
1-280 pdf (1)
.pdf
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
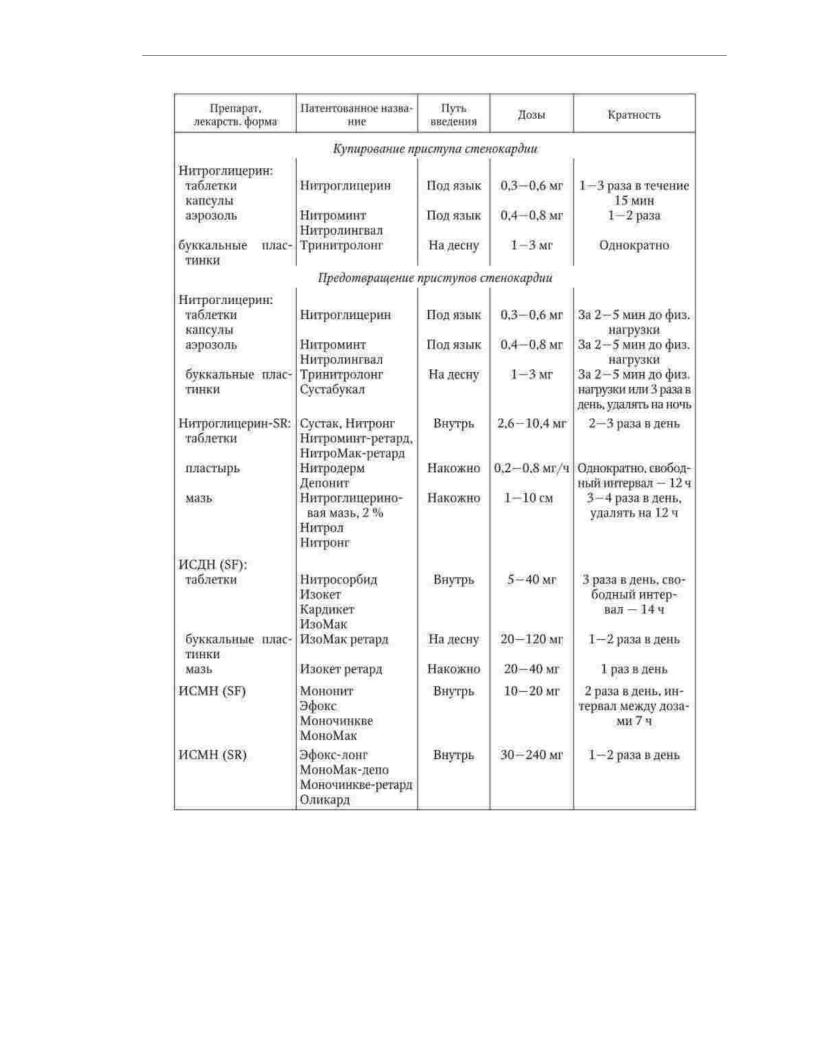
depending on the dose is 2 - 3 times a day. Isosorbide dinitrate compared
with nitroglycerin has greater bioavailability, but the level of its active metabolites in the blood is subject to significant fluctuations depending on the functional state of the liver. Isosorbide-5-mononitrate is used orally to prevent seizures.
angina. The compound is not metabolized in the liver and has 100% bioavailability.
Due to the long half-life, conventional preparations of isosorbide-5-mononitrate are used 2 times a day, prolonged - 1 time per day. With angina pectoris I - II
functional class, it is recommended to use mainly short-acting nitrates before the intended physical activity. With angina pectoris III-IV functional class, nitrates in the form of longacting dosage forms are used constantly according to an asymmetric scheme (Table 1.21).
