
- •Preface
- •Contents
- •1 Elements of the Nervous System
- •2 Somatosensory System
- •3 Motor System
- •4 Brainstem
- •5 Cerebellum
- •6 Diencephalon and Autonomic Nervous System
- •7 Limbic System
- •8 Basal Ganglia
- •9 Cerebrum
- •10 Coverings of the Brain and Spinal Cord; Cerebrospinal Fluid and Ventricular System
- •Further Reading
- •Index
- •Abbreviations
- •1 Elements of the Nervous System
- •Elements of the Nervous System
- •Information Flow in the Nervous System
- •Synapses
- •Neurotransmitters and Receptors
- •Functional Groups of Neurons
- •Glial Cells
- •Development of the Nervous System
- •2 Somatosensory System
- •Peripheral Nerve, Dorsal Root Ganglion, Posterior Root
- •Peripheral Regulatory Circuits
- •Central Components of the Somatosensory System
- •Posterior and Anterior Spinocerebellar Tracts
- •Posterior Columns
- •Anterior Spinothalamic Tract
- •Lateral Spinothalamic Tract
- •Other Afferent Tracts of the Spinal Cord
- •Central Processing of Somatosensory Information
- •Somatosensory Deficits due to Lesions at Specific Sites along the Somatosensory Pathways
- •3 Motor System
- •Central Components of the Motor System and Clinical Syndromes of Lesions Affecting Them
- •Motor Cortical Areas
- •Corticospinal Tract (Pyramidal Tract)
- •Corticonuclear (Corticobulbar) Tract
- •Other Central Components of the Motor System
- •Lesions of Central Motor Pathways
- •Peripheral Components of the Motor System and Clinical Syndromes of Lesions Affecting Them
- •Clinical Syndromes of Motor Unit Lesions
- •Complex Clinical Syndromes due to Lesions of Specific Components of the Nervous System
- •Spinal Cord Syndromes
- •Vascular Spinal Cord Syndromes
- •Nerve Root Syndromes (Radicular Syndromes)
- •Plexus Syndromes
- •Peripheral Nerve Syndromes
- •Syndromes of the Neuromuscular Junction and Muscle
- •4 Brainstem
- •Surface Anatomy of the Brainstem
- •Medulla
- •Pons
- •Midbrain
- •Olfactory System (CN I)
- •Visual System (CN II)
- •Eye Movements (CN III, IV, and VI)
- •Trigeminal Nerve (CN V)
- •Facial Nerve (CN VII) and Nervus Intermedius
- •Vagal System (CN IX, X, and the Cranial Portion of XI)
- •Hypoglossal Nerve (CN XII)
- •Topographical Anatomy of the Brainstem
- •Internal Structure of the Brainstem
- •5 Cerebellum
- •Surface Anatomy
- •Internal Structure
- •Cerebellar Cortex
- •Cerebellar Nuclei
- •Connections of the Cerebellum with Other Parts of the Nervous System
- •Cerebellar Function and Cerebellar Syndromes
- •Vestibulocerebellum
- •Spinocerebellum
- •Cerebrocerebellum
- •Cerebellar Tumors
- •6 Diencephalon and Autonomic Nervous System
- •Location and Components of the Diencephalon
- •Functions of the Thalamus
- •Syndromes of Thalamic Lesions
- •Thalamic Vascular Syndromes
- •Epithalamus
- •Subthalamus
- •Hypothalamic Nuclei
- •Afferent and Efferent Projections of the Hypothalamus
- •Functions of the Hypothalamus
- •Sympathetic Nervous System
- •Parasympathetic Nervous System
- •Visceral and Referred Pain
- •7 Limbic System
- •Anatomical Overview
- •Internal and External Connections
- •Microanatomy of the Hippocampal Formation
- •Amygdala
- •Functions of the Limbic System
- •Types of Memory
- •8 Basal Ganglia
- •Preliminary Remarks on Terminology
- •The Role of the Basal Ganglia in the Motor System: Phylogenetic Aspects
- •Connections of the Basal Ganglia
- •Function and Dysfunction of the Basal Ganglia
- •Clinical Syndromes of Basal Ganglia Lesions
- •9 Cerebrum
- •Development
- •Gross Anatomy and Subdivision of the Cerebrum
- •Gyri and Sulci
- •Histological Organization of the Cerebral Cortex
- •Laminar Architecture
- •Cerebral White Matter
- •Projection Fibers
- •Association Fibers
- •Commissural Fibers
- •Functional Localization in the Cerebral Cortex
- •Primary Cortical Fields
- •Association Areas
- •Frontal Lobe
- •Coverings of the Brain and Spinal Cord
- •Dura Mater
- •Arachnoid
- •Pia Mater
- •Cerebrospinal Fluid Circulation and Resorption
- •Arteries of the Anterior and Middle Cranial Fossae
- •Arteries of the Posterior Fossa
- •Collateral Circulation in the Brain
- •Dural Sinuses
- •Venous Drainage
- •Cerebral Ischemia
- •Arterial Hypoperfusion
- •Particular Cerebrovascular Syndromes
- •Impaired Venous Drainage from the Brain
- •Intracranial Hemorrhage
- •Intracerebral Hemorrhage (Nontraumatic)
- •Subarachnoid Hemorrhage
- •Subdural and Epidural Hematoma
- •Impaired Venous Drainage
- •Spinal Cord Hemorrhage and Hematoma
- •Further Reading
- •Index

Intracranial Hemorrhage · 477 11
published case, a patient with a congenitally hypoplastic transverse sinus on one side developed obstruction of the transverse sinus on the opposite side because of a slowly growing meningioma of the sinus wall.
