
- •Table of Contents
- •Copyright
- •Dedication
- •Introduction to the eighth edition
- •Online contents
- •List of Illustrations
- •List of Tables
- •1. Pulmonary anatomy and physiology: The basics
- •Anatomy
- •Physiology
- •Abnormalities in gas exchange
- •Suggested readings
- •2. Presentation of the patient with pulmonary disease
- •Dyspnea
- •Cough
- •Hemoptysis
- •Chest pain
- •Suggested readings
- •3. Evaluation of the patient with pulmonary disease
- •Evaluation on a macroscopic level
- •Evaluation on a microscopic level
- •Assessment on a functional level
- •Suggested readings
- •4. Anatomic and physiologic aspects of airways
- •Structure
- •Function
- •Suggested readings
- •5. Asthma
- •Etiology and pathogenesis
- •Pathology
- •Pathophysiology
- •Clinical features
- •Diagnostic approach
- •Treatment
- •Suggested readings
- •6. Chronic obstructive pulmonary disease
- •Etiology and pathogenesis
- •Pathology
- •Pathophysiology
- •Clinical features
- •Diagnostic approach and assessment
- •Treatment
- •Suggested readings
- •7. Miscellaneous airway diseases
- •Bronchiectasis
- •Cystic fibrosis
- •Upper airway disease
- •Suggested readings
- •8. Anatomic and physiologic aspects of the pulmonary parenchyma
- •Anatomy
- •Physiology
- •Suggested readings
- •9. Overview of diffuse parenchymal lung diseases
- •Pathology
- •Pathogenesis
- •Pathophysiology
- •Clinical features
- •Diagnostic approach
- •Suggested readings
- •10. Diffuse parenchymal lung diseases associated with known etiologic agents
- •Diseases caused by inhaled inorganic dusts
- •Hypersensitivity pneumonitis
- •Drug-induced parenchymal lung disease
- •Radiation-induced lung disease
- •Suggested readings
- •11. Diffuse parenchymal lung diseases of unknown etiology
- •Idiopathic pulmonary fibrosis
- •Other idiopathic interstitial pneumonias
- •Pulmonary parenchymal involvement complicating systemic rheumatic disease
- •Sarcoidosis
- •Miscellaneous disorders involving the pulmonary parenchyma
- •Suggested readings
- •12. Anatomic and physiologic aspects of the pulmonary vasculature
- •Anatomy
- •Physiology
- •Suggested readings
- •13. Pulmonary embolism
- •Etiology and pathogenesis
- •Pathology
- •Pathophysiology
- •Clinical features
- •Diagnostic evaluation
- •Treatment
- •Suggested readings
- •14. Pulmonary hypertension
- •Pathogenesis
- •Pathology
- •Pathophysiology
- •Clinical features
- •Diagnostic features
- •Specific disorders associated with pulmonary hypertension
- •Suggested readings
- •15. Pleural disease
- •Anatomy
- •Physiology
- •Pleural effusion
- •Pneumothorax
- •Malignant mesothelioma
- •Suggested readings
- •16. Mediastinal disease
- •Anatomic features
- •Mediastinal masses
- •Pneumomediastinum
- •Suggested readings
- •17. Anatomic and physiologic aspects of neural, muscular, and chest wall interactions with the lungs
- •Respiratory control
- •Respiratory muscles
- •Suggested readings
- •18. Disorders of ventilatory control
- •Primary neurologic disease
- •Cheyne-stokes breathing
- •Control abnormalities secondary to lung disease
- •Sleep apnea syndrome
- •Suggested readings
- •19. Disorders of the respiratory pump
- •Neuromuscular disease affecting the muscles of respiration
- •Diaphragmatic disease
- •Disorders affecting the chest wall
- •Suggested readings
- •20. Lung cancer: Etiologic and pathologic aspects
- •Etiology and pathogenesis
