
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
11
Malformations
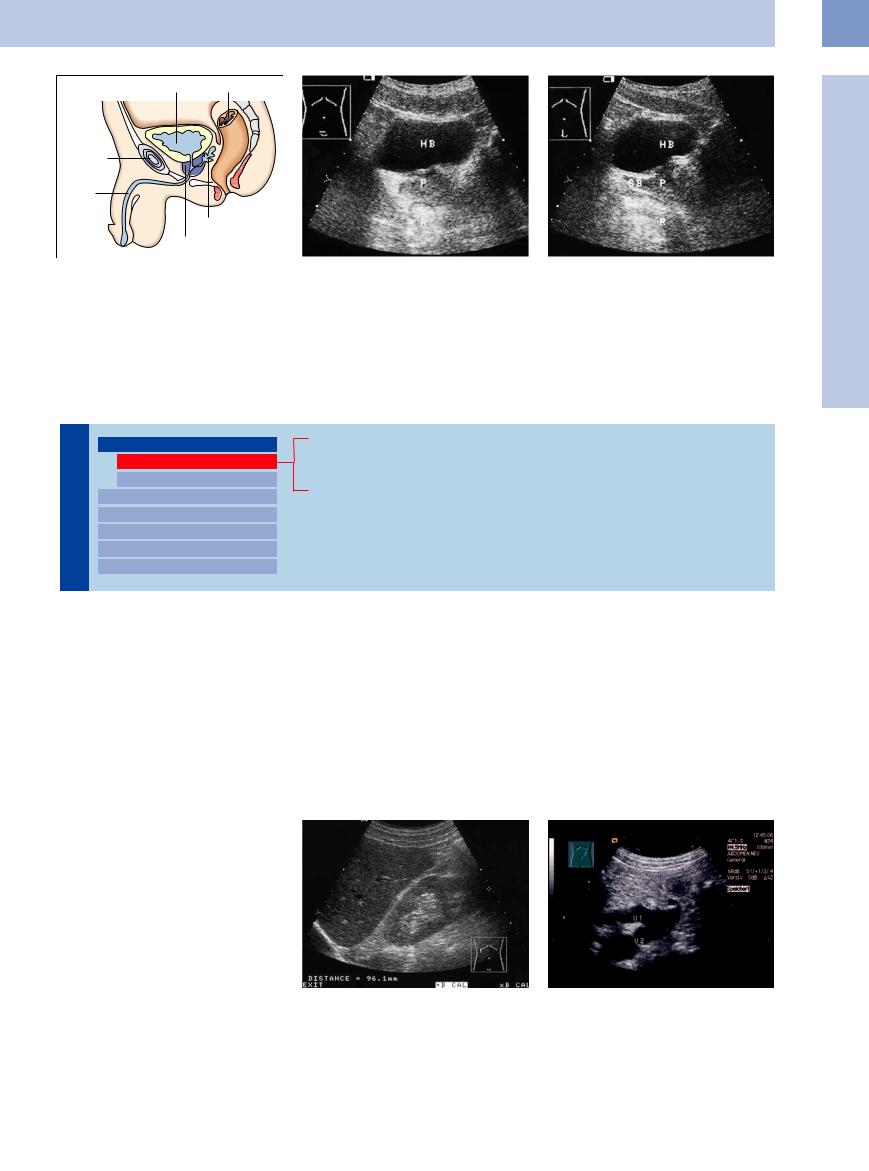
Fig. 11.6
a Diagram showing a sagittal section through the bladder and male reproductive tract.
b |
and c Sonographic relationship of the bladder (HB), prostate (PR), seminal vesicle (SB; see Fig. 11.3), and rectum (R). |
|
b Lower abdominal transverse scan. |
c Lower abdominal longitudinal scan. |
|
■ Malformations
Duplication Anomalies
Tract |
Malformations |
||||
|
|
|
|||
|
|
|
|
Duplication Anomalies |
|
|
|
|
|
||
Urinary |
|
Dilatations and Stenoses |
|||
Dilated Renal Pelvis and Ureter |
|||||
|
|
|
|||
|
|
|
Renal Pelvic Mass, Ureteral Mass |
||
|
|
|
|||
|
|
|
Changes in Bladder Size or Shape |
||
|
|
|
|||
|
|
|
Intracavitary Mass |
||
|
|
|
|||
|
|
|
Wall Changes |
||
|
|
|
|||
Duplex Kidney
Duplex Ureter
Bifid Ureter
The renal collecting ducts, renal pelvis, and ureter are formed by the differentiation of the cranial end of the ureteral bud in the fourth to fifth week of gestation. The ureteral bud itself forms posteriorly and medially from the primary ureter, the wolffian