
Gale Encyclopedia of Genetic Disorder / Gale Encyclopedia of Genetic Disorders, Two Volume Set - Volume 1 - A-L - I
.pdf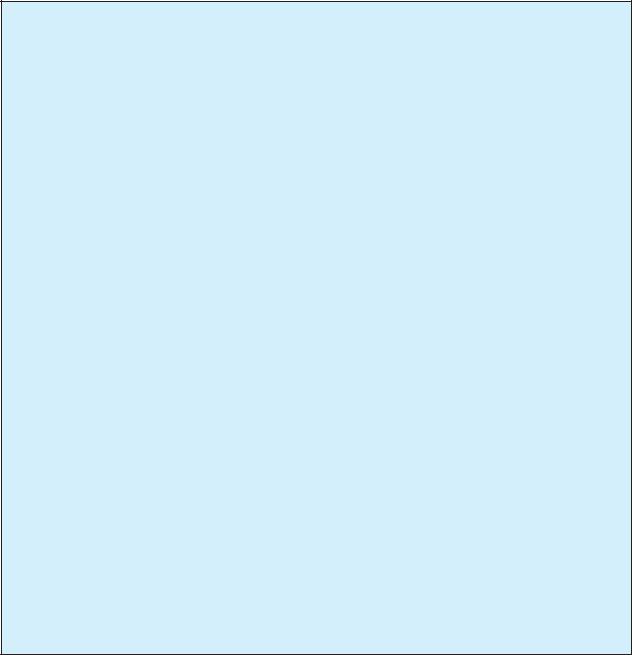
TABLE 1
Types of glaucoma and related genetic information
Disorder |
Alternative names |
Inheritance |
Abnormal protein |
Abnormal gene |
Gene location |
Glaucoma 1, open angle, |
Juvenile onset primary |
Autosomal dominant |
Trabecular meshwork- |
MYOC, (also known as |
1q24.3–q25.2; |
A (GLC1A) |
open-angle glaucoma; |
|
induced glucocorti- |
TIGR, GLC1A, JOAG, |
|
|
Hereditary juvenile |
|
coid response protein |
GPOA) |
|
|
glaucoma |
|
(myocilin) |
|
|
|
|
|
Unknown |
Unknown |
9q34.1 |
Glaucoma 1, open angle, |
Adult onset primary |
Autosomal dominant |
Unknown |
Unknown |
2qcen–q13; (additional |
B (GLC1B) |
open-angle glaucoma; |
|
|
|
loci under |
|
Hereditary adult |
|
|
|
investigation) |
|
glaucoma |
|
|
|
|
Glaucoma 1, open angle, |
Adult onset primary |
Autosomal dominant |
Unknown |
Unknown |
3q21–q24 |
C (GLC1C) |
open-angle glaucoma; |
|
|
|
|
|
Hereditary adult |
|
|
|
|
|
glaucoma |
|
|
|
|
Glaucoma 1, open angle, |
Adult onset primary |
Autosomal dominant |
Unknown |
Unknown |
8q23 |
D (GLC1D) |
open-angle glaucoma; |
|
|
|
|
|
Hereditary adult |
|
|
|
|
|
glaucoma |
|
|
|
|
Glaucoma 1, open angle, |
Adult onset primary |
Autosomal dominant |
Unknown |
Unknown |
10p15–p14 |
E (GLC1E) |
open-angle glaucoma; |
|
|
|
|
|
Hereditary adult |
|
|
|
|
|
glaucoma |
|
|
|
|
Glaucoma 1, open angle, |
Adult onset primary |
Autosomal dominant |
Unknown |
Unknown |
7q35–36 |
F (GLC1F) |
open-angle glaucoma; |
|
|
|
|
|
Hereditary adult |
|
|
|
|
|
glaucoma |
|
|
|
|
Glaucoma 3, primary |
Congenital glaucoma; |
Autosomal recessive |
Cytochrome P4501B1 |
CYP1B1 |
2p22–p21 |
infantile, A (GLC3A) |
Buphthalmos |
|
|
|
|
Glaucoma 3, primary |
Congenital glaucoma |
Autosomal recessive |
Unknown |
Unknown |
1p36.2–36.1 |
infantile, B (GLC3B) |
|
|
|
|
|
Iridogoniodysgenesis, |
Iridogoniodysgenesis |
Autosomal dominant |
Forkhead Transcription |
FKHL7 |
6P25 |
type 1 (IRID1) |
anomaly; familial |
|
factor |
|
|
|
glaucomaIridogonio- |
|
|
|
|
|
dysplasia |
|
|
|
|
Iridogoniodysgenesis, |
Iridogoniodysgenesis |
Autosomal dominant |
Paired-like |
PITX2 (also known as; |
4q25–q26 |
type 2 (IRID1) |
anomaly; Iris |
|
homeodomain |
IDG2,RIEG1, RGS, |
|
|
hypoplasia with early- |
|
transcription factor-2 |
IGDS2) |
|
|
onset glaucoma |
|
|
|
|
Rieger syndrome, type 1 |
Iridogoniodysgenesis |
Autosomal dominant |
Paired-like |
PITX2 (also known as; |
4q25–q26 |
(RIEG1) |
with Somatic |
|
homeodomain |
IDG2,RIEG1, RGS, |
|
|
anomalies |
|
transcription factor-2 |
IGDS2) |
|
Rieger syndrome, type 2 |
Iridogoniodysgenesis |
Autosomal dominant |
Unknown |
Unknown |
13q14 |
(RIEG2) |
with Somatic |
|
|
|
|
|
anomalies |
|
|
|
|
Glaucoma-related |
Pigment dispersion |
Autosomal dominant |
Unknown |
Unknown |
7q35–q36 |
pigment dispersion |
syndrome and |
|
|
|
|
syndrome (GPDS1) |
pigmentary glaucoma |
|
|
|
|
Glaucoma
within the first three years of life. Symptoms include cloudy corneas, excessive tearing, and sensitivity to light. Because the eye is very flexible in infants, increased fluid pressure may cause bulging of the eye (buphthalmos, or “ox eye”). Children with glaucoma in only one eye are usually diagnosed earlier because a difference in eye size can be noticed. When the disorder affects both eyes, many parents view the large eyes as attractive and do not seek help until other symptoms develop, delaying the diagnosis.