- •Pathology
- •Suggested readings
- •21. Lung cancer: Clinical aspects
- •Clinical features
- •Diagnostic approach
- •Principles of therapy
- •Bronchial carcinoid tumors
- •Solitary pulmonary nodule
- •Suggested readings
- •22. Lung defense mechanisms
- •Physical or anatomic factors
- •Antimicrobial peptides
- •Phagocytic and inflammatory cells
- •Adaptive immune responses
- •Failure of respiratory defense mechanisms
- •Augmentation of respiratory defense mechanisms
- •Suggested readings
- •23. Pneumonia
- •Etiology and pathogenesis
- •Pathology
- •Pathophysiology
- •Clinical features and initial diagnosis
- •Therapeutic approach: General principles and antibiotic susceptibility
- •Initial management strategies based on clinical setting of pneumonia
- •Suggested readings
- •24. Bacterial and viral organisms causing pneumonia
- •Bacteria
- •Viruses
- •Intrathoracic complications of pneumonia
- •Respiratory infections associated with bioterrorism
- •Suggested readings
- •25. Tuberculosis and nontuberculous mycobacteria
- •Etiology and pathogenesis
- •Definitions
- •Pathology
- •Pathophysiology
- •Clinical manifestations
- •Diagnostic approach
- •Principles of therapy
- •Nontuberculous mycobacteria
- •Suggested readings
- •26. Miscellaneous infections caused by fungi, including Pneumocystis
- •Fungal infections
- •Pneumocystis infection
- •Suggested readings
- •27. Pulmonary complications in the immunocompromised host
- •Acquired immunodeficiency syndrome
- •Pulmonary complications in non–HIV immunocompromised patients
- •Suggested readings
- •28. Classification and pathophysiologic aspects of respiratory failure
- •Definition of respiratory failure
- •Classification of acute respiratory failure
- •Presentation of gas exchange failure
- •Pathogenesis of gas exchange abnormalities
- •Clinical and therapeutic aspects of hypercapnic/hypoxemic respiratory failure
- •Suggested readings
- •29. Acute respiratory distress syndrome
- •Physiology of fluid movement in alveolar interstitium
- •Etiology
- •Pathogenesis
- •Pathology
- •Pathophysiology
- •Clinical features
- •Diagnostic approach
- •Treatment
- •Suggested readings
- •30. Management of respiratory failure
- •Goals and principles underlying supportive therapy
- •Mechanical ventilation
- •Selected aspects of therapy for chronic respiratory failure
- •Suggested readings
- •Index
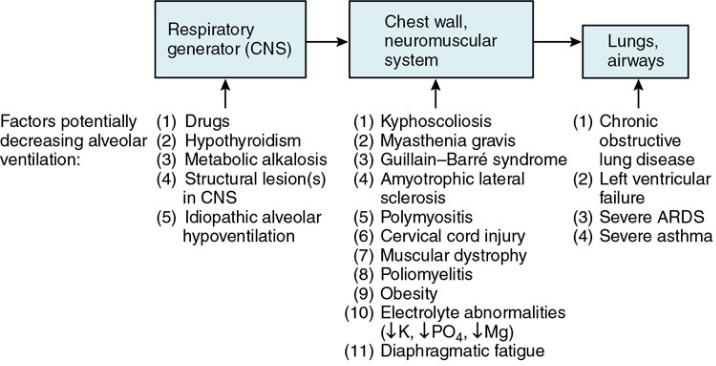
FIGURE 28.1 Levels at which interference with normal ventilation give rise to
alveolar hypoventilation. Factors contributing to decreased ventilation are listed
under each level. ARDS, acute respiratory distress syndrome; CNS, central nervous
system.
In the hypercapnic form of respiratory failure, hypoventilation also leads to a decrease in alveolar PO2. As a result, arterial PO2 falls even if ventilation-perfusion matching and gas exchange at the alveolar level are well maintained. In practice, however, many of the diseases associated with alveolar hypoventilation, ranging from neuromuscular and chest wall disease to chronic airflow obstruction, are accompanied by significant ventilation-perfusion mismatch. Therefore, patients generally have two major reasons for hypoxemia: hypoventilation and ventilation-perfusion mismatch. Interestingly, true shunts usually play a limited role in causing hypoxemia in these disorders, unlike the situation in ARDS.
