
1-280 pdf (1)
.pdf
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Vulnerable or immature atherosclerotic plaque is distinguished by a thin connective tissue capsule and a liquid lipid core. Immature atherosclerotic plaques usually
do not cause hemodynamically significant vasoconstriction. Meanwhile, they are more dangerous formations than stable plaques, since the fibrous cap of such plaques are less resistant to hemodynamic factors and proteases. Violation
integrity of the tegmentum of an immature atherosclerotic plaque can lead to the formation occlusive thrombus and acute ischemia of the organ without previous signs of chronic
ischemia - for example, to the development of myocardial infarction without previous angina pectoris. At ed of a non-occlusive thrombus in the area of damage to an immature atherosclerotic plaque,
ischemia can increase due to the constrictor reaction of the smooth muscles of the vascular wall that have not lost their ability to contract in response to the effect of platelet secreted vasoactive compounds.
Morphology. Atherosclerotic lesions of the vascular wall are divided into
six stages (types). Type I is characterized by the accumulation of macrophages and foam cells under endothelium in places subject to the most intense mechanical stress
(branching and sharp bends of the arteries). Deposits of foam cells and lipid-laden smooth muscle cells form lipid streaks, which are a sign
type II lesions. Type III lesion is characterized by the presence of not only intracellular,
but also extracellular lipid deposition, as well as a violation of the integrity of the intima. By as they grow, extracellular accumulations of lipids merge into the lipid core of atherosclerotic plaques, the formation of which is regarded as a type IV lesion. For defeat type
V is characterized by the formation of a thick layer of fibrous connective tissue, which forms cover of an atherosclerotic plaque. The tegmentum is separated from the blood flow by a layer of endothelial cells. Signs of type VI lesions are cracks in the atherosclerotic plaque cap, hematomas, and internal thrombi.
Immature atherosclerotic plaques usually occupy less than half the circumference of the affected artery and slightly narrow its lumen. Due to the high content of lipids and the presence of a relatively thin connective tissue capsule, such plaques
are yellow. Mature atherosclerotic plaques are usually concentric and cause hemodynamically significant vasoconstriction. Plaques of this type have a white
color, because through their fibrous capsule (thicker than that of immature plaques) the lipid core does not shine through. A characteristic feature of mature atherosclerotic plaques is pronounced hypertrophy of smooth muscle cells.
clinical picture. Clinical manifestations of atherosclerosis are determined by localization, rate of progression, and severity of morphological changes. Most
often atherosclerosis develops in the coronary, cerebral, renal arteries, arteries of the lower extremities and the aorta. Until the narrowing of the vessel reaches a critical degree, thrombosis, aneurysm or embolism will not develop, atherosclerosis is asymptomatic. At
slow progression of the process and gradual narrowing of the affected vessel
naya symptomatology of atherosclerosis reflects the impossibility of increasing blood flow with an increase
reducing tissue oxygen demand. Examples of such a variant of the course of atherosclerosis can be serve as angina pectoris and intermittent claudication. Slow narrowing of the renal arteries
is manifested by vasorenal hypertension. In the event of a sudden blockage of an artery due to thrombosis or embolism, clinical symptoms of acute ischemia occur (for example,
MI, stroke). With a widespread lesion of large arteries, the formation of aneurysm. The most common cause of atherosclerosis is abdominal aneurysms. aorta.
Sometimes, usually in patients with familial (hereditary) hyperlipidemia, there is a
deposition of lipids in the thickness of the skin - xanthoma and xanthelasma. Xanthomas represent
21

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
a thickening along the Achilles and other tendons, in the area of the metacarpophalangeal joints. In some cases, tuberous xanthomas form on the elbows and small xanthomas on
body skin. Xanthelasma are yellowish nodules on the eyelids and the skin around eye. Lipoid arch is a pathognomonic sign of familial hypercholesterolemia.
cornea - a bright formation in the form of a ring or half ring along the edge of the cornea. Laboratory and instrumental diagnostics. In a significant proportion of patients with
clinical signs of the disease, which is based on atherosclerosis, reveal characteristic changes in the lipid spectrum of the blood. Dyslipidemias are often detected and
at the preclinical stage of the course of atherosclerosis. However, the normal lipid spectrum
blood does not exclude the diagnosis of atherosclerosis.