With closed-angle glaucoma, symptoms come on suddenly. People may experience blurred vision, severe pain, headache, sensitivity to light, and nausea. The development of this type of glaucoma is an emergency and requires immediate treatment.
Diagnosis
The diagnosis of glaucoma may be suggested by certain physical findings, especially in infants, but is con-
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
485 |

Glaucoma
K E Y T E R M S
Aqueous humor—A fluid produced by the ciliary body and contained within the front chamber of the eye.
Autosomal dominant—A pattern of genetic inheritance where only one abnormal gene is needed to display the trait or disease.
Autosomal recessive—A pattern of genetic inheritance where two abnormal genes are needed to display the trait or disease.
Buphthalmos—A characteristic enlargement of one or both eyes associated with infantile glaucoma.
Ciliary body—A structure within the eye that produces aqueous humor.
Closed-angle glaucoma—An increase in the fluid pressure within the eye due to a complete, and sometimes sudden, blockage of the fluid drainage passages.
Cornea—The transparent structure of the eye over the lens that is continuous with the sclera in forming the outermost protective layer of the eye.
Glaucoma—An increase in the fluid eye pressure, eventually leading to damage of the optic nerve and ongoing visual loss.
Gonioscope—An instrument used to examine the
trabecular meshwork; consists of a magnifier and a lens equipped with mirrors.
Ophthalmologist—A physician specializing in the medical and surgical treatment of eye disorders.
Ophthalmoscope—An instrument, with special lighting, designed to view structures in the back of the eye.
Optic disc—The region where the optic nerve joins the eye, also refered to as the blind spot.
Optic nerve—A bundle of nerve fibers that carries visual messages from the retina in the form of electrical signals to the brain.
Optometrist—A medical professional who examines and tests the eyes for disease and treats visual disorders by prescribing corrective lenses and/or vision therapy. In many states, optometrists are licensed to use diagnostic and therapeutic drugs to treat certain ocular diseases.
Retina—The light-sensitive layer of tissue in the back of the eye that receives and transmits visual signals to the brain through the optic nerve.
Tonometer—A device used to measure fluid pressures of the eye.
Trabecular meshwork—A sponge-like tissue that drains the aqueous humor from the eye.
firmed by tests with special instruments. Parents may bring their young infant to a physician if they notice signs of infantile glaucoma, such as changes in the eye shape and size. In adults, who do not show obvious signs of glaucoma, the condition is frequently detected by routine screening eye exams and other tests.
Using an ophthalmoscope (a hand-held or machine mounted instrument using a light source), a physician or optometrist will look through the pupil to the back of the eye. There, they may detect characteristic changes in the region where the optic nerve meets the eye, called the optic disk.
In another portion of a routine eye exam, an ophthalmologist or optometrist will measure the fluid pressure of the eye through the use of a special instrument called a tonometer. The test is painless and involves brief contact of a small probe with the surface of the eye. Presence of elevated pressure (more than 21 mm Hg) means that a person is at risk for glaucoma.
Once high pressures or changes in the optic disk are noted, an ophthalmologist can also use a gonioscope
(small lens with a reflecting mirror) to inspect the drainage passageways of the eye and determine if they are blocked. Visual field tests (in which a patient indicates whether they can see small flashing lights that are directed in different spots of the patient’s visual field) are used as a final indicator for the presence of glaucoma or a measurement of how far glaucoma-related visual loss has progressed.
Treatment and management
Although there is no treatment for the optic nerve injury and vision loss caused by glaucoma, it is possible to prevent further visual loss by lowering eye fluid pressure. In the adult, this is primarily achieved through medications. Medications can reduce eye fluid pressure by either decreasing fluid production or by increasing fluid drainage from the eye, and can be taken by mouth or applied to the eye through drops. The names of different classes of medications used to treat glaucoma include beta-blockers, alpha agonists, carbonic anhydrase inhibitors, and prostaglandin analogues.