duct, before it opens into the urogenital sinus. The presence of a second, separate ureteral bud gives rise to a complete ureteral duplication, while division of the ureteral bud at the later stage results in
a partial duplication. When two ureters are present, the Weigert–Meyer rule states that the upper-pole ureter inserts closer to the bladder neck, frequently at an ectopic site, owing to the medial and caudal rotation of the wolffian duct that occurs during embryonic development. Meanwhile the lower-pole ureter inserts closer to the bladder roof. This accounts for the tendency for reflux to occur in the lower-pole
system whereas the upper system is more susceptible to obstruction.
A ureterocele is another relatively common anomaly resulting from abnormal development of the initially higher ureteral bud, which drains the upper-pole system but opens in the bladder floor due to caudal rotation. This leads to frequent dysplasia with megaureter formation and hydronephrosis of the upper system.
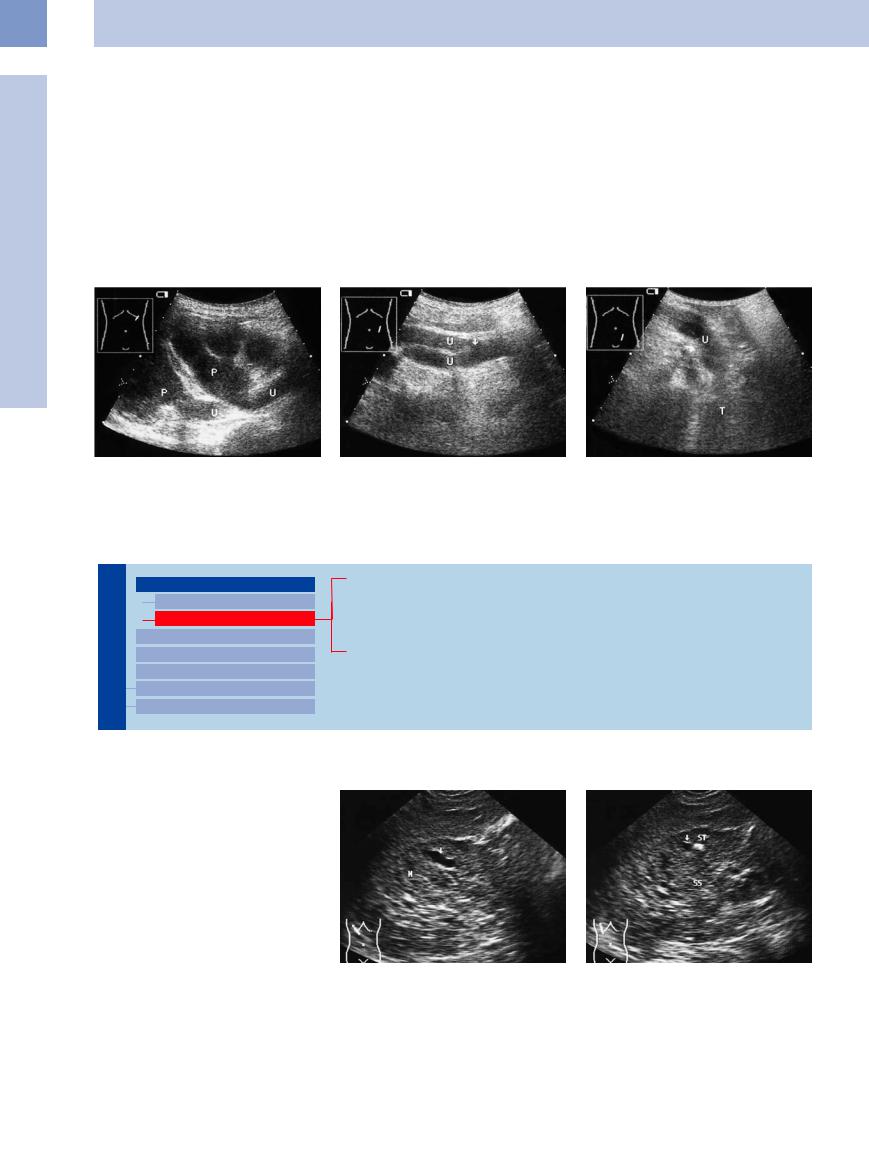
Duplex Kidney




















































