
Полезные материалы за все 6 курсов / Учебники, методички, pdf / INBDEBooster Oral Pathology
.pdf
INBDE ORAL PATHOLOGY NOTES |
1 |
Oral Pathology
Oral pathology is one of the focuses of the INBDE that requires candidates to draw upon their knowledge of diseases of the teeth, gums, bones, joints, glands, skin, and muscles around the mouth and relate them to appropriate diagnoses and treatments. The following notes cover high-yield information to know for the oral pathology portion of the INBDE, as well as helpful mnemonics and pictures to solidify understanding!
1Developmental & Hereditary Conditions
Having a good grasp of oral pathologies and understanding of disease etiologies can make a world of a difference in how efficiently a dentist can identify and monitor oral diseases. We start off our discussion with learning about developmental and hereditary conditions — conditions that may not necessarily be a result of choices we make during our lives as is seen in a number of other diseases of the oral cavity.
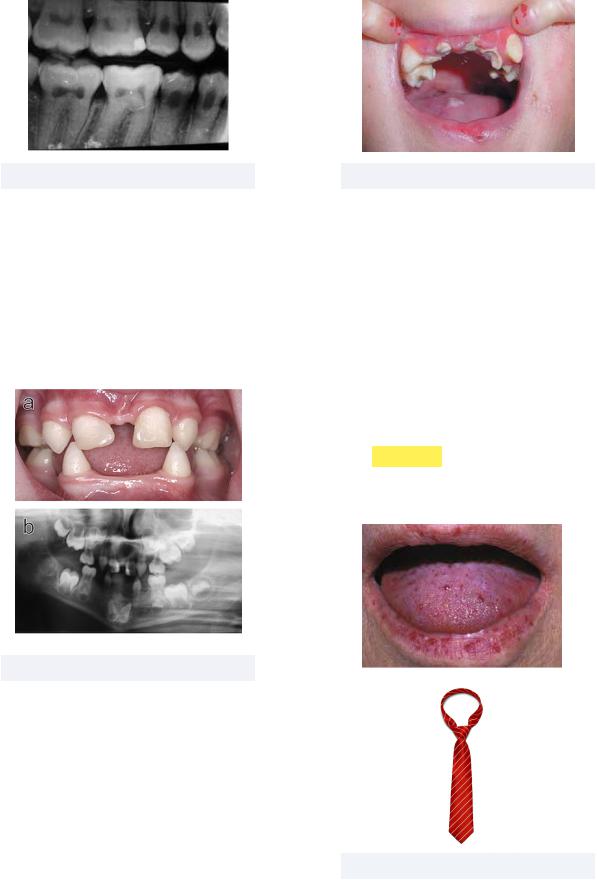
•Cleft Lip - an opening or split between the medial nasal process and maxillary process, embryological structures that should normally fuse together
Must know: Can present as unilateral (seen in 80% of cases) or bilateral (seen in 20% of cases)
-Cleft palate is similar to cleft lip, however this defines a lack of fusion between the palatal shelf embryological structures
Prevalence: Very rare, with fewer than 20,000 US cases per year
Treatment: Surgery restores normal function, speech therapy may be helpful
Figure 1.01 Cleft lip
• Fordyce Granules - ectopic sebaceous glands found on the vermillion border of the lips or around the oral cavity
Must know: Often most prominent around puberty, these granules appear as yellow-white papules that may be hyperplastic or nodular
Prevalence: Common, occurs in 70-80% of adults
Treatment: Completely benign, no treatment necessary
Figure 1.02 Fordyce granules
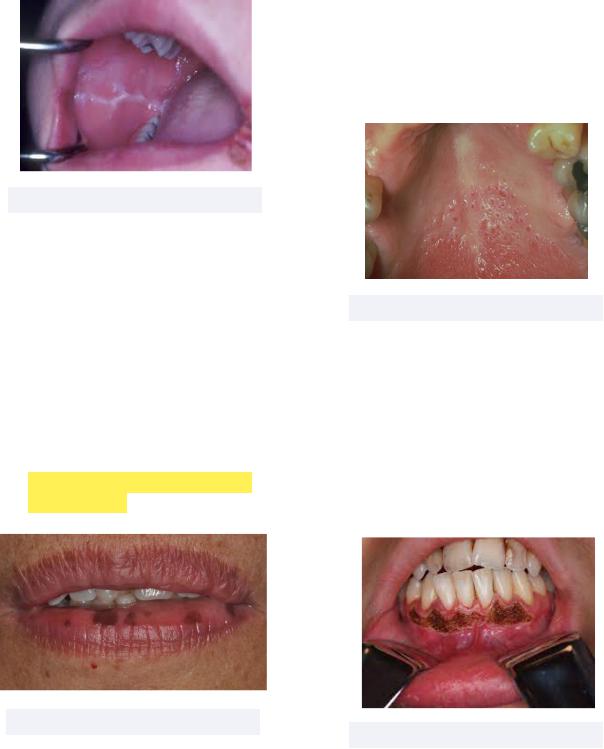
•Fissured Tongue - deep and prominent grooves and fissures across the tongue surface
Must know: benign condition
-Melkersson-Rosenthal Syndrome (MRS) is a rare neurological disorder that includes a fissured tongue, granulomatous cheilitis, and facial paralysis as main characteristics
Prevalence: Common, affects 2-5% of US population
Treatment: None
