
- •Preface
- •Contents
- •1 Elements of the Nervous System
- •2 Somatosensory System
- •3 Motor System
- •4 Brainstem
- •5 Cerebellum
- •6 Diencephalon and Autonomic Nervous System
- •7 Limbic System
- •8 Basal Ganglia
- •9 Cerebrum
- •10 Coverings of the Brain and Spinal Cord; Cerebrospinal Fluid and Ventricular System
- •Further Reading
- •Index
- •Abbreviations
- •1 Elements of the Nervous System
- •Elements of the Nervous System
- •Information Flow in the Nervous System
- •Synapses
- •Neurotransmitters and Receptors
- •Functional Groups of Neurons
- •Glial Cells
- •Development of the Nervous System
- •2 Somatosensory System
- •Peripheral Nerve, Dorsal Root Ganglion, Posterior Root
- •Peripheral Regulatory Circuits
- •Central Components of the Somatosensory System
- •Posterior and Anterior Spinocerebellar Tracts
- •Posterior Columns
- •Anterior Spinothalamic Tract
- •Lateral Spinothalamic Tract
- •Other Afferent Tracts of the Spinal Cord
- •Central Processing of Somatosensory Information
- •Somatosensory Deficits due to Lesions at Specific Sites along the Somatosensory Pathways
- •3 Motor System
- •Central Components of the Motor System and Clinical Syndromes of Lesions Affecting Them
- •Motor Cortical Areas
- •Corticospinal Tract (Pyramidal Tract)
- •Corticonuclear (Corticobulbar) Tract
- •Other Central Components of the Motor System
- •Lesions of Central Motor Pathways
- •Peripheral Components of the Motor System and Clinical Syndromes of Lesions Affecting Them
- •Clinical Syndromes of Motor Unit Lesions
- •Complex Clinical Syndromes due to Lesions of Specific Components of the Nervous System
- •Spinal Cord Syndromes
- •Vascular Spinal Cord Syndromes
- •Nerve Root Syndromes (Radicular Syndromes)
- •Plexus Syndromes
- •Peripheral Nerve Syndromes
- •Syndromes of the Neuromuscular Junction and Muscle
- •4 Brainstem
- •Surface Anatomy of the Brainstem
- •Medulla
- •Pons
- •Midbrain
- •Olfactory System (CN I)
- •Visual System (CN II)
- •Eye Movements (CN III, IV, and VI)
- •Trigeminal Nerve (CN V)
- •Facial Nerve (CN VII) and Nervus Intermedius
- •Vagal System (CN IX, X, and the Cranial Portion of XI)
- •Hypoglossal Nerve (CN XII)
- •Topographical Anatomy of the Brainstem
- •Internal Structure of the Brainstem
- •5 Cerebellum
- •Surface Anatomy
- •Internal Structure
- •Cerebellar Cortex
- •Cerebellar Nuclei
- •Connections of the Cerebellum with Other Parts of the Nervous System
- •Cerebellar Function and Cerebellar Syndromes
- •Vestibulocerebellum
- •Spinocerebellum
- •Cerebrocerebellum
- •Cerebellar Tumors
- •6 Diencephalon and Autonomic Nervous System
- •Location and Components of the Diencephalon
- •Functions of the Thalamus
- •Syndromes of Thalamic Lesions
- •Thalamic Vascular Syndromes
- •Epithalamus
- •Subthalamus
- •Hypothalamic Nuclei
- •Afferent and Efferent Projections of the Hypothalamus
- •Functions of the Hypothalamus
- •Sympathetic Nervous System
- •Parasympathetic Nervous System
- •Visceral and Referred Pain
- •7 Limbic System
- •Anatomical Overview
- •Internal and External Connections
- •Microanatomy of the Hippocampal Formation
- •Amygdala
- •Functions of the Limbic System
- •Types of Memory
- •8 Basal Ganglia
- •Preliminary Remarks on Terminology
- •The Role of the Basal Ganglia in the Motor System: Phylogenetic Aspects
- •Connections of the Basal Ganglia
- •Function and Dysfunction of the Basal Ganglia
- •Clinical Syndromes of Basal Ganglia Lesions