486 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |

For infantile glaucoma, the treatment is primarily surgical. Laser surgery or microsurgery to open the drainage canals can be effective in increasing drainage of eye fluid. Other types of surgery can be performed to reduce the amount of fluid production. Many children require several operations to lower or maintain their eye fluid pressures adequately, and long-term treatment with medications may still be necessary. For closed-angle glaucoma, immediate hospitalization and treatment with medication is required. Once the person’s condition has been stabilized, laser surgery is used to create a passageway for fluid drainage.
All individuals with glaucoma should see an ophthalmologist regularly to evaluate progress of the condition and whether it is being adequately treated. Beginning at the age of 40, all people should receive regular screening exams to detect early signs of glaucoma. People with a family history of glaucoma or with diabetes should receive these screening tests beginning in young adulthood.
Prognosis
Since even small amounts of vision loss due to glaucoma cannot be reversed, early detection of the condition through regular eye examinations is critical. If glaucoma is detected early, lifelong medical treatment can halt the progress of the disease and result in relatively normal vision. If left undiagnosed or untreated, many people with glaucoma will progress to blindness.
Closed-angle glaucoma is an emergency and the prognosis depends on how quickly medical attention is obtained and the severity of the attack. If left untreated, the condition can quickly lead to total vision loss in the affected eye.
Resources
BOOKS
Marks, E., and R. Mountauredes. Coping With Glaucoma. Garden City Park, NY: Avery Publishing Group, 1997.
Trope, G. E. Glaucoma: A Patient’s Guide to the Disease.
Toronto: University of Toronto Press, 1996.
PERIODICALS
Coleman, A. L. “Glaucoma.” Lancet 354 (November 1999): 1803-1810.
Migdal, C. “Glaucoma Medical Treatment: Philosophy, Principles and Management.” Eye 14 (June 2000): 515-518.
ORGANIZATIONS
Glaucoma Foundation. 33 Maiden Lane, New York, NY 10038. (800) 452-8266 http://www.glaucoma-foundation.org .
Glaucoma Research Foundation. 200 Pine St., Suite 200, San Francisco, CA 94104. (800) 826-6693
Retinal photographs, like the one shown here, can be used to check for signs of glaucoma, such as increased fluid and damage to the optic nerve. (Custom Medical Stock Photo, Inc.)
WEBSITES
“Glaucoma.” Online Mendelian Inheritance in Man. National Center for Biotechnology Information, National Center for Biotechnology Information, National Library of Medicine. Building 38A, Room 8N805, Bethesda, MD 20894.http://www3.ncbi.nlm.nih.gov/htbin-post/Omim
Glaucoma Resources on the Internet.http://www.healthcyclopedia.com/glaucoma.html .
Oren Traub, MD, PhD
GLB1 deficiency see GM1 gangliosidosis
Globoid cell leukodystrophy (GCL) see
Krabbe disease
Glucocerebrosidase deficiency see
Gaucher disease
Glycogen storage disease II see Acid maltase deficiency
I GM1-gangliosidosis
Definition
GM1-gangliosidosis is a lysosomal storage condition caused by a reduction or the absence in the amount of the enzyme, beta-galactosidase, in cells. This condition has been referred to by other names such as NormanLanding disease, Gangliosidosis-GM1 beta-galactosidase-1 deficiency, Hurler-variant, pseudo-Hurler disease, Tay-
gangliosidosis-GM1
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
487 |
GM1-gangliosidosis
Sachs disease with visceral involvement, and GLB1 deficiency.
Description
Lysosomes are structures found inside cells that contain specific proteins and enzymes that help digest or breakdown many of the complex biological substances found within the cells. After the lysosomes digest these substances, the remnants are then released from the cell. The role of the lysosome is to keep the inside of the cell clean and to help the cell function normally.
One of the lysosomal enzymes, beta-galactosidase, is necessary to digest a substance called GM1-ganglio- side. When there is not enough beta-galactosidase within the lysosomes, GM1-ganglioside breaks down at a slower rate or not at all. Since GM1-ganglioside is not being digested as fast as it is being produced, GM1-ganglioside accumulates within the lysosomes. When too much GM1-ganglioside accumulates, the lysosomes stop functioning effectively, thereby causing the cell not to function properly.
When there are enough cells in an organ or organ system that stop functioning normally, the entire organ or organ system begins to experience problems. One of the first areas where GM1-ganglioside accumulates and causes problems is within the central nervous system. Other organs and systems in the body can also accumulate GM1-ganglioside; however, signs of the excessive accumulation are sometimes not immediately apparent.
There are three types of GM1-gangliosidoses; they are grouped according to the amount of beta-galactosi- dase detected in the individual’s leukocytes (white blood cells) or skin cells, the individual’s age when they start to show symptoms (called age of onset), and the specific symptoms that the individual exhibits. These types are labeled Type I, Type II, and Type III.
Genetic profile
All three types of GM1-gangliosidosis are inherited in an autosomal recessive manner. Symptoms of GM1gangliosidosis occur when the pair of genes that produce beta-galactosidase (called GLB1) both contain a change, causing them not to work properly. When the GLB1 genes do not work properly, less or no beta-galactosidase is produced. Individuals with GM1-gangliosidosis inherit one of their non-working GLB1 genes from their mother and the other non-working GLB1 gene from their father. These parents are called carriers of GM1-gangliosidosis. When two people are known carriers for an autosomal recessive condition, like GM1-gangliosidosis, they have a 25% chance with each pregnancy to have a child affected with the disease.
