
1-280 pdf (1)
.pdf
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
fixed and dynamic coronary obstruction are combined. At different stages of the disease, one or another mechanism of coronary insufficiency may predominate, which determines the individual characteristics of its clinical manifestations.
Relatively rare, mainly in women after menopause, is diagnosed
a clinical variant of angina pectoris, which is combined with unchanged (according to coronary angiography) main coronary arteries and the absence of signs of vasospasm. It is assumed that it is based on atherosclerotic lesions and impaired endotheliumdependent vasodilation of small myocardial arterioles. As additional pathogenetic mechanisms, estrogen deficiency, a decrease in the threshold of pain sensitivity, an increase in the stiffness of the vascular wall, and metabolic disorders are discussed. myocardium. This clinical variant is called "syndrome X" or microvascular angina.
The discrepancy between myocardial oxygen demand and its delivery leads to metabolic disorder of cardiomyocytes. During ischemia, the synthesis of macroergic
compounds is disrupted in myocardial cells. Due to the activation of glycolysis in cardiomyocytes, ca
unoxidized fatty acids are poured out, the lactate content increases and
intracellular acidosis. There is an overload of cells with calcium ions, the formation of free radicals is enhanced, enzyme systems are activated. As a result, damage to the structure of cell membranes occurs, and transmembrane ion currents are disrupted. A change in cellular metabolism leads to a violation first of the diastolic, and then and systolic myocardial function. In ischemia zones, local transient
contractility disorders and changes in the electrophysiological properties of the myocardium,
which is manifested by heart failure, rhythm and conduction disturbances.
Acute ischemia leads to myocardial damage that persists after reperfusion and is characterized by reversible local dysfunction lasting from several hours to several days. This phenomenon is called "stunned myocardium".
The severity and duration of functional disorders of the heart muscle in the postischemic period are determined by the duration of acute ischemia. With a chronic decrease in coronary blood flow, a reversible adaptive decrease in metabolism develops. and functional activity of cardiomyocytes, allowing to maintain the viability
heart muscle in the ischemic zone. Local myocardial dysfunction disappears completely or significantly decreases after the restoration of coronary blood flow and / or a decrease in myocardial oxygen demand. This adaptive reaction is designated by the term "hibernating myocardium". Recurrent brief episodes of ischemia may
cause the formation of the phenomenon of increased myocardial tolerance to ischemic damage - the so-called "preconditioning". Adaptive changes
metabolism of cardiomyocytes hinder the development of morphological and functional disorders of the heart muscle, however, the possibilities of this adaptive mechanism have certain time limits.
The sequence of events that manifest myocardial ischemia is called the ischemic cascade. The main sequentially developing stages of the ischemic cascade are: hypoperfusion, metabolic disorders, changes in diastolic function, regional myocardial dyssynergy, typical ECG changes, global
left ventricular dysfunction, pain. Pathophysiological concept of the ischemic cascade serves as a theoretical basis for diagnosing myocardial ischemia in patients complaining of pain in the chest.
Morphology. Angina pectoris is not accompanied by the formation of foci of
necrosis in the heart muscle. However, episodes of acute ischemia and permanent hypoperfusion lea the formation of areas of chronically stunned and hibernating myocardium, stimulate
61

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
apoptosis is the process of natural death of cardiomyocytes and promotes the growth of connective tissue, as a result of which cardiosclerosis fields are formed in the heart muscle. At stable angina pectoris, as a rule, mature atherosclerotic plaques are found in the coronary arteries, causing hemodynamically significant stenosis of the affected vessel.
For this form of coronary artery disease, the presence of fresh damage to the atherosclerotic plaques with the formation of subintimal hemorrhages, parietal and occlusive thrombi is uncharacteristic. Unstable angina usually develops as a result of injury
immature (vulnerable) atherosclerotic plaque. Violation of the integrity of its fibrous capsule can cause the formation of an unstable platelet aggregate, a red thrombus, not
completely blocking the lumen of the vessel, or hemorrhage into the plaque with a rapid increase in its size and the formation of a hemodynamically significant stenosis, as well as provoke a spasm of the coronary artery.
Classification. According to the nature of the course, angina pectoris is divided into stable and unstable, according to the dynamics of the frequency of seizures - into progressive and non-progressive, according to the connection of seizures with physical and / or emotional stress - for angina pectoris
niya and rest angina.
