
- •Contents
- •Preface
- •Contributors
- •1 Vessels
- •1.1 Aorta, Vena Cava, and Peripheral Vessels
- •Aorta, Arteries
- •Anomalies and Variant Positions
- •Dilatation
- •Stenosis
- •Wall Thickening
- •Intraluminal Mass
- •Perivascular Mass
- •Vena Cava, Veins
- •Anomalies
- •Dilatation
- •Intraluminal Mass
- •Compression, Infiltration
- •1.2 Portal Vein and Its Tributaries
- •Enlarged Lumen Diameter
- •Portal Hypertension
- •Intraluminal Mass
- •Thrombosis
- •Tumor
- •2 Liver
- •Enlarged Liver
- •Small Liver
- •Homogeneous Hypoechoic Texture
- •Homogeneous Hyperechoic Texture
- •Regionally Inhomogeneous Texture
- •Diffuse Inhomogeneous Texture
- •Anechoic Masses
- •Hypoechoic Masses
- •Isoechoic Masses
- •Hyperechoic Masses
- •Echogenic Masses
- •Irregular Masses
- •Differential Diagnosis of Focal Lesions
- •Diagnostic Methods
- •Suspected Diagnosis
- •3 Biliary Tree and Gallbladder
- •3.1 Biliary Tree
- •Thickening of the Bile Duct Wall
- •Localized and Diffuse
- •Bile Duct Rarefaction
- •Localized and Diffuse
- •Bile Duct Dilatation and Intraductal Pressure
- •Intrahepatic
- •Hilar and Prepancreatic
- •Intrapancreatic
- •Papillary
- •Abnormal Intraluminal Bile Duct Findings
- •Foreign Body
- •The Seven Most Important Questions
- •3.2 Gallbladder
- •Changes in Size
- •Large Gallbladder
- •Small/Missing Gallbladder
- •Wall Changes
- •General Hypoechogenicity
- •General Hyperechogenicity
- •General Tumor
- •Focal Tumor
- •Intraluminal Changes
- •Hyperechoic
- •Hypoechoic
- •Nonvisualized Gallbladder
- •Missing Gallbladder
- •Obscured Gallbladder
- •4 Pancreas
- •Diffuse Pancreatic Change
- •Large Pancreas
- •Small Pancreas
- •Hypoechoic Texture
- •Hyperechoic Texture
- •Focal Changes
- •Anechoic Lesion
- •Hypoechoic Lesion
- •Isoechoic Lesion
- •Hyperechoic Lesion
- •Irregular (Complex Structured) Lesion
- •Dilatation of the Pancreatic Duct
- •Marginal/Mild Dilatation
- •Marked Dilatation
- •5 Spleen
- •Nonfocal Changes of the Spleen
- •Diffuse Parenchymal Changes
- •Large Spleen
- •Small Spleen
- •Focal Changes of the Spleen
- •Anechoic Mass
- •Hypoechoic Mass
- •Hyperechoic Mass
- •Splenic Calcification
- •6 Lymph Nodes
- •Peripheral Lymph Nodes
- •Head/Neck
- •Extremities (Axilla, Groin)
- •Abdominal Lymph Nodes
- •Porta Hepatis
- •Splenic Hilum
- •Mesentery (Celiac, Upper and Lower Mesenteric Station)
- •Stomach
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •Small/Large Intestine
