
1-280 pdf (1)
.pdf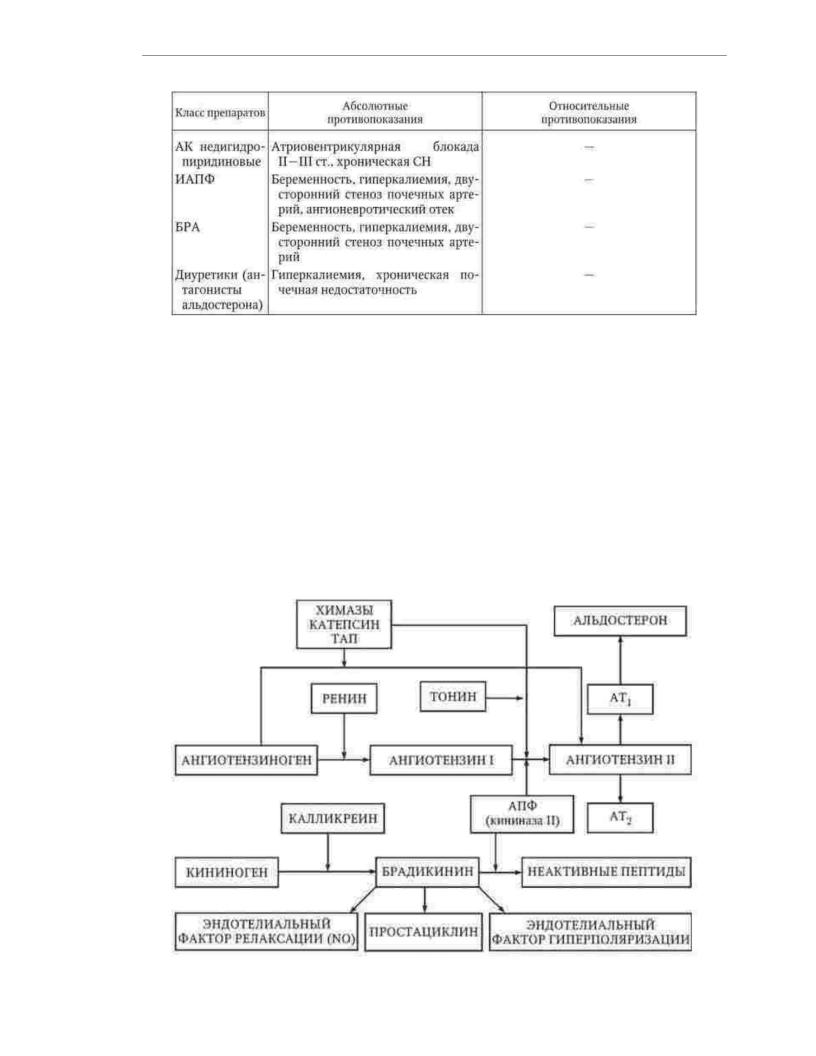
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
ACE inhibitors have the widest range of indications for use in patients
GB. Drugs of this class, reducing the activity of ACE, reduce the formation of angiotensin II in the blood and tissues, and also prevent the degradation of bradykinin (Fig. 1.4).
Angiotensin II, acting on specific type 1 receptors, causes vasoconstriction and promotes damage to target organs, stimulates the secretion of aldosterone, causes sodium and water retention. Under the influence of bradykinin in endothelial cells
increased secretion of nitric oxide, prostacyclin and endothelial hyperpolarization factor, which have vasodilatory, antiproliferative and antiplatelet properties.
Cardiovascular effects of ACE inhibitors include arterial and venous vasodilation, regression of left ventricular hypertrophy and myocardiofibrosis, prevention of left ventricular dilatation, inhibition of smooth muscle cell proliferation
vascular wall. Thus, ACE inhibitors cause a decrease in blood pressure and provide protection of target organs, and not only due to the hypotensive effect.