Stable exertional angina is the most common clinical form.
ischemic heart disease. The course of angina pectoris is regarded as stable, provided that the frequency, duration, level of load at which anginal pain occurs, and the effectiveness of relief of attacks have remained unchanged over the past 2 months. (at least,
at least 4 weeks). The functional class of stable angina is determined by the ability
the patient to perform household physical activity in accordance with the classification of the Canadian Heart Association (Table 1.18).
Table 1.18
Classification of stable exertional angina
Unstable angina is a syndrome caused by an exacerbation of coronary artery disease, which characterized by a high risk of MI and sudden death. According to working
Classification of coronary artery disease distinguishes the following clinical variants of unstable angina: first-time angina pectoris (stress or rest, progressive or non-progressive
62
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
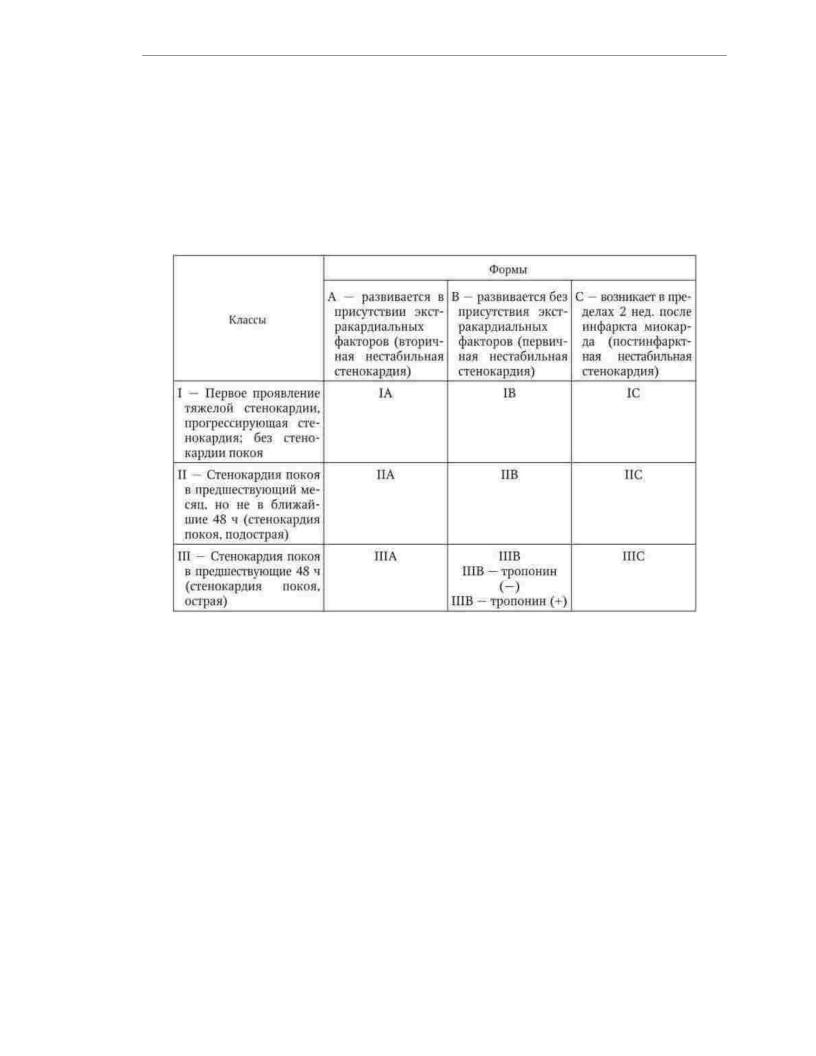
rubbing) during the previous 4 weeks; progressive angina after a period of stable flow; early postinfarction or postoperative angina pectoris. C. W. Hamm
and E. Braunwald in 2000 proposed a classification of unstable angina, in which
the nature and change in the incidence of anginal pain, their relationship with physical
activity and extracardiac factors that increase myocardial ischemia are taken into account (Table 1). 1.19).
Table 1.19
Classification of unstable angina
Spontaneous angina pectoris is a clinical variant of angina pectoris, which is characterized by the occurrence of attacks of anginal pain at rest, lasting 10 minutes or more, resistant to nitroglycerin. Variant angina pectoris (Prince metal angina pectoris) is manifested by spontaneous attacks, which are often accompanied by autonomic
symptoms (hyperemia of the skin, sweating, tachycardia, tremor), disorders
heart rate, mental reactions (anxiety, fear of death), motor excitation. ECG changes are expressed in ST segment elevation and are transient.
