
1-280 pdf (1)
.pdf
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
There is not always a direct relationship between the brightness of the description,
subjective intolerance of arrhythmias, on the one hand, and their clinical significance, on the other hand. another. This fully applies to complaints of palpitations. The most striking complaints
as a rule, not allowing to doubt the cause of the heartbeat, present patients with the so-called paroxysmal AV tachycardias due to the presence of an anomaly
conducting system of the heart (WPW syndrome, etc.). An important differential diagnostic sign is the sudden onset and end of an attack. Patients usually say that the heartbeat begins suddenly, with a sharp increase in heart rate. It ends with stupas just as suddenly, with a sensation of a blow (shock), "fading" of the heart. Many are turning
attention to the presence of polyuria at the time of the attack, but polyuria can also occur during
paroxysmal AF, and even with sinus tachycardia. Most often, AV tachycardia has to be differentiated from sinus tachycardia and paroxysmal AF. With careful
collecting anamnesis, it turns out that the onset of sinus tachycardia almost never happens instantaneous: the rhythm increases gradually, at least a few seconds should pass, more often minutes. Similarly, a palpitation attack, which is a sinus tachycardia,
never ends abruptly: patients report that the heart rate decreases
gradually. As for paroxysms of AF, they, like paroxysms of AV tachycardia, can begin suddenly (although not always, they are often preceded by interruptions in work
hearts), but almost never suddenly end. In addition, FP is usually arrhythmic palpitations in contrast to AV tachycardia and sinus tachycardia.
It is advisable to isolate night attacks of palpitations, which are especially often women complain. Typically, these attacks are sinus tachycardia.
and are the result of panic attacks in patients with anxiety-depressive disorders
properties.
Actions that patients take to stop palpitations,
quite often help to answer the question about their origin. Thus, even before their first visit to the doctor, many patients with AV tachycardia know that a heart attack can stop with a deep breath and holding the breath. At the same time, we note
that the most common subjective sign of paroxysmal tachycardia or AF is a sensation palpitations - in a number of patients may be absent. This happens either with a small Heart rate (within 130 in 1 min), or, oddly enough, with severe tachysystole (220 - 250
in 1 min or more), when, in the absence of complaints about the heartbeat, the patient may present
complaints of severe weakness, dizziness, shortness of breath, etc.
Often the appearance of paroxysmal tachyarrhythmias is not associated with any external reasons. However, when questioning, it is often possible to find a relationship between an attack of tachycardia and physical or emotional stress, sudden movements. Especially
this information is important for patients with paroxysmal AF: sympathetic-dependent
AF (at the height of the load, an increase in heart rate) and vagodependent (in the evening and at night, at background of sinus bradycardia) are treated differently.
Important clinical characteristics of tachyarrhythmias revealed during questioning and often determining treatment tactics are the frequency of occurrence and duration
seizures, conditions for relief, as well as the presence and nature of complications. Depending on the of these characteristics in tachyarrhythmias, treatment tactics can vary over a very wide range. limits: the use of vagal techniques, relief of seizures with antiarrhythmic drugs (AAP),
permanent antiarrhythmic therapy, surgical treatment.
The totality of complaints that appear in patients against the background of palpitations can (very conditionally) combined under the name "complications": after all, we evaluate the subjective
feelings of patients, among whom the proportion of emotionally labile people is quite large. So, for example, complaints about a sharp weakness that appears during an attack of tachycardia,
201

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
dizziness, blurred vision, tinnitus may, but need not, be associated with a decrease (fall) in blood pressure due to a decrease in heart rate.
ejection and minute volume of blood circulation against the background of a large heart rate. Syncope with tachyarrhythmias due to a sharp hemodynamic disorder is more rare, but rather formidable complication, often indicating the need for surgical
treatment. However, even emotionally labile subjects can often complain of fainting even
against the background of sinus tachycardia. Even more difficult to associate with hemodynamic disorders complaints about the appearance of paresthesias or sweating, but they cannot be ignored, since they many patients pay attention to the doctor.
Pain in the region of the heart during a heart attack can be very important
symptom. Of course, most often these are cardialgias (pain of a stabbing or aching nature, different in intensity and duration, often radiating to the left shoulder blade), but
sometimes - typical anginal pain, which, apparently, should be considered as angina pectoris voltage. Their distinguishing feature is a greater duration than with ordinary angina attacks; they can end with the development of an acute MI in a patient.
