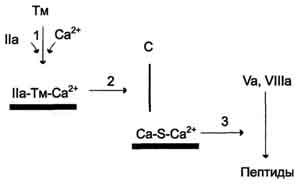
Противосвёртывающая система
Let’s write!
Антикоагулянтная фаза ограничивает время существования активных факторов в крови и инициируется самим тромбином. Этот этап представляет собой короткий каскад реакций, в котором кроме тромбина участвуют белок-активатор тромбомодулин (Тм), витамин К-зависимая сериновая протеаза протеин С, белокактиватор S и факторы Va и VIIIa.
Антикоагулянтная фаза вызывает торможение каскада реакций свёртывания крови, а ингибиторы ферментов свёртывания инактивируют активные ферменты в кровяном русле.
Blood clotting enzyme inhibitors
Physiological inhibitors of blood coagulation enzymes limit the spread of a blood clot to the site of vascular damage. Antithrombin III blood plasma protein is the most powerful blood coagulation inhibitor; it accounts for about 80-90% of anticoagulant blood activity. It inactivates a number of serine blood proteases: thrombin, factors IXa, Xa, XIIa, kallikrein, plasmin and urokinase. Antithrombin III does not inhibit factor VIIIa and does not affect factors in the composition of membrane complexes, but eliminates enzymes in the blood plasma, preventing the spread of thrombus formation in the bloodstream. The interaction of antithrombin with blood coagulation enzymes is accelerated in the presence of heparin.

Fibrinolytic blood system
A blood clot dissolves within a few days after formation. Fibrinolysis - enzymatic cleavage of fibrin fibers with the formation of soluble peptides that are removed from the vascular bed. The destruction of fibrin in the blood clot occurs under the action of a serine protease plasmin.
Plasmin is formed from plasminogen by the action of activators. Inactive plasminogen proenzyme plasminogen is synthesized in the liver, kidneys and bone marrow.