51
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Rice. 1.4. Scheme of the renin-angiotensin-aldosterone system
This class of drugs is recommended for patients with hypertension associated with left ventricular hypertrophy, microalbuminuria, proteinuria, and impaired renal function. patients with diabetes mellitus, chronic heart failure and paroxysmal atrial fibrillation. Absolute contraindications to the use of ACE inhibitors are pregnancy,
severe hyperkalemia, bilateral stenosis of the renal arteries (or stenosis of the artery of the only functioning kidney), anamnestic information about angioedema,
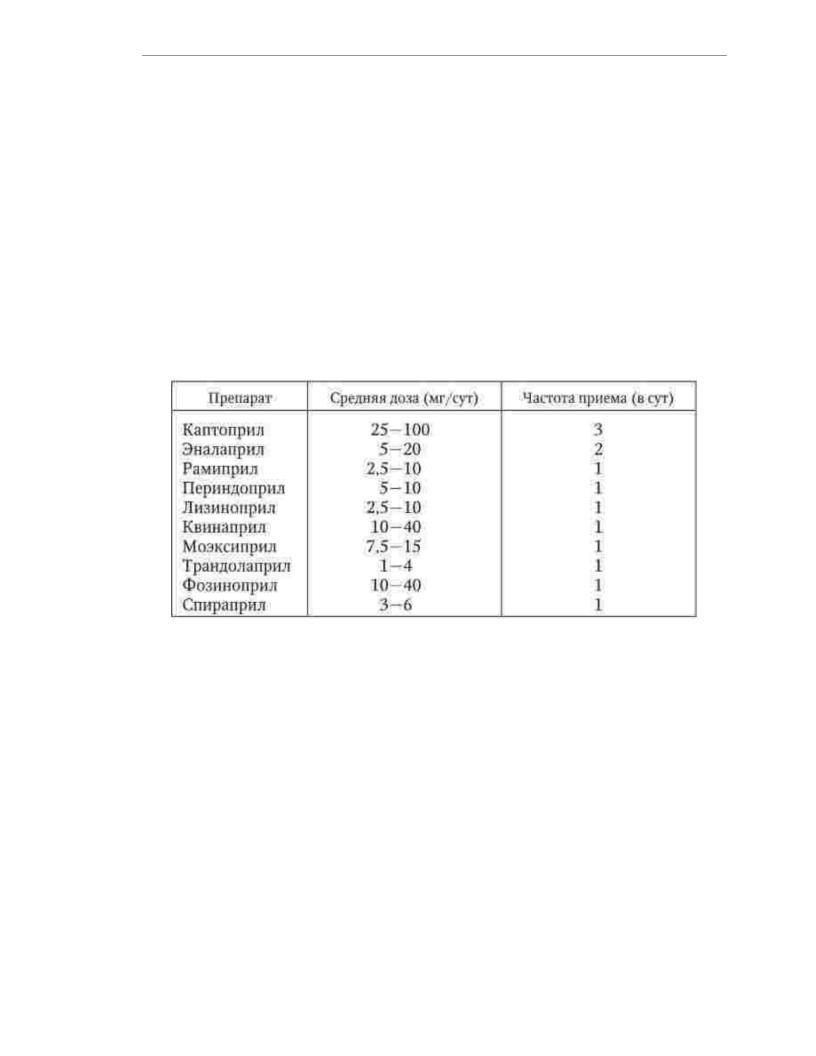
developed during treatment with drugs of this class. ACE inhibitors should be used with great caution in the treatment of patients with aortic stenosis and obstructive hypertrophic cardiomyopathy. Average doses and frequency of administration of the most
ACE inhibitors widely used in clinical practice are presented in Table. 1.13.
Table 1.13
Average doses and frequency of ACE inhibitors, the most widely used
for the treatment of patients with hypertension
The class side effects of ACE inhibitors are dry cough,
due to the accumulation of bradykinin, and angioedema. Dry cough on the background
taking ACE inhibitors is observed in 3 - 7% of patients of the Caucasian race, more often in women and smokers. The incidence of angioedema does not exceed 1%. The use of ACE inhibitors
can cause the development of renal failure and hyperkalemia,
therefore, in patients with impaired renal function, it is necessary to control the content of creatinine and potassium in the blood at the beginning of treatment. In patients taking diuretics, nitrates, and other antihypertensive drugs, there is a risk of developing hypotension
after the first dose of an ACE inhibitor. To avoid hypotension, the first dose should be discontinued. diuretics the day before taking an ACE inhibitor and start treatment with low doses of the drug.
In the process of treating patients with GB with ACE inhibitors, a gradual weakening of their
effects due to the activation of non-ACE-dependent pathways for the formation of angiotensin II (see. rice. 1.4).
Angiotensin II receptor blockers, as well as ACE inhibitors, reduce the activity of the renin-angiotensin-aldosterone system and therefore have similar indications for application. The main mechanism of the antihypertensive action of drugs of this class is
associated with the selective suppression of the effects of angiotensin II mediated by 1st receptors. type. An additional mechanism of their hypotensive effect is due to increased exposure
52
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
effects of angiotensin II on specific type 2 receptors, the activation of which causes vasodilation, increased diuresis and natriuresis (see Fig. 1.4). Compared to ACE inhibitors, drugs of this class provide a more complete blockade of the renin-angiotensin-aldosterone system, as they make type 1 receptors inaccessible to angiotensin II.
regardless of how it was formed. Absolute contraindications for use
angiotensin II receptor blockers are pregnancy, hyperkalemia, and bilateral renal artery stenosis.