Often, patients complain of a feeling of lack of air and even suffocation.
However, they are associated with acute left ventricular failure only in exceptional cases: for example, in patients with chronic heart failure III-IV functional class on
background of postinfarction cardiosclerosis, valvular heart disease.
When questioning patients with bradyarrhythmias (AV blockade, dysfunction of the SU), complaints reflecting the presence of syncopal or presyncopal conditions are of great importance: sudden unmotivated weakness, dizziness, darkening in the eyes, noise in
ears, feeling of "cotton legs", partial or complete loss of consciousness. Necessary if possible
it is necessary to ask not only patients, but also their relatives who were present at the
fainting or fainting. Note that patients with bradyarrhythmias are very rare
lose consciousness absolutely suddenly, "fall backwards, as if knocked down." It'sthe same as involuntary urination and defecation, more typical for tachyarrhythmias, in particular ventricular. Patients with bradyarrhythmias usually have time to sit or lie down, so severe injuries from syncope are relatively rare. They are not characterized by convulsions,
tongue biting, retrograde amnesia.
Typical for patients with bradyarrhythmias are complaints of weakness, increased fatigue, limitation of physical activity, etc. They arise due to
inconsistencies in heart rate to the needs of the patient and are called chronotropic insufficiency.
Of considerable importance in the diagnosis of some arrhythmias and even in determining the therapeutic
tactics may have a family history. As you know, there is a whole group of genetically deterministic, inherited diseases: long QT-interval syndrome, syndrome
Brugada and others, manifested by life-threatening ventricular arrhythmias. Therefore, when asking patients with a history of presyncopal and syncope, it is necessary to
find out if there was an unexplained early sudden death, unmotivated syncope among close relatives.
Examination of patients with rhythm and conduction disturbances is not as important as questioning. Even 100 years ago, rhythm and conduction disorders of the heart identified and differentiated by observing the venous pulse and palpating at the same time heart impulse, comparing arterial and venous pulses, etc. However, just as in
many other branches of internal medicine, the role of examination has been largely lost with the advent of modern instrumental methods of examination.
Of course, in some, especially urgent situations, determine the nature of the arrhythmia It is possible with the help of such basic characteristics of the pulse as frequency, rhythm
and filling. It will not be difficult to identify extrasystole by pulse. With the help of simple functions
202

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
rational tests (exercise, breath holding), it is possible to make a differential diagnosis between sympathetic-dependent and vago-dependent extrasystoles. Using a sample with
physical activity (squats), in some cases it is possible to distinguish weakness syndrome SU (SSSU) and vagotonic dysfunction of the SU. It is also quite enough to detect AF palpation of the pulse. The concept of pulse deficit has not lost its clinical significance. with FP.
Thus, it can be argued that at the present time questioning and examination are
an integral part of the examination of patients with rhythm and conduction disorders of the heart. Methods of instrumental examination of patients with rhythm and conduction disorders
of the heart, drug tests. The most common method for diagnosing arrhythmias and conduction disorders of the heart is an ECG, usually in 12 conventional leads, including 6 chest ones. However, there are a number of more modern methods
examinations of patients with arrhythmias, the basis of which is also an ECG. Holter monitoring with wearable recorders (see color incl.,
rice. 1.17) provides for recording an ECG in two, three or twelve leads for 24,
48, 72 hours or more.
Long-term monitoring not only increases the diagnostic capabilities of the ECG,
but also allows assessing the dynamics of the disease, the effectiveness and safety of drug and interventional treatment. The technique allows to identify asymptomatic arrhythmias,
establish their exact number and characteristics, compare them with complaints, identify conditions, in which they occur (physical or emotional stress, time of day, etc.).
The use of multifunctional monitoring (ECG + blood pressure, ECG + blood pressure +
respiration, ECG + blood pressure + respiration + pulse oximetry) expands the diagnostic possibilities. event recorders. To diagnose rare arrhythmias,
so-called event recorders (event-recorder), wearable and implantable (see color on, fig. 1.18) were used. The latter are implanted under the skin for a period of 1 to 3 years.