- •Focal Wall Changes
- •Extended Wall Changes
- •Dilated Lumen
- •Narrowed Lumen
- •8 Peritoneal Cavity
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Anechoic Structure
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Wall Structures
- •Smooth Margin
- •Irregular Margin
- •Intragastric Processes
- •Intraintestinal Processes
- •9 Kidneys
- •Anomalies, Malformations
- •Aplasia, Hypoplasia
- •Cystic Malformation
- •Anomalies of Number, Position, or Rotation
- •Fusion Anomaly
- •Anomalies of the Renal Calices
- •Vascular Anomaly
- •Diffuse Changes
- •Large Kidneys
- •Small Kidneys
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Irregular Structure
- •Circumscribed Changes
- •Anechoic Structure
- •Hypoechoic or Isoechoic Structure
- •Complex Structure
- •Hyperechoic Structure
- •10 Adrenal Glands
- •Enlargement
- •Anechoic Structure
- •Hypoechoic Structure
- •Complex Echo Structure
- •Hyperechoic Structure
- •11 Urinary Tract
- •Malformations
- •Duplication Anomalies
- •Dilatations and Stenoses
- •Dilated Renal Pelvis and Ureter
- •Anechoic
- •Hypoechoic
- •Hypoechoic
- •Hyperechoic
- •Large Bladder
- •Small Bladder
- •Altered Bladder Shape
- •Intracavitary Mass
- •Hypoechoic
- •Hyperechoic
- •Echogenic
- •Wall Changes
- •Diffuse Wall Thickening
- •Circumscribed Wall Thickening
- •Concavities and Convexities
- •12.1 The Prostate
- •Enlarged Prostate
- •Regular
- •Irregular
- •Small Prostate
- •Regular
- •Echogenic
- •Circumscribed Lesion
- •Anechoic
- •Hypoechoic
- •Echogenic
- •12.2 Seminal Vesicles
- •Diffuse Change
- •Hypoechoic
- •Circumscribed Change
- •Anechoic
- •Echogenic
- •Irregular
- •12.3 Testis, Epididymis
- •Diffuse Change
- •Enlargement
- •Decreased Size
- •Circumscribed Lesion
- •Anechoic or Hypoechoic
- •Irregular/Echogenic
- •Epididymal Lesion
- •Anechoic
- •Hypoechoic
- •Intrascrotal Mass
- •Anechoic or Hypoechoic
- •Echogenic
- •13 Female Genital Tract
- •Masses
- •Abnormalities of Size or Shape
- •Uterus
- •Abnormalities of Size or Shape
- •Myometrial Changes
- •Intracavitary Changes
- •Endometrial Changes
- •Fallopian Tubes
- •Hypoechoic Mass
- •Anechoic Cystic Mass
- •Solid Echogenic or Nonhomogeneous Mass
- •14 Thyroid Gland
- •Diffuse Changes
- •Enlarged Thyroid Gland
- •Small Thyroid Gland
- •Hypoechoic Structure
- •Hyperechoic Structure
- •Circumscribed Changes
- •Anechoic
- •Hypoechoic
- •Isoechoic
- •Hyperechoic
- •Irregular
- •Differential Diagnosis of Hyperthyroidism