Imaging methods are used to detect atherosclerosis in large and medium arteries, mainly radiopaque angiography and ultrasound. In recent years, more and more advanced methods have been used in clinical practice.
imaging methods - intravascular ultrasound, computed tomography, magnetic resonance imaging. With the help of modern imaging techniques
it became possible to diagnose the initial signs of atherosclerosis, assess the size of atheromas and their relationship with the vascular wall, and detect ulcerated atherosclerotic plaques.
According to the requirements of national recommendations for the diagnosis and correction of lipid metabolism disorders, all men are subject to screening for the detection of dyslipidemia. over 35 and all women over 45. Screening is recommended for
contacting a doctor, regardless of the reason, and in the process of periodic preventive examinations. In these categories of patients, it is recommended to determine the concentration total cholesterol in the blood and at its normal value, repeat the analysis of total cholesterol once a 5 years. If the concentration of total cholesterol exceeds 5 mmol / l, it is necessary to obtain a
detailed lipid spectrum: total cholesterol, TG, HDL cholesterol, LDL cholesterol, determine the risk of complication SCORE scale, make recommendations for lifestyle changes and then, if necessary,
prescribe medication. In men aged 20-35 and women aged 20-45, screening
it is recommended to carry out in the presence of diabetes mellitus, heredity aggravated by cardiovascular diseases, family history suggesting hereditary
hyperlipidemia, and a combination of several risk factors. In this category of patients
you need to get a complete lipid profile. In children and adolescents, analysis of the full blood lipid spectrum is considered necessary if there is a family history aggravated by
on cardiovascular diseases.
The examination of a patient with suspected dyslipidemia or a disease whose morphological basis is atherosclerosis involves several stages. First, it is necessary to determine the complete lipid profile in the blood taken on an empty stomach (after 9–12 hours of fasting) and calculate
the atherogenic coefficient. Then you need to determine the presence of the main
clinical manifestations of atherosclerosis (IHD, atherosclerosis of the carotid arteries, obliterating atherosclerosis of the vessels of the lower extremities, aneurysm of the abdominal aorta) and / or
main risk factors (smoking, hypertension, family history of early manifestation of coronary artery disease, age).
After that, it is necessary to determine the category of 10-year risk of death from cardiovascular diseases and set the target value of LDL-C in accordance with the category
risk. The listed measures are necessary for a reasonable choice of treatment tactics. in relation to a particular patient and monitoring the effectiveness of his treatment.
Diagnosis. In those cases when atherosclerosis is the morphological basis of any disease that has distinct independent clinical manifestations (various clinical forms of coronary artery disease, acute cerebrovascular accident, vasorenal
AG), this term is not accepted when formulating the diagnosis. If the disease
22

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Since structural disorders of the wall of large arteries and valvular apparatus associated with atherosclerosis, the term "atherosclerosis" is included in the diagnostic formula.
Diagnosis examples.
1.Atherosclerosis of the aorta. Aneurysm of the abdominal aorta.
2.Atherosclerosis of the aorta. Dissecting aortic aneurysm. Acute
aortic valve insufficiency.
Flow. Atherosclerosis is characterized by an undulating course with a change of periods exacerbations and remissions. During exacerbation of atherosclerosis, the formation of
new atherosclerotic plaques and their rapid growth, damage to plaques with the formation
of intravascular thrombi and corresponding clinical symptoms are noted. During the period of remissio clinical manifestations of atherosclerosis are determined by the localization and severity
of vascular obstruction, i.e., the degree of chronic ischemia of the organ receiving blood supply from the affected artery. In cases of slow progression, atherosclerosis can
time - until the formation of a physiologically significant vasoconstriction - not accompanied by
clinical symptoms.
Forecast and outcomes. Risk of development and nature of complications, life expectancy patients and the causes of deaths are determined by the type and characteristics of the
course of diseases developing on the basis of atherosclerosis. Important for the forecast are
the rate of progression of atherosclerosis and the severity of adaptive processes in the organs and
ischemic tissues.
Treatment. Non-drug treatment. The basis of primary and secondary prevention of atherosclerosis is a change in lifestyle. Non-pharmacological treatment measures interventions include diet, weight management, increased physical activity, and smoking cessation.