It should be noted that modern pacemakers and implantable cardioverter-defibrillators (ICDs) are also equipped with the function of recording an electrocardio signal; they can be used to diagnose arrhythmias. ECG transmission is also used
by phone (when complaints arise or at a fixed time).
The signal-averaged ECG is used to record the late potentials of the ventricles.
kov - low-amplitude high-frequency electrical signals localized at the end
QRS complex or at the beginning of the ST segment. The relationship between the presence
of ventricular late potentials and the risk of life-threatening ventricular arrhythmias has been established. in patients with structural changes in the heart, especially after myocardial infarction (M. Simson, 1981
– 1987).
Late ventricular potentials are not visible on a conventional ECG, since their amplitude is comparable to the noise level. For their selection, the Simson method is used - averaging a
number of QRS complexes with subsequent filtering of the signal. During the averaging process, the level de noise, which usually requires averaging from 150 to 300 cardiocycles. According to received
signal, three indicators are calculated: the duration of the filtered QRS complex,
the duration of low-amplitude signals at the end of the complex and the average amplitude
the last 40 ms of the filtered QRS complex. The presence of late potentials of the ventricles is judged when at least two of the three signs are detected. Identification of all three signs improves the predictive value of the method. It is believed that the presence of late potentials
ventricular increases the risk of developing life-threatening ventricular arrhythmias in myocardial infarction by 5 -
8 times.
Assessment of heart rate variability. A very important diagnostic tool
is an assessment of the irregularity (variability) of the heart rate, which is understood as
203

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
variability of intersystolic intervals (R-R intervals on the ECG), due to changes in the state of the autonomic nervous system. The technique involves the calculation of the temporal and spectral characteristics of the heart rhythm. Clinical Meaning of Variability Assessment heart rate is that when it decreases ("rigid" rhythm) in patients with structural changes in the heart (especially those who have had MI), the risk of ventricular arrhythmias increases.
Other methods to identify patients at high risk of sudden cardiac death.
In addition to the accepted methods for assessing late ventricular potentials and heart rate variability, to identify the risk of life-threatening ventricular arrhythmias
there are less common ones. These include heart rate turbulence
(physiological two-phase response of SU to ventricular extrasystoles, consisting of short initial acceleration followed by a slowing of the heart rate), T wave alternation
(variation in the morphology (amplitude and shape) of the T wave in successive heartbeats) and QT interval dispersion (difference between the maximum and minimum values of the QT interval). It should be noted that all of the above
techniques for assessing the risk of sudden cardiac death (signal-averaged ECG, heart rate variability, heart rate turbulence, T-wave alternation, dispersion
QT-interval) are used both independently and with Holter monitoring and
implemented in modern Holter systems.
Test with passive orthostasis (tilt test). Tilt test (from the English. Tilt - slope) is used to diagnose syncopal conditions (fainting). This test is based on the determination of hemodynamic reactions due to regulatory (compensatory) mechanisms
with orthostasis. This requires a special turntable, with the help of which the patient, after being in a horizontal position, is transferred to a semi-vertical position. So
thus, neurocardial syncope is provoked, which can be cardioinhibitory (with severe bradycardia and / or asystole), vasodepressor (with severe
decrease in blood pressure) or mixed.
Transesophageal electrocardiostimulation. Close anatomical location
heart (atria) and esophagus allows the use of an electrode inserted through the nose into esophagus, both for registration of a transesophageal ECG, and for carrying out a transesophageal pacing (ECS), usually atrial, for diagnostic and/or therapeutic purposes. Transesophageal pacemaker is used to assess the function of the SU and the state of AV conduction, identify anomalies of the conduction system of the heart and clarify their EF characteristics, and differential diagnosis of paroxysmal supraventricular tachycardias. Except
In addition, transesophageal pacemaker is used to stop spontaneously developed paroxysms of tachycardia and atrial flutter with regular AV conduction. Recently transesophageal pacemaker is rarely used to diagnose disorders of the SU function, since Holter monitoring is a more informative technique for this.
An endocardial EF study is an invasive procedure used when
when diagnostic problems cannot be solved by non-invasive methods. It provides for the installation of multi-contact catheter electrodes in various
sections of the heart. The diagnostic possibilities of endocardial EP study are significantly higher than those of transesophageal pacemaker. Standard electrode placement for EF
study the following: the upper sections of the right atrium, the septal part of the ring three
cuspid valve (the area of registration of the electrogram of the bundle of His) and the right ventricle. If it is necessary to assess the nature of the conduction of excitation in the left parts of the
heart, an electrode is additionally placed in the coronary sinus. In some cases, it may stimulate the left ventricle.