This type of angina pectoris is based on spasm of the coronary artery.
Painless myocardial ischemia is a form of coronary artery disease that manifests itself by electrocardiographic signs of ischemia without typical anginal pain. The absence of pain in the presence of ischemic ECG changes is associated with an increase in the
threshold of pain sensitivity. Painless myocardial ischemia is detected by Holter monitoring and tests with physical activity. Microvascular angina ("syndrome X") is characterized by the
occurrence of typical anginal attacks in the absence of angiographic signs of narrowing of the epicardial coronary arteries, clinical and angiographic evidence of coronary artery spasm, hypertrophy and systolic dysfunction of the left
ventricle.
63

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
clinical picture. According to the Framingham study, coronary artery disease debuts clinical symptoms of angina pectoris in 40% of men and 56% of women. For the first time, the clinical picture of angina pectoris was described in 1772 by W. Heberden, who called
this syndrome is "angina pectoris". For typical (defined) angina
characterized by compressive pain, a feeling of pressure or heaviness behind the sternum with irradiation in left arm, area of the left collarbone and left shoulder blade, left half of the neck and lower jaw.
In some cases, the pain radiates to the epigastric region, the right half of the chest
cells and right hand. In a number of patients, anginal pain is accompanied by shortness of breath, weakness,
dizziness, heart rhythm disturbances. With angina pectoris, pain is provoked by physical, emotional stress, exposure to cold, increased blood pressure, and abundant food intake. The pain disappears or significantly decreases at rest or after 1-3 minutes
after taking nitroglycerin. The duration of the attack is usually 5-10 minutes and does not exceed 15 min.
Destabilization of the course of coronary artery disease is most often manifested by an
increase in the frequency, intensity and duration of anginal attacks, a decrease in the level of stress that causes pain, weakening the stopping effect of nitroglycerin. Diagnosis of unstable angina
lawful if from the moment of the first attack of anginal pain or the onset
progression of angina pectoris has passed no more than 4 weeks. diagnostic criteria for early post-infarction or postoperative angina is considered the appearance of anginal pain
in the first 2 weeks. after the development of MI or myocardial revascularization surgery. One of the options for unstable angina is intermediate coronary
syndrome. This term is used to refer to the clinical form of acute coronary insufficiency, which occupies an intermediate position between angina pectoris and MI.
Intermediate coronary syndrome is manifested by an attack of anginal pain lasting 20–30 minutes, which is often accompanied by heart rhythm disturbances, a decrease or
increased blood pressure and ECG changes in the form of T wave inversion, depression or ST segment elevation. In contrast to MI, ECG changes in intermediate coronary syndrome are reversible - the ECG shape returns to its original shape within the next day. It is not uncommon for patients with intermediate coronary syndrome to have elevated levels of myoglobin.
and creatine phosphokinase in the blood, which, however, should not exceed the upper limit of normal values by more than 50%.
Painless myocardial ischemia is a fairly common occurrence. According to the Framingham Study, up to 25% of MIs are first diagnosed only on retrospective ECG analysis, and half of these cases are asymptomatic. In patients with stable angina pectoris, two types of this form of coronary artery disease are distinguished: type 1 - painless ischemia, detected
with Holter monitoring or stress tests in the absence of angina attacks,
Type 2 - painless ischemia in combination with typical angina attacks. Besides,
painless ischemia can be registered in patients with unstable angina pectoris as a component of various clinical variants of this syndrome. Painless myocardial ischemia
Type 1 is registered in 18% of patients with angiographic signs of atherosclerosis coronary arteries. Painless myocardial ischemia type 2 is much more common. At
In patients with typical angina pectoris, about half of the episodes of myocardial ischemia are not accompanied by pain. With the highest frequency of painless myocardial ischemia
occurs in diabetic patients. In the absence of pain, myocardial ischemia can manifest itself with other symptoms - shortness of breath, weakness, dizziness, rhythm disturbances.
hearts which quite often manage to be found out at careful questioning of the patient.