- •9 Cerebrum
- •Development
- •Gross Anatomy and Subdivision of the Cerebrum
- •Gyri and Sulci
- •Histological Organization of the Cerebral Cortex
- •Laminar Architecture
- •Cerebral White Matter
- •Projection Fibers
- •Association Fibers
- •Commissural Fibers
- •Functional Localization in the Cerebral Cortex
- •Primary Cortical Fields
- •Association Areas
- •Frontal Lobe
- •Coverings of the Brain and Spinal Cord
- •Dura Mater
- •Arachnoid
- •Pia Mater
- •Cerebrospinal Fluid Circulation and Resorption
- •Arteries of the Anterior and Middle Cranial Fossae
- •Arteries of the Posterior Fossa
- •Collateral Circulation in the Brain
- •Dural Sinuses
- •Venous Drainage
- •Cerebral Ischemia
- •Arterial Hypoperfusion
- •Particular Cerebrovascular Syndromes
- •Impaired Venous Drainage from the Brain
- •Intracranial Hemorrhage
- •Intracerebral Hemorrhage (Nontraumatic)
- •Subarachnoid Hemorrhage
- •Subdural and Epidural Hematoma
- •Impaired Venous Drainage
- •Spinal Cord Hemorrhage and Hematoma
- •Further Reading
- •Index
Central Components of the Somatosensory System · 47 |
2 |
|
|
The loss of proprioceptive sense can be compensated for, to a considerable extent, by opening the eyes (which is not the case, for example, in a patient with a cerebellar lesion).
The fibers in the posterior columns originate in the pseudounipolar neurons of the spinal ganglia, but the fibers in the anterior and posterior spinothalamic tracts do not; they are derived from the second neurons of their respective pathways, which are located within the spinal cord (Fig. 2.16c,d, p. 42).
Anterior Spinothalamic Tract
The impulses arise in cutaneous receptors (peritrichial nerve endings, tactile corpuscles) and are conducted along a moderately thickly myelinated peripheral fiber to the pseudounipolar dorsal root ganglion cells, and thence by way of the posterior root into the spinal cord. Inside the cord, the central processes of the dorsal root ganglion cells travel in the posterior columns some 215 segments upward, while collaterals travel 1 or 2 segments downward, making synaptic contact onto cells at various segmental levels in the gray matter of the posterior horn (Fig. 2.16c, p. 42). These cells (the second neurons) then give rise to the anterior spinothalamic tract, whose fibers cross in the anterior spinal commissure, ascend in the contralateral anterolateral funiculus, and terminate in the ventral posterolateral nucleus of the thalamus, together with the fibers of the lateral spinothalamic tract and the medial lemniscus (Fig. 2.17, p. 43). The third neurons in this thalamic nucleus then project their axons to the postcentral gyrus in the thalamocortical tract.
Lesions of the anterior spinothalamic tract. As explained above, the central fibers of the first neurons of this tract ascend a variable distance in the ipsilateral posterior columns, giving off collaterals along the way to the second neurons, whose fibers then cross the midline and ascend further in the contralateral anterior spinothalamic tract. It follows that a lesion of this tract at a lumbar or thoracic level generally causes minimal or no impairment of touch, because many ascending impulses can circumvent the lesion by way of the ipsilateral portion of the pathway. A lesion of the anterior spinothalamic tract at a cervical level, however, will produce mild hypesthesia of the contralateral lower limb.