The most common side effects of nitrates are headache associated with
with the expansion of cerebral vessels, and a decrease in blood pressure. Regular and long-term use nitrates is often accompanied by a weakening, and in some cases even the disappearance antianginal effect. The most effective way to prevent tolerance
to nitrates is the intermittent intake of drugs during the day with the provision of a "nitratefree" interval lasting 10-12 hours. In connection with the expansion of opportunities
of non-drug treatment of patients with chronic coronary artery disease, the patient's persistent need for the use of nitrates is considered as the basis for discussing the feasibility of coronary angiography and subsequent myocardial revascularization. Absolute contraindications to the use of nitrates: hypersensitivity to nitrates; pronounced
arterial hypotension; hypovolemia; left ventricular failure with low end-diastolic pressure in the left ventricle; constrictive pericarditis; hemorrhagic
stroke. Relative contraindications: orthostatic arterial hypotension; hypertrophic cardiomyopathy with obstruction of outflow tracts; severe stenosis of the aorta or left AV
holes; increased intracranial pressure; closed-angle glaucoma.
Antiplatelet agents are used as part of the complex pharmacotherapy of stable angina pectoris to prevent thrombosis of the coronary arteries. The main means of solving this problem is acetylsalicylic acid (aspirin). The mechanism of action of aspirin is non-selective inactivation of a key enzyme in the metabolism of arachidonic acid.
acids are platelet cyclooxygenases. This enzyme is essential for the synthesis of thromboxane A2 - a powerful proaggregant and vasoconstrictor factor. The platelet is a non-nuclear cell,
so it is not capable of synthesizing enzymes. Intracellular reserves of cyclooxygenase obtained by a platelet at birth are not replenished during its life.
Once under the influence of aspirin, a platelet loses its ability to aggregate until the end of its life cycle, which is 9–11 days. The optimal dose of aspirin is
75 - 100 mg / day.
Side effects of aspirin are mainly due to its ulcerogenic and hemorrhagic effects. Aspirin is recommended to reduce the risk of their occurrence.
in minimal doses that provide an antiaggregatory effect, use drugs that enteric-coated and preparations containing antacids. Absolute
contraindications to the use of aspirin are gastrointestinal bleeding,
allergies, previously identified individual intolerance. Relative contraindications: bleeding tendency, active hepatitis, thrombocytopenia, thrombocytopathies.
Table 1.21
Average doses, route of administration and frequency of administration of organic nitrates, the most commonly used for the treatment of patients with angina pectoris
71
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
In patients with stable angina, chronic aspirin significantly reduces the risk of
exacerbations of coronary artery disease, especially the risk of recurrent myocardial infarction. If it is impos aspirin for the prevention of thrombotic complications in patients with stable angina pectoris,
the appointment of clopidogrel is recommended. The antithrombotic effect of this drug caused by blockade of ADP receptors in platelets. Clopidogrel has no direct effect on the gastric mucosa and is less likely than aspirin to cause dyspepsia,
however, the risk of gastrointestinal bleeding is increased with any anti-
72

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
rhombocytic agent. The recommended dose of clopidogrel for continuous use is 75 mg/ day.
Lipid-lowering drugs, reducing the levels of total cholesterol and LDL cholesterol in blood plasma, significantly reduce the likelihood of cardiovascular complications of atherosclerosis.
Statins are recommended for all patients with stable angina, regardless of
the initial content of total cholesterol in the blood. The dose of the drug should ensure the achievement the level of LDL cholesterol is less than 2.5 mmol / l. If statins fail to achieve target levels
LDL cholesterol or poorly tolerated, additional administration of ezetimibe is recommended. ACE inhibitors, in the absence of contraindications and good tolerability, are
indicated in patients with stable angina pectoris with signs of heart failure or asymptomatic left ventricular dysfunction, in patients who have had a myocardial
infarction, who have high blood pressure and who suffer from diabetes mellitus. Improvement of the f patients is considered a class effect of ACE inhibitors. For uncomplicated CAD
proven to reduce the risk of cardiovascular events
for ramipril and perindopril.
ÿ- blockers have an anti-ischemic effect due to the ability to interact with ÿ1adrenergic receptors, as a result of which they become temporarily inaccessible to endogenous catecholamines. Due to negative chronotropic and inotropic
the action of ÿ- blockers decreases myocardial oxygen demand. Besides,
an increase in the duration of diastole improves the blood filling of the coronary arteries. In the treatment of patients with stable angina pectoris, selective ÿ- blockers are mainly used, since they cause fewer side effects than non-selective drugs. ÿ- blockers with their own (intrinsic) sympathomimetic activity are not recommended for the treatment of patients with stable angina pectoris, since
how under their influence a significant decrease in heart rate does not occur, namely this effect mainly due to the antianginal effect of drugs of this class.