- •Types of Autonomy
- •15 Pleura and Chest Wall
- •Chest Wall
- •Masses
- •Parietal Pleura
- •Nodular Masses
- •Diffuse Pleural Thickening
- •Pleural Effusion
- •Anechoic Effusion
- •Echogenic Effusion
- •Complex Effusion
- •16 Lung
- •Masses
- •Anechoic Masses
- •Hypoechoic Masses
- •Complex Masses
- •Index
3
Biliary Tree and Gallbladder
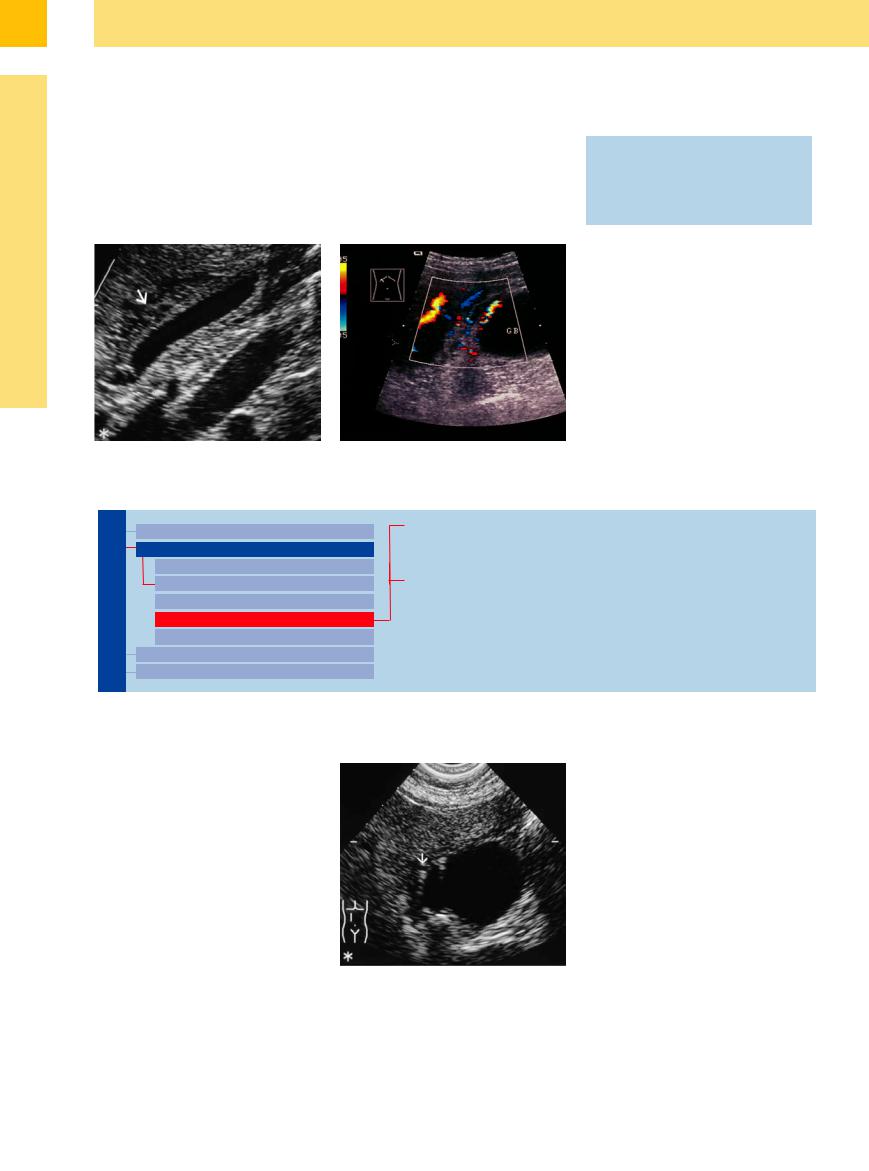
Gallbladder Varicosity
















































When hypoechoic tubular intramural and extramural changes in the gallbladder wall are encountered, the differential diagnosis should include varicosity (Fig. 3.53; see Fig.1.99b, p. 50). It is characteristic of portal hypertension (in prehepatic or posthepatic block). The suspected diagnosis is confirmed by color-flow duplex scanning (Table 3.3). This modality is
also important in preoperative delineation of vascular anomalies. Its application in the differentiation of a benign polypoid mass (perfusion of the stalk in adenomas) from a malignancy is still experimental (Table 3.3). The significance of contrast enhancement in differentiating between benign polypoid masses and malignant tumors is still unknown.
Table 3.3 Color-flow duplex scanning in gallbladder disease
●Vascular anomalies in the hepatoduodenal ligament before surgery
●Varicosity of the gallbladder wall
●Perfusion of the polyp stalk (experimental)
●Vascularization of tumors (experimental)
Fig. 3.53 Varicose veins of the gallbladder wall: intraand perimural tubular formations (arrow) are typical.
a Portal venous collaterals in the gallbladder wall.
b Thickened gallbladder wall in portal hypertension, CDS.
General Tumor
Gallbladder
Changes in Size
Wall Changes
General Hypoechogenicity
General Hyperechogenicity
Focal Hypoechogenicity/Hyperechogenicity
General Tumor
Focal Tumor
Intraluminal Changes
Nonvisualized Gallbladder
Adenomyomatosis
Cholesteatosis
Gallbladder Carcinoma
Adenomyomatosis 

















































Adenomyomatosis is a special case of gallbladder cholesteatosis and belongs to the group of hyperplastic cholecystoses. It appears as a hyperechoic pseudotumorous thickening of the wall (generalized or focal), originating from hypertrophied Rokitansky–Aschoff sinuses. This disorder is characterized by coexistent cholesterol deposits (with their typical “comet tail” artifacts) and cystic intramural inclusions (Fig. 3.54; see Fig. 3.63, Table 3.4).