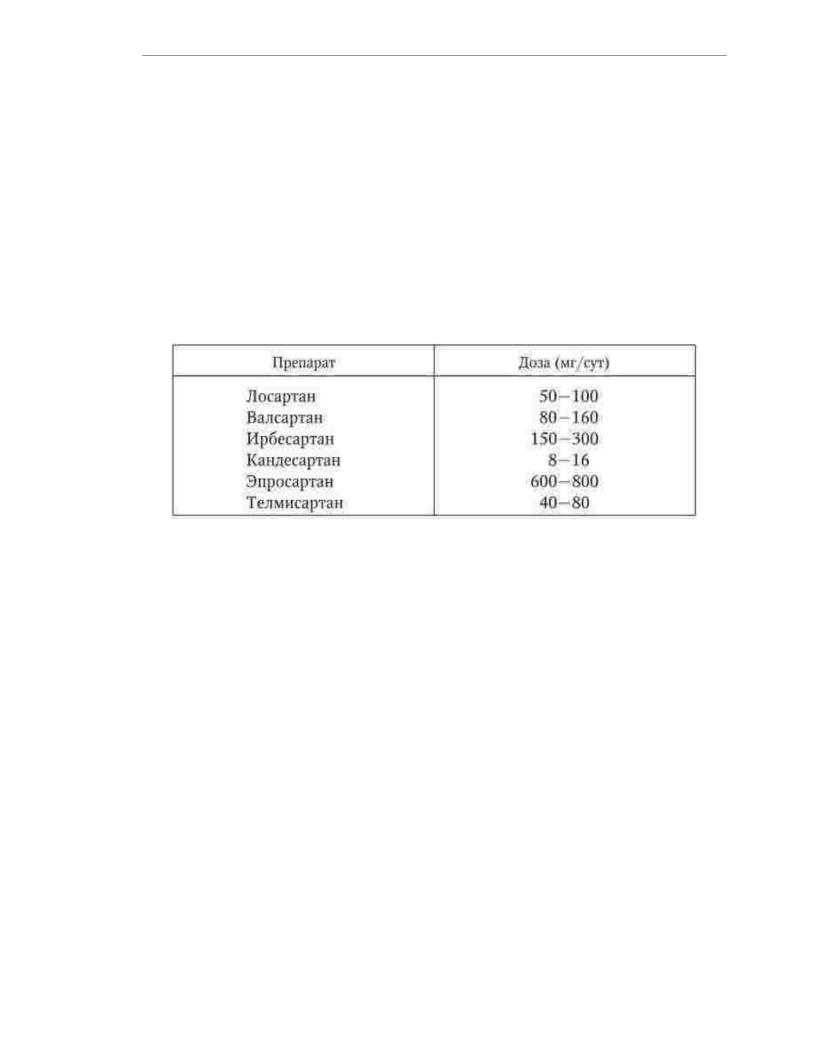
Maintenance doses of angiotensin II receptor blockers, the most widely used in clinical practice, are presented in Table. 1.14. All drugs are intended
to be taken once a day.
Table 1.14
Average doses of angiotensin II receptor blockers, most widely
changed for the treatment of patients with hypertension
Angiotensin II receptor blockers are well tolerated. Without affecting ACE, and, accordingly, on the kallikrein-kinin system, drugs of this class are less
degree than ACE inhibitors, affect the function of the endothelium, but at the same time do not cause
dry cough. At the beginning of therapy, a reversible deterioration in renal function is possible.
ÿ- blockers cause a decrease in blood pressure due to the weakening of the influence
of the sympathetic nervous system on organs and tissues. Under the influence of ÿ- adrenergic blockers, central weakening of sympathetic tone, renin release is suppressed, myocardial contractility
decreases, heart rate (HR) and cardiac output decrease. In the treatment of hypertension, non-selective and selective ÿ- blockers are used.
Due to the fact that non-selective ÿ- blockers with long-term use often cause adverse events (negative changes in the blood lipid spectrum, bronchospasm,
deterioration of microcirculation, etc.), in clinical practice, preference is given to selective drugs (metoprolol, bisoprolol, betaxolol, nebivolol).
ÿ- blockers are preferred for the treatment of patients in whom hypertension is combined with IHD and chronic heart failure, as well as patients with tachyarrhythmias. Absolute contraindications to the use of ÿ- blockers are atrioventricular (AV) blockade II - III
degree and bronchial asthma. This class of drugs should be used with extreme caution. treatment of patients with a tendency to bradycardia, chronic obstructive pulmonary disease, impaired glucose tolerance, Raynaud'sdisease, atherosclerosis obliterans
vessels of the lower extremities, peptic ulcer during the period of exacerbation.