The number of calories consumed with food should not exceed what is necessary to maintain the ideal body weight for the patient. You need to limit your fat intake animal origin. The amount of fat (including vegetable fats) consumed in
during the day, should be no more than 30% of the total calorie content, and the proportion saturated fat should be no more than 7% of their total. In individuals without dyspoproteinemia, clinical manifestations of atherosclerosis, and a 10-year high risk of death from cardiovascular diseases, the intake of cholesterol from food should not exceed 300 mg / day In other cases, the daily intake of cholesterol with food should be limited to 200 mg.
The negative effect of dietary cholesterol on lipid metabolism is less significant than consumption saturated fats. In this regard, when explaining to the patient the principles of healthy eating
the need to reduce the consumption of saturated fats should be emphasized first of all. It is advisable to replace hard margarines and cooking fats with vegetable oil. From the diet should be excluded meat products with a high fat content,
replacing them with lean meats, fish, poultry, legumes. Oily sea fish (salmon, tuna, mackerel), containing omega-3-polyunsaturated fatty acids that prevent the development of atherosclerosis, it is recommended to use 2-3 times a week. Daily consumption
fresh vegetables and fruits that contain dietary fiber that prevents absorption cholesterol, should be (excluding potatoes) at least 400 g. Daily should be consumed milk and dairy products with low fat content. The proportion of sugar in the daily diet (including sugar found in food) should not exceed 10% of the total calories. The total amount of table salt consumed per day should not exceed
more than 6 g. The following energy ratio is considered optimal: proteins - 15%, fats - 30%, carbohydrates - 55% of the total calories per day.
23

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Body mass index (BMI) is used to estimate body weight, which is calculated
according to the following formula:
2 BMI \u003d Weight, kg: Height, m
The normal body mass index is in the range of 18.5 - 25 kg / m2 . Weight reduction body is achieved by a low-fat diet and regular exercise. In cases where achieving optimal body weight is difficult,
it is recommended to reduce the weight by 10% from the original or achieve a decrease in body mass index up to
27 kg/m2 with subsequent maintenance of this indicator at the achieved level.
When choosing the level of daily physical activity, it is necessary to take into account the age of the patient, the state of the cardiovascular system, the musculoskeletal system, and other anatomical and physiological systems. The most physiological, safe and affordable type of physical activity is walking. Recommended duration of classes -
30 - 45 minutes, frequency - 4 - 5 times a week. When choosing an individual walking pace, it is advisable to focus on the heart rate, which is at the height of the load
should reach 70% of the maximum for a given age. The maximum heart rate is calculated using the formula:
HRmax = 220 - age (years)
For patients with coronary artery disease, when determining the optimal pace of walking, it is necessary dimo take into account the results of the test with physical activity (veloergometry).
Smoking cessation is an essential component of successful prevention atherosclerosis. When receiving recommendations to give up this bad habit, the patient should be informed that not only
active, but also passive smoking. If needed to facilitate smoking cessation
nicotine replacement therapy may be used.
According to the results of a number of experimental and clinical studies, consumption
small doses of alcohol may reduce the risk of death from coronary artery disease. The protective effect of alcohol
associated with its anti-stress effect, an increase in the level of HDL cholesterol and a decrease in the pro-coagulant potential of blood plasma. However, alcohol abusers
the risk of death increases significantly. Safe for health is the daily consumption of pure alcohol, not exceeding 30 g for men and 20 g for women. Patients with hypertension gout, obesity and heart rhythm disorders alcohol consumption is not recommended.
In patients taking statins, alcohol consumption can provoke rhabdomyolysis. Taking into account national characteristics, it is inappropriate for residents of Russia to recommend
the goal of preventing atherosclerosis is regular consumption of even small doses of alcohol, since this is associated with a high risk of developing alcohol dependence, the harm of which far outweighs the benefit of this recommendation.