Duplex kidney is an anomaly characterized by the presence of two renal pelvises that are joined at the level of the ureteropelvic junction. Sonographically, the kidney appears elongated and the moieties are separated by a band of parenchyma, creating a visible notch in the renal outline (Fig.11.7, Fig.11.8).
Fig. 11.7 Duplex kidney: normal renal size (9.6 cm), complete parenchymal band with a notch in the renal outline (cystic renal cell carcinoma was diagnosed 5 years later; see Fig. 9.57a contralateral kidney and Fig. 11.23).
Fig. 11.8 Bifid ureter, therefore also duplex kidney. The duplicated upper ureters (U) are joined inferior to the level of the ureteropelvic junction. Urinary obstruction (for the cause, see Fig. 11.14a).
383
11
Urinary Tract
Duplex Ureter




















































Duplex ureter refers to a complete ureteral |
duplex kidney, because normally both ureters |
tion is present, but excretory urography can |
duplication with two separate renal pelvises. |
cannot be visualized. Ultrasound can confirm a |
consistently demonstrate the anomaly. |
The ultrasound appearance is like that of a |
duplex ureter only when urinary tract obstruc- |
|
Bifid Ureter 





















































Bifid ureter is a partial ureteral duplication in which the ureters arise from separate renal pelvises and unite between the pelvis and bladder to form a single ureter (Fig.11.8, Fig.11.9).
Fig. 11.9 Bifid ureter: both ureters (U) are obstructed.
a Oblique upper abdominal scan through the left kidney (P = renal pelvis).
Dilatations and Stenoses
b Oblique midabdominal scan on the left side, showing the site where the ureters join together.
c Oblique lower abdominal scan on the left side. Cause of the ureteral obstruction: metastatic tumor (T) of the left ovary.
Urinary Tract

Malformations Duplication Anomalies
Dilatations and Stenoses
Dilated Renal Pelvis and Ureter Renal Pelvic Mass, Ureteral Mass Changes in Bladder Size or Shape Intracavitary Mass
Wall Changes
Caliceal and Ureteral Diverticula
Megacalicosis
Ureteropelvic Junction Obstruction
Ureterovesical Junction Obstruction (Megaureter)
Caliceal and Ureteral Diverticula 










































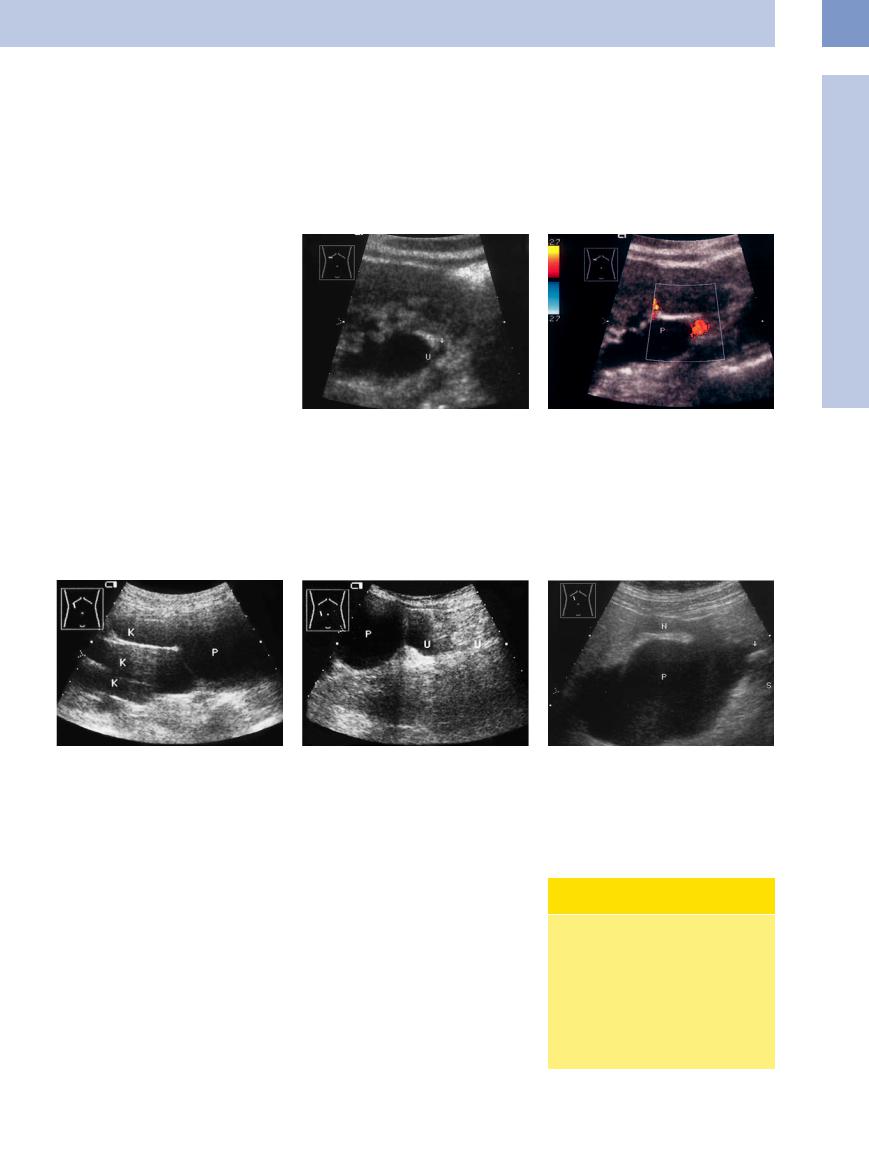
Caliceal and ureteral diverticula are very rare congenital lesions. Stone precipitation occurs in caliceal diverticula and can lead to clinical symptoms. Diverticula appear sonographically as anechoic masses in calices or along the course of a ureter (Fig.11.10).
Fig. 11.10 Caliceal diverticulum (12-year-old boy). a Oval, echo-free area of caliectasis. N = kidney.
b A stone (ST; arrow = acoustic shadow) is visible in the distended calix of a child with colicky episodes. It is likely that the caliectasis is primary and that the stone formed secondarily. SS = shadowing.
384
Megacalicosis 




















