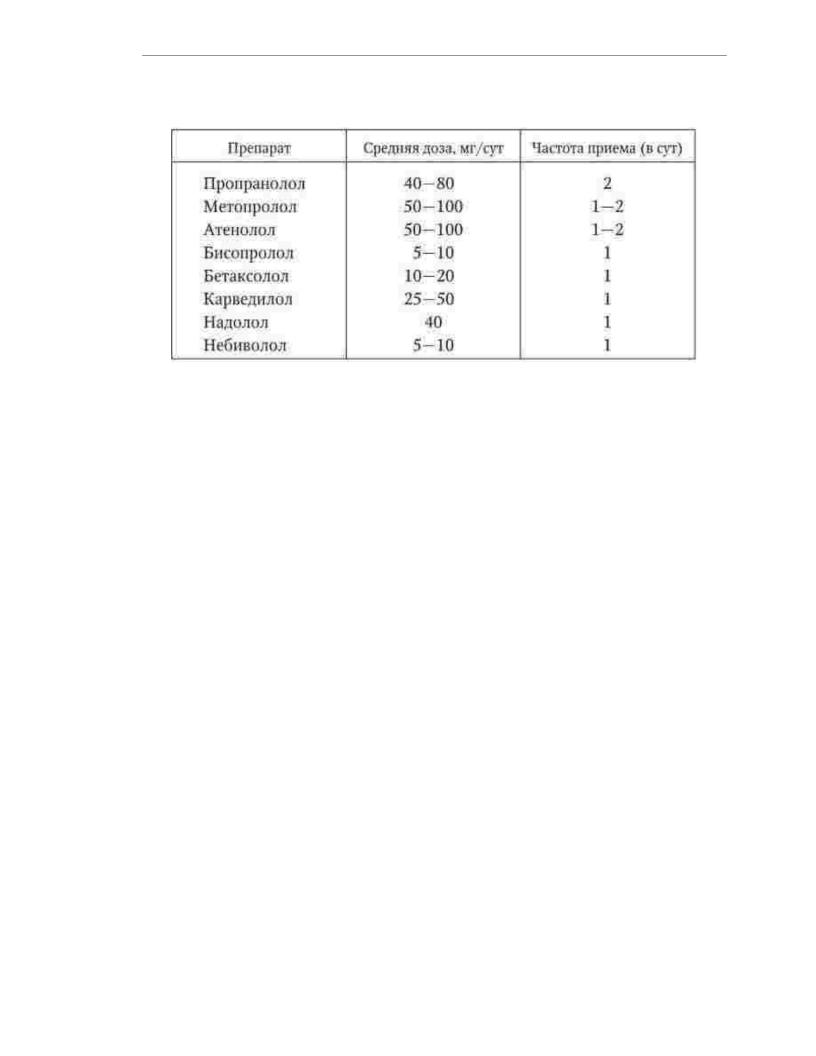
In table. 1.15 shows the average doses and frequency of taking ÿ- blockers, the most widely used in clinical practice.
Table 1.15
53
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Average doses and frequency of taking ÿ- blockers, the most widely used for the treatment of patients with hypertension
Against the background of therapy with ÿ- blockers, bradycardia may develop, slowing sinoauricular and AV conduction, increased bronchospasm, impaired glucose metabolism, as well as a number of undesirable central effects due to penetration
drugs through the blood-brain barrier: weakness, fatigue, depression, nightmares, memory impairment.
Calcium channel blockers or calcium antagonists are effective
antihypertensive agents. For the treatment of patients with hypertension, mainly longacting calcium antagonists of the second and third generations are used. Drugs in this class prevent the entry of calcium ions into the smooth muscle cells of the vascular wall and cardiomyocytes, resulting in a decrease in peripheral vascular resistance and cardiac output.
Dihydropyridine calcium antagonists (nifedipine, amlodipine, felodipine, isra dipine, nicardipine, nitrendipine, nisoldipine, lacidipine) are preferred for treatment
patients with left ventricular hypertrophy, signs of atherosclerosis of the carotid and peripheral arteries, elderly patients with isolated systolic hypertension, can be used during pregnancy. Dihydropyridines cause marked vasodilation but may lead to reflex activation of the sympathetic nervous system. This effect is especially
expressed in short-acting drugs, however, even prolonged antagonists
calcium dihydropyridine series, it is advisable to prescribe to patients with normal heart rate or tendency to bradycardia. In some patients during treatment with dihydropyridine
calcium antagonists cause swelling of the legs and feet. The development of tissue edema is associated with
dilatation of arterioles. Non-dihydropyridine calcium antagonists (verapamil and diltiazem)
recommended for the treatment of patients with hypertension in combination with coronary artery
disease and supraventricular tachycardia. This group of drugs does not cause activation of the sympathetic nervous sy system, but have negative chronotropic, dromotropic and inotropic effects, so they should
not be prescribed to patients with AV block II-III degree and chronic CH.