204

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
The objectives of the EF study are: to characterize the EF features of the conductive
systems of the heart, induction of arrhythmias and verification of their mechanisms, evaluation of effectiveness
treatment (medical or interventional).
Medical tests. In arrhythmology, a number of drug tests are used,
aimed at evaluating the function of the SU, studying the state of the conduction system of the heart, and revealing the sensitivity of a number of cardiac arrhythmias to certain drug effects.
Tests with intravenous administration are used to diagnose SU function disorders. atropine or atropine with propranolol (medical denervation of SU), as well as with adenosine or adenosine triphosphate (ATP). Medical denervation of SU is part of
transesophageal pacemaker or endocardial EF study performed for diagnosis dysfunction of the SU.
For provocation of supraventricular and ventricular tachyarrhythmias during EF study use atropine and isoproterenol. Samples with nitroglycerin and isoproterenol are used during tilt tests.
Samples with adenine nucleotides (adenosine, ATP) have found wide application: for differential diagnosis of normal and altered SU function, differential
diagnosis of various supraventricular tachyarrhythmias, visualization of abnormal pathways of excitation, evaluation of the effectiveness of catheter ablation in WPW syndrome.
Drug tests with AARP (aymalin, procainamide) are currently being carried out
rarely, mainly for the manifestation of ECG manifestations in latent Brugada syndrome (see. below).
1.12.3. Supraventricular arrhythmias
Supraventricular (supraventricular) arrhythmias include rhythm disturbances
hearts, the source of which is located in the SU, atria, AV node or trunk of the bundle of His, pulmonary or hollow veins. Supraventricular tachyarrhythmias are also associated with functioning of the abnormal atrioventricular pathways.
Supraventricular extrasystole
The source of supraventricular extrasystole may be the atria flowing into them
pulmonary and vena cava, AV node and trunk of the bundle of His. Extrasystole can be monotopic (from one source) or polytopic (from different sources), single and paired (two extrasystoles in
a row). Three extrasystoles in a row or more are called supraventricular tachycardia, although the term “group extrasystole” has not completely lost its relevance.
The causes of supraventricular extrasystole may be pathological automatism, trigger activity and re-entry of the excitation wave. The most common are atrial extrasystoles (Fig. 1.19).
Their main distinguishing features are prematureness, a different configuration of the ECG P-wave in comparison with the sinus one, an incomplete compensatory pause (interval from the sinus P-wave before the extrasystole to the sinus P-wave following the extrasystole, less than two sinus P-P intervals preceding the extrasystole). The QRS complex in atrial extrasystole is narrow, but can be wide if the conduction of excitation along the bundle branch of His is disturbed (aberrant atrial extrasystole). Except
In addition, the expected QRS complex may not occur behind an extrasystolic P-wave when blockade of excitation through the AV node (blocked atrial extrasystole).
205
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Supraventricular extrasystole has no independent clinical significance and does not require treatment, except when it is a trigger for supraventricular tachyarrhythmias (atrial and AV tachycardias, atrial flutter or AF).