INBDE Booster | Booster PrepTM

INBDE ORAL PATHOLOGY NOTES |
2 |
Figure 1.03 Fissured tongue
•Geographic Tongue - aka erythema migrans, loss of papillae resulting in red patches that migrate over time (like the Pangea continental drift)
Must know: aka benign migratory glossitis and erythema migrans
-Look for a characteristic white ringed lesion surrounding the red patches
Prevalence: Very common with more than 3 million US cases per year
Treatment: None if asymptomatic, topical corticosteroid if symptomatic
Figure 1.04 Geographic tongue
•Leukoedema - white or white/gray swollen fluid lesion of buccal or labial oral mucosa
Must know: the lesion dissipates when tissue is stretched, as a result of the edematous quality of the lesion
Prevalence: Somewhat rare; mostly seen among black men
Treatment: Completely benign, no treatment necessary
Figure 1.05 Leukoedema
•Lingual Thyroid - mass of thyroid tissue at midline base of tongue
Must know: located along embryonic path of embryonic descent; can be found between foramen cecum of tongue and just past the larynx
-If found past the foramen cecum, the condition is known as a thyroglossal duct cyst, and may be visible on the skin surface
Prevalence: Very rare, reported incidence of 1 in 100,000
Treatment: Surgical methods include excision or autotransplantation into muscle; non-surgical methods include hormonal therapy or radioactive ablation
Figure 1.06 Lingual thyroid
Figure 1.07 Thyroglossal duct cyst
INBDE Booster | Booster PrepTM
INBDE ORAL PATHOLOGY NOTES
•Lip Pits - pits and fistulas that occur near lip commissures or midline
Must know: Van der Woude Syndrome defines a condition in which the patient presents cleft lip/palate as well as lip pits
Prevalence: Very rare, with incidence of about 1 in 75,000 to 1 in 100,000
Treatment: Usually doesn’t require treatment, but surgical excision may be necessary for more severe cases
Figure 1.08 Lip pits
Still discussing developmental conditions, we now shift our attention to angiomas, or benign tumors that consist of small blood or lymph vessels. Angiomas can be present on the skin surface or inside the oral cavity. Surface angiomas include cherry angioma, or a small red mole that forms from accumulated capillaries and vessels, and hemangioma, a bright red birthmark that appears at birth that is made up of extra blood vessels in the skin.