Pain is the final stage of the ischemic cascade. The damaging effect of ischemia on the myocardium is determined not by the intensity of the pain syndrome, but by the severity and duration of deterioration in cardiac muscle perfusion. Decreased pain sensitivity
64

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
It prevents early recognition of myocardial ischemia and makes it difficult to take measures,
aimed at preventing its negative consequences. With the same damage to the coronary arteries in patients with painless myocardial ischemia of the 1st type, detected during
exercise tests, the risk of developing myocardial infarction and sudden death is several times higher, than in patients with typical angina attacks. Painless myocardial ischemia is regarded as a
predictor of an unfavorable outcome of coronary artery disease.
Physical examination of patients with angina may reveal clinical signs of atherosclerosis: xanthomas, xanthelasma, corneal lipoid arch. Some patients have symptoms of stenotic lesions of the main arteries:
intermittent claudication and weakening of the pulsation in the arteries of the feet, systolic murmur in
carotid arteries. In conditions of physical activity, immediately after its completion, and sometimes even during at rest, a III tone and a systolic murmur at the apex of the heart can be heard, arising
due to mitral regurgitation due to ischemic papillary dysfunction
ny muscles.
Laboratory and instrumental diagnostics. If angina pectoris is suspected it is recommended to perform a series of laboratory studies to identify factors the risk of cardiovascular disease and conditions that can provoke ischemia
myocardium: determination of the content of hemoglobin in the blood, total cholesterol, LDL cholesterol, HDL cholesterol,
TG, glucose. In patients with intense pain attacks, the duration of which
exceeds 20 minutes, markers of myocardial damage should be determined (MB-fraction of creat inphosphokinase, troponins T and I).
Instrumental methods for examining patients with suspected angina pectoris are divided into non-invasive and invasive. Non-invasive methods of instrumental diagnostics include electrocardiography, ECG Holter monitoring, exercise
electrocardiographic tests, ischemic test, provocative pharmacological
samples, echocardiography, perfusion scintigraphy and positron emission tomography of the myocardium, electron beam tomography and multilayer spiral computed
tomography of the coronary arteries. The main invasive method for the study of patients with coronary artery disease
is selective coronary angiography.
Electrocardiography is a mandatory method for examining patients with suspected angina. Outside of a pain attack in 70% of patients, ECG changes are absent or have non-specific character. With the same frequency, typical signs of myocardial ischemia are detected on the ECG recorded during a pain attack. to typical ischemic
ECG changes include shifting the ST segment down (depression) or up (elevation) from the isoelectric line, T-wave inversion. ST-segment elevation during anginal
attack is a specific sign of variant angina (Prince metal angina). After relief of pain, the form of the ECG returns to the original. In patients with intermediate coronary syndrome, ECG changes that occurred during an attack also
are transient, but can persist for a longer time - up to a day. Holter ECG monitoring provides valuable diagnostic
information, since ECG registration during an attack is not always possible. Besides, this method allows fixing painless myocardial ischemia, transient arrhythmias and
conduction disturbances. Comparative evaluation of the results of ECG Holter monitoring during treatment allows us to evaluate the effectiveness and safety of the drug.
therapy.
Stress testing is a method for examining patients with suspected angina pectoris, which allows you to confirm or reject this diagnosis, clarify the pathogenesis and evaluate the severity of coronary insufficiency, to identify painless myocardial ischemia, to determine the functional status of the patient and prognosis. Carrying out stress tests is shown
65

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
all patients with angina pectoris who do not have contraindications based on the results of clinical studies and electrocardiography at rest. To perform stress tests, a bicycle ergometer or treadmill is used. sensitivity and specificity of ECG changes during
physical activity for the diagnosis of coronary heart disease are respectively 70 and 90%.
An ischemic test and provocative pharmacological tests are performed in the presence of contraindications to conduct or due to the impossibility of performing tests with physical activity. When performing an ischemic test, an increase in heart rate (and, therefore,
myocardial oxygen demand) is provided by transesophageal pacing (ECS). The test is considered positive when ischemic ECG changes occur.
and / or the development of an anginal attack. Dipyridamole and ergometrine are most commonly used for pharmacological testing. Intravenous administration of dipyridamole (a drug that causes vasodilation) can provoke an angina attack in patients with significant
obstructive lesion of the coronary arteries due to the development of the “steal syndrome”. A test with intravenous administration of ergometrine is used in some cases for
diagnosis of vasospastic angina in patients with spontaneous chest pain
cell if other studies have not confirmed the presence of myocardial ischemia and angiography did not reveal significant narrowing of the coronary arteries.