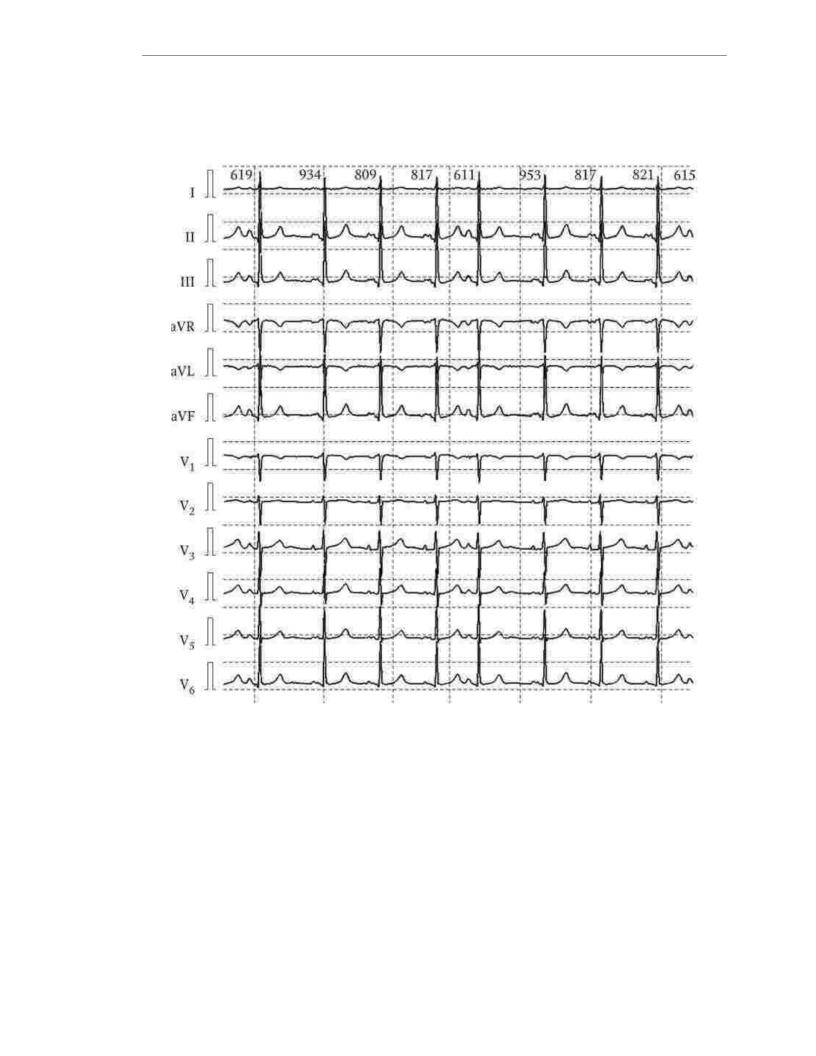
Rice. 1.19. Atrial extrasystole
Supraventricular tachycardia
Supraventricular tachycardias are most often paroxysmal, but can be continuously recurrent and even chronic. According to the source of occurrence, supraventricular tachycardia can be sinus, sinoatrial, atrial, AV-nodal, and also due to the presence of extranodal abnormal pathways of excitation. This section will discuss the most important of them from a clinical point of view. The main complaint
of patients with supraventricular tachycardia is palpitations. With paroxysmal tachycardia, palpitations begin, as a rule, suddenly and end just as suddenly, giving way to SR. Their duration can vary from a few seconds to several days. With a high heart rate (200 per 1 min or more), the heartbeat is
206
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
It may be accompanied by a significant decrease in blood pressure, partial or even complete
loss of consciousness. In patients with coronary artery disease, paroxysmal tachycardia can cause acute coronary insufficiency or even acute myocardial infarction. In rare cases, patients with
structural changes in the heart against the background of paroxysmal tachycardia may develop acute left ventricular failure.
A feature common to all supraventricular tachycardias is the presence of a narrow, the same as with SR, the QRS complex. The exception is the functional (tachy-dependent) blockade of the bundle branch of His, in which the QRS complex becomes wide, as well as called antidromic tachycardia in patients with WPW syndrome, in which arousal anterograde (from the atria to the ventricles) spreads along the bundle of Kent.
Atrial tachycardia
Most of the atrial tachycardias are focal (automatic and trig gerny) tachycardia (Fig. 1.20).
There may be several focal points. Most common short episodes (“jogs”)
atrial tachycardia with a relatively low heart rate, detected using Holter monitoring, which do not pose a real threat to the patient and do not reduce
significant quality of life. Much less common are prolonged, clinically
significant paroxysms of atrial tachycardia. Very rarely, atrial tachycardia takes on a continuously relapsing or chronic character.
AV conduction in focal atrial tachycardias may be 1:1, 2:1, or irregular. Ectopic P waves are usually (but not necessarily) positive on the ECG in leads II, III, and aVF.
Asymptomatic atrial tachycardia usually does not require treatment. Sometimes treatment is limited to control (normalization) of heart rate, for which ÿ- blockers are used, less often - calcium antagonists (verapamil, diltiazem), even more rarely (with continuously recurrent or chronic atrial tachycardia) - cardiac glycosides (digoxin). For
recovery of CP and prevention of seizures in paroxysmal atrial tachycardia, antiarrhythmics of classes I and III are used. Radical treatment, especially for monofocal tachycardias, is possible with the help of interventional treatment - high-frequency
catheter destruction (ICD) of the arrhythmogenic zone.
