
1-280 pdf (1)
.pdf
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
melts 2-3 times compared to women of the same age who do not take these drugs. In most cases, hypertension induced by oral contraceptives
is reversible.
During a normal pregnancy, regular changes occur
blood pressure levels in the form of a slight decrease in diastolic blood pressure in the first trimester and a moderate increase in systolic and diastolic blood pressure in late pregnancy. After delivery, blood pressure returns to its original values. The diagnosis of AH is established
in women who have had a stable increase in blood pressure without signs of secondary AH before pregnancy and persist after childbirth. Preeclampsia is a syndrome directly associated with pregnancy that includes hypertension first diagnosed after
20 weeks pregnancy, proteinuria more than 0.3 g/day and/or edema. Gestational hypertension is called isolated increase in blood pressure in the second half of pregnancy with its normalization after
childbirth, without proteinuria.
Resistant, or refractory, hypertension is called in cases where, against the background of the use three antihypertensive drugs, including a diuretic, at doses close to the maximum,
within 6 weeks. unable to reach target blood pressure. There are three groups of causes of resistant hypertension: those associated with the physician (inaccurate blood pressure
measurement, incorrect choice of drug therapy, incorrect recommendations for non-drug treatment), associate patient (lack of adherence to treatment, excessive fluid and salt intake, smoking, alcohol abuse, psycho-emotional stress, sedentary lifestyle) and independent causes (obesity and
hyperinsulinemia, hypertension
white coat", neurosis-like disorders, genetically determined features metabolism of drugs, causing their accelerated inactivation).
Malignant hypertension is characterized by extremely high blood pressure (more than 180/120 mm Hg) with
the development of severe changes in the vascular wall in the form of fibrinoid necrosis, which leads to tissue ischemia and rapidly progressive dysfunction of various organs.
Malignant hypertension is characterized by pronounced activation of neurohormonal systems, which causes an increase in natriuresis, development of hypovolemia, damage to the endothelium, and proliferation of smooth muscle elements of the vascular wall. These changes
not only contribute to the stabilization of hypertension, but also stimulate the release of vasoconstrictors into t leads to an even greater increase in blood pressure. In the malignant course of hypertension,
visual disturbances are often noted due to edema of the papilla of the optic nerve and hemorrhages in the retin cerebrovascular accident, myocardial infarction, progressive renal failure. At
some patients develop disorders of the rheological properties of blood and hemostasis, up to before the development of disseminated intravascular coagulation. This clinical variant is rare in practice, mainly in patients with secondary and/or severe hypertension.
The course of GB acquires special features when it is combined with the pathology of the bronchi and lungs,
impaired renal function, coronary artery disease, cerebrovascular disease, chronic heart failure and others pathological conditions. The most common complications of hypertension are hypertensive
crisis, cerebrovascular accident, myocardial infarction, heart failure, hemorrhage and bleeding. various localizations.
A hypertensive crisis is an acute, pronounced increase in blood pressure, accompanied by the appearance or aggravation of clinical symptoms on the part of target organs and requiring an immediate controlled decrease in blood pressure. With the advent of effective antihypertensive drugs, the frequency of the crisis course of GB decreased. In modern Russia due to the significant prevalence of hypertension and poor adherence of patients crises complicate the course of GB in 5% of patients and are one of the most frequent reasons for calling ambulances.
41

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
For the diagnosis of a hypertensive crisis, an increase in systolic and diastolic
BP is of equal importance, and there are no general quantitative criteria for hypertension that allow establishing this diagnosis without regard to clinical symptoms. The nature of an individual reaction to an increase in blood pressure depends not only on its level, but also on the state of autoregulation of cerebral blood flow, therefore, in some patients, even a moderate increase in blood pressure causes symptoms of a hypertensive crisis, while other patients do not experience discomfort even with a more pronounced increase in blood pressure. Level
The blood pressure to be aimed at during treatment is also determined individually, since with its decrease there is a potential danger of cerebral hypoperfusion
brain and other organs.
At the heart of a sharp increase in blood pressure is a sudden imbalance between the volume of intravascular fluid and vascular resistance. Leading role in pathogenesis hypertensive crisis play neurohumoral disorders. Due to hyperstimulation
the renin-angiotensin-aldosterone and sympathetic-adrenal systems damage the vascular endothelium, increase the synthesis of vasoconstrictors (angiotensin II, vasopressin, endothelin 1, catecholamines) and decrease the formation of endogenous vasodilators
(nitric oxide and prostacyclin). An increase in aldosterone production, combined with impaired renal perfusion, leads to sodium and water retention. Tissue ischemia contributes
further overproduction of renin and an increase in blood pressure. As a result of tissue hypoperfusion, fibrinoid necrosis of arterioles develops and vascular permeability increases. wall, which leads to the formation of perivascular edema. The combination of these factors as damage to the endothelium with a weakening of its fibrinolytic activity and increased
production of thromboxane with subsequent activation of platelets, create conditions for the development
Tiya disseminated intravascular coagulation.