Fig. 3.54 Adenomyomatosis: typical “comet-tail” pattern (arrow) caused by cholesterol deposits.
156
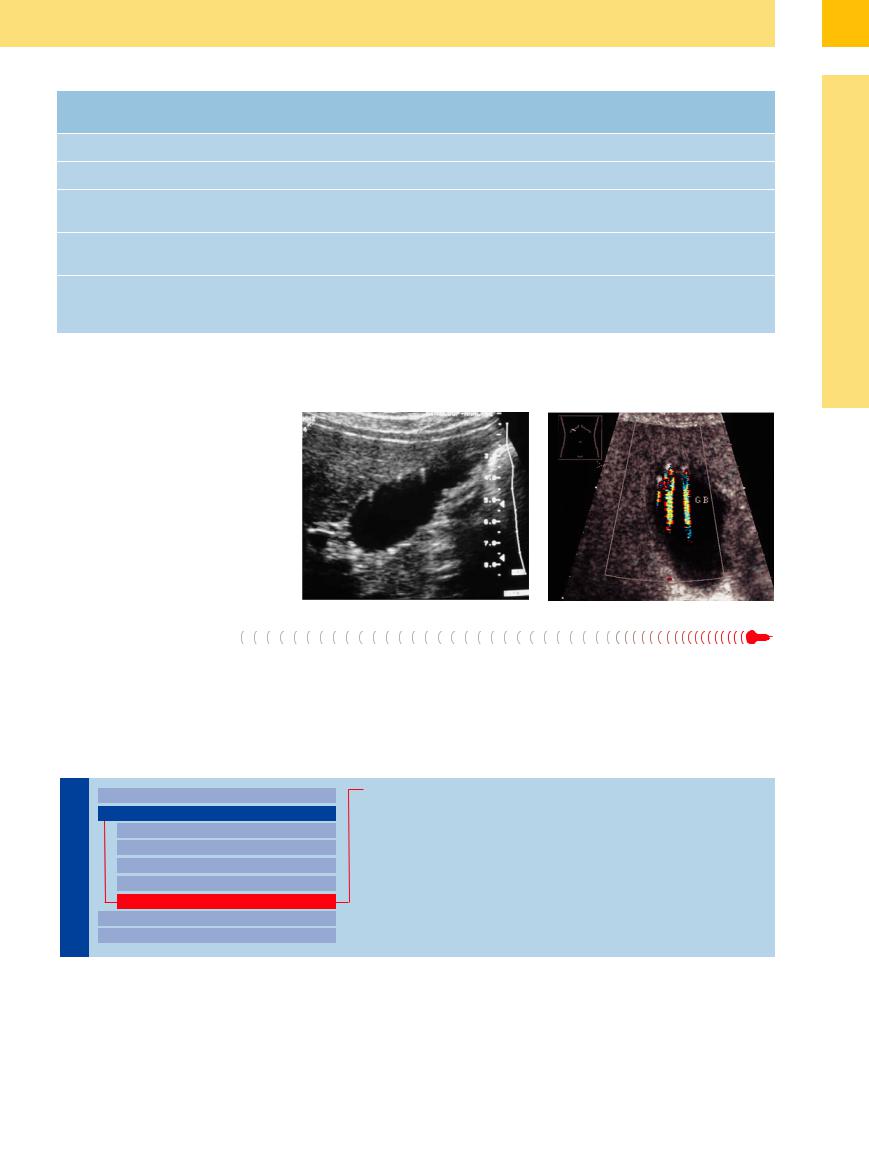
Table 3.4 Comet-tail artifacts in gallbladder ultrasound |
|
|
|
||
|
Emphysematous |
Cholesteatosis |
Adenomyomatosis |
Microliths |
Pneumobilia |
|
cholecystitis |
|
|
|
|
Size |
Large |
Normal |
Normal or smaller |
Normal |
Normal |
Shape |
Round |
Normal |
Hourglass furrows |
Normal |
Normal |
Lumen |
Sludge |
Normal |
Constricted |
Floating (calculi |
Normal |
|
|
|
|
< 5 mm) |
|
Wall |
Hypoechoic wall thick- |
Often normal or |
Hyperechoic, thick- |
Normal |
Normal |
|
ening |
slightly thickened |
ened, cystic inclusions |
|
|
Comet-tail artifacts |
Intramural or intralu- |
Intramural, partly few, |
Localized, intramural |
Floating in the lumen |
Position-dependent |
|
minal gas collections |
partly di use |
or di use |
|
gas collections at the |
|
|
|
|
|
anterior wall |
Cholesteatosis




















































Adenomyomatosis |
should be |
differentiated |
|
from cholesteatosis |
(strawberry |
gallbladder), |
|
which is also characterized by numerous |
|
||
comet-tail artifacts but mostly without the |
|
||
wall thickening (Fig. 3.55a,b). |
|
|
|
Fig. 3.55 |
|
|
|
a Cholesteatosis (“strawberry gallbladder”): classic intra- |
|
||
mural hyperechoic “spotted” echoes with comet-tail arti- |
|
||
facts. |
|
|
|
b Twinkling artifact in the region of comet-tail artifacts. |
|
||
Gallbladder Carcinoma |
|
||
General adenomyomatosis should also be dif- |
Gallbladder carcinoma lacks the Rokitan- |
||
ferentiated from diffuse infiltrating gallbladder |
sky–Aschoff sinuses and intramural comet-tail |
||
carcinoma, although the latter completely de- |
artifacts. |
||
stroys the regular wall layering (see Fig. 3.64). |
|
||
Focal Tumor