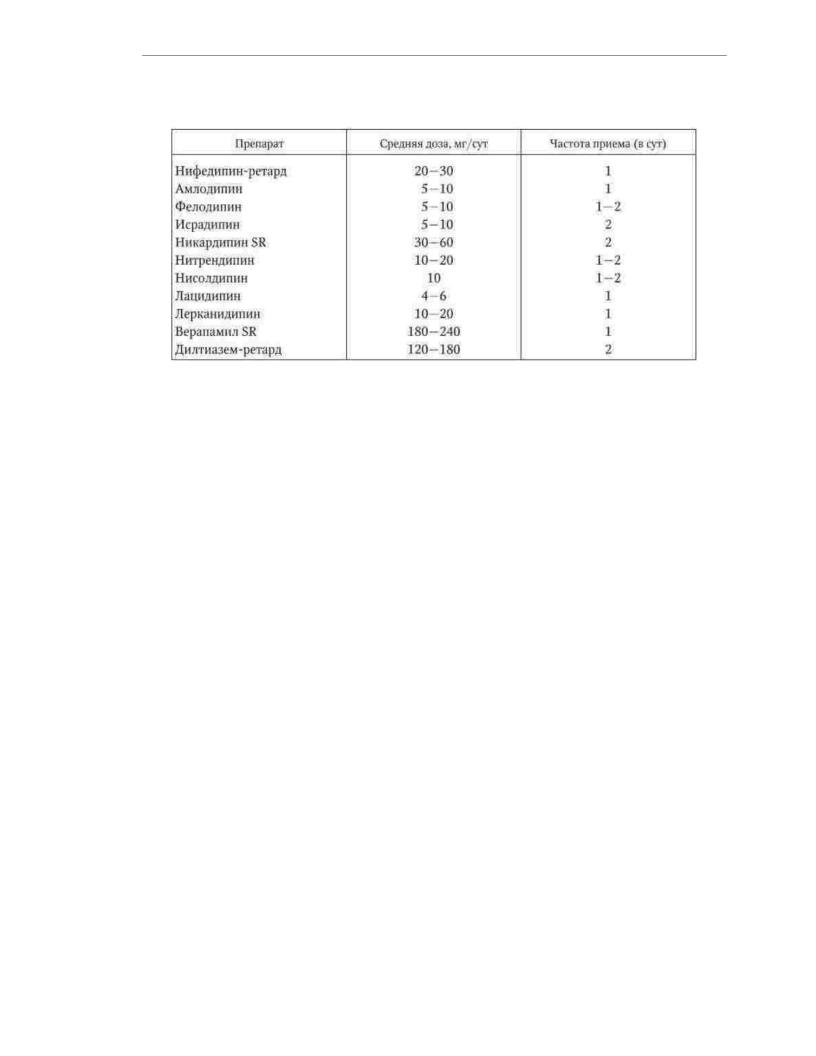
Average doses and frequency of administration of calcium antagonists, the most widely used
in the treatment of hypertension are listed in Table. 1.16.
Table 1.16
54
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Average doses and frequency of calcium antagonists, most widely
changed for the treatment of patients with hypertension
Diuretics are a heterogeneous class of antihypertensive drugs. Diuretics are divided according to the site of action on the nephron, the severity of the diuretic and antihypertensive effects, the duration of action, and the effect on metabolism. In
general, the hypotensive effect of diuretics is due to their ability to inhibit sodium reabsorption, as a result, diuresis increases, the volume of extracellular fluid and circulating
plasma decreases. Indapamide due to its effect on smooth muscle cells of the vascular wall has a direct vasodilatory effect.
In the treatment of hypertension, hydrochlorothiazide and
indapamide retard. These drugs should be used in combination of hypertension with chronic HF, accompanied by congestive syndrome, and in patients with isolated systolic
AG. Indapamide has the ability to reduce the severity of left ventricular hypertrophy. The mean doses of hydrochlorothiazide and indapamide retard are 12.5, respectively. - 25 and 1.5 mg once a day. Furosemide is mainly used in the treatment of hypertensive crises and acute HF, as well as in severe congestive syndrome,
potassium-sparing diuretics (triamterene, spironolactone) in the treatment of patients with hypokalemia and chronic HF.
Decreased extracellular fluid volume due to diuretics
can lead to the development of hypotension and be accompanied by a feeling of weakness. Application thiazide and loop diuretics can cause electrolyte disturbances, primarily
hypokalemia, which is manifested by cardiac arrhythmias and convulsions. Among
the undesirable consequences of long-term therapy with thiazide diuretics include metabolic disorders: increased risk of developing diabetes mellitus, proatherogenic changes in lipid
blood spectrum, hyperuricemia.
The hypotensive effect of ÿ- blockers (phentolamine, prazosin, etc.) is due to
blockade of the vasoconstrictor action of norepinephrine. Clonidine, methyldopa, guanfacine stimulate ÿ2adrenergic receptors in the vasomotor center of the medulla oblongata,
which leads to a weakening of the central sympathetic stimulation. Moxonidine and
rilmenidine act as agonists of the I1-imidazoline receptors of the central nervous system, activatio which is caused by inhibition of the release of catecholamines. Additional classes of antihypertensive drugs are rarely used as monotherapy. To their destination
resorted to in cases of insufficient effectiveness, contraindications to use or poor tolerance of drugs of the main classes.