Given the causes of hypoxemia in the hypercapnic/hypoxemic form of respiratory failure, patients frequently respond to supplemental O2 with a substantial rise in arterial PO2. However, most of these patients have at least mild chronic CO2 retention, with their acute respiratory failure resulting from some precipitating insult or worsening of their underlying disease. Administration of supplemental O2 to these chronically hypercapnic patients may lead to a further increase in arterial PCO2 for a number of pathophysiologic reasons (see Chapter 18). With judicious use of supplemental O2, substantial additional elevation of arterial PCO2 can usually be avoided.
An elaboration of further features of the hypercapnic/hypoxemic form of respiratory failure follows.
Clinical and therapeutic aspects of hypercapnic/hypoxemic respiratory failure
Whether the underlying disease is chest wall disease (e.g., kyphoscoliosis) or COPD, this type of respiratory failure often develops in patients who already have some degree of chronic respiratory insufficiency. However, this is not true of all cases. In certain neurologic conditions such as Guillain-

Barré syndrome, hypercapnic respiratory failure occurs in a previously healthy, eucapnic individual. As noted earlier, when the patient has chronic disease upon which acute respiratory failure is superimposed, the phrase acute-on-chronic respiratory failure is frequently used. In such cases, a
specific different problem often precipitates the acute deterioration, and identification of the problem is important.
Frequent precipitants of acute-on-chronic respiratory failure:
1.Respiratory infection
2.Drugs (e.g., sedatives, narcotics)
3.Heart failure
4.Exacerbation of underlying neuromuscular disease (e.g., myasthenic crisis)
What are some of the intercurrent problems or factors that precipitate acute respiratory failure in these patients? Perhaps the most common is an acute respiratory infection, such as bronchitis, usually caused by a virus. However, bacterial causes must always be considered because they are amenable to antibiotic therapy. The use of drugs that suppress the respiratory center, such as sedatives or narcotics, may precipitate hypercapnic respiratory failure by depressing central respiratory drive in a person whose condition already was marginal. Other intercurrent problems include heart failure, pulmonary emboli, and exposure to environmental pollutants, each of which may be sufficient to induce further CO2 retention in the patient with previously borderline compensation.
The general therapeutic approach to these patients has three main components: (1) support of gas exchange, (2) treatment of the acute precipitating event, and (3) treatment of the underlying pulmonary disease. The support of gas exchange involves maintaining adequate oxygenation and elimination of CO2 (see Chapter 30). Briefly, supplemental O2, generally in a concentration only slightly higher than that found in ambient air, is administered to raise PO2 and SaO2 to acceptable levels (i.e., more than 60 mm Hg and more than 90%, respectively). If CO2 elimination deteriorates and PCO2 rises much beyond its usual level, then an acute respiratory acidosis is superimposed on the patient’s usual acid-base status. If significant acidemia develops or if the patient’s mental status changes significantly due to CO2 retention, some form of ventilatory assistance, either intubation and mechanical ventilation or noninvasive positivepressure ventilation with a mask, may be required.
Treating the factor precipitating acute respiratory failure is most successful when bacterial infection or heart failure is responsible for the acute deterioration. Antibiotics for suspected bacterial infection, or diuretics and afterload reduction for heart failure, are appropriate forms of therapy in these circumstances. For patients in whom respiratory secretions seem to be playing a role either chronically or in an acute exacerbation of their disease, attempts to assist with clearance of secretions may be beneficial. In particular, chest physical therapy, in which percussion and vibration of the chest are performed and cough is assisted mechanically, may be beneficial.
Treatment of the underlying pulmonary disease depends on the nature of the disease. For patients with obstructive lung disease, intensive therapy with bronchodilators and corticosteroids may be helpful in reversing whatever components of bronchoconstriction and inflammation are present. If neuromuscular or chest wall disease is the underlying problem, specific therapy may be available, as is the case with myasthenia gravis. Unfortunately, for many neuromuscular or chest wall diseases, no specific form of therapy exists, and support of gas exchange and treatment of any precipitating factors are the major modes of therapy.