The GLB1 gene is located on the short arm of chromosome 3, called 3p, in the region 21.33. This is written as 3p21.33. There have been over 20 mutations identified in the GLB1 gene that can cause the gene not to work properly. The most common type of mutation detected is a missense mutation. Typically, a gene is made up of DNA that codes for specific amino acids. It is the amino acids, when combined, that make a protein. When there is a missense mutation in a gene, the DNA code for a particular amino acid has been changed, often coding for a different amino acid. Changing the amino acid often changes the protein that is made. A change in the structure or production of a protein often alters its ability to function properly.
Most individuals with GM1-gangliosidosis are compound heterozygotes. This means that an individual with GM1-gangliosidosis has one GLB1 gene containing one mutation and his or her other GLB1 gene has a different mutation. Researchers do not believe that there is any correlation between specific mutations in the GLB1 gene and the severity of GM1-gangliosidosis. An exception to this is the discovery of mutations in the GLB1 gene that, instead of causing an individual to have GM1-gangliosi- dosis, cause the individual to have another condition called Morquio syndrome type B.
Demographics
GM1-gangliosidosis is a rare condition. It is estimated that approximately one in 100,000–200,000 live births is affected with this condition. Type I GM1-gan- gliosidosis is considered to occur more often than the other two types. There has also been an increased number of individuals living in Japan, Brazil, and Maltese Island diagnosed with all types of GM1-gangliosidosis. However, many researchers state that this condition is not more common in individuals of certain ethnic groups, although many of the individuals with Type III GM1gangliosidosis are Japanese. Additionally, GM1-gan- gliosidosis occurs with equal frequency in males and females.
Signs and symptoms
GM1-gangliosidosis Type I
Type I GM1-gangliosidosis is also called infantile GM1-gangliosidosis or infantile type, and it is considered the most severe form of GM1-gangliosidosis. Infants with GM1-gangliosidosis Type I tend to have less than 1% of the normal amount of beta-galactosidase in their cells.
Some of the symptoms seen with Type I can be apparent at birth, but all infants with Type I will show
488 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |

characteristics of the condition before six months of age. All infants with Type I will reach a point where they fail to gain new skills and begin to regress and lose the skills they have learned.
Several of the initial symptoms seen in infants with Type I are caused by the storage of GM1-ganglioside in the cells of the infant’s central nervous system. One sign of a problem with the central nervous system seen in some infants with Type I is the infant’s inability to eat much food or formula because of a poor appetite and/or difficulties with sucking on a bottle or nipple. As a result, they tend to gain very little weight. Another sign of GM1ganglioside storage in the central nervous system is muscle problems. Most of these infants will have low muscle tone, called hypotonia. These babies appear “floppy” or “loose”. As the disease progresses, the infant presents with other central nervous system problems, such as an exaggerated reaction to sound, atrophy of the optic nerves, their bodies becoming rigid and stiff, developing tight joints (joint contractures), and experiencing seizures. Infants with Type I can also develop brain atrophy and/or areas of decreased amount of white matter in the brain.
In GM1-gangliosidosis Type I, GM1-ganglioside is also stored in the skeleton, causing visible changes on radiographs. Some of the more common bone changes are: differences with their vertebrae causing spine curvature, thicker skull, wider bones and hands, and wide, short fingers. Also, the growth of the bones tends to slow down or stop, causing infants with GM1-gangliosidosis Type I to appear smaller than expected for their age.
Additionally, infants with Type I usually develop certain characteristic facial features. The facial features typically seen in infants with Type I include frontal bossing, ears that are set lower on the head than normal, thicker skin, hair on forehead and neck, an elongated space between the nose and mouth, and an enlarged tongue. Children with these facial changes are often described as appearing “coarse”. Coarse facial features can also be seen in infants and children who have other types of storage disorders.
Other characteristics of GM1-gangliosidosis Type 1 include an enlarged spleen and liver (called hepatosplenomegaly), cardiomyopathy (which has only been described in caucasian patients), and an enlargement of the cells in the bone marrow. Additionally, infants with Type I have cherry-red spots in the macula of their retinas, and several develop corneal clouding.
GM1-gangliosidosis Type II
GM1-gangliosidosis Type II is also referred to as the juvenile type. In children with Type II, the amount of
K E Y T E R M S
Amino acid—Organic compounds that form the building blocks of protein. There are 20 types of amino acids (eight are “essential amino acids” which the body cannot make and must therefore be obtained from food).
Ataxia—A deficiency of muscular coordination, especially when voluntary movements are attempted, such as grasping or walking.
Atrophy—Wasting away of normal tissue or an organ due to degeneration of the cells.
Basal ganglia—A section of the brain responsible for smooth muscular movement. Cardiomyopathy—A thickening of the heart muscle.
Cytoplasm—The substance within a cell including the organelles and the fluid surrounding the nucleus.
Deoxyribonucleic acid (DNA)—The genetic material in cells that holds the inherited instructions for growth, development, and cellular functioning.
Dystonia—Painful involuntary muscle cramps or spasms.
Enzyme—A protein that catalyzes a biochemical reaction or change without changing its own structure or function.