Figure 1.09 Hemangioma vs cherry angioma
3
The oral angioma to know in detail is as follows:
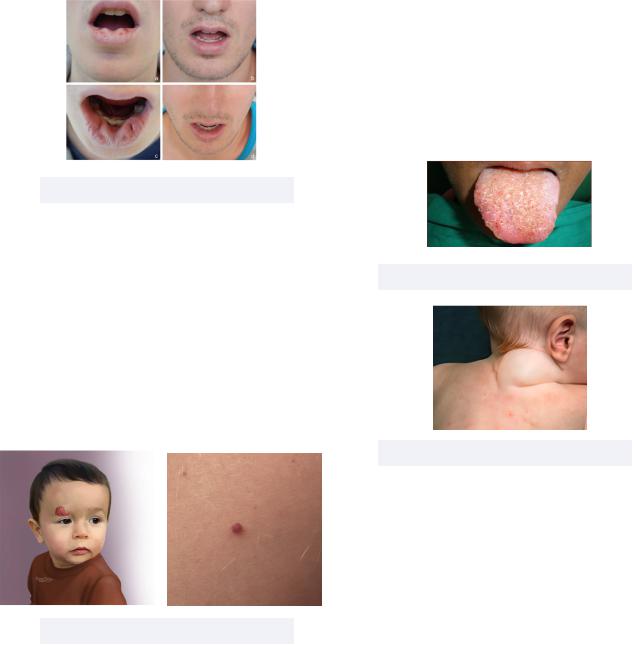
•Oral Lymphangioma - congenital abnormal proliferation of lymphatic vessels on the tongue
Must know:
-Referred to as cystic hygroma when occurs in the neck (more common than oral lymphangioma)
-A syndrome involving lymphangioma is
Sturge-Weber Syndrome, in which angiomas form on the leptomeninges and skin along the trigeminal nerve
Prevalence: Very rare, 1-2/1000 newborns
Treatment: Surgical excision, radiation therapy, or steroid administration are common treatments
Figure 1.10 Oral lymphangioma
Figure 1.11 Cystic hygroma
Another category of developmental conditions to know for the INBDE include exostoses (or tori) which are incidences of excessive cortical bone growth. Exostoses are named primarily based on where they occur, such as buccal exostosis, or toris mandibularis, a bony overgrowth on the lingual aspect of the mandible.
INBDE Booster | Booster PrepTM

INBDE ORAL PATHOLOGY NOTES
Figure 1.12 Buccal exostosis and torus palatinus
We transition our discussion of developmental conditions to learning about different types of cysts, which are abnormal, usually noncancerous growths filled with liquid, air or other substances. Make sure to know the following conditions!
•Branchial Cyst - cyst within lymph node of the neck that ‘branches’ out from branchial cleft
Must know: also known as cleft sinus
Prevalence: Most common congenital cause of neck mass; exact incidence is unknown
Treatment: Either surgical removal or drainage of fluid
4
-Dermoid cysts can contain structures such as hair, fluid, teeth, or skin glands, and have a very doughy consistency
Prevalence: Common, mostly found in children ages 5 and younger
Treatment: Surgical removal
Figure 1.14 Dermoid cyst
•Globulomaxillary Lesion - a cyst appearing between a maxillary lateral incisor and the adjacent canine
Must know: appears as inverted pearshaped radiolucency
-Can cause roots of adjacent teeth to diverge
-Not a diagnosis, and not considered a distinct, classifiable entity