Among the side effects of ÿ- blockers associated with cardiovascular
system, include: severe bradycardia; severe arterial hypotension; slowing down of AV conduction; progression of heart failure; exacerbation of intermittent claudication. Most Common side effects that are not related to the cardiovascular system are: bronchospasm; exacerbation of peptic ulcer; depression; insomnia; allergic reactions. Long-term use of non-selective ÿ- blockers can cause proatherogenic changes in the blood lipid spectrum, as well as reduce glucose tolerance in patients with
disorders of carbohydrate metabolism and reduce the severity of clinical manifestations of hypoglycemia in patients with diabetes mellitus. Absolute contraindications to the use of ÿ- blockers: bronchial asthma or severe obstructive respiratory failure; unstable chronic HF III-IV functional class without tachycardia; sconce dycardia less than 50 bpm; AV block II - III degree; sick sinus syndrome;
arterial hypotension (systolic blood pressure less than 100 mm Hg). Relative contraindications: severe obliterating atherosclerosis of the vessels of the lower extremities; obliterating endarteritis; insulin-dependent diabetes mellitus; peptic ulcer of the stomach and duodenum in the acute stage; AV block I degree.
ÿ- blockers improve the prognosis of patients with stable angina pectoris with a history of myocardial infarction and have a pronounced antianginal effect. This class
of drugs is recommended for all patients with stable angina who have no contraindications to their application. Doses of ÿ- blockers are selected individually in the mode of increasing titration. To achieve the result of therapy with ÿ- blockers, it is necessary to maintain
heart rate at rest at the level of 55-60 bpm.
73

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Calcium antagonists block L-type calcium channels and thus prevent transmembrane transport of calcium ions into the cell. The antianginal effect of calcium antagonists is due to a decrease in the contractility of cardiomyocytes and
relaxation of the smooth muscle elements of the vascular wall. Vasodilating effect calcium antagonists is manifested at the level of arterioles, which leads to a decrease in afterload, as well as at the level of coronary arteries, which is accompanied by an improvement in blood supply to the heart muscle.
The most common side effects of calcium antagonists are arterial hypotension and flushing of the skin. In some cases, dihydropyridines cause reflex tachycardia and pastosity of the lower extremities, phenylalkylamines and
benzothiazepines - AV conduction disorders, bradycardia and increased heart failure. General Pro
contraindications to the use of calcium antagonists: severe arterial hypotension,
hemodynamically significant aortic stenosis, hypersensitivity. Dihydropyridines are not recommended for patients with unstable angina and other acute
coronary syndromes, with tachycardia. Phenylalkylamines and benzothiazepines are contraindicated in severe bradycardia, II-III degree AV block, sinoatrial block, sick sinus syndrome, uncompensated heart failure.
Calcium antagonists do not affect the prognosis of patients with stable angina pectoris. Derivatives of phenylalkylamine and benzothiazepine that reduce heart rate (verapamil, diltiazem) can be considered as an alternative to ÿ- blockers if they are poorly
tolerated in patients who have had myocardial infarction without HF. Long acting dihydropyridines
(amlodipine, felodipine) it is advisable to use in the treatment of patients with vasospastic angina (instead of ÿ- blockers), as well as in the combination of coronary artery disease with hypertension (in combination with ÿ- blockers).
If-channel inhibitors are a new class of antianginal drugs, the only
currently represented by ivabradine. The mechanism of action of ivabradine is the blockade of specific ion channels in the cells of the sinus node. The inhibition of the ion current along f-channels is accompanied by a decrease in heart rate. Thereby
myocardial oxygen demand decreases, and by increasing the duration of diastole increased oxygen delivery to the myocardium. Unlike ÿ- blockers, ivabradine does not has a negative inotropic effect. In patients with stable angina pectoris,
In combination with left ventricular dysfunction, the use of ivabradine is associated with a reduced risk of MI and the need for revascularization. In order to achieve the target
Heart rate in patients with stable angina and preserved sinus rhythm, ivabradine may be used instead of ÿ- blockers (for example, if there are contraindications to their use), and in combination with drugs of this class.