Frontal bossing—A term used to describe a rounded forehead with a receded hairline.
Gray matter—Areas of the brain and spinal cord that are comprised mostly of unmyelinated nerves. Lysosome—Membrane-enclosed compartment in cells, containing many hydrolytic enzymes; where large molecules and cellular components are broken down.
Mutation—A permanent change in the genetic material that may alter a trait or characteristic of an individual, or manifest as disease, and can be transmitted to offspring.
Myelin—A fatty sheath surrounding nerves in the peripheral nervous system, which help them conduct impulses more quickly.
Organelle—Small, sub-cellular structures that carry out different functions necessary for cellular survival and proper cellular functioning.
White matter—A substance found in the brain and nervous system that protects nerves and allows messages to be sent to and from to brain to the various parts of the body.
gangliosidosis-GM1
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
489 |
GM1-gangliosidosis
beta-galactosidase in the cells is approximately 1–5% of normal.
There are no symptoms that are specific to GM1Gangliosidosis Type II. Signs of Type II often appear late in infancy or in early childhood. Although each individual with Type II may present differently, several children with Type II have been reported to have difficulty walking and/or developed seizures. The bone changes seen in Type I may or may not occur in children with Type II. Furthermore, children with Type II do not have macular cherry-red spots, enlarged spleen or liver, or the facial changes.
GM1-gangliosidosis Type III
Individuals with GM1-gangliosidosis Type III are also labeled as having the adult or chronic type of this condition. Individuals with Type III tend to have approximately 10% of the normal amount of beta-galactosidase in their cells. The age when symptoms begin to appear in individuals with Type III is extremely variable. There have been reports of individuals with Type III exhibiting symptoms as early as three years of age to as late as 30 years old. The symptoms slowly worsen over many years.
Individuals with GM1-gangliosidosis Type III tend to experience some symptoms related to the storage of GM1-ganglioside in their central nervous system; however, these symptoms are not as severe as those seen in infants with Type I. The signs of GM1-ganglioside storage can be different in each person affected with the GM1-gangliosidosis Type III, but many individuals with Type III have been reported to have signs of dystonia. Other neurological symptoms in Type III can include difficulty or unusual method of walking (ataxia), mild mental delays, and slurred speech. Often the ataxia and slurred speech are some of the first symptoms to appear.
Individuals with Type III also have GM1-ganglioside storage in bone cells, but bone changes are considered milder than those seen in Type I. Often the vertebrae of individuals with Type III tend to have a flattened appearance and/or the presence of other mild vertebral changes. On CT or MRI examinations, mild brain atrophy with signs of storage in the basal ganglia can be present in some individuals with Type III. Also, some individuals with Type III have experienced corneal clouding. However, the macular cherry-red spots, facial changes, and differences in the bones are not seen in individuals with GM1-gangliosidosis Type III.
Diagnosis
The diagnosis of GM1-gangliosidosis in an individual can be made by measuring the amount of beta-galac- tosidase in either skin cells or in leukocytes. Additionally,
prenatal testing to determine if a fetus is affected with GM1-gangliosidosis prior to its delivery can be accomplished by measuring the amount of beta-galactosidase on cultured cells from an amniocentesis or chorionic villus sampling (CVS). Amniocentesis is a procedure used to remove some of the fluid, which contains fetal cells, from around the fetus. CVS is used to obtain cells from the placenta. With both of these procedures, the cells collected are stimulated to multiply so that there are enough cells to perform certain analyses, in this case measuring the amount of beta-galactosidase. Both of these procedures have their own risks, benefits, and limitations.
X rays can detect bone changes and organ enlargement. However, in early stages of the condition, bone differences may not have developed or the organs may not yet be enlarged. Also, a CT scan and/or MRI can identify brain changes, such as cerebral atrophy or a loss of myelin in the white matter of the brain. An eye examination can detect any macular cherry-red spots or other changes.
Analysis of the amount of beta-galactosidase in an individual’s cells cannot be used to determine if the person is a carrier of GM1-gangliosidosis. This is because the range for the amount of beta-galactosidase seen in carriers of this condition overlaps with the range of the amount of beta-galactosidase seen in individuals who are not carriers.
Treatment and management
There is no cure for GM1-gangliosidosis. Most of the treatments revolve around trying to alleviate some of the symptoms, such as helping infants with Type I to eat and devices that can help with problems walking in individuals with Type III. Additionally, there is ongoing research into gene therapy for GM1-gangliosidosis to infuse genes that produce beta-galactosidase into the body.
Prognosis
In Type I GM1-gangliosidosis, the child dies within a few years after the symptoms begin, typically by age two. In Type II GM1-gangliosidosis, the prognosis is variable. Some individuals have died during childhood and others have lived many years after symptoms began. In Type III GM1-gangliosidosis, no decrease in lifespan has been reported.
Resources
BOOKS
Suzuki, Yoshiyuki, Hitoshi Sakuraba, and Akihiro Oshima.
“Beta-Galatosidase Deficiency (Beta-Galactosidosis):
490 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |

GM1 Gangliosidosis and Morquio B Disease.” In The Metabolic and Molecular Bases of Inherited Disease, edited by Charles R. Scriver et al. New York: McGraw Hill, 1995, pp. 2785-2823.