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/
When patients with irreversible chest wall or neuromuscular disease are in frank respiratory failure, they may require some form of ventilatory assistance on a chronic basis. (Modalities for chronic ventilatory support are discussed in Chapter 30.) It is important to emphasize that the primary decision to be made is whether chronic ventilatory support is acceptable to a patient with this type of irreversible disease. In many cases the patient, family, and physician make the joint decision that life should not be prolonged with chronic ventilator support, given the projected poor quality of life and irreversible nature of the process.
Suggested readings
General
Böing S. & Randerath W.J. Chronic hypoventilation syndromes and sleep-related hypoventilation Journal of Thoracic Disease 2015;7: 1273-1285.
Dupuy-McCauley K. & Selim B. Perioperative care and medication-related hypoventilation
Sleep Medicine Clinics 2020;15: 471-483.
Levy M.M. Pathophysiology of oxygen delivery in respiratory failure Chest 5 Suppl. 2, 2005;128: 547S553S.
Narendra D.K, Hess D.R, Sessler C.N, Belete H.M, Guntupalli K.K, Khusid F., et al. Update in management of severe hypoxemic respiratory failure Chest 2017;152: 867-879.
Pierce A.M. & Brown L.K. Obesity hypoventilation syndrome: Current theories of pathogenesis Current Opinion in Pulmonary Medicine 2015;21: 557-562.
Pisani L, Corcione N. & Nava S. Management of acute hypercapnic respiratory failure
Current Opinion in Critical Care 2016;22: 45-52.
Simonds A.K. Chronic hypoventilation and its management European Respiratory Review 2013;22: 325-332.
Weinberger S.E, Schwartzstein R.M. & Weiss J.W. Hypercapnia New England Journal of Medicine 1989;321: 1223-1231.
Williams R, Salt G, Jackson T, Mazur L, Briceno N, Clapp B., et al. Severe respiratory failure Lancet 10057, 2016;388: e12.
Respiratory failure in obstructive lung disease
Bergin S.P. & Rackley C.R. Managing respiratory failure in obstructive lung disease Clinics in Chest Medicine 2016;37: 659-667.
Duiverman M.L, Arellano-Maric M.P. & Windisch W. Long-term noninvasive ventilation in patients with chronic hypercapnic respiratory failure: Assisting the diaphragm, but threatening the heart? Current Opinion in Pulmonary Medicine 2016;22: 130-137.
McNicholas W.T. COPD-OSA overlap syndrome: Evolving evidence regarding epidemiology, clinical consequences, and management Chest 2017;152: 1318-1326.
O’Donnell D.E, Ciavaglia C.E. & Neder J.A. When obesity and chronic obstructive pulmonary disease collide. Physiological and clinical consequences Annals of the American Thoracic Society 2014;11: 635-644.
O’Donnell D.E. & Parker C.M. COPD exacerbations. 3: Pathophysiology Thorax 2006;61: 354-361.

Robinson T.D, Freiberg D.B, Regnis J.A. & Young I.H. The role of hypoventilation and ventilation-perfusion redistribution in oxygen-induced hypercapnia during acute exacerbations of chronic obstructive pulmonary disease American Journal of Respiratory and Critical Care Medicine 2000;161: 1524-1529.
Respiratory failure in neuromuscular and chest wall disease
Boentert M, Wenninger S. & Sansone V.A. Respiratory involvement in neuromuscular disorders Current Opinion in Neurology 2017;30: 529-537.
Hocker S. Primary acute neuromuscular respiratory failure Neurologic Clinics 2017;35: 707-721.
Seneviratne J, Mandrekar J, Wijdicks E.F. & Rabinstein A.A. Noninvasive ventilation in myasthenic crisis Archives of Neurology 2008;65: 54-58.
Singh T.D. & Wijdicks E.F.M. Neuromuscular respiratory failure Neurologic Clinics 2021;39: 333-353.
Wenninger S. & Jones H.N. Hypoventilation syndrome in neuromuscular disorders Current Opinion in Neurology 2021;34: 686-696.
1
The abbreviation ARDS formerly was used for adult respiratory distress syndrome, but acute has now replaced adult because the entity can occur in individuals of any age.
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/