Gallbladder |
|
|
|
Changes in Size |
|
Cholesterol Pseudopolyps |
|
|
|||||
|
|
|
Wall Changes |
|
Adenomas and Papillomas |
|
|
|
|
|
|
||
|
|
|
|
General Hypoechogenicity |
|
Adenomyomatosis |
|
|
|
|
General Hyperechogenicity |
|
Gallbladder Carcinoma |
|
|
|
|
Focal Hypoechogenicity/Hyperechogenicity |
|
|
|
|
|
|
|
Metastasis |
|
|
|
|
|
General Tumor |
|
|
|
|
|
|
|
|
|
|
|
|
|
Focal Tumor |
|
|
|
|
|
|
Intraluminal Changes |
|
|
|
|
|
|
|
|
|
|
|
|
|
Nonvisualized Gallbladder |
|
|
|
|
|
|
|
|
In order of frequency, focal changes in the gallbladder wall are mural polypoid lesions, partial wall thickening, and infiltrating lesions.
3
Wall Changes
157
3
Biliary Tree and Gallbladder
Cholesterol Pseudopolyps
Cholesterol pseudopolyps are the most frequently demonstrated. They are hyperplastic polypoid neoplasms, usually hyperechoic, smoothly contoured, round or ovoid. Sometimes they are visualized as small hyperplastic (often hyperechoic) tumors, pendulant from the gallbladder wall, that may display a short
stalk (hypoechoic lobulation is rather rare). Usually, their size is less than 6 mm and they are found in multiples (Figs. 3.56, 3.57, 3.58). The gallbladder wall always appears normal. Cholesterol polyps measuring more than 1 cm in diameter are the exception and therefore should undergo surgery. The detection of cho-
lesterol pseudopolyps is highly dependent on the quality of the equipment. The most recent studies show that cholesterol pseudopolyps 1 mm in size can be detected (in up to 10% of all cases examined).10
Fig. 3.56 Cholesterol pseudopolyp: characteristic visualization of a hyperechoic 5 mm cholesterol pseudopolyp at the floor of the gallbladder.
Fig. 3.57 Cholesterol pseudopolyps. Multiple small sessile hyperechoic polyps of 3–5 mm at the gallbladder wall (some with longer stalks).