ORGANIZATIONS
Association for Neuro-Metabolic Disorders. 5223 Brookfield Lane, Sylvania, OH 43560-1809. (419) 885-1497.
WEBSITES
Lysosomal Storage Disease: A Family Source Book.
http://mcrcr2.med.nyu.edu/murphp01/lysosome/hgd.htm .
Online Mendelian Inheritance in Man. National Center for Biotechnology Information. http://www.ncbi.nlm.nih
.gov/Omim/ .
Sharon A. Aufox, MS, CGC
Goiter-sensorineural deafness syndrome see
Pendred syndrome
Golabi-Rosen syndrome see Simpson-
Golabi-Behmel syndrome
Goldberg syndrome see Neuraminidase deficiency with beta-galactosidase deficiency
I Goldenhar syndrome
Definition
Goldenhar syndrome is a congenital condition that is associated with abnormalities of the head and the bones of the spinal column. The abnormalities of the head can include differences with the eyes, ears, facial bones, and mouth. These differences are extremely variable in severity. The exact cause of Goldenhar syndrome remains unknown.
Description
Goldenhar syndrome was first described by Dr. Maurice Goldenhar in 1952. Individuals with Goldenhar syndrome have physical differences that are present at birth (congenital). These abnormalities are typically limited to the head and bones of the spinal column (vertebrae) and may be severe or mild. In some cases, the changes are seen on both sides of the face (bilateral). In other cases, the changes are limited to one side of the face (unilateral).
Another name for Goldenhar syndrome is oculo- auriculo-vertebral spectrum. This name describes the common birth defects seen in Goldenhar syndrome. The term oculo represents the eye, auriculo represents the ear, and vetebral stands for the physical problems present in the vertebrae.
In Goldenhar syndrome, the facial bones, including the jaw bones (mandible) and cheek bones (maxilla), can be underdeveloped (hypoplasia). This underdevelopment can be limited to one side of the face. This is called hemifacial microsomia. Hemifacial microsomia can occur alone or with Goldenhar syndrome. If an individual has hemifacial microsomia without additional birth defects, Goldenhar syndrome is unlikely. Although this is the case, hemifacial microsomia and Goldenhar syndrome are thought to have similar causes.
Genetic profile
Goldenhar syndrome is caused by a disruption of normal facial development. A baby’s face forms very early, normally between the eighth and twelfth weeks of pregnancy. Normal facial development depends on many different tissues growing together. When the movement and development of these tissues is disrupted, the face may have abnormal openings, underdevelopment, and/or excess skin.
The exact cause of Goldenhar syndrome is unknown. There are most likely many factors that lead to the abnormal development of the facial tissues. In some cases the factors may be environmental. For example, there are certain medications a woman can take while pregnant that can cause the baby to have the symptoms of Goldenhar syndrome. However, in the vast majority of cases, Goldenhar syndrome is not caused by something taken during pregnancy.
In other cases, normal development of the facial tissues may be disrupted by genetic factors. The exact genetic factors are unknown. Unlike some other syndromes, there has not been a gene identified that, if changed, causes Goldenhar syndrome. A few families in which Goldenhar syndrome occurs show an autosomal recessive inheritance pattern, while other families clearly support an autosomal dominant pattern of inheritance. However, most cases of Goldenhar syndrome are not inherited, meaning that it does not normally run in families.
Goldenhar syndrome typically occurs randomly. Doctors are often unable to explain why it occurs. Since it is sporadic in nature, if a child is diagnosed with Goldenhar syndrome, the risk for the parents to have another child with Goldenhar syndrome is low. In rare
syndrome Goldenhar
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
491 |

Goldenhar syndrome
K E Y T E R M S
Anopthalmia—A medical condition in which one eye is missing.
Anotia—Absence of an ear.
Auriculo—Related to the ear.
Bilateral—Relating to or affecting both sides of the body or both of a pair of organs.
Cleft lip—A separation of the upper lip that is present from birth but originates early in fetal development. A cleft lip may appear on one side (unilateral) or both sides (bilateral) and is occasionally accompanied by a cleft palate. Surgery is needed to completely repair cleft lip.
Cleft palate—A congenital malformation in which there is an abnormal opening in the roof of the mouth that allows the nasal passages and the mouth to be improperly connected.
Coloboma—A birth defect in which part of the eye does not form completely.
Congenital—Refers to a disorder which is present at birth.
Deoxyribonucleic acid (DNA)—The genetic material in cells that holds the inherited instructions for growth, development, and cellular functioning.
Ear tags—Excess pieces of skin on the outside of the ear.
Epibulbar dermoids—Cysts on the eyeball.
Facial asymmetry—Term used to describe when one side of the face appears different than the other.
Hemifacial microsomia—Term used to describe when one side of the face is smaller than the other.
Hemivertebra—A defect in which one side or half of a vertebra fails to form.
Hypoplasia—Incomplete or underdevelopment of a tissue or organ.
Macrostomia—A mouth that is larger or wider than normal.
Malar hypolplasia—Small or underdeveloped cheekbones.
Mandible—Lower jaw bone.
Mandibular hypoplasia—Underdevelopment of the jaw.