Prevalence: N/A
Treatment: Surgical removal
Figure 1.13 Branchial cyst
•Dermoid Cyst - mass of tissue collecting under the skin that usually appear at birth
Must know: depending on whether the cyst forms above the mylohyoid bone or below, it will be on the floor of the mouth (above) or in the upper neck (below)
Figure 1.15 Globulomaxillary Lesion
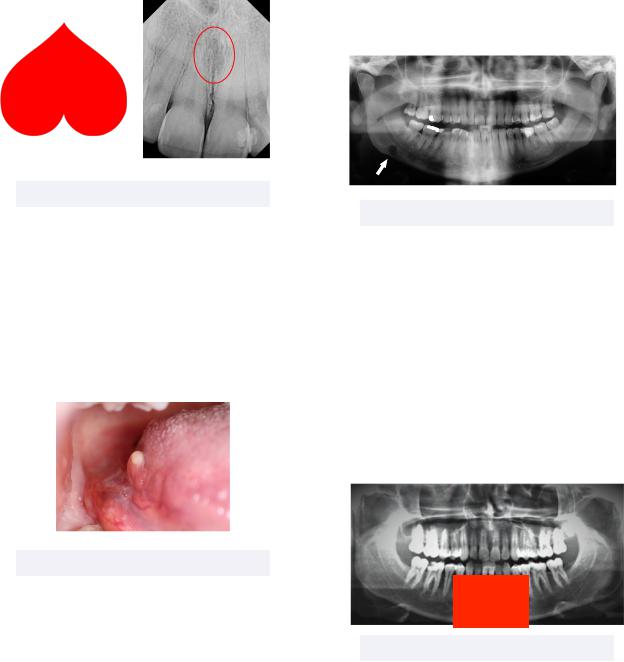
•Nasopalatine Cyst - a nonodontogenic developmental cyst
Must know: appears as a heart-shaped radiolucency in the nasopalatine canal
INBDE Booster | Booster PrepTM
INBDE ORAL PATHOLOGY NOTES |
5 |
|
Prevalence: Most common |
- Referred to as a pseudocyst because it |
|
|
nonodontogenic cyst |
can be mistaken for one from a |
|
|
Treatment: Surgical removal |
radiograph |
|
|
|
Prevalence: Rare, more often found in |
|
|
|
males over 40 years old |
|
|
|
Treatment: None required |
|
|
|
|
|
|
|
|
|
Figure 1.16 Nasopalatine cyst
•Oral Lymphoepithelial Cyst - cyst within lymphoid tissue of oral mucosa
Must know: the palatine and lingual tonsils are common regions for these cysts which appear white or yellowish in color
Prevalence: Rare, usually occurs in adults
Treatment: Surgical removal
Figure 1.17 Oral lymphoepithelial cyst
Finally, we can wrap up our discussion of developmental conditions with learning about two important bone defects.
•Stafne Bone Defect - depression of mandible on the lingual surface
Must know: appears as oval shaped radiolucency in posterior mandible beneath the mandibular canal
Figure 1.18 Stafne Bone Defect
•Traumatic Bone Cyst - an asymptomatic non epithelial lined cavity of the jaw
Must know: appears as a large radiolucency scalloped around roots
-May also be referred to as a simple bone cyst or an idiopathic bone cavity
Prevalence: Rare, mainly diagnosed in young adults; usually associated with jaw trauma
Treatment: Vary from none required to surgical intervention
Figure 1.19 Traumatic Bone Defect
That completes developmental conditions for the INBDE! Let’s now move onto hereditary conditions to learn about their inheritance, and some high-yield information about them.