Pharmacotherapy of painless myocardial ischemia has no fundamental differences from tactics of medical treatment of patients with stable angina pectoris. Patients who have myocardial ischemia is not manifested by anginal pain, need more careful monitoring
the effect of treatment using instrumental methods, primarily Holter ECG monitoring.
Treatment of patients with unstable angina along with the use of oral drugs
The classes listed above include heparin therapy (parenteral administration of unfractionated heparin or low molecular weight heparins), and, if necessary,
intravenous administration of nitrates and ÿ- blockers.
Preservation of stable exertional angina above functional class III for
background of optimal combined drug therapy, as well as the lack of stabilization of the patient'scondition with one or another clinical variant of unstable angina pectoris
within 2-3 days is regarded as an indication for coronary angiography to assess the possibility
74

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
ness of invasive treatment. Depending on the characteristics of the coronary lesion with
the purpose of myocardial revascularization is either percutaneous coronary balloon angioplasty with a stent placed at the site of the narrowing of the coronary artery, or surgery
coronary artery bypass surgery.
1.4.2. myocardial infarction
Definitions. The period of exacerbation of coronary artery disease is designated by the term "acute coronary
syndrome". This term includes myocardial infarction and unstable angina, which are is a manifestation of a single pathophysiological process - coronary artery thrombosis.
The clinical variant of acute coronary syndrome is determined by the degree of thrombotic narrowing of the coronary artery.
Acute coronary syndrome is any group of clinical signs or symptoms suggesting myocardial infarction or unstable angina. The introduction of this term into
practice is due to the frequent impossibility of confidently distinguishing between its clinical options in the first hours after the onset of symptoms and, at the same time, the need for emergency treatment to improve the prognosis. The diagnosis of "acute coronary syndrome" is temporary and is used to identify a category of patients with clinical signs of coronary artery disease exacerbation, whose treatment is started before information is received.
necessary and sufficient for a confident nosological diagnosis. After identifying the clinical variant of acute coronary syndrome based on the results of diagnosing
Gnostic tests are used to correct therapy.
ST-segment elevation myocardial infarction is an acute process of myocardial ischemia, accompanied by the formation of a focus of necrosis in the heart muscle. On the ECG recorded immediately after the onset of clinical symptoms of acute coronary
syndrome, there is an elevation of the ST segment. Subsequently, pathological Q waves form on the ECG in most patients. There is a diagnostically significant increase in the content biochemical markers of myocardial necrosis in the blood.
Non-ST elevation myocardial infarction is an acute process of myocardial ischemia that causes necrosis of the heart muscle. There is no ST elevation on the ECG recorded immediately after the onset of clinical symptoms of acute coronary syndrome. Subsequently
pathological Q waves are not formed. There is a diagnostically significant increase the content of biochemical markers of myocardial necrosis in the blood.
Unstable angina is an acute process of myocardial ischemia, accompanied by clinical symptoms, but not leading to the formation of a focus of necrosis in the heart
muscle. There is no ST segment elevation on the ECG. The content of biochemical markers of myocardial necrosis in the blood either remains normal or slightly increases, but does not reach dia
gnostic level.
Before receiving information confirming or excluding the presence of a focus of necrosis in the myocardium, the terms
"acute coronary syndrome with ST segment elevation" and "acute coronary syndrome without ST segment elevation.
Prevalence. The incidence of MI varies widely depending on age and sex. So, in men 30-39 years old, about 1 case of MI per 1000 is registered.
people, and in the age group of 60-64 years, the incidence of myocardial infarction increases to 18 cases per
1000 people. In women under 50, MI is 5 times less common than in men of the same age. In the group of 51 - 60 years old, this difference is reduced to 2 times. In the group of elderly and senile people, the frequency of MI in men and women becomes the same.
75

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Etiology. Acute coronary syndromes are based on a critical mismatch
coronary blood flow to the metabolic needs of the myocardium. The main reasons for this discrepancies are thrombosis and spasm of the coronary artery affected by atherosclerosis.
Factors provoking an exacerbation of coronary artery disease include physical and psycho-emotional tension, a sharp increase in systemic arterial pressure, paroxysmal heart rhythm disturbances.