Maxiallary hypoplasia—Underdevelopment of the jaw.
Maxilla—One of the bones of the face.
Microphthalmia—Small or underdeveloped eyes.
Microtia—Small or underdeveloped ears.
Oculo—Related to the eye.
Scoliosis—An abnormal, side-to-side curvature of the spine.
Strabismus—An improper muscle balance of the ocular musles resulting in crossed or divergent eyes.
Unilateral—Refers to one side of the body or only one organ in a pair.
Vertebra—One of the 23 bones which comprise the spine. Vertebrae is the plural form.
Vertebral—Related to the vertebrae.
cases, one parent may have some of the physical symptoms of Goldenhar syndrome. If this is the case, the risk to have a child with the disorder may be much higher.
Demographics
Goldenhar syndrome occurs in one of every 3,000 to 5,000 live births. Males are affected more frequently than females. This syndrome is seen in all ethnic groups and cultures.
Signs and symptoms
The abnormalities seen in Goldenhar syndrome are typically limited to the face and vertebrae. Thirty per-
cent of patients have bilateral facial abnormalities. In these patients, the right side is usually affected more severely.
The symptoms associated with Goldenhar syndrome are highly variable. Some individuals with Goldenhar syndrome have many severe abnormalities, while other individuals have few minor birth defects.
Hemifacial microsomia is a common physical difference seen in Goldenhar syndrome. This is caused by hypoplasia (underdevelopment) of the bones of the face. These bones are called the mandible and the maxilla. In addition to the bones of the face, the muscles of the face can also be underdeveloped. Cleft lip and cleft palate are another facial difference associated with Goldenhar syn-
492 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
drome. Cleft lip is an abnormal split or opening in the lip that can extend towards the nose or towards the cheek. Cleft palate is an opening in the roof of the mouth. Individuals with Goldenhar can also have wide mouth (macrostomia).
Birth defects of the eye are common in Goldenhar syndrome. Cysts on the eyeball (epibulbar dermoids) are common, as is micropthalmia (small eye). Some individuals with Goldenhar syndrome have tissue missing from the upper eyelid (coloboma). Strabismus (crossing of the eyes) is also prevalent.
Abnormal development of the ears is another characteristic of Goldenhar syndrome. The ears may be smaller than normal (microtia), or absent (anotia). Ear tags (excess pieces of skin) may be seen on the cheek next to the ear and may extend to the corner of the mouth. The shape of the ears may also be unusual. Hearing loss is common in individuals with Goldenhar syndrome.
The vertebral problems seen in Goldenhar syndrome result from incomplete development of the vertebrae. Vertebrae can be incompletely developed (hemivertebrae), absent, or fused. Ribs can also be abnormal. Approximately 50% of individuals with Goldenhar syndrome will have curvature of the spine (scoliosis).
Other differences outside of the face and vertebra can occasionally be seen in Goldenhar syndrome. Approximately 15% of individuals with Goldenhar syndrome have developmental delay or mental retardation. The likelihood for mental retardation increases if the individual has micropthalmia. Heart defects and kidney defects can also occur.
Diagnosis
There is not a genetic test that can diagnose Goldenhar syndrome. The diagnosis is made when an individual has the common symptoms associated with the condition. The diagnosis is made by a physician.
Treatment and management
Once a child is diagnosed with Goldenhar syndrome, additional tests should be performed. A hearing evaluation is necessary to determine if there is hearing loss. If hearing loss is evident, the child should be referred to a hearing specialist. Speech therapy may also be helpful. X rays of the spine are recommended to determine if there are vertebral problems, and the severity. Individuals with Goldenhar syndrome should also be regularly evaluated for scoliosis. Renal ultrasounds and ultrasounds of the
heart may also be recommended, due to the increased risk for birth defects in these areas. A doctor would make this recommendation. Finally, individuals with Goldenhar syndrome should be evaluated by an eye doctor (ophthalmologist).
Surgery may be required to correct the birth defects seen in Goldenhar syndrome. Surgery to correct the facial birth defects can improve appearance and function.
Prognosis
The prognosis for individuals with Goldenhar syndrome is very good. These individuals typically have a normal life span and normal intelligence.
Resources
BOOKS
Cohen, M. Michael, Robert Gorlin, and F. Clarke Fraser. “Craniofacial Disorders.” In Emery and Rimoin’s
Principles and Practice of Medical Genetics. 3rd ed. New York: Churchill Livingstone, 1996, pp. 1132-1134.
Jones, Kenneth Lyons. “Oculo-Auriculo-Vertebral Spectrum.” In Smith’s Recognizable Patterns of Human Malformation.
Philadelphia: W.B. Sanders, 1997, pp. 642-643.
PERIODICALS
Schaefer, G.Bradley, Ann Olney, and Peg Kolodziej. “Oculo-
auriculo-vertebral Spectrum.” ENT—Ear, Nose & Throat
Journal 77 (1998): 17-18.
ORGANIZATIONS
Alliance of Genetic Support Groups. 4301 Connecticut Ave. NW, Suite 404, Washington, DC 20008. (202) 966-5557. Fax: (202) 966-8553. http://www.geneticalliance.org .