INBDE Booster | Booster PrepTM
INBDE ORAL PATHOLOGY NOTES
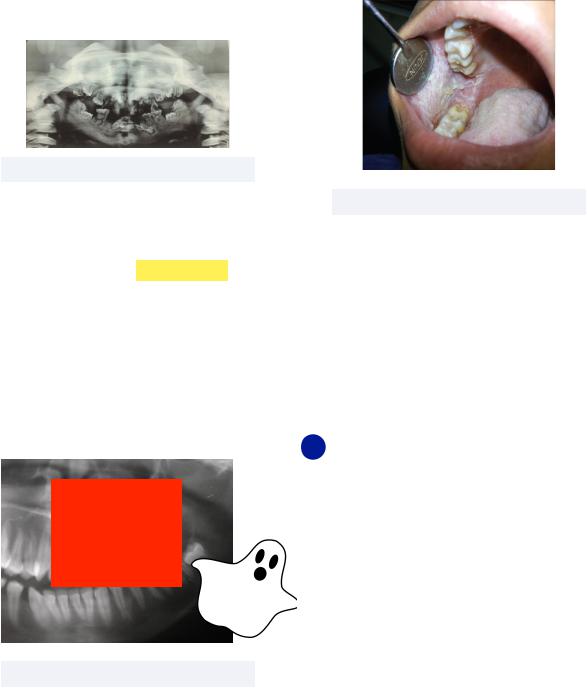
•Amelogenesis Imperfecta - disorder of tooth development leading to small, discolored, misshapen teeth
Must know: Characterized by abnormal enamel formation (think: ENAMELogensis imperfecta), while dentin and pulp are normal
Inheritance pattern: Autosomal dominant, recessive, or X-linked
Treatment: Full coverage crowns for aesthetics
6
•Dentinogenesis Imperfecta - disorder of tooth development affecting primary and permanent dentition, leading to small, discolored, misshapen teeth
Must know: Characterized by abnormal dentin formation, resulting in short roots, bell-shaped and bulbous crowns, and obliterated pulps
-Patients with DI have blue sclera (whites of the eyes)
-Can be associated with osteogenesis imperfecta
Inheritance pattern: Autosomal dominant
Treatment: Full coverage crowns for aesthetics
Figure 1.20 Amelogenesis Imperfecta
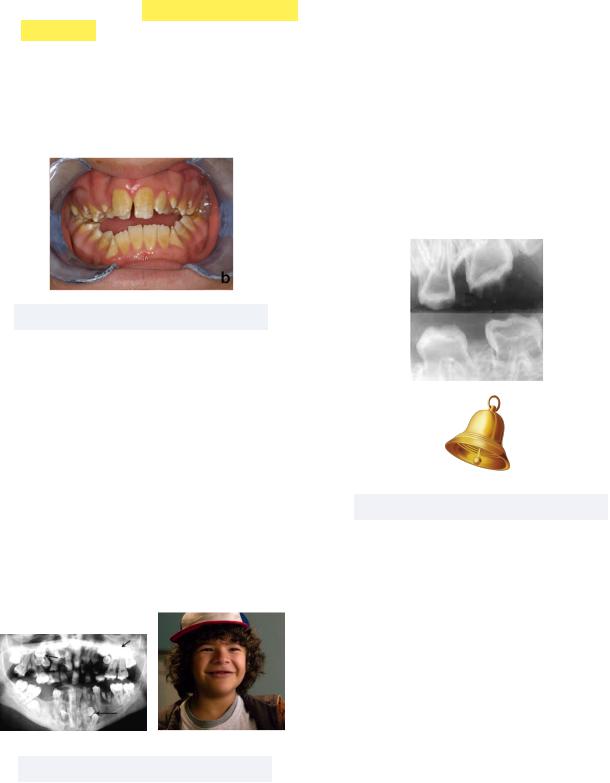
•Cleidocranial Dysplasia - fragile bones and teeth, collarbones (clavicles) may be absent
Must know: Dental abnormalities such as delayed loss of primary teeth, delayed appearance of secondary teeth, misshapen teeth, or supernumerary teeth are observed
-Fun fact, Stranger Things star, Gaten Matarazzo “Dustin Henderson” was born with CCD!