Fig. 3.58 Characteristic sonographic morphology of five hyperechoic cholesterol pseudopolyps of less than 5 mm diameter.
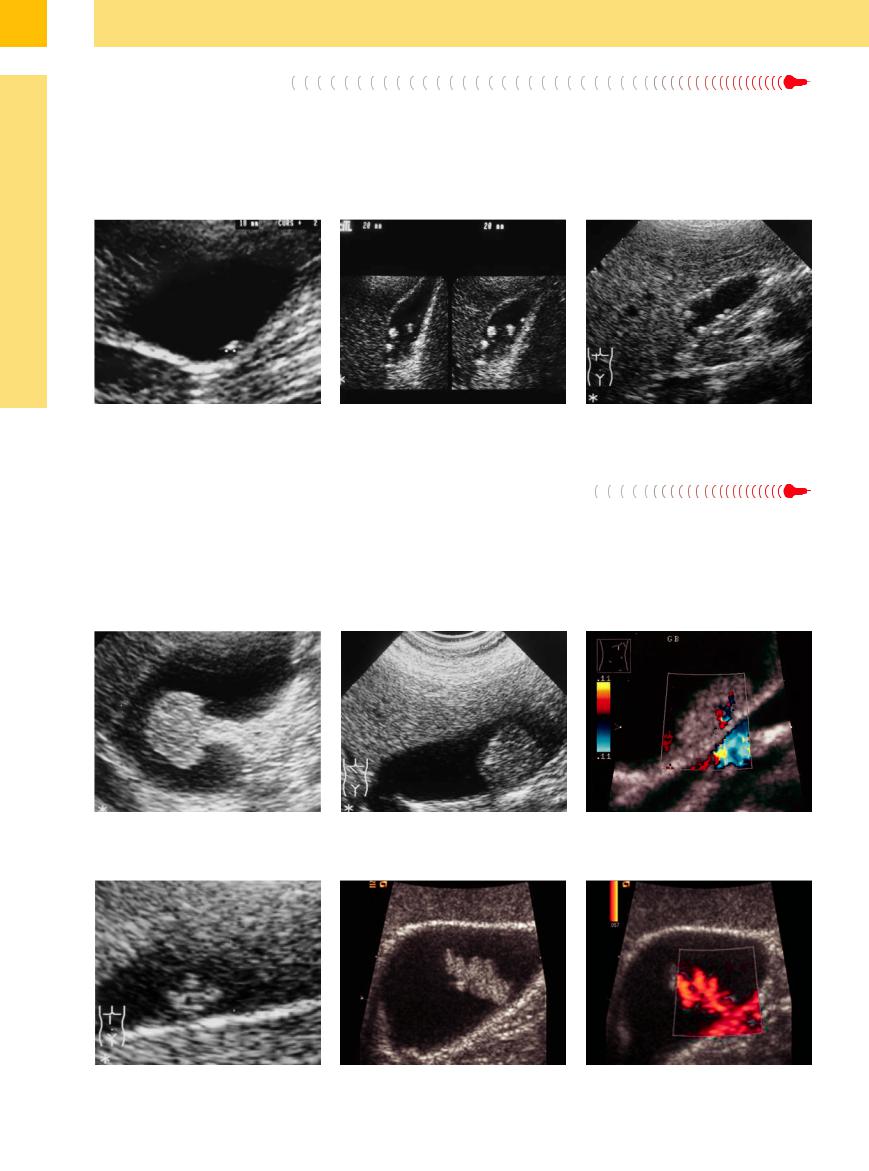
Adenomas and Papillomas
and Papillomas 






















Adenomas. Compared with the more common |
size. Because of the known adenoma–carci- |
cholesterol pseudopolyps (>1% of the popula- |
noma sequence they have to undergo surgery. |
tion) adenomas are infrequent findings (Figs. |
|
3.59, 3.60, 3.61). Usually, they are hypoechoic |
Papillomas. The differentiation of adenomas |
sessile structures resting on the intraluminal |
from papillomas relies on the fact that papillo- |
wall and are frequently found in the neck of |
mas tend to be pedunculated, displaying a lo- |
the gallbladder. They usually exceed 10 mm in |
bulated surface. Papillomas tend to be located |
at the fundus and usually are hypoechoic (Fig. 3.62, Table 3.5). All polyps are easily differentiated from calculi by their sessile growth, although sometimes viscous pseudopolypoid sludge may mimic a polyp. If a papilloma is suspected, surgical treatment is indicated.