All provocative tests can cause a sharp deterioration in the patient'scondition,
therefore, they are carried out according to strict indications by specially trained personnel in
conditions, allowing, if necessary, to provide emergency care to the patient.
Resting echocardiography can detect and quantify myocardial dysfunction and detect nonatherosclerotic causes of angina pectoris, such as aortic stenosis,
left ventricular hypertrophy, hypertrophic cardiomyopathy. Stress echocardiography, i.e., a study performed using physical activity, transesophageal
pacing and pharmacological preparations (dipyridamole, dobutamine), allows to detect local changes in myocardial contractility caused by ischemia, which often precede the appearance of its clinical and electrocardiographic signs
cov.
Myocardial perfusion scintigraphy is a method that allows, by assessing the uniformity of the distribution of the radiopharmaceutical, to identify areas of cardiac hypoperfusion.
muscles. The diagnostic value of the results of the study increases when it is combined with physical activity - by changing the size of the area of the heart muscle with a reduced concentration of the radiopharmaceutical at rest and during exercise, ischemia can be differentiated
and scarring damage to the myocardium. Positron emission tomography makes it possible to evaluate not only perfusion, but also myocardial metabolism. The advantage of this research method is the ability to assess the viability of the myocardium, which is very important for determining indications for revascularization.
Electron beam tomography of the coronary arteries is used to quantify coronary artery calcification. The values of the so-called "calcium
index" are consistent with the degree of atherosclerotic lesions of the coronary arteries.
However, this method does not allow assessing the degree of narrowing of the lumen of the coronary artery. and identify non-calcified atherosclerotic plaques most prone to rupture and thrombosis. Multilayer
spiral computed tomography provides the possibility of retrospective image reconstruction at any given phase of the cardiac
cycle, which allows you to determine the degree of calcification and stenosis of the coronary arteries, to evaluate
patency of autovenous shunts and stents.
Non-invasive diagnostic studies are carried out not only to verify the diagnosis of angina pectoris, but also to assess the individual risk of adverse outcomes. Determination of the degree of risk is necessary for the choice of treatment tactics. Group patients
66
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
high risk (mortality more than 3% per year), coronary angiography is recommended to assess the feasibility and choice of the method of myocardial revascularization.
High-risk signs include: 1) severe
left ventricular dysfunction (ejection fraction < 35% at rest and/or during exercise);
2)low exercise tolerance (ST segment depression occurs at a heart rate of 7120 per minute, persists for 6 minutes or more after the cessation of exercise, is
accompanied by a decrease in blood pressure by 10 mm Hg or more and / or ventricular arrhythmias
3)large or multiple perfusion defects in myocardial scintigraphy during exercise,
absorption of the indicator by lung tissue, post-exercise dilatation of the left ventricle
daughter; 4) impaired contractility of more than two segments of the left ventricular wall during stress echocardiography after administration of dobutamine at low doses (710 ÿg/ kg/min) or with heart rate < 120 per minute.
Selective coronary angiography is the "gold standard" in identifying and assessing the prevalence and severity of atherosclerotic lesions of the coronary arteries.