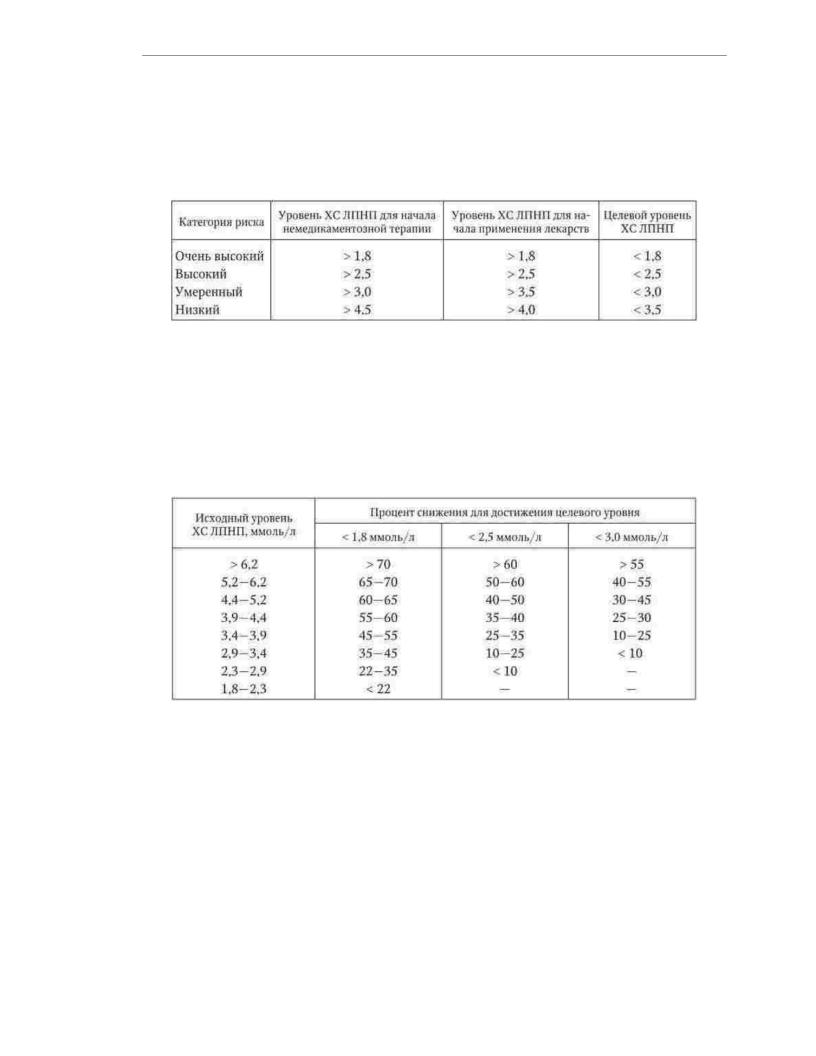
Medical treatment. Indications for the use of drugs are determined depending on the category of 10-year risk of death from cardiovascular diseases and the level of LDL-C of the patient (Table 1.4). In individuals with moderate and low risk, only non-pharmacological measures for the prevention of atherosclerosis can be used for
3 months If during this time it is not possible to achieve the target level of LDL-C, medical treatment is started. In high and very high risk patients, the use of drugs
drugs should be started simultaneously with non-drug treatment. Before the beginning
24
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
treatment, it is recommended to calculate by how much (as a percentage of the initial value)
it is necessary to reduce the content of LDL cholesterol in the blood to achieve the target level (Table 1.5).
Table 1.4
Levels of LDL cholesterol to determine the tactics of treating patients and target levels
LDL cholesterol depending on risk category (mmol/l)
Medications for the correction of lipid metabolism disorders include:
HMG-CoA reductase inhibitors (statins), ezetimibe, bile acid sequestrants (ion exchange resins), fibric acid derivatives (fibrates), nicotinic acid (niacin)
and omega-3 polyunsaturated fatty acids.
Table 1.5
LDL-C reduction required to achieve target level (% from original)
Statins. The mechanism of action of statins is based on the inhibition of the key
enzyme of the initial stages of cholesterol synthesis, HMG-CoA reductase. With a decrease in the activity o enzyme, a short-term intracellular deficiency of cholesterol occurs. As a result, hepatocytes
express an increased number of LDL receptors, which leads to an increase in the uptake of LDL-C from blood plasma. At the same time, due to a change in the ratio of intermediate
forms of lipoproteins, a moderate decrease in the level of triglycerides occurs, and in connection with this and some increase in HDL levels. In addition to affecting the blood lipid spectrum, statins
have a number of additional (pleiotropic) effects, the main of which are:
suppression of the synthesis of inflammatory mediators, improvement of endothelial function, prevention oxidative modification of LDL, stabilization of the fibrous capsule of atherosclerotic
plaques, antithrombogenic action. Statins are used to treat patients with type IIa, IIb, and III hyperlipidemias. This class of drugs can lower LDL cholesterol levels.