55

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Combination therapy with two or more antihypertensive drugs
enhance the therapeutic effect by influencing various pathogenetic mechanisms of hypertension, reduce the risk of side effects due to the mutual neutralization of the mechanisms of their development and reduce the doses of drugs, provide more effective organ protection, and reduce the risk of cardiovascular complications. Rational combinations of antihypertensive drugs include:
1)ACE inhibitor + diuretic;
2)angiotensin II receptor blocker + diuretic;
3)ACE inhibitor + calcium antagonist;
4)angiotensin II receptor blocker + calcium antagonist;
5)dihydropyridine calcium antagonist + ÿ- blocker;
6)calcium antagonist + diuretic;
7)ÿ- blocker + diuretic;
8)ÿ- blocker + á- blocker.
In the treatment of patients with high and very high risk of vascular complications, all fixed combinations of antihypertensive drugs containing two drug compounds with a different mechanism in one tablet are more widely used.
actions. The use of fixed combinations makes it possible to reduce the number of pills taken and increase the patient'sadherence to the prescribed treatment.
Treatment of hypertensive crisis. Treatment of patients with complicated hypertensive crisis is carried out in the intensive care unit (ward). Therapeutic measures
therapy should begin as soon as possible after the diagnosis of a hypertensive crisis, but
press blood pressure should be gradual to avoid deterioration of the blood supply to the brain, heart
and kidneys. For the first 1-2 hours, it is recommended to reduce blood pressure by no more than 25% of the initial level,
and over the next 2-6 hours to achieve a decrease in systolic blood pressure to 160 mm Hg. Art., diastolic blood pressure - up to 100 mm Hg. Art. In patients with life-threatening conditions such as dissecting aortic aneurysm and acute left ventricular failure, the rate
reduction in blood pressure should be accelerated, and in patients with acute cerebrovascular
accident, on the contrary, it should be slowed down due to the high risk of increased cerebral ischemia. IN 1 - On the 3rd day after the development of ischemic stroke, active antihypertensive therapy is
recommended for blood pressure exceeding 200/120 mm Hg. Art. Treatment of patients with complicated hype
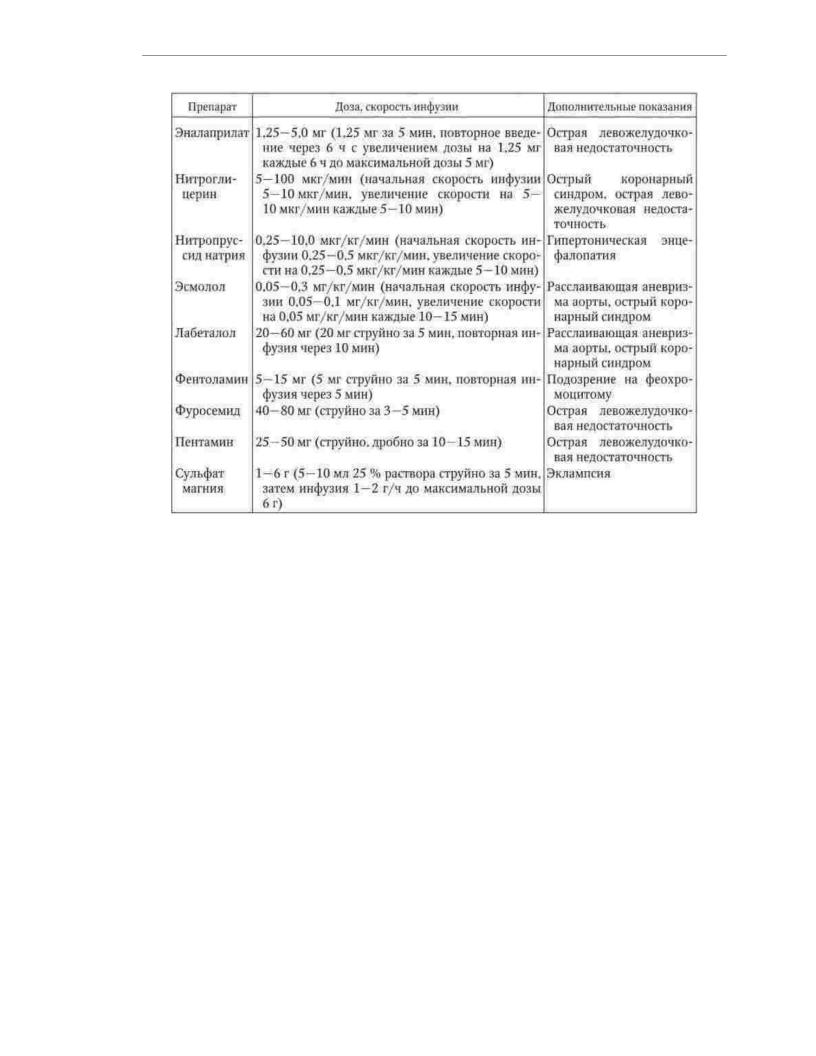
tonic crisis begins with intravenous administration of antihypertensive drugs
funds (Table 1.17). After stabilization of the patient'scondition, they switch to taking drugs. inside.