Indications for coronary angiography in stable angina pectoris are: 1) severe angina pectoris III-IV functional class, which persists with optimal
Noah antianginal therapy;
2) signs of severe myocardial ischemia based on the results of non-invasive methods; 3) the patient has a history of episodes of sudden death or dangerous
ventricular arrhythmias; 4) progression of the disease according to the dynamics of non-invasive tests; 5) early development of severe angina (III functional class) after a heart attack
myocardium and myocardial revascularization (up to 1 month);
6) questionable results of invasive tests in persons with socially significant occupations. siay (drivers of public transport, pilots, etc.). Indications
for coronary angiography in unstable angina are: 1) the presence of signs of a poor prognosis, ineffectiveness of therapy; 2) severe left ventricular dysfunction (ejection fraction < 35%); 3) the presence of life-threatening ventricular arrhythmias; 4) operation (procedure) of myocardial revascularization in history. Diagnosis. The tactics of examining a patient
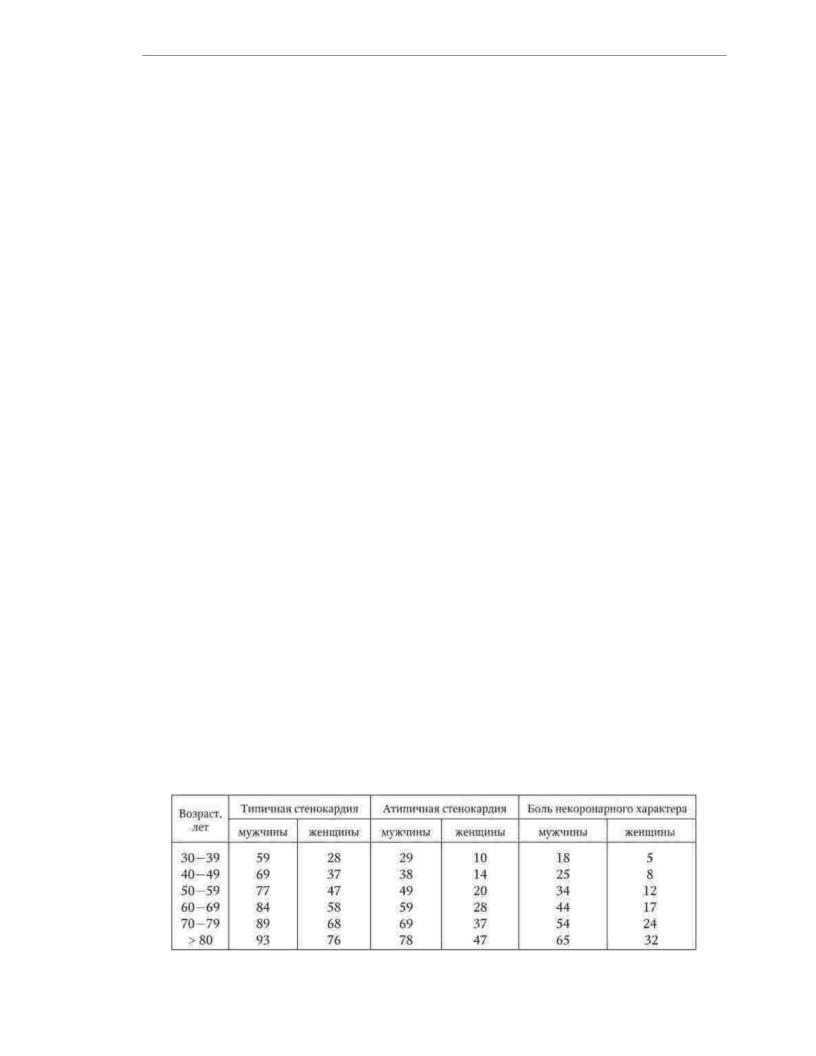
with chronic coronary artery disease is determined by the clinical features and severity of angina pectoris, the age of the patient and the nature of the comorbidity (Table 1.20).
Table 1.20
Prior probability of diagnosis of chronic coronary artery disease depending on the nature tera of chest pain, %
67

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
If, according to the results of primary studies, the a priori probability of chronic coronary artery disease exceeds 85%, additional studies to clarify the diagnosis can be omitted,
and immediately begin to assess the risk of complications, the choice and implementation of treatment. In cases where
based on the results of primary studies, the a priori probability of chronic CAD does not exceed 15%, non-ischemic heart disease or non-cardiac causes of symptoms
should be suspected. Patients with an a priori probability of coronary artery disease of 15–85% are i additional non-invasive imaging studies, and if indicated -
coronary angiography.
In the diagnosis, it is necessary to indicate the form of chronic coronary artery
disease, in patients with stable angina - functional class, in patients with unstable angina - clinical variant and date of destabilization, and in case of achieving a stable state, the date of
stabilization and the functional class of stable angina pectoris after the exacerbation of coronary artery dis
Examples of diagnoses:
1.IHD, angina pectoris III f. to.
2.IHD, spontaneous angina.
3.IHD, unstable angina (first-time progressive angina pectoris from 10.11.09).
4.IHD, unstable angina (progressive angina
tension from 10.11.09, intermediate coronary syndrome 15.11.09), stabilization from 22.11.09, angina pectoris II f. to.
differential diagnosis. Chest pain is a fairly common symptom
which is characteristic of many diseases. The differential diagnosis should be made with MI, myocarditis, pericarditis, dissecting aortic aneurysm, hypertrophic cardiomyopathy, and other diseases of the cardiovascular system. The cause of pain
in the chest can be diseases of the lungs and pleura (thromboembolism of the branches pulmonary artery, pneumothorax, pleurisy, pneumonia, primary pulmonary hypertension), pathology of muscles, ribs and nerves (myositis, costochondritis,
cervicothoracic sciatica, traumatic injuries, herpes zoster), diseases of the esophagus (esophagitis, esophagus), diseases of the gastrointestinal tract (gastric ulcer, intestinal
colic, cholecystitis, pancreatitis). Angina must also be differentiated from conditions caused by mental disorders (hyperventilation, panic attack,
primary anxiety, depression, etc.).