by 25 - 50%. Some statins also have hypotriglyceridemic effects. For example, the use of atorvastatin can reduce the level of triglycerides by 25-45%. In clinical
25

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
In practice, the following drugs are used: lovastatin (mevacor) - 20 - 80 mg / day, simvastatin (zocor) - 10 - 40 mg / day, pravastatin (lipostat) - 20 - 40 mg / day, fluvastatin (lescol) - 20 - 40 mg / day, atorvastatin (liprimar) - 10 - 20 mg / day, rosuvastatin (crestor) - 5 - 10 mg / day
day In recent years, the concept of "aggressive" lipid-lowering therapy has become increasingly popular, according to which patients at high and very high risk for
achievement of target LDL-C values, high doses of statins are used: simvastatin
and atorvastatin - up to 80 mg / day, rosuvastatin - up to 40 mg / day. To lower LDL cholesterol levels simvastatin at a dose of 40 mg/day, atorvastatin at a dose of 20 mg/day, rosuvastatin at a dose
of 5–10 mg/day, to reduce LDL cholesterol by 45–50%
from the initial dose of simvastatin should be 80 mg / day, the dose of atorvastatin - 40 mg / day, dose of rosuvastatin - 20 mg / day. Statins are used once a day, in the evening, after meals. Statins are fairly safe drugs. Occasionally taking statins
may be accompanied by abdominal pain, flatulence, constipation. In 1-3% of patients, an increase in the activity of liver enzymes is observed. Stopping statins is considered justified if, during treatment, the level of alanine or aspartic aminotransferase in two consecutive measurements exceeds the upper limit by more than 3 times
normal values. Myalgia and myopathy occur in less than 1% of statin cases. Severe myopathy is manifested by muscle pain, muscle weakness, and an increase in creatine phosphokinase activity, 5 times the upper limit of normal.
If myopathy is not diagnosed in a timely manner and statins are not stopped, it is possible the development of rhabdomyolysis, a rare and severe complication of drug therapy.
Ezetimibe inhibits cholesterol absorption, which causes a decrease in its content in
hepatocytes, and as a result, an increase in the expression of LDL receptors and an increase in cholesterol up LDL from blood plasma. The drug does not affect the absorption of fatty acids, triglycerides
and fat-soluble vitamins. Ezetimibe is recommended for use in combination with statins for their insufficient effectiveness in average therapeutic doses. It is possible to use this
the drug and in monotherapy with individual intolerance to statins. ezetimibe is prescribed at a dose of 10 mg once a day, regardless of food intake.
Bile acid sequestrants are complex polymeric compounds that bind bile acids in the lumen of the small intestine, preventing their reabsorption. As a result, the synthesis of bile acids in the liver is activated and the need for
in the cholesterol required for this process. Increased expression of receptors in hepatocytes LDL, which increases the flow of cholesterol from the blood to the liver cells. On the background treatment with bile acid sequestrants, the level of LDL cholesterol is reduced by 15 - 30%. Bile acid sequestrants have been used as lipid-lowering drugs for more than 30 years.
The best known drugs of this class are cholestyramine (8–24 g/day) and cholestipol (5–30 g/ day). Treatment with these drugs often causes constipation and dyspeptic disorders. Side effects of bile acid sequestrants include
hypertriglyceridemia. In this regard, they are contraindicated in hyperlipidemia III and IV. types. In addition, bile acid sequestrants interfere with the absorption of other drugs and fatsoluble vitamins, so they should be taken 1 to 2 hours before or
4 hours after taking other drugs.
Fibrates activate hepatic lipoprotein lipase, inhibit enzymes involved in the synthesis of fatty acids, increase the excretion of cholesterol in the bile. Due to the influence on the metabolism of VLDL, fibrates significantly, by 30-50%, reduce the level of triglycerides. In
addition, drugs of this class cause a decrease in the level of LDL cholesterol by 10–15% and an increase in the HDL cholesterol by 10 - 20%. The main indication for the use of fibrates is type IV
hyperlipoproteinemia in combination with a low level of HDL-C. In cases of combined hyperlipoproteinemia (types IIb and III), a combination of fibrates with statins is possible. Doses
26

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
and the frequency of taking the main drugs in this group are: ciprofibrate (Lipanor) - 100 mg 1-2 times a day, bezafibrate (cholestenorm) - 200 mg 2-3 times a day, fenofibrate (lipantil 200 M and tricor 145 mg) - 200 mg and 145 mg, respectively, 1 time per day. Side effects of fibrates are observed in 5-10% of patients. The most frequent of these are nausea, abdominal pain, constipation, diarrhea, flatulence. In some cases, headaches
pain and insomnia. The combination of fibrates with statins increases the risk of myopathy. The use of first generation fibrates was associated with an increased risk of gallstone disease. This side effect is not characteristic of modern drugs.