Manifestations. The characteristic manifestations of chronic venous outflow obstruction are headache and papilledema, possibly accompanied by impaired visual acuity. Focal neurological deficits or epileptic seizures are usually not a component of the clinical picture.
Diagnostic evaluation. No parenchymal lesions are seen in the brain (in contrast to acute venous outflow obstruction). MRI sometimes reveals dilatation of the optic nerve sheaths as a result of intracranial hypertension and pressurerelated changes of the sella turcica, but it generally does not show the cause of the impairment of venous outflow. In such cases, intra-arterial digital subtraction angiography is indispensable for the demonstration of circumscribed stenoses and for the assessment of venous flow dynamics. The diagnosis can be confirmed by lumbar puncture with measurement of the cerebrospinal fluid pressure.
Treatment. If etiological treatment is not possible, chronic elevation of the cerebrospinal fluid pressure can be treated by a permanent CSF deviation procedure (lumboperitoneal or ventriculoperitoneal shunt).
Differential diagnosis. Chronic intracranial hypertension is seen with increased frequency in young, overweight women in the absence of an obstruction to venous outflow. The cause of this condition is unknown. Its poorly descriptive traditional name is pseudotumor cerebri.
Intracranial Hemorrhage
Spontaneous, i.e., nontraumatic, bleeding in the brain parenchyma (intracerebral hemorrhage) or the meningeal compartments around it (subarachnoid, subdural, and epidural hemorrhage) accounts for 1520% of clinical strokes, in the wider sense of the term. Although headache and impairment of consciousness occur in intracranial hemorrhage more commonly than in cerebral infarction, clinical criteria alone cannot reliably distinguish hemorrhagic from ischemic stroke. The diagnostic procedure of choice is CT.
An understanding of subarachnoid, subdural, and epidural hemorrhage requires knowledge of the anatomy of the meninges, as described on p. 402ff.
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

11 478 · 11 Blood Supply and Vascular Disorders of the Central Nervous System
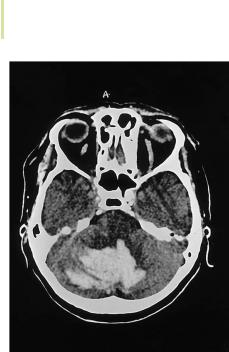
Fig. 11.29 Large left basal ganglionic hemorrhage with midline shift and intraventricular hemorrhage
Intracerebral Hemorrhage (Nontraumatic)
Hypertensive Hemorrhage
Etiology. Themostcommoncauseofintracerebralhemorrhageisarterial hypertension.Pathologicallyelevatedbloodpressuredamagesthewallsofsmallerarteries, creating microaneurysms (Charcot aneurysms) that can rupture spontaneously. Sites of predilection for hypertensive intracerebral hemorrhage are the basal ganglia (Fig. 11.29), the thalamus, the cerebellar nuclei, and the pons. The deep cerebral white matter, on the other hand, is only rarely involved.
Manifestations. The manifestations of intracerebral hemorrhage depend on its location. Basal ganglionic hemorrhage with destruction of the internal capsule usually produces severe contralateral hemiparesis, while pontine hemorrhage produces brainstem signs.