Of great importance in the formation of acute coronary insufficiency is the activation of the sympathetic-adrenal system. Hypercatecholaminemia stimulates
adhesion and activation of platelets, promotes vasoconstriction and increases the need
myocardium in oxygen.
Quite rarely (no more than 2% of cases) acute coronary syndromes, including myocardial infarction, caused by other reasons. These include: damage to the coronary arteries of an inflammatory
nature in systemic vasculitis and diffuse connective tissue diseases (Takayasu'sdisease, periarteritis nodosa, systemic lupus erythematosus); compression
coronary arteries due to traumatic impact or aortic dissection; embolism
coronary arteries in infective endocarditis, thrombosis of the left chambers of the heart, as well as due to cardiac surgery (implantation of heart valves, coronary angioplasty and stenting, coronary bypass grafting); arterial wall thickening
due to metabolic diseases or intimal proliferation (mucopolysaccharidosis, juvenile idiopathic calcification of the coronary arteries, etc.); hemocoagulation disorders (disease Vakeza, polycythemia, disseminated intravascular coagulation, etc.); anomalies
coronary arteries.
Pathogenesis. The process of thrombus formation is initiated by rupture of the atherosclerotic plaques, as a result of which there is a contact of the blood flowing through the vessel with the thrombogenic contents of the atheroma. Damage to the atherosclerotic plaque cover most often starts from the periphery - in this place the fibrous capsule is the thinnest and at the same time
time is subjected to the strongest mechanical impact during the movement of blood along the artery, vasospasm and contraction of the heart muscle.
One of the factors contributing to damage to the atherosclerotic capsule
plaque, is a local inflammatory reaction. Inflammatory cells - macrophages and T-lymphocytes - secrete enzymes that destroy the collagen framework of the atherosclerotic plaque capsule. In addition, activated T-lymphocytes, which are part of the lipid core,
produce inflammatory cytokines that inhibit collagen synthesis. Oxidized LDL contained in the core of an atherosclerotic plaque have a distinct pro-inflammatory activity. A local inflammatory reaction can also be provoked by some microorganisms - in particular, Chlamidia pneumoniae, Helicobacter pylori, cytomegaloviruses
and herpes viruses.
Endothelial dysfunction plays an important role in the pathogenesis of acute coronary syndromes. Violation of endothelium-dependent vascular relaxation and strengthening of adhesive properties of the endothelium contribute to intravascular thrombosis, and local spasm
coronary artery is one of the causes of damage to the atherosclerotic capsule plaques. On the other hand, vascular spasm can also develop as a result of rupture
plaques, since vasoconstrictor agents are released into the bloodstream from the damaged atheroma.
Despite the high thrombogenicity of the core of an atherosclerotic plaque, not all ruptures of its membrane lead to the formation of a thrombus that restricts blood flow through the artery in the degree necessary for the formation of acute coronary syndrome. An important condition triggering the process of thrombus formation is to increase the activity of the coagulation system blood. The state of hypercoagulability is determined by the content of activated VII in the blood.
76

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
factor, X factor activity and the concentration of other compounds that accelerate the process thrombin formation.
The first reaction from the blood in response to the rupture of the atherosclerotic membrane plaque and/or endothelial defect formation is platelet adhesion. Glycoproteins, new platelet receptors, interact with adhesive proteins of the subendothelium, following
The effect of which is that platelets stick to the site of damage to the surface of the vessel wall.
Under the influence of a number of biologically active compounds released from the vascular wall at the site of injury, platelet activation occurs. This process is
conformational change in glycoprotein IIb/IIIa receptors, resulting in a sharp increases the ability of platelets to bind molecules of certain blood glycoproteins, mainly fibrinogen. They form "protein bridges" between cells, which
leads to the formation of a platelet aggregate. The most potent agonists of platelet activation are collagen and thrombin. Activated platelets themselves secrete compounds that enhance the aggregation process, as well as promote the formation
thrombin - thromboxane A2, serotonin, adenosine diphosphate. With the weakening of the proaggregant exposure to platelet aggregates may disintegrate. If this does not happen, erythrocytes begin to
get stuck in the fibrin threads, and the process of thrombus formation passes into the phase red thrombus. In most cases, the thrombus is located above the site of atherosclerotic plaque rupture, directly blocking the lumen of the coronary artery, but often it
penetrates into the plaque and the subendothelial space, which leads to an increase in the size of the plaque and local thickening of the vessel wall with a sharp limitation or complete predominance. reduction in blood flow.