Table 1.17
Antihypertensive drugs used for parenteral (intravenous) venous) administration in the treatment of hypertensive crisis
56
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
In an uncomplicated hypertensive crisis, both intravenous and oral or sublingual use of antihypertensive drugs is possible. Treatment is started
immediately, the recommended rate of BP reduction is 25% of baseline in the first 2 hours
with the achievement of the target level of blood pressure over the next 24 - 48 hours. Therapeutic measures
(depending on the severity of clinical symptoms) can be carried out in the cardiological, therapeutic departments of a hospital or outpatient settings. To stop an uncomplicated hypertensive crisis, drugs with a relatively fast and short-term effect are used. However, the use of drugs that cause
a sharp uncontrolled decrease in blood pressure (rapid-release nifedipine, hydralazine) is considered potentially dangerous. In the absence of bilateral renal artery stenosis, oral or sublingual captopril is recommended.
25 mg every 30 to 40 minutes up to a total dose of 150 mg. Patients with a water-salt variant hypertensive crisis, especially in the presence of clinical signs of congestive heart
failure, the use of furosemide at a dose of 40–80 mg once is indicated. Absolute contraindication to the use of diuretics is gout. The drug of choice for stopping the neurovegetative
variant of a hypertensive crisis is clonidine - 0.15 mg orally, then
0.075 mg every 30 minutes for a total dose of 0.6 mg. However, the use of clonidine is contraindicated in alcohol-induced hypertensive crises, since against the background of intoxicatio this can increase the patient'slethargy and cause severe bradycardia. In these cases
it is advisable to use short-acting ÿ- blockers (propranolol, metoprolol tartrate). For suspected pheochromocytoma or use of cocaine for relief
hypertensive crisis, phentolamine (5 mg intravenously, if necessary with repeated infusion of the same dose after 5-10 minutes) should be used.
57

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
To achieve the desired result in the treatment of a patient with a hypertensive crisis and
to ensure subsequent control of blood pressure, the combined use of two is recommended, and when the need for three antihypertensive drugs.
Prevention. Secondary prevention of GB is a long-term, multi-year process, including lifestyle changes, drug use and control
the effectiveness of therapeutic measures. At the stage of achieving the target level of blood pressure, the assessment
the effectiveness of therapeutic measures, tolerability and safety of pharmacotherapy is
recommended to be carried out with an interval of 3-4 weeks. After stabilization of blood pressure at the target lev follow-up examinations by a doctor of patients with low and medium risk of vascular complications
can be done once every 6 months. Intervals between medical examinations of patients with high and very high risk, as well as patients with low adherence to treatment are not
must exceed 3 months.
Due to the fact that HD is a chronic disease, antihypertensive therapy should be carried out continuously. Withdrawal of effective drug therapy in most cases
leads to an increase in blood pressure. Only in patients with low and moderate risk, it is possible to reduce the doses and number of drugs taken, provided that changes are taken.
lifestyle and persistent reduction of blood pressure to the target level.
When compiling a program for the secondary prevention of GB in a particular patient, the
doctor must take into account not only the specifics of the disease, but also a number of other individual characteristics of the patient, including their socioeconomic status and psychological
peculiarities. The process of secondary prevention of GB requires the active participation of both the doctor and
and the patient. The most important condition for the successful prevention of cardiovascular complications of HD is to improve the medical literacy of the patient. The doctor should inform the patient about the risk factors for the disease, the nature of possible complications, the benefits of drug and drug treatment, explain the mechanisms of action of the prescribed
him drugs, discuss the main aspects of efficacy and safety
pharmacotherapy, as well as to teach the patient how to use the tonometer and give recommendations on possible independent change in doses of drugs depending on the results of measuring blood
pressure. The formation of motivation for treatment, the transformation of a patient from a passive consumer of medical services into an active participant in the treatment process helps to increase the patient'sadherence to the doctor'srecommendations and thereby reduce the likelihood unfavorable course of the disease.
58

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
1.4. CARDIAC ISCHEMIA
Definition. Ischemic heart disease (CHD) is a disease that is based on a discrepancy between coronary blood flow and the metabolic needs of the heart.
muscles.
Prevalence. IHD is one of the most common diseases and is one of the leading causes of death in the population of economically developed countries. In the Russian Federation, coronary heart disease steadily occupies the first place in the structure of mortality from diseases of the circulatory
system - this disease accounts for about half of deaths from cardiovascular causes. Taking into account the fact that mortality from diseases of the circulatory system over the past 10 years has been about 55% of the total mortality of the population, every fourth death in our country is due to coronary artery disease.
Etiology. In most cases, coronary artery disease develops as a result of atherosclerosis of the coronary arteries, so risk factors for atherosclerosis are also etiological factors of coronary artery disease. Dyslipidemia, hypertension, smoking and diabetes mellitus are among the main factors contributing to the development of coronary artery disease. Important non-modifiable risk factors for CAD are age, male sex, and a poor family history. In addition, the likelihood of developing coronary artery disease is associated with obesity, physical inactivity, dietary, socioeconomic and other modifiable risk factors.