Atrial tachycardia may also be based on the mechanism of re-entry of the wave excitation (reentry). Since stable reentry implies either a sufficient length
loops of excitation circulation, or the presence of zones of delayed conduction, then reentry atrial tachycardia occurs either in people of the older age group (with developed conduction anisotropy), or in patients after interventional treatment around postoperative scar areas. Such tachycardias can in some cases be induced and stopped during a transesophageal pacemaker or endocardial EP study.
Antiarrhythmic therapy for reentry atrial tachycardia is possible and does not differ fundamentally from the treatment of focal tachycardias, but the method of choice is still IVKD.
Paroxysmal reciprocal atrioventricular tachycardias
The anatomical substrate of paroxysmal reciprocal AV tachycardia is
extranodal anomalous path of excitation conduction: Kent'sbundle connecting the atria directly with the contractile myocardium of the ventricles and capable of making two links of the excitation re-entry chain (reentry) with the AV connection. Kent'sbundle is an additional muscle bridge and, in comparison with the AV junction, the area
207
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
gives a greater speed of excitation. It is these properties that determine ECG features. Since excitation spreads from the atria to the ventricles
quickly along the Kent beam, then the P – Q-interval is short. Due to the fact that from the place of confluence
Kent beam into the right or left (depending on the location of the anomalous conductive path) ventricle, excitation further spreads along the contractile myocardium of the ventricles, the QRS complex is wide due to the so-called delta wave, and the
repolarization is changed (Fig. 1.21). This is called pre-excitation (pre-excitation). Delta wave the mo (and, accordingly, the wider the QRS complex), the farther the place of entry of the
Kent'sbundle is from the specialized conducting system.
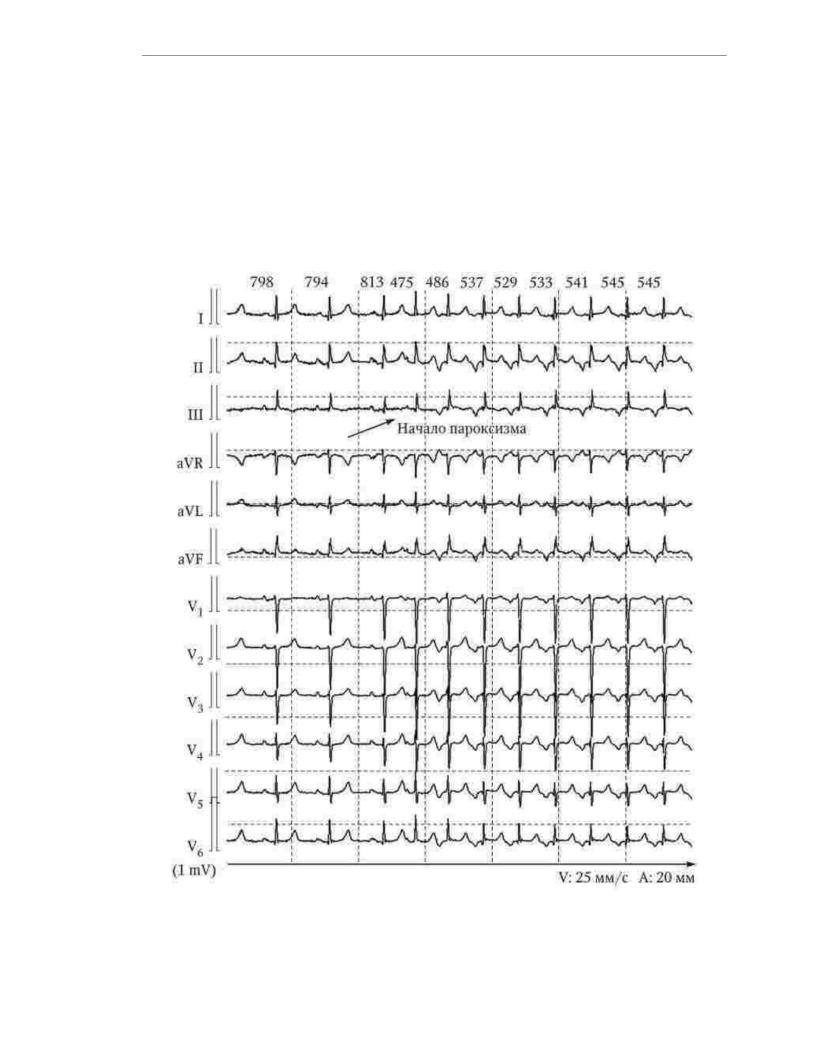
Rice. 1.20. Paroxysm of atrial tachycardia
208
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
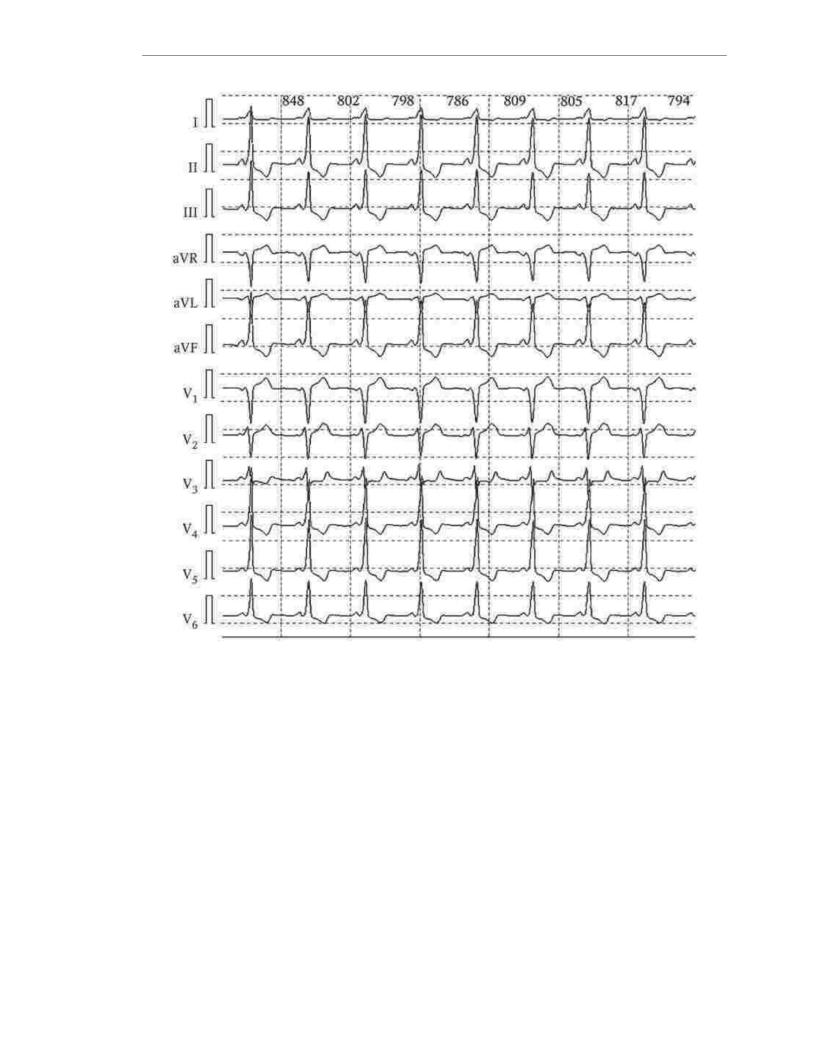
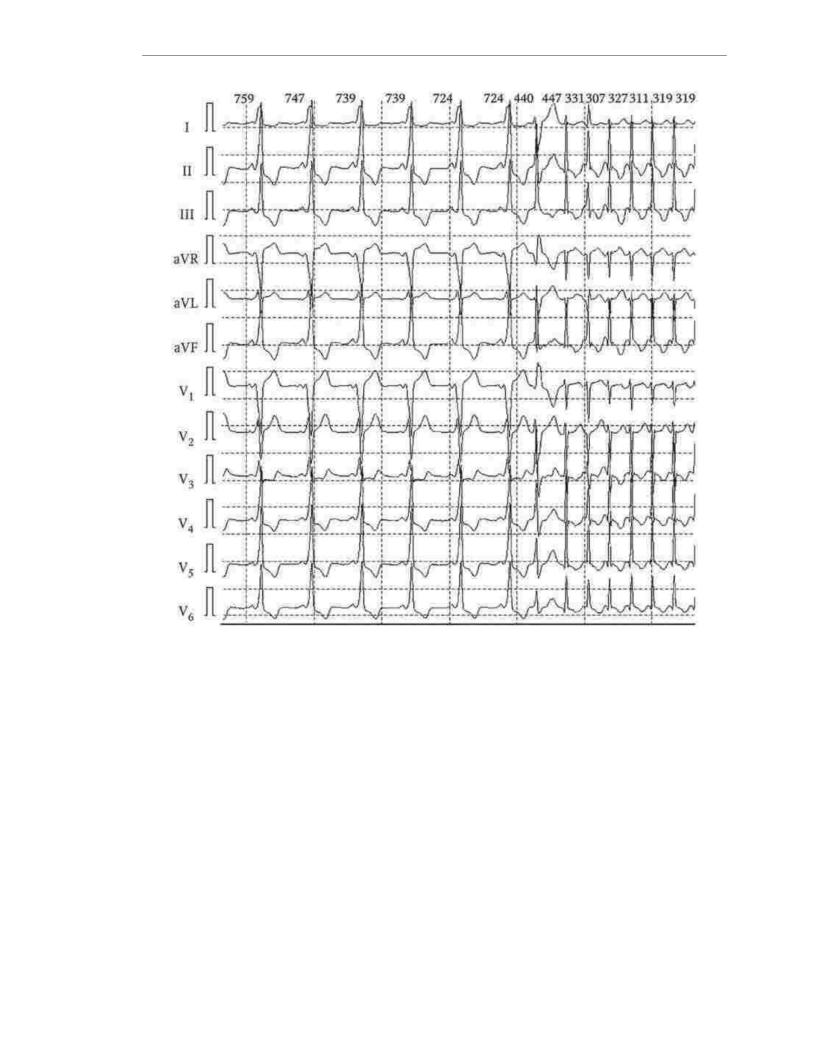
Rice. 1.21. Manifesting WPW (Wolf-Parkinson-White) syndrome
Most (but not all) patients with abnormal pathways have
paroxysmal supraventricular tachyarrhythmias. If they are present, it is customary to speak of the WPW syndrome, and in the absence of them, the WPW phenomenon. The
most common WPW syndrome is orthodromic reciprocal AV tachycardia, in which excitation is antero atria to the ventricles) spreads along the AV junction, and retrograde (from the ventricles
to the atria) - along the Kent bundle (Fig. 1.22). Much less likely to encounter antidromic tachycardia, in which excitation spreads anterogradely along the bundle Kent, and retrograde - through a specialized conduction system, the AV junction. Approximately 10% of patients have paroxysmal AF. With orthodromic paroxysmal reciprocal AV tachycardia QRS complexes are narrow, as excitation spreads along His-Purkinje system. With antidromic, the QRS complexes are wide, since from the end of the Kent bundle in the ventricles, excitation propagates asynchronously, along the contractile myocardium.
209
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Rice. 1.22. Manifesting syndrome WPW. Paroxysm of reciprocal orthodromic
AV tachycardia
Syndrome (phenomenon) WPW can be manifesting, intermittent, latent and hidden. With the manifesting WPW syndrome, signs of pre-excitation (shortening of the P-Q interval, the presence of a delta wave, the expansion of the QRS complex and changes
repolarization processes) are observed on all ECGs of the patient. Intermittent Syndrome
WPW involves alternating conduction from the atria to the ventricles with and without involvement of the abnormal conduction pathway. Therefore, signs of conduction along an additional pathway of excitation are clearly visible on some ECGs and absent on others. A similar picture is also possible within the registration of one ECG.
In latent WPW syndrome at rest and in normal activities, the AV junction conduction velocity always prevails over the abnormal conduction pathway, and therefore there are no signs of preexcitation. However,
against the background of EKS or pronounced loads, in the event of supraventricular tachyarrhythmias, and also, with the introduction of certain drugs (for example, ATP), the ratio of conduction velocities
along the AV junction and the Kent bundle changes and characteristic signs of the WPW syndrome appear.
210