Inheritance pattern: Autosomal dominant
Treatment: Reconstructive surgery,
Figure 1.21 Cleidocranial dysplasia
Figure 1.22 Dentinogenesis Imperfecta
•Dentin Dysplasia - disorder of tooth development leading to small, discolored, misshapen teeth
Must know: Characterized by abnormal dentin, resulting in chevron pulps and short roots
-Has Type I (poor root development) and Type II (poor crown development)
Inheritance pattern: Autosomal dominant
Treatment: Not good candidates for restoration, due to both chevron pulps and short roots
INBDE Booster | Booster PrepTM
INBDE ORAL PATHOLOGY NOTES
Figure 1.23 Dentin dysplasia
•Ectodermal Dysplasia - abnormal development of ectodermal structures such as teeth, mucosal membranes, nails, & hair
Must know: dental manifestations include hypodontia, anodontia, and heat intolerance
Inheritance pattern: X-linked recessive
Treatment: Dental restorative procedures
Figure 1.24 Ectodermal dysplasia
•Epidermolysis Bullosa - defines a group of rare diseases that cause blistering skin
Must know: Mechanical fragility and blistering lead to eventual dental decay due to difficult oral hygiene maintenance
Inheritance pattern: Autosomal dominant or recessive
Treatment: Topical aids for blisters
7
Figure 1.25 Epidermolysis Bullosa
•Hereditary Hemorrhagic Telangiectasia - abnormal formation of capillaries on skin, mucosa, and viscera
Must know: Also known as Olser-Weber- Rendu Syndrome
-Telangiectasia (spider veins) are dilated or broken blood vessels near skin or mucosa membranes
-Iron deficiency is a common consequence
-Epistaxis, or nosebleeds, are the most common manifestations of HHT
Think: TIE
Inheritance pattern: Autosomal dominant
Treatment: Bevacizumab (Avastin)
Figure 1.26 HHT
INBDE Booster | Booster PrepTM
INBDE ORAL PATHOLOGY NOTES
•Osteopetrosis - disorder in which bones become overly dense, which causes them to brittle and fracture easily
Must know: Also called AlbergsSchonberg disease or marble bone disease
Inheritance pattern: Autosomal dominant or recessive
Treatment: Surgery for severe functional deformities
8
•White Sponge Nevus - asymptomatic thick and spongey white patches of tissue that cannot be wiped off
Must know: Commonly found in buccal mucosa
Inheritance pattern: Autosomal dominant
Treatment: None, no serious complications
Figure 1.27 Osteopetrosis
•Regional Odontodysplasia - development anomaly impacting enamel, dentin, and cementum components of teeth
Must know: Termed “ghost teeth” this condition results in quadrants of teeth to exhibit short roots, enlarged pulp chambers, and open apical foramen
-The thin enamel and dentin layers result in a faint, fuzzy image of the teeth when x-rayed, hence the name “ghost teeth”
Inheritance pattern: Unknown
Treatment: Extraction of affected teeth
Figure 1.28 Dentin dysplasia
Figure 1.29 White sponge nevus
We wrap up this first section by distinguishing between tooth fusion and gemination, which have been alluded to throughout our general discussion of different conditions. Fusion involves the merging of two buds into one tooth, resulting in the tooth count to be one less tooth than normal. Gemination, on the other hand, results when one root buds into two crowns, giving us a normal tooth count.
2 Mucosal Lesions
We now transition to more targeted discussions of conditions of the oral cavity, and will start with mucosal lesions. Mucosal lesions describe chemical and physical injury to the mucosal membranes of the mouth, and can vary widely in their severity. This section will focus on five categories of mucosal lesions: reactive, infectious, immunologic diseases, premalignant, and malignant.
INBDE Booster | Booster PrepTM
INBDE ORAL PATHOLOGY NOTES
Reactive Mucosal Lesions
Reactive lesions are hyper-plastic tissues that form as a result of a repair response. Let’s learn some high-yield information about assorted reactive mucosal lesions!