Formation of a red thrombus with complete occlusion of the coronary artery, usually leads to necrosis of the area of the heart muscle located in the pool of blood supply
the affected vessel, that is, to the development of MI. If the process of thrombus formation is limited by the formation of a platelet aggregate, and also in cases where the main mechanism of acute coronary insufficiency is vasospasm, the clinical picture of unstable angina pectoris develops.
Morphology. Localization of myocardial damage, as a rule, corresponds to the basin of the affected vessel. Thrombosis of the anterior interventricular coronary artery causes
MI of the anterior wall and apex of the heart, occlusion of the left circumflex artery - MI of the lateral and posterior walls, with damage to the right coronary artery, myocardial infarction of the lower
localization develops. The severity of morphological changes in the myocardium during ischemia depends on the and the level of thrombotic occlusion of the coronary artery, the state of collateral blood flow, the
initial state of the heart muscle. Necrotic changes in the myocardium separate
into transmural (the zone of necrosis extends throughout the entire thickness of the heart muscle
- from the endocardium to the epicardium) and non-transmural (the focus of necrosis is limited to subendocardial subepicardial departments or localized in the thickness of the myocardium). Thrombotic occlusion
of the main coronary artery in most cases leads to the development of transmural MI. The formation of a parietal thrombus that does not completely block the lumen
vessel, or rapid recanalization of an occluded coronary artery is accompanied by formation of non-transmural MI.
During MI, 4 periods are distinguished: developing MI - from 0 to 6 hours, acute MI - from 6 hours to 7 days, healing (scarring) MI - from 7 to 28 days, healed (healed)
MI - starting from 29 days. Developing MI is characterized by destruction of cardiomyocytes. AT
in the acute period, there is an accumulation in the zone of necrosis of polymorphonuclear leukocytes. For the scarring period is characterized by the presence of mononuclear cells and fibroblasts in the lesion.
A sign of a healed MI is the formation of scar tissue without cellular infiltration. Scarring of MI occurs on average after 5-6 weeks.
77

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
The consequence of the formation of a focus of necrosis in the heart muscle is postinfarction remodeling of the heart. This term refers to the process of changing the structure, form
and the function of the chambers of the heart, which initially ensures the adaptation of the heart to the changed conditions, and then his progressive functional inferiority. An increase in the volume of the
left ventricle is observed within a few weeks after the development of MI, and with extensive necrosis of the heart muscle - continues months and even years after myocardial infarction. Initially, dilatation of the left ventricle is compensatory in nature, since
in accordance with the Frank-Starling law, this allows you to save stroke volume at lesser degree of systolic shortening of myocardial fibers. To maintain the one-time performance at the required level, the ventricle is forced to develop a greater voltage. The hyperfunction of the unaffected parts of the heart muscle is ensured by their gradual
hypertrophy, which is a physiological response to the exclusion of part of the myocardium from work on the movement of blood. Over time, the process of postinfarction remodeling of the
left ventricle loses its adaptive nature and passes into a pathological phase.
The progression of hypertrophy of the initially unaffected parts of the heart muscle is accompanied by an increase in energy deficit, which leads to a decrease in their contractile force. capabilities. Increases stimulation of apoptosis - programmed cell death. intensifies
the process of formation of connective tissue, not only in the damaged area of the heart muscle, but also outside the infarct zone - cardiosclerosis progresses. These changes entail an increase in systolic and diastolic dysfunction of the left ventricle, its further dilatation and spherification. Due to depletion of the contractile
myocardial reserve develops congestive heart failure. a key role in cardiac remodeling and its transition to the maladaptive phase is played by generalized neurohumoral activation and primarily hyperactivation of the renin-angiotensin-aldosterone system.