Nicotinic acid has a hypolipidemic effect by inhibiting the synthesis of VLDL due to a decrease in the intake of fatty acids from adipose tissue. This
the effect is manifested when using nicotinic acid at a dose of 2 - 4 g / day. Against the backdrop of treatment nicotinic acid, there is a decrease in the level of LDL cholesterol by 10 - 20%, a decrease in the level TG by 20 - 30% and an increase in HDL cholesterol levels by 15 - 20%. The main indication
for the use of nicotinic acid is type IIb hyperlipoproteinemia, as well as hypertriglyceridemia in combination with a low level of HDL cholesterol. Nicotinic acid is advisable to prescribe patients in whom the listed types of hyperlipidemia are combined with obliterating atherosclerosis of the vessels of the lower extremities, since this compound has a strong vasodilating effect. The prolonged form of nicotinic acid - the drug enduracin - is prescribed at a dose of 0.5 g 3 times a day. Side effects: flushing of the face and upper
half of the body, feeling of heat, tachycardia, pruritus. These events can be mitigated
increasing the dose of nicotinic acid gradually and prescribing aspirin 30 minutes before taking it at a dose of 0.125 g. It is recommended to take nicotinic acid during a meal.
Omega-3-polyunsaturated fatty acids have a combined anti-atherogenic effect by enhancing the fibrinolytic activity of plasma, anti-inflammatory action, restoring endothelial function, and improving the functional state
cell membranes, lowering the level of triglycerides in the blood plasma. Drugs in this class recommended for the treatment of patients with hyperlipidemia IV and V types. The use of omega-3- polyunsaturated fatty acids can improve the prognosis of patients after myocardial infarction,
by reducing the risk of general, cardiovascular and sudden death. This effect is associated with their stabilizing effect on cardiomyocyte membranes. In Russia, one drug containing highly purified omega-3-polynene saturated fatty acids, omacor, has been registered. One capsule of the drug contains about 0.9 g of omega-3-
polyunsaturated fatty acids. It is recommended to correct hypertriglyceridemia take 2-4 capsules of omacor per day.
In some cases, usually in patients with familial dyslipoproteinemia, with a significant increase in the levels of cholesterol and atherogenic lipoproteins, a plasmapheresis procedure is used to correct the blood lipid spectrum. Selective plasmapheresis makes it possible to selectively remove LDL from the blood using immune and chemical sorbents. Regular plasmapheresis procedures in combination with drug therapy provide
stable lipid-lowering effect and inhibition of the progression of atherosclerosis.
27

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
1.3. HYPERTONIC DISEASE
Definition. The term "arterial hypertension" refers to a syndrome of increased
HELL. The diagnostic criterion for hypertension is an increase in systolic blood pressure to 140 or more.
mmHg Art. and / or an increase in diastolic blood pressure to 90 or more mm Hg. Art.
Hypertension (AH) is a chronic disease, the main manifestation
which is the syndrome of hypertension, not associated with the presence of pathological
processes, in which the increase in blood pressure is due to known causes (symptomatic or secondary AG). The term "hypertension" was proposed by G. F. Lang and is synonymous with
used in other countries, the term "essential arterial hypertension".
Prevalence. Elevated blood pressure is recorded on average in 25% of adults.
The frequency of hypertension progressively increases with age: in the population up to 39 years,
the prevalence of hypertension is 10–15%, in the population over 60 years it is more than 50%. In the elderly and senile age is somewhat less common than in young and middle-aged people, it is noted
isolated diastolic hypertension, but isolated systolic hypertension is much more common.
In the Russian Federation, the prevalence of hypertension is 39.2% among men and 41.1% among women. Know about the presence of hypertension 37.1% of men and 58.9% of women. 21.6% of men and 45.7% of women take antihypertensive drugs, but only 5.7% of men and 17.5% of women are treated effectively (i.e. achieve normal blood pressure levels).