•Amalgam Tattoo - gray/blue/black discoloration on oral mucosal membranes
Must know: This common and benign lesion is often mistaken for melanoma, and the radiopaque particles can be viewed on radiographs
Figure 2.01 Amalgam tattoo
•Chemical Burn - a whiteish sloughing appearance on mucosal membranes as a result of chemical reactivity
Must know: Common compounds that cause chemical burns include hydrogen peroxide, aspirin, silver nitrate, and phenol
Figure 2.02 Chemical burn
•Dentifrice-Associated Sloughing - sloughing of mucosal membranes due to sodium lauryl sulfate, a common surfactant in toothpastes and mouthwashes
9
Must know: to treat, suggest non-SLS brands such as Sensodyne, Tom’s of Maine, etc
Figure 2.03 Dentifrice-associated sloughing
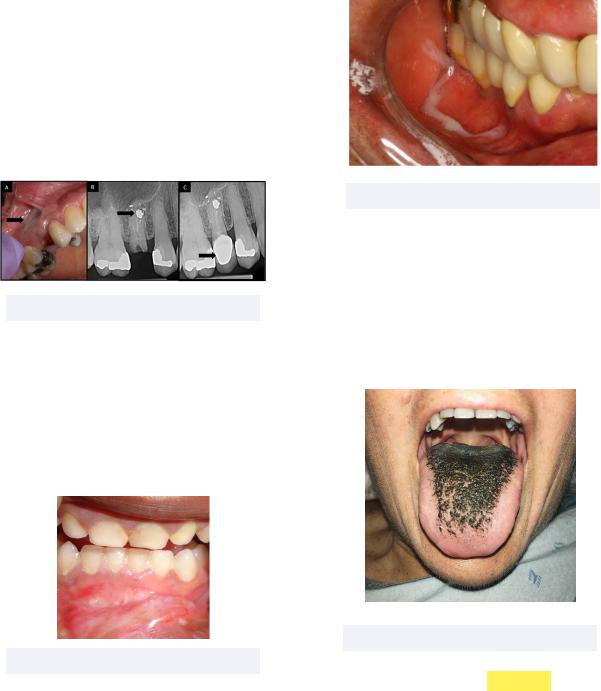
•Hairy Tongue - tongue appears dark and furry due to buildup of dead skin cells on filiform papillae
Must know: poor oral hygiene, certain medications or antibiotics, tobacco use, or radiation treatment of head/neck are all potential causes of this condition
Figure 2.04 Hairy tongue
•Linea Alba - a fibrous white line in the buccal mucosa
Must know: linea alba is a type of focal hyperkeratosis that forms as a result of chronic friction on mucosa
INBDE Booster | Booster PrepTM
INBDE ORAL PATHOLOGY NOTES |
10 |
inflamed salivary duct openings. - Nicotine stomatitis may be
premalignant if associated with reverse smoking (the lit end of the cigarette is in the mouth)
Figure 2.05 Linea alba
•Melanotic Macule - benign hyperpigmentation in the mucosal membrane
Must know: this is essentially just a freckle of the mucosa
-Peutz-Jeghers Syndrome (PJS) is a condition that puts patients at an increased risk of developing certain cancers, with colorectal cancers being the most common. A feature of PJS is freckling, often around the lips and mouth
-Think: Pigmented lips/mouth and Jejunal polyps
Figure 2.06 Melanotic macule
•Nicotine Stomatitis - reaction seen on the palate caused by extreme heat from tobacco smoking
Must know: Also known as “smoker’s palate” this condition presents red dots scattered on the palate, which are
Figure 2.07 Nicotine stomatitis
•Smoking-Associated Melanosis - increased tissue pigmentation due to irritation from tobacco smoke
Must know: Tobacco chemicals can stimulate melanocytes, which results in diffuse brown macules that are typically seen in anterior gingiva
-This condition is reversible if tobacco smoking is ceased
Figure 2.08 Smoking-associated melanosis
•Submucosal Hemorrhage - extravascular lesions that do not blanch — or blood that has escaped the vessels into tissues and thus blood pressure cannot be altered
Must know: these hemorrhages are
INBDE Booster | Booster PrepTM