Classification. According to the results of an electrocardiographic study, MI is traditionally divided into transmural, non-transmural and subendocardial, as well as MI with pathological Q wave and MI without pathological Q wave. In addition, in
Currently, types of MI are distinguished depending on the mechanism (cause) of development: Type 1. MI that developed for no apparent reason (spontaneously) as a result of a
primary violation of coronary blood flow due to the formation of erosion, rupture, crack or dissection of atherosclerotic plaque.
Type 2. MI resulting from ischemia associated with increased demand
myocardium in oxygen or with a decrease in its delivery to the myocardium, for example, with spasm or
coronary artery embolism, anemia, cardiac arrhythmias, hypertension or hypotension.
Type 3 Sudden cardiac death, including cardiac arrest, often accompanied by symptoms suggestive of myocardial ischemia in patients with suspected acute ST elevation, acute left bundle branch block, or a fresh thrombus in a coronary artery identified by coronary angiography and/or
pathological study. Death occurred before blood sampling
or earlier than there is an increase in the level of biochemical markers of necrosis in the blood. Type 4a. MI associated with a percutaneous coronary intervention procedure.
Type 4b. MI associated with coronary stent thrombosis documented in coronary naroangiography or pathoanatomical examination.
Type 5. MI associated with coronary bypass surgery.
clinical picture. Clinical manifestations of MI are determined by the extent and localization of the focus of necrosis, the rate of its formation, the severity of the previous cardiosclerosis, the functional state of the heart muscle, individual characteristics of the regulation of the cardiovascular system, the nature of concomitant pathology.
Allocate typical (painful) and atypical variants of MI.
78

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
The classic pain variant of MI is observed in an average of 85% of patients. The intensity of pain, as a rule, exceeds the strength of anginal attacks habitual for the patient.
Often, heart attack pain becomes extremely strong, unbearable. Localized behind the sternum, the pain can spread to the left and right halves of the chest, the epigastric region. Along with typical irradiation to the left, pain sometimes radiates to the right
arm, right shoulder and right shoulder blade. The duration of the pain attack is from 20
– 30 min to several hours. In some cases, the pain syndrome acquires a wave-like character - periods of increased pain sensations alternate with periods of their weakening and even disappearance. A characteristic sign of pain in MI is the absence of the effect of oral administration of nitroglycerin and other antianginal agents.
Heart attack pain, as a rule, is stopped only by parenteral administration of narcotic drugs. analgesics. In most cases, the pain syndrome is accompanied by emotional motor excitement, fear of death, and a feeling of lack of air.
Physical examination of patients usually reveals pallor and increased moisture of the skin. Heart rate in many patients remains within normal limits,
however, moderate tachycardia is often observed due to emotional pain
stress. Moderate hypertension is often detected in the first hours of the disease. The
boundaries of relative cardiac dullness can be moderately expanded to the left, I tone is weakened. However, signs are not specific - even in combination with a weak systolic murmur on
at the apex of the heart and at the Botkin point, as well as the accent of the II tone on the pulmonary artery, they can
be associated with pre-MI cardiosclerosis. A somewhat more specific symptom is protodiastolic gallop (III tone), but this sign also indicates only a decrease in the contractile function of the left ventricle, which is not necessarily
caused by the development of MI. The diagnostic significance of the listed features is significantly increases if the doctor noted not just the presence, but their appearance in the patient.
Extensive transmural MI is characterized by the appearance of a pericardial friction rub, which is heard for a short time (sometimes only a few hours) on days 2–3.
diseases. A very common symptom of MI is arrhythmia. Single monotopic ventricular extrasystoles on the 1st day of the disease are recorded in more than 90% of patients. AT the first few days of the disease, an increase in body temperature to a subfebrile level is recorded, due to the development of resorption-necrotic syndrome and asep
tic inflammation in the tissues of the heart.
The clinic of the pain variant of MI is often supplemented by a variety of symptoms,
the appearance of which is determined by the nature and severity of the complications of the disease. For
atypical forms of MI (with the exception of oligosymptomatic) is characterized by a pronounced predominance
giving a complex of clinical signs corresponding to a specific complication, over
typical pain syndrome.