The diagnostic algorithm in most cases includes questioning, physical research, ECG at rest and the use of stress tests. If severe myocardial ischemia or other indications are detected, coronary angiography is performed. In some cases (for example, in patients with typical clinical and electrocardiographic signs of severe myocardial ischemia at rest, unstable angina pectoris, anginal
seizures that resumed after myocardial revascularization) coronary angiography
performed immediately after questioning, physical examination, and resting ECG recording. In doubtful cases, laboratory and instrumental research methods are used to test competing diagnostic hypotheses.
Flow. Angina flows in waves: periods of stable flow are replaced
periods of instability. For patients with unstable angina, there are two options for the development of events: stabilization of angina pectoris or the development of MI. Stabilization of angina usually occurs either at the level of the functional class
preceding the exacerbation of coronary artery disease, or at the level of the next functional class. B cessation of the progressive decline in exercise tolerance and the achievement of
constant characteristics of angina attacks (frequency, duration, response
68

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
nitroglycerin) for at least 3 to 5 days. Sometimes as a result of successful treatment after a period of unstable angina, anginal pain disappears for a while
hut at all.
Forecast and outcomes. The mortality rate in patients with stable angina pectoris is 2-3%. in year. Another 2-3% of patients develop non-fatal MI. With destabilization of angina pectoris the risk of developing myocardial infarction and death is greatly increased. The most
unfavorable clinical variants of unstable angina pectoris are early postinfarction and spontaneous angina. The individual prognosis of patients with angina pectoris depends on the
characteristics of coronary artery lesions (prevalence, localization and degree of
stenosis), the functional state of the myocardium, the presence and severity of factors provoking ische myocardium, the nature of therapeutic measures.
Treatment. The main goals of treating patients with angina pectoris include: improving prognosis by preventing the progression of coronary artery disease, the development of acute
coronary syndromes, the prevention of arrhythmias, acute and chronic heart failure; improving the quality of l
reducing the frequency, intensity of anginal attacks and increasing tolerance to
physical load.
Non-drug effects. The most important condition for the successful treatment of a
patient with angina pectoris is the elimination of risk factors: smoking cessation, normalization
body weight and blood pressure, correction of dyslipidemia, compensation of diabetes mellitus. Patients with stable angina shows therapeutic exercises with an individual determination of the
permissible level of physical activity. Physical exercise helps
reduce excess body weight and increase tissue sensitivity to insulin, have a beneficial effect on fat metabolism and blood pressure levels. Nutrition advice
consist in increasing the consumption of vegetables, fruits, fish, limiting the consumption of animal fats and carbohydrates, and reducing alcohol consumption. A low-calorie diet is recommended for obese patients.