Megacalicosis is an anomaly in which the calices in one kidney are dilated and increased in number. Most cases are clinically asymptomatic. Ultrasound examination reveals enlarged, dilated, fluid-filled calices.
Ureteropelvic Junction Obstruction 








































The most common congenital disorder of the urinary tract is the ureteropelvic junction obstruction. As a fibrous stenosis it depicts a similar appearance to an aberrant artery. It leads to a dilatation up to a hydronephrosis with loss of function. It appears sonographically as a pyelectasis or a hydronephrotic sac in long-stand- ing cases without a demonstrable dilation of the ureter. A unilateral pyelocaliectasis in children indicates a congenital urinary stasis (Figs. 11.11, 11.12, 11.13).
Aberrant arteries can occur in the necks of the calices and at the ureteropelvic junction. Ultrasound may show caliceal enlargement in cases where an interlobar artery leads to caliectasis, or it may show enlarged groups of calices when pyelectasis has developed due to tethering of the upper ureter by an aberrant renal artery. Color duplex examination can demonstrate an aberrant vessel in 91% of cases (Fig.11.11).
Fig. 11.11 Subpelvic ureteral stenosis. Ultrasound shows marked separation of the sinus echo complex by a bandlike, echo-free mass representing the fluid-filled renal pelvis (P). Vascular tethering?
a B-mode image: small, anechoic round feature by the ureteropelvic junction (U, arrow).
b Color duplex: aberrant lower-pole vessel. P = pelvis.
11
Malformations
Fig. 11.12a and b Hydronephrotic sac. Dilated proximal ureter (U). Cause: severe ureteropelvic junction obstruction (surgery)? P, K = massive pyelocaliectasis.
Fig. 11.13 Differential diagnosis: ureteropelvic junction stone (arrow, acoustic shadow S). Severe dilatation of the pelvis. Scans should always include the ureteropelvic junction to aid the differential diagnosis. N = kidney; P = pelvis.
Ureterovesical Junction
Junction Obstruction
Obstruction  (Megaureter)
(Megaureter) 
































Megaureters and megacalices are congenital anomalies involving the dilatation of urinary passages. The classification of Hohenfellner and Walz,1 as modified by Kröpfl,2 is shown below. Nowadays a congenital megaureter is generally diagnosed with antenatal ultrasound, but this modality is of limited value for classifying the lesion.
●Primary idiopathic megaureter is caused by a perivesical fibrotic stenosis of less than
4 cm. Concomitant reflux is present (Fig.11.14a).
●Primary refluxive megaureter is based on an anomalous insertion of the ureteral bud.
●Secondary refluxive and obstructive megaureters are usually caused by bladder wall changes due to subvesical stenosis.
●A nonobstructive, nonrefluxive megaureter shows a changing degree of dilatation; intermittent dilatation of the urinary tract also occurs.Furtherdifferentiationrequiresaspecial urological examination (Fig.11.14b).
Classification of Megaureter
(Ureterovesical Function Obstruction)
●Obstructive megaureter
–Primary, idiopathic
–Secondary (e. g., to neurogenic bladder, subvesical obstruction)
●Refluxing megaureter
–Primary due to reflux
–Secondary to neurogenic bladder, subvesical obstruction
●Nonobstructive, nonrefluxive megaureter
385