The main danger in intracerebral hemorrhage is intracranial hypertension due to the mass effect of the hematoma. Unlike an infarct, which raises the intracranial pressure slowly as the associated cytotoxic edema worsens, an intracerebral hemorrhage raises it very rapidly. Intraventricular rupture of an intracerebral hemorrhage can cause hydrocephalus, either by obstructing the ventricular outflow with blood clot or by impairing CSF resorption from the arachnoid granulations; if present, hydrocephalus raises the intracranial pressure still further. There is hardly any free space in the posterior fossa, so intraparenchymal hemorrhages below the tentorium rapidly elevate the local intracranial pressure, possibly resulting in herniation of the posterior fossa con-
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

Intracranial Hemorrhage · 479 11
tents, either upward through the tentorial notch, or downward into the foramen magnum. Thus, an intraparenchymal hemorrhage in the brainstem or cerebellum carries a much worse prognosis than an equal-sized hemorrhage in a cerebral hemisphere.
Prognosis and treatment. The brain tissue in an area of hemorrhage (as opposed to an infarct) is generally not totally destroyed; living brain tissue can often be found amid the extravasated blood. This explains why the patient’s neurological deficits usually resolve more rapidly, as the hematoma is resorbed, than they would if produced by an ischemic stroke.
The goal of treatment is, therefore, to preserve whatever brain tissue remains viable in the area of hemorrhage. Persistent intracranial hypertension must be treated to prevent secondary damage, not only of the brain tissue inside and around the hematoma but also of distant tissue. The intracranial pressure can be lowered by pharmacotherapy and/or by neurosurgical removal of the hematoma. Surgery should be performed only when indicated according to strict criteria, taking the patient’s age into account, as well as the location and size of the hematoma. Large-scale studies have shown a therapeutic benefit only from the removal of large hematomas ( 20 cm3). The operative removal of smaller hematomas may actually be detrimental, as it may destroy more viable brain tissue than it saves; and the operative removal of hematomas deep within the brain always involves the destruction of some normal brain tissue along the neurosurgeon’s path to the hematoma. For these reasons, the neurosurgical treatment of smaller intraparenchymal hematomas is limited to the treatment of hydrocephalus (if present) with external ventricular drainage, which can be performed with minimal injury to normal brain tissue. Patients with very large hematomas ( 60 cm3) will not benefit from removal of the hematoma because too much brain tissue has already been destroyed.
Nonhypertensive Intracerebral Hemorrhage
Intracerebral hemorrhage may be due to many causes besides arterial hypertension. The more important ones are arteriovenous malformations, tumors, aneurysms, vascular diseases including vasculitis and amyloid angiopathy, cavernomas, and venous outflow obstruction (as discussed above). An intracerebral hemorrhage is likely to have been caused by something other than arterial hypertension when it is not located at one of the sites of predilection for hypertensive hemorrhage, or when the patient does not suffer from marked arterial hypertension. In such cases (at least), a follow-up MRI scan should be performed once the hematoma is resorbed to detect the underlying cause of hemorrhage. Digital subtraction angiography is sometimes indicated as well.
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
11 480 · 11 Blood Supply and Vascular Disorders of the Central Nervous System
Fig. 11.30 Cerebellar hemorrhage. CT scan of a hypertensive patient who suddenly complained of an intense headache and then became less responsive. A large, hyperdense (bright) hemorrhage is seen in the region of the deep cerebellar nuclei. The brainstem is ventrally displaced and pushed against the clivus, and the prepontine cistern is markedly narrowed.
Cerebellar Hemorrhage
The cerebellar nuclei lie within the distribution of the superior cerebellar artery. One particular branch of this artery, which supplies the dentate nucleus, is particularly susceptible to rupture. In hypertensive individuals, hemorrhage from this vessel is more common than ischemia in its territory (Fig. 11.30).
Hemorrhage in this region often causes acute mass effect in the posterior fossa, with all of its attendant consequences (herniation of the brainstem and cerebellum upward through the tentorial notch and downward into the foramenmagnum).Theclinicalmanifestationsaresevereoccipitalheadache,nausea and vomiting, and vertigo, generally accompanied by unsteady gait, dysarthria, and head turning and gaze deviation to the side opposite the lesion. Large hemorrhages rapidly produce somnolence, stupor, or coma. In the late phase, patients manifest extensor spasms, hemodynamic instability, and, finally, respiratory arrest, unless the posterior fossa can be operatively decompressed.
Smaller hemorrhages, particularly in the cerebellar hemispheres, produce focal manifestations including limb ataxia, a tendency to fall to the side of the lesion, and deviation of gait to the side of the lesion. These manifestations resolve incompletely when the deep cerebellar nuclei are damaged.
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