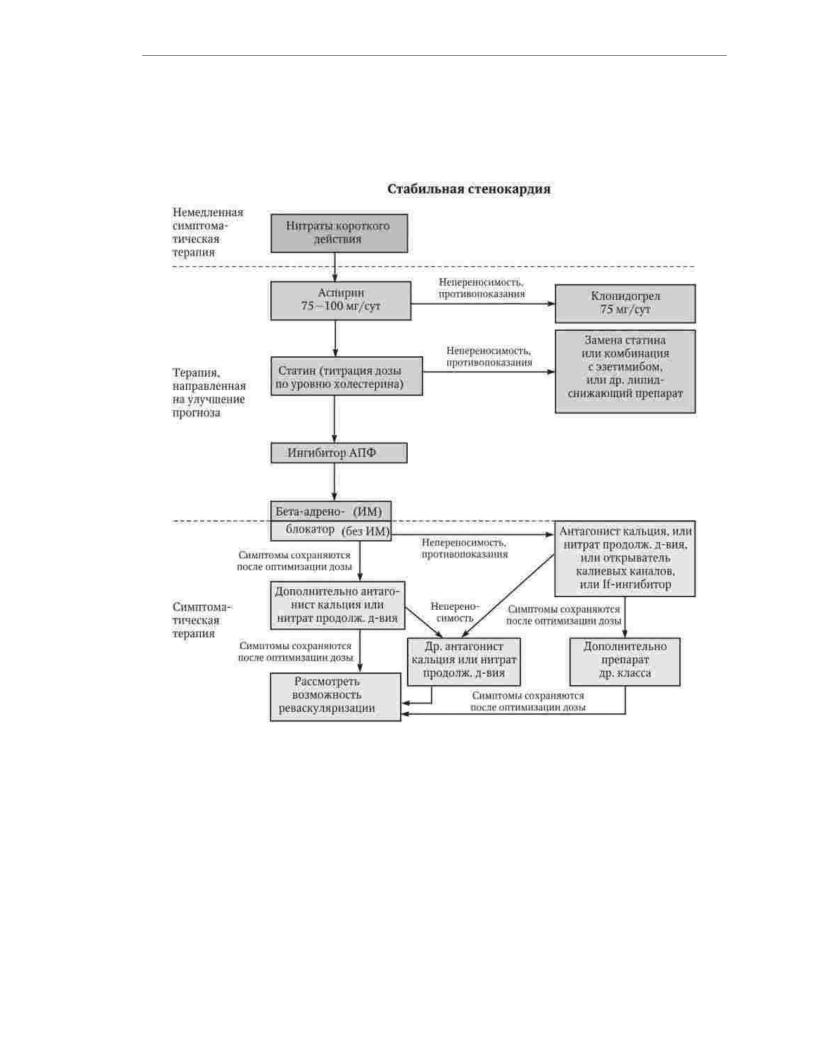
Medical treatment. Medicines recommended for use in
As part of the pharmacotherapy of stable angina pectoris, they are divided into three groups. To the first group include drugs intended for the relief of anginal attacks (nitrates
short-acting), the second group - drugs that improve the prognosis (antiplatelet agents, lipid-lowering drugs, ACE inhibitors, ÿ- blockers), the third group includes drugs used to prevent angina attacks (ÿ- blockers, long-acting calcium antagonists, long-acting nitrates, If-channel inhibitors, potassium channel opener) (Fig. .1.5).
Nitrates have a strong vasodilating effect. Vasodilator
The effect of organic nitrates is due to their conversion into nitric oxide (NO), a structural analogue of the endothelium dependent relaxing factor that activates guanylate cyclase, resulting in the accumulation of cyclic guanosine monophosphate in the smooth muscle cells of the vascular wall, causing relaxation of contractile elements. Except
In addition, nitrates promote the release of prostacyclin, which has vasodilating and antiaggregatory effects. In small doses, nitrates act as venodilators,
with increasing dose, their arteriolodilating effect develops and intensifies. An increase in the capacity of the venous bed and deposition of blood in the vessels of the abdominal
cavity lead to a decrease in the venous return of blood to the heart. As a result, the pressure drops filling, wall tension and stroke volume of the left ventricle, which helps to reduce
myocardial oxygen consumption. Thus, the decrease in preload, which occurs under the influence of nitrates, ensures the restoration of the balance between oxygen consumption by the heart muscle and its reduced delivery through sclerosed coronary arteries.
arteries. Along with peripheral vasodilation, under the influence of nitrates, there are expressions
69
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
female expansion of the epicardial arteries and collaterals, redistribution of the coronary blood flow towards the ischemic areas of the heart muscle, and due to a decrease intraventricular pressure improves blood supply and subendocardial areas
myocardium.
Rice. 1.5. Algorithm for the treatment of stable angina pectoris
Nitroglycerin in the form of tablets, oily solution in gelatin capsules and aerosols is used sublingually for the relief of angina attacks. Duration
effect is 15 - 20 minutes. Long-acting forms of nitroglycerin, intended for oral administration, have a longer antianginal effect - up to 4 hours, but
due to intensive metabolism in the liver, they are characterized by a poorly predictable clinical effect and are currently not recommended for the treatment of patients with
angina pectoris. Cutaneous application of nitroglycerin in the form of an ointment or patch prevent destruction during the first passage through the liver. However, regular use of
transdermal formulations causes rapid development of nitrate tolerance. Isosorbide dinitrate non-prolonged action is used both for cupping (sublingually) and for
Prevention (by mouth) of angina attacks. Multiplicity of reception of prolonged forms
70