Fig. 3.59 Pedunculated adenoma of about 2 cm (con- |
Fig. 3.60 Sessile adenoma: sessile adenoma of about 2 cm |
Fig. 3.61 Flat adenoma (14 mm; histology) of the gallblad- |
firmed histologically) in the body of the gallbladder. |
diameter in the body of the gallbladder. |
der. CDS shows intratumoral vessels. Intact wall. Young |
|
|
female, incidental finding. |
Fig. 3.62 Papilloma.
a Lobulated papilloma of the body of the gallbladder with a diameter of about 1.2 cm.
b |
and c Papilloma (adenomatous polyp): lobulated papilloma of the body of the gallbladder. |
|
b Gray-scale image. |
c CDS with intratumoral branching vessels. |
|
158
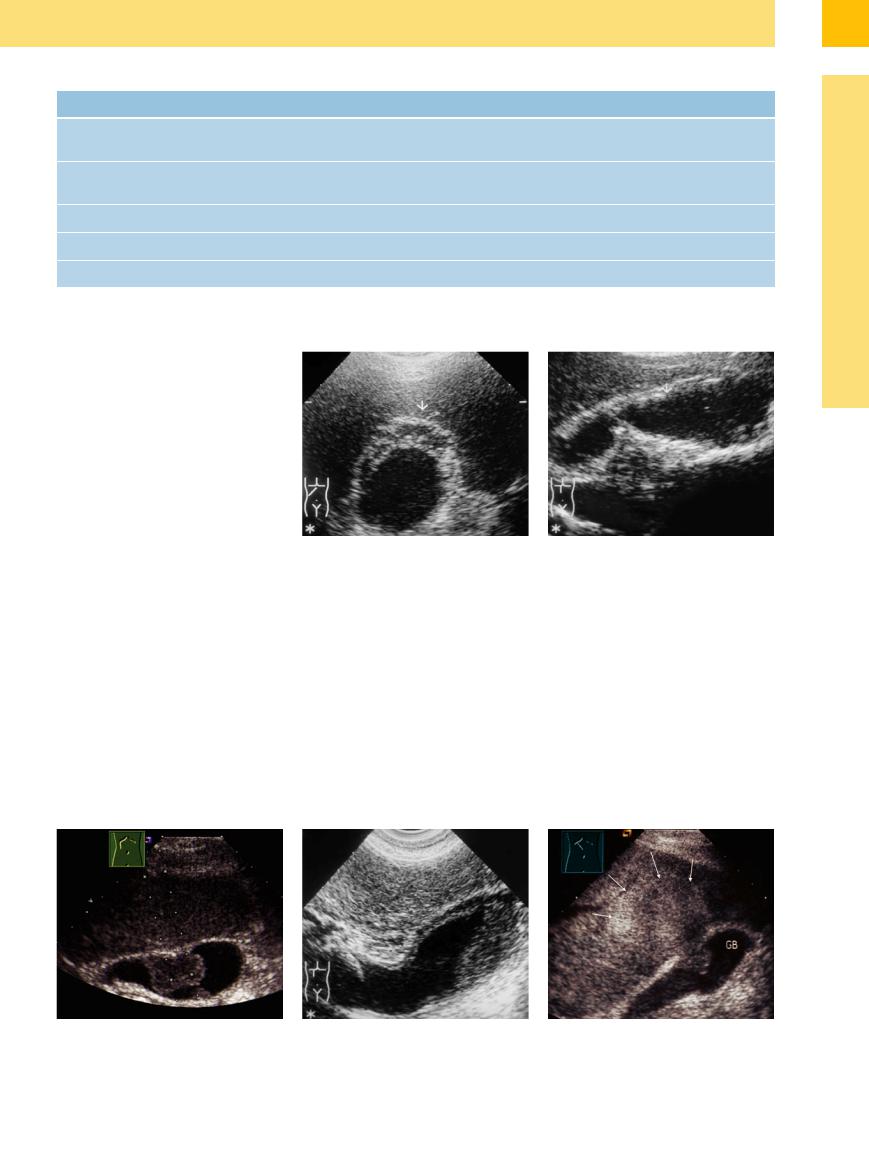
Table 3.5 Focal intraluminal polypoid wall changes |
|
|
|
|
|
Cholesterol pseudopolyp |
Adenoma |
Papilloma |
Carcinoma |
Size |
Often 2–6 mm and multiple, |
Solitary, often > 1 cm |
Solitary, > 7 mm |
Solitary, > 1–2 cm |
|
rarely > 8 mm |
|
|
|
Shape |
Mostly round, sometimes bi- |
Sessile, polypoid, or superficial |
Lobulated |
Polypoid |
|
zarre, short stalk |
|
|
|
Echogenicity |
Mostly rather hyperechoic |
Usually hyperechoic |
Rather more hypoechoic |
Hypoechoic, inhomogeneous |
Wall |
Regular |
Normal |
Normal |
Infiltrated |
Location |
Varying |
Rather more in the neck |
Rather more in the fundus |
Varying |
Adenomyomatosis 

















































A good example of partial wall thickening is adenomyomatosis, which may also present as a hyperechoic focal lesion (Fig. 3.63a). Combined with the focal cystic inclusions and the classic comet-tail artifacts, the focal hypertrophied Aschoff–Rokitansky sinuses will round out the characteristic image in sonographic morphology. In focal adenomyomatosis the gallbladder may undergo segmental constriction (hourglass gallbladder) (Fig. 3.63b).
Fig. 3.63 Adenomyomatosis (focal and segmental). |
b “Hourglass gallbladder” in adenomyomatosis. In seg- |
a Typical adenomyomatosis of the fundus (“fundus ad- |