Lateral Spinothalamic Tract
The free nerve endings of the skin are the peripheral receptors for noxious and thermal stimuli. These endings constitute the end organs of thin group A fibers and of nearly unmyelinated group C fibers that are, in turn, the peripheral
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

248 · 2 Somatosensory System
processes of pseudounipolar neurons in the spinal ganglia. The central processes pass in the lateral portion of the posterior roots into the spinal cord and then divide longitudinally into short collaterals that terminate within one or two segments in the substantia gelatinosa, making synaptic contact with funicular neurons (second neurons) whose processes form the lateral spinothalamic tract (Fig. 2.16d, p. 42). These processes cross the midline in the anterior spinal commissure before ascending in the contralateral lateral funiculus to the thalamus. Like the posterior columns, the lateral spinothalamic tract is somatotopically organized; here, however, the fibers from the lower limb lie laterally, while those from the trunk and upper limb lie more medially (Fig. 2.20).
The fibers mediating pain and temperature sensation lie so close to each other that they cannot be anatomically separated. Lesions of the lateral spinothalamic tract thus impair both sensory modalities, though not always to the same degree.
Central continuation of the lateral spinothalamic tract. The fibers of the lateral
spinothalamic tract travel up through the brainstem together with those of the medial lemniscus in the spinal lemniscus, which terminates in the ventral posterolateral nucleus of the thalamus (VPL, p. 265; see Fig. 6.4, p. 266, and Fig. 2.19). The third neurons in the VPL project via the thalamocortical tract to the postcentral gyrus in the parietal lobe (Fig. 2.19). Pain and temperature are perceived in a rough manner in the thalamus, but finer distinctions are not made until the impulses reach the cerebral cortex.
Lesions of the lateral spinothalamic tract. The lateral spinothalamic tract is the main pathway for pain and temperature sensation. It can be neurosurgically transected to relieve pain (cordotomy); this operation is much less commonly performed today than in the past, because it has been supplanted by less invasive methods and also because the relief it provides is often only temporary. The latter phenomenon, long recognized in clinical experience, suggests that pain-related impulses might also ascend the spinal cord along other routes, e. g., in spinospinal neurons belonging to the fasciculus proprius.
If the lateral spinothalamic tract is transected in the ventral portion of the spinal cord, pain and temperature sensation are deficient on the opposite side one or two segments below the level of the lesion, while the sense of touch is preserved (dissociated sensory deficit).
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
|
Central Components of the Somatosensory System · 49 |
2 |
||||
|
Posterior funiculus |
|
|
|
|
|
|
Fasciculus |
Fasciculus |
|
|
Semilunar tract |
|
Substantia gelatinosa |
|
|
(comma of Schultz) |
|
||
cuneatus |
gracilis |
|
|
|
||
Dorsolateral tract |
(of Goll) |
|
|
|
|
|
(of Burdach) |
S |
L |
|
|
||
(Lissauer’s tract) |
|
|
|
T |
|
|
|
|
|
|
|
||
Posterior spinocerebellar |
|
|
|
|
C |
|
|
|
|
|
|
|
|
tract |
|
|
|
|
|
|
Lateral corticospinal tract
Thoracic nucleus
Rubrospinal and reticulospinal tracts
X
Reticular formation Anterior spinocerebellar tract
Lateral spinothalamic tract
Olivospinal tract Spinotectal tract Spino-olivary tract
Anterior spinothalamic tract
Vestibulospinal tract
Reticulospinal tract Tectospinal tract
Anterior corticospinal tract
I–III |
S |
|
|
|
|
||
IV |
|
L |
Lo |
|
|
|
|
V |
|
T |
|
wer |
|
|
|
VI |
|
T |
|
lim |
|
||
|
|
|
|
||||
|
Up |
ru |
|
b |
|
||
|
C |
|
n |
|
|
|
|
|
per |
k |
|
|
|
||
|
|
|
|
|
|||
|
|
|
|
|
|
||
|
|
|
l |
|
|
|
|
|
|
|
im |
|
|
S |
|
VII |
|
|
b |
|
|
||
|
|
|
C |
T |
L |
|
|
|
|
|
|
|
|||
VIII |
|
|
|
|
|
|
|
IX |
|
|
|
|
|
|
|
Pressure |
|
|
|
|
|
Pain |
Temperature |
|
|
|
|
|
|
|
|
Touch
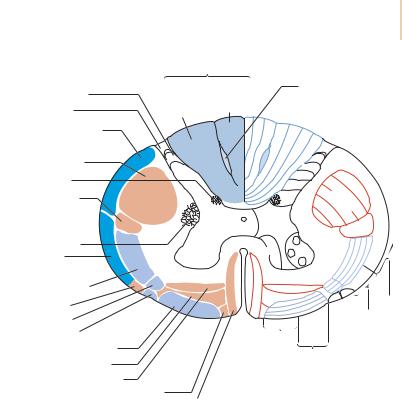
Fig. 2.20 Somatotopic organization of spinal cord tracts in cross section. The laminae of Rexed are also designated with Roman numerals (cytoarchitectural organization of the spinal gray matter).