Hypertension is the most important risk factor for cardiovascular disease. Population studies have shown that hypertensive patients, compared with those with normal blood pressure,
are significantly more likely to develop stroke, coronary artery disease, and congestive heart failure. insufficiency. As a result, the decrease in mortality from cardiovascular diseases in
largely determined by the effectiveness of the treatment of GB.
Etiology. According to modern concepts, the main risk factor for the development of HD is hereditary burden for this disease. By now
Numerous genes have been identified whose defects predispose to hypertension. These include genes for angiotensin converting enzyme (ACE), angiotensinogen, renin, genes,
determining the volume of extracellular fluid, response to salt load and reabsorption sodium, sensitivity of tissues to insulin, permeability of cell membranes, function
ion channels, etc. Other factors also contribute to the development of HD: age, overweight body, the consumption of table salt in an amount exceeding the physiological norm, insufficient content of potassium, calcium and magnesium in food, hypodynamia, smoking, alcohol abuse. Psychoemotional stress is the strongest exogenous risk factor for HD. The importance of the neuropsychic overstrain that occurs
after acute and prolonged emotional overload, in the stabilization of hypertension was emphasized in classical works of G. F. Lang and A. L. Myasnikov. Later, an association was found
development of this disease with personality traits. Patients at high risk of AH stabilization are characterized by latent aggressiveness, ambition, striving for leadership,
emotional lability, haste and impulsivity. These qualities are often combined with a feeling of constant anxiety and periods of depression.
The development of HD depends on the interaction of genetic and environmental factors. Mechanisms
this interaction remains completely unexplained. However, there is reason to believe that the causal relationships between the two groups of factors indicated are
bidirectional character: on the one hand, genetic characteristics determine the reaction organism on environmental factors, and on the other hand, exogenous influences contribute to the manifestation of genetic defects.
28

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Pathogenesis. The main physiological parameters that determine the level of blood pressure, are stroke volume, circulating blood volume, aortic wall elasticity and
its large branches, resistance to blood flow at the level of small arteries and arterioles, viscosity blood. The leading role in the formation of blood pressure is played by two hemodynamic indicators: minute volume of blood circulation, which is the product of stroke volume
on heart rate, and total peripheral vascular resistance. Under conditions of normal neurohumoral regulation of blood circulation, the volume of blood pumped by the heart into the vessels, and vascular tone are interdependent - a change in one of these parameters leads to opposite changes in
the other. Due to the balance of the minute volume of blood circulation and the total peripheral vascular resistance, the level of blood pressure, which is optimal for the body, is maintained and its sharp fluctuations are prevented. Violation
regulation of cardiac performance and vascular tone, as well as their mutual influence
leads to inadequate changes in blood pressure.
The following options for changes in central hemodynamics are distinguished, causing
sustained increase in blood pressure:
1) an increase in the minute volume of blood circulation in the absence of an adequate decrease vascular resistance;
2)an increase in vascular resistance in the absence of an adequate decrease minute volume of blood circulation;
3)combined increase in minute volume of blood circulation and vascular resistance
leniya.
The prevalence of various hemodynamic variants of AH is not the same. More
than in 80% of cases in patients with GB there is an increase in the total peripheral vascular resistance.
According to the neurogenic concept of the pathogenesis of HD, developed by G.F. Lang and A. L. Myasnikov, the basis of this disease is a violation of the regulation of blood circulation, which occurs as a result of overstrain and traumatization of the human mental sphere. An important role in the development of hypertension is played by the activation of the sympathetic-adrenal system. On the At the initial stage of the disease, many patients have hypercatecholaminemia, which is manifested by an increase in heart rate and myocardial contractility with the formation of a hyperdynamic type of hemodynamics and an increase in vascular tone. Besides,
sympathicotonia is accompanied by an increase in the synthesis of other neurohormones that contribute to increase in blood pressure due to the effect on arterial tone, sodium and water reabsorption (renin, angiotensin II, aldosterone, vasopressin). Activation of the sympathetic-adrenal system is a mechanism through which the hemodynamic effects of psycho-emotional stress are realized, which combines this concept with the neurogenic concept.
pathogenesis of GB. However, there are other causes of hypersympathicotonia: a change
sensitivity of baroreceptors and adrenoreceptors, impaired reuptake of noradrenaline in the synaptic cleft, decreased tone of the parasympathetic nervous system.