Goldenhar Parent Support Network. Attn: Kayci Rush, 3619 Chicago Ave., Minneapolis, MN 55407-2603. (612) 8233529
Goldenhar Syndrome Research & Information Fund. PO Box 61643, St. Petersburg, FL 33714. (813) 522-5772http://www.goldenhar.com .
Goldenhar Syndrome Support Network 9325 163 St., Edmonton, ALB T5R 2P4. Canada http://i.am/bbds
.page .
National Organization for Rare Disorders (NORD). PO Box 8923, New Fairfield, CT 06812-8923. (203) 746-6518 or (800) 999-6673. Fax: (203) 746-6481. http://www
.rarediseases.org .
WEBSITES
“Oculoauriculovertebral Dysplasia.” Online Mendelian Inheritance in Man. www.ncbi.nlm.nih.gov/entrez/dispomim
.cgi?id=164210 .
Holly Ann Ishmael, MS, CGC
syndrome Goldenhar
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
493 |

Goltz syndrome
I Goltz syndrome
Definition
Goltz syndrome, also known as focal dermal hypoplasia or Goltz-Gorlin syndrome, is a rare form of an abnormal skin condition that is believed to be a dominant, X-linked trait. It is named after R. W. Goltz, who first described this syndrome in 1962.
Description
Goltz syndrome is a genetic condition primarily found in females that affects the appearance and function of the skin. An unrelated syndrome, nevoid basal cell carcinoma syndrome (NBCCS), is also known as GorlinGoltz syndrome. NBCCS is a non-sex linked dominant disorder characterized by a predisposition to cancer, particularly of the basal cells. Care should be taken not to confuse Gorlin-Goltz syndrome with Goltz, or GoltzGorlin, syndrome.
Goltz syndrome has many other synonyms, but it is most often referred to as focal dermal hypoplasia (which can be found in the medical literature abbreviated as FDH, FODH, or DHOF) because of the characteristic, localized (focal) skin (dermal) patches that are thin or absent (hypoplasia). Other synonyms include: combined mesoectodermal dysplasia, congenital ectodermal and mesodermal dysplasia, ectodermal and mesodermal dysplasia with osseous involvement, focal dermal hypoplasia syndrome, and focal dermato-phalangeal dysplasia.
Goltz syndrome is part of a larger family of diseases known as the ectodermal dysplasias, or abnormalities of the skin, hair, teeth, and nails. In Goltz syndrome, the skin abnormalities take the form of areas of thin skin (lesions) where the skin is completely absent, or discolored, itchy, or blistered. Hair may also be missing in patches, and the teeth are usually poorly formed. Nails may also be unusual in appearance. In addition to these characteristics of the skin and related organs, Goltz syndrome affected individuals can also have skeletal malformations and eye problems.
The obvious bodily symptoms of Goltz syndrome are the result of improper functioning of the skin, an organ whose multiple functions are often overlooked. The skin consists of two layers, the outer skin (epidermis) and the lower skin (dermis). The epidermis layer protects the body from environmental threats such as temperature variations, bacterial infections, and toxic chemicals. In Goltz syndrome, the epidermis is deformed or completely absent. The dermis layer contains cells, which manufacture the protein collagen. Collagen makes up about one-fourth of all the body’s protein and plays a
vital role in wound healing, skin and muscle support, and bone formation. In Goltz syndrome, abnormal formation of type IV collagen has been found in the dermis including loose collagen bundles and fibers with loss of regular bands. The importance of collagen for many of the body’s tissues explains the varied symptoms of Goltz syndrome, which is observed in parts of the body as different as the bones, skin, hair, and fingernails.
Genetic profile
The locus of the gene responsible for Goltz syndrome has been localized to the short arm of the X chromosome at locus Xp22.3. At or near this same locus is the gene responsible for microphthalmia with linear skin defects (MLS) and the gene responsible for Aicardi syndrome. Because of the relatively low number of males diagnosed with this condition, it is assumed that Goltz syndrome is dominant and X-linked with close to 100% fetal mortality in males. Nearly all of the cases of Goltz syndrome are believed to result from de novo mutations (new mutations which occur after conception) since parents of affected individuals have normal chromosomes.
Demographics
As of 1998, 150 cases of Goltz syndrome in females and only 11 cases in males were reported in the medical literature. Goltz syndrome is not linked to any particular sub-populations. It appears with equal frequency in all races and across all geographies. Because it is an X- linked dominant condition, it is observed with a much higher frequency in surviving females than it is in surviving males.
Signs and symptoms
Goltz syndrome is characterized by localized areas of malformed skin (skin lesions) that appear underdeveloped, streaked, or absent. The skin of an individual affected with Goltz syndrome may lack color (pigmentation) in the affected areas or, the skin may look streaked with lines (linear pigmentation). The affected areas may look and feel inflamed or irritated in various ways such as by exhibiting itching, blistering, reddening and swelling, and even crusting and bleeding. Fatty deposits (papillomas) are usually present in areas of typically sensitive skin, such as the gums, lips, tongue, armpits, vaginal opening, and the anus. Nodules of yellowish fatty tissue can grow on the affected skin, particularly in skin folds.
People with Goltz syndrome often experience excessive skin growth in the palms of the hands and on the soles of the feet. Because of this overgrowth of skin lay-
494 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