The asthmatic variant of MI is manifested by lack of air, shortness of breath, turning into suffocation. The pathophysiological basis of the asthmatic variant of MI is acute left
ventricular failure, so its detailed clinical picture corresponds to
clinic of cardiac asthma or pulmonary edema. Pain syndrome in this form of the disease it is expressed slightly or is perceived by the patient less acutely than suffocation. The
asthmatic variant is observed predominantly with repeated MI, especially in patients with left ventricular aneurysm, as well as in elderly and senile patients. Development of pulmonary
edema in the first hours after the development of MI in the absence of signs of severe cardiosclerosis often due to damage to the papillary muscles and the occurrence of relative insufficiency of
the mitral valve, resulting in a rapid increase
pressure in the pulmonary artery. In these cases, in addition to the clinical picture of acute left ventricular failure, physical examination reveals expansion
79

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
left atrium, weakening of the I tone and a rough systolic murmur at the apex of the heart and in the Botkin point.
The abdominal or gastralgic form of MI is characterized by pain in the epigastric area or right hypochondrium with irradiation into the interscapular space and along the sternum. The pain syndrome is combined with nausea, repeated, without relief vomiting, belching with air, hiccups, flatulence, paresis of the gastrointestinal tract. At in a number of patients, the abdominal form of MI is manifested by gastric or intestinal
bleeding due to the formation of erosions and acute ulcers of the gastrointestinal mucosa. tract. In most cases, patients with abdominal MI have bloating. If the paresis of the gastrointestinal tract progresses, symptoms develop
"Peritonism": there is pain on palpation of the abdomen and tension in the upper sections
of the abdominal wall. Most often, the abdominal form is observed in patients with diaphragmatic MI.
In the arrhythmic variant of MI, cardiac arrhythmias prevail over all other symptoms of the disease. Pain in the chest is either absent or
insignificantly expressed. The clinical picture is determined mainly by the nature
rhythm and conduction disorders of the heart. Usually, the arrhythmic variant of MI manifests itself paroxysms of ventricular and supraventricular tachycardia, AF, frequent extrasystole,
complete AV block. Rhythm and conduction disturbances such as paroxysmal ventricular tachycardia (VT), ventricular fibrillation, and complete AV block are accompanied by severe disorders of central hemodynamics and the development of Morgagni-Adams- Stokes syndrome.
The cerebrovascular variant of MI is characterized by a predominance of symptoms of cerebrovascular accident and is diagnosed mainly in elderly and
old age. Within this variant of MI, two clinical forms are distinguished, which are based on diffuse or local cerebral ischemia. diffuse
cerebral ischemia due to an acute decrease in cardiac output, manifests itself in the form fainting, cerebral symptoms (dizziness, nausea, vomiting) and mental disorders: weakening of memory, disorders of orientation in time, apathy, psychosis. Local ischemia of the brain occurs as a result of simultaneous thrombosis or spasm of the sclerotic cerebral artery with MI and is manifested by the symptoms of a cerebral stroke. The
development of hemiparesis may be accompanied by the appearance of cerebral symptoms. The asymptomatic variant of MI includes cases with poor clinical symptoms, for
example, an increase in angina pectoris attacks that are usual for a patient, the appearance of episodes of arrhythmia, shortness of breath, general weakness, malaise, etc.
symptoms of the disease is often the reason that the patient does not turn to doctor. The diagnosis of MI in such cases is established by chance - during the next
electrocardiographic study. About 1% of cases are not accompanied by clinical symptoms at all. However, asymptomatic MI appears to be much more common,
than diagnosed in hospitalized patients. According to the Framingham study, due to the absence of clinical manifestations of the disease, about 25% are not recognized.
THEM.
Laboratory and instrumental research. Myocardial enzymes enter the blood from necrotic cardiomyocytes. By activity and changes in the content of enzymes in the blood serum, the presence of MI and the timing of its occurrence are judged. Among
many enzymes contained in the cells of the heart muscle, aspartate aminotransferase, lactate dehydrogenase and creatine phosphokinase are considered the most significant for the diagnosis of MI. In addition to enzymes in MI, other compounds contained in
cardiomyocytes enter the bloodstream, in particular, myoglobin and cardiac troponins. Among the main
80