Classification. There is no generally accepted classification of coronary artery disease to date. To solve problems of a clinical nature, the working classification of IHD is used, which is given below. Working classification of coronary artery disease: 1. Sudden cardiac death (primary cardiac arrest). 2.
Angina: 2.1. Stable exertional angina. 2.2. Unstable angina: 2.2.1. First-time angina pectoris. 2.2.2. Progressive angina. 2.2.3. Early postinfarction or postoperative angina pectoris. 2.3. Spontaneous (vasospastic, variant, Prinzmetal) angina pectoris. 3. Painless myocardial ischemia. 4. Microvascular angina (“X syndrome”). 5. Myocardial infarction: 5.1. Myocardial infarction with Q wave (large-focal, transmural); 5.2. Myocardial infarction without Q wave (small-focal, nontransmural). 6. Postinfarction cardiosclerosis. 7. Heart failure. 8. Violations of the heart rhythm and conduction. Clinical manifestations of coronary artery disease differ significantly in terms of symptoms and prognosis, which allows us to consider them as independent diseases. The presence of any one of the listed clinical variants of IHD in a patient does not exclude the appearance of another. For example, debuting MI, coronary artery disease for many years to come can only manifest itself as angina pectoris. In other cases, there is a slow or rapid progression of the disease in the form of a gradual decrease in exercise tolerance with the subsequent development of MI. In the postinfarction period, there is often a significant decrease in the functional class, and sometimes the disappearance of angina pectoris. Sometimes IHD is manifested not so much by attacks of anginal pain, but by chronic HF and disorders
59

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
heart rhythm. In some patients, the first and only manifestation of coronary artery disease is sudden death.
1.4.1. Angina pectoris (angina pectoris)
Definition. Angina pectoris is a clinical manifestation of transient myocardial ischemia, which develops as a result of an acute discrepancy between myocardial demand
in oxygen and its delivery.
Prevalence. In most European countries, the prevalence of angina pectoris is 20-40 thousand per 1 million population. The proportion of people suffering from angina pectoris increases with age. In the age group of 45 - 54 years, angina is diagnosed in 2 -
5% of men and 0.5 - 1% of women, in the group of 65 - 74 years - 10 - 20% of men and 10 - 15% women, in the group older than 75 years, the prevalence of angina pectoris is 25-33% and not has gender differences.
Pathogenesis. The main factors determining the need of the heart muscle
in oxygen, are myocardial tension, myocardial contractility, heart rate, preand post-load. Because coronary artery perfusion occurs during diastole,
delivery of oxygen to the myocardium depends not only on the capacity of the coronary arteries, but also on the level of diastolic pressure in the aorta and the duration of diastole. Under physiological conditions, the correspondence of myocardial oxygen supply to its metabolic needs is achieved by changing the resistance of the coronary arteries. At a constant perfusion pressure due to the expansion of the coronary arteries, the volume velocity coronary blood flow can increase 4-5 times compared to its value in
rest. This mechanism makes it possible to avoid myocardial ischemia during physical and emotional stress.
The main reason for the discrepancy between oxygen delivery and metabolic needs myocardium is atherosclerosis of the coronary arteries, the morphological features of which found in 90% of patients with angina pectoris. A decrease in the elasticity of the walls and
the subsequent narrowing of the lumen of the coronary arteries lead to a decrease in the coronary reserve A clinically significant level of stenosis is considered to be a decrease in the internal diameter
coronary artery by 70 - 75%. With this degree of narrowing of the lumen of the artery, the coronary blood flow is insufficient to meet the metabolic needs of the myocardium under conditions
of physical exertion or emotional stress. Among others
possible causes of angina pectoris include congenital anomalies of the coronary arteries, coronaryitis, severe anemia, as well as conditions associated with an increase in myocardial oxygen demand to a level exceeding the capacity of unchanged coronary arteries: hypertrophic cardiomyopathy (HCM), hypertension, hyperthyroidism, aortic malformations heart, excessive physical stress, etc.
The atherosclerotic process is accompanied by the development of endothelial
dysfunction, which is manifested by the impaired ability of the coronary bed to vasodilate in response to vasodilating stimuli and increased adhesiveness of the endothelial vascular lining. In a
number of patients, the leading mechanism for reducing oxygen delivery to the myocardium is inorganic narrowing of the coronary arteries and limitation of their expansion.
reserve, but vasospasm or reversible intravascular thrombosis. Increased response of the coronary artery to neurohormonal vasoconstrictive stimuli and formation
unstable platelet aggregates are noted not only in places of pronounced atherosclerotic damage to the vascular wall, but also in areas of vessels without visible anatomical changes, since the pathophysiological basis of dynamic coronary obstruction
is local damage and dysfunction of the endothelium. In most patients
60