The development of hypertension may be associated with a disorder in the mechanisms of regulation of water-salt
exchange, due to which sodium retention occurs and hypervolemia develops. Nephrosclerosis (including developing in the late stages of HD) is not the only cause of impaired renal excretory function. Retention of sodium and water in the body can
be due to the activation of sympathetic-adrenal and renin-angiotensin-aldosterone
systems, as well as a decrease in the activity of the natriuretic peptide system. According to the concept of A. Guyton, a decrease in the ability of the kidneys to excrete sodium, which is noted in a number of patients at an early stage of the disease, is not a consequence, but the cause of
hypertension. An increase in blood pressure in such cases is a compensatory reaction that provides
29

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
increased natriuresis and thus aimed at maintaining a normal water-electrolyte balance.
The "membrane" theory of the pathogenesis of hypertension, proposed by Yu. V. Postnov and S. N. Orlov, explains the increase in blood pressure by a genetically determined defect in plasma membranes, as a result of which the transmembrane transport of calcium ions is disrupted.
The accumulation of calcium in the cytosol causes an increase in the tone of smooth muscle cells of the vascular walls and increased contractility of cardiomyocytes, and also contributes to the activation of the sympathetic-adrenal system and is accompanied by an increase in the sensitivity of cells to the
pressor action of norepinephrine.
According to modern concepts, neurohumoral imbalance plays a leading role in the increase in blood pressure in the early stages of AH development, the most important manifestation of which is impaired functioning of the renin-angiotensin-aldosterone system.
systems. The main effector peptide of this neurohumoral system, angiotensin II, not only circulates in the bloodstream, but is also formed in tissues. Circulating angiotensin II causes short-term effects: increased heart rate, vasoconstriction, sodium and water retention. Tissue angiotensin II causes long-term effects of activation of the renin-angiotensin-aldosterone system, which include
myocardial hypertrophy, formation and progression of cardiosclerosis, hypertrophy
smooth muscle cells of the vascular wall, decreased elasticity and persistent narrowing of the lumen of small arteries, increased pressure in the renal glomeruli with their subsequent death and development of nephrosclerosis. Activation of the renin-angiotensin-aldosterone system contributes to the development of endothelial dysfunction, which is manifested by an imbalance of biologically active substances secreted by endothelial cells: production of nitric oxide, endothelial hyperpolarization factor and prostacyclin, which have vasodilatory, antiproliferative and antiaggregant properties, decreases, and the production of endothelins,
thromboxane A2 and other compounds that cause vasoconstriction, proliferation of smooth muscle cells and platelet aggregation increases.
In the "metabolic" theory of the formation of hypertension, the central role is given to insulin resistance of tissues. Decreased tissue sensitivity to insulin due to mutation
genes and the influence of environmental factors. In most cases, insulin resistance combined with obesity and is accompanied by endothelial dysfunction, increased content
sodium and calcium in the smooth muscle cells of the vascular wall, which contributes to their proliferation and increase the sensitivity of small arteries to vasoconstrictor effects.
Insulin resistance results in hyperinsulinemia, which in turn
leads to an increase in the activity of the sympathetic-adrenal system, hypertrophy of the smooth vascular musculature, increased sodium reabsorption. In addition to the changes that
an increase in blood pressure, insulin stimulates the synthesis of cholesterol and the process of lipid oxidation in the vascular wall, thereby contributing to the progression of atherosclerosis.
Thus, the mechanisms of AH formation are diverse. The combination of pathogenetic mechanisms and their role in the formation and progression of HA are determined by the individual set of genetically determined and environmental factors of each patient.
Morphology. AH is accompanied by the development of morphological changes in target organs, the main of which are the heart, arterial vessels, kidneys and brain.
A characteristic sign of "hypertonic heart" is an increase in the mass of the myocardium of
the left ventricle. In the myocardium of hypertensive patients, not only the mass of myocytes increases, but and the content of the extracellular matrix, fibroblast hyperplasia develops and collagen production increases, i.e. cardiosclerosis progresses. Similar changes occur in the walls of the main arteries, thickening and fibrosis of which are accompanied by
thirty