mental adenomyomatosis the gallbladder displays seg- |
enoma”): hyperechoic wall thickening with hypoechoic |
mental constriction at the body. |
inclusions (here no comet-tail artifacts). |
|
Gallbladder Carcinoma 















































Every polypoid mass of irregular shape within the lumen of the gallbladder as well as every infiltrating lesion with destruction of the normal wall should be highly suspicious for gallbladder carcinoma. In the early stages (still manageable by surgery), gallbladder carcinoma is clinically quiescent and will typically present in two manifestations: polypoid carcinoma, mostly filling the lumen; or primarily diffuse infiltrating carcinoma, with destruction of the
normal texture of the gallbladder wall as well as early invasion of the surrounding tissue (Fig. 3.64). The delineation between the mostly hypoechoic infiltrates and the hepatic parenchyma may be ill defined (Fig. 3.64c,d). Local lymph node metastasis takes place at an early stage. Histologically, it is a scirrhous adenocarcinoma. Gallstones and chronic cholecystitis play an important role in the carcinogenesis: 2–3% of people with gallstones will develop a
carcinoma of the gallbladder. Most tumors appear hypovascular in color-flow duplex scanning, but a chaotic vascular pattern can be detected in suspected gallbladder carcinoma. Contrast-enhanced ultrasonography (CEUS) is more useful than color-flow duplex scanning and can demonstrate the extent of the tumor with greater precision (Fig. 3.64e).11
Fig. 3.64 Gallbladder carcinoma. |
b Carcinoma of the fundus: hypoechoic adenocarcinoma |
c Polypoid infiltrating carcinoma of the body: infiltrating |
a Carcinoma of about 3 cm—with the appearance of a |
with segmental infiltration of the fundus and body of the |
diffusely from the body of the gallbladder into the liver |
large polyp—in the body of the gallbladder (FNB). |
gallbladder. |
(arrows); ill-defined delineation between wall and liver |
|
|
parenchyma. |
3
Wall Changes
159