Other Afferent Tracts of the Spinal Cord
In addition to the spinocerebellar and spinothalamic tracts discussed above, the spinal cord contains yet other fiber pathways ascending to various target structuresinthebrainstemanddeepsubcorticalnuclei.Thesepathways,whichoriginate in the dorsal horn of the spinal cord (second afferent neuron) and ascend in its anterolateral funiculus, include the spinoreticular, spinotectal, spino-olivary, and spinovestibular tracts. The spinovestibular tract is found in the cervical spinal cord, from C4 upward, in the area of the (descending) vestibulospinal tract and is probably a collateral pathway of the posterior spinocerebellar tract.
Figure 2.20 is a schematic drawing of the various sensory (ascending) tracts, as seen in a cross section of the spinal cord. The motor (descending) tracts are
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

250 · 2 Somatosensory System
also indicated, so that the spatial relationships between the various tracts can be appreciated. Finally, in addition to the ascending and descending tracts, the spinal cord also contains a so-called intrinsic apparatus, consisting of neurons that project upward and downward over several spinal segments in the fasciculus proprius (Fig. 2.9, p. 31).
Central Processing of Somatosensory Information
Figure 2.17 traces all of the sensory pathways discussed above, in schematically simplified form and in spatial relation to one another, as they ascend from the posterior roots to their ultimate targets in the brain. The sensory third neurons in the thalamus send their axons through the posterior limb of the internal capsule (posterior to the pyramidal tract) to the primary somatosensory cortex, which is located in the postcentral gyrus (Brodmann cytoarchitectural areas 3a, 3b, 2, and 1). The third neurons that terminate here mediate superficial sensation, touch, pressure, pain, temperature, and (partly) proprioception (Fig. 2.19, p. 46).
Sensorimotor integration. In fact, not all of the sensory afferent fibers from the thalamus terminate in the somatosensory cortex; some terminate in the primary motor cortex of the precentral gyrus. Thus, the sensory and motor cortical fields overlap to some extent, so that the precentral and postcentral gyri are sometimes together designated the sensorimotor area. The integration of function occurring here enables incoming sensory information to be immediately converted to outgoing motor impulses in sensorimotor regulatory circuits, about which we will have more to say later. The descending pyramidal fibers emerging from these circuits generally terminate directly—without any intervening interneurons—on motor neurons in the anterior horn. Finally, even though their functions overlap, it should be remembered that the precentral gyrus remains almost entirely a motor area, and the postcentral gyrus remains almost entirely a (somato)sensory area.
Differentiation of somatosensory stimuli by their origin and quality. It has already been mentioned that somatosensory representation in the cerebral cortex is spatially segregated in somatotopic fashion: the inverted sensory homunculus has been encountered in Figure 2.19 and will be seen again in Figure 9.19, p. 374. But somatosensory representation in the cerebral cortex is also spatially segregated by modality: pain, temperature, and the other modalities are represented by distinct areas of the cortex.
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