An important cause of disorders of cerebral hemodynamics in hypertensive crisis
is a violation of autoregulation of cerebral blood flow. Normally, cerebral blood flow is maintained at a constant level with an average blood pressure of 60 to 120 mm Hg. Art. With an increase in systemic blood pressure, cerebral hypoperfusion is prevented by compensatory constriction cerebral vessels. Disruption of autoregulation mechanisms occurs with an increase in the average
BP to values above 180 mm Hg. Art. Cerebral edema develops against the background of vasodilation, which
accompanied by clinical symptoms of hypertensive encephalopathy.
In typical cases, a hypertensive crisis is manifested by symptoms due to
increased blood pressure (headache, shortness of breath, discomfort in the heart area, minor visual disturbances in the form of flickering "flies" and "fog" before the eyes), and clinical manifestations of hypertensive encephalopathy (dizziness, nausea, vomiting,
lethargy, severe visual impairment, up to blindness). In the neurovegetative variant of a hypertensive crisis, the clinical picture is dominated by symptoms of hypersympathicotonia: psycho-emotional arousal, tremor, tachycardia, facial flushing,
increased moisture content of the skin. This clinical variant is characterized
polyuria. In the water-salt (edematous) variant, signs of moderately pronounced cerebral edema dominate in the form of lethargy, disorientation in time and space, and nausea. The appearance of an extended symptomatology of a crisis is often preceded by a decrease in diuresis. The convulsive variant develops in patients with severe cerebral edema, which
manifested by increasing nausea, vomiting, clonic and tonic convulsions, a progressive disorder of consciousness from confusion to its complete loss, pronounced
visual impairments. During a hypertensive crisis, cerebrovascular accident of a transient nature or cerebral stroke, MI, acute HF, manifested by cardiac asthma or pulmonary edema, may develop.
42

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Hypertensive crises are divided into complicated (life-threatening) and uncomplicated. non-life-threatening.
A complicated hypertensive crisis is accompanied by life-threatening complications, the appearance or aggravation of target organ damage and requires an emergency reduction in blood pressure with the help of parenterally administered drugs. Hypertensive
A crisis is considered complicated in cases when its development is combined with the following conditions and features of hypertension:
1)hypertensive encephalopathy;
2)cerebral stroke;
3)acute coronary syndrome;
4)acute left ventricular failure;
5)dissecting aortic aneurysm;
6)pheochromocytoma;
7)preeclampsia or eclampsia of pregnant women;
8)severe hypertension associated with subarachnoid hemorrhage or trauma
brain;
9)patients in the postoperative period with a threat of bleeding;
10)patients taking amphetamine, cocaine and other drugs with a hypertensive
effect.
Uncomplicated hypertensive crisis is characterized by severe clinical symptoms, but is not accompanied by life-threatening complications and significant dysfunction of target organs. in the treatment of patients with uncomplicated hypertension
crisis, both intravenous and oral or sublingual use is possible
antihypertensive agents.
Violation of cerebral circulation. The results of numerous epidemiological studies
have confirmed the existence of a direct relationship between the incidence of cerebral stroke and the risk of death from this disease with the level of blood pressure. Structural and functional changes vascular walls that develop in patients with GB become the morphological basis as
ischemic and hemorrhagic strokes. Local cerebral ischemia develops as a result of thrombosis of an atherosclerotic artery, or its embolism due to arrhythmia (most often atrial fibrillation - AF) or the presence of a blood clot in the cavity
left ventricle. The cause of transient ischemia may be the formation of a platelet
aggregate in the area of damaged atherosclerotic plaque, followed by platelet mobilization. Hemorrhagic stroke develops due to rupture of microaneurysms
small cerebral arteries.
In the acute period of a stroke, most patients have an increase in systolic blood pressure > 150 and diastolic blood pressure > 90 mm Hg. Art. When determining the optimal
for a patient'sblood pressure level and the rate of its drug correction, it must be taken into account that long-lasting hypertension contributes to the development of cerebral edema, can lead to
the transformation of ischemic stroke into hemorrhagic one, and increases bleeding
from the damaged vessel into the brain tissue. On the other hand, mild hypertension in ischemic stroke is a compensatory reaction aimed at preventing negative consequences
acute cerebral ischemia. The presence of a U-shaped relationship between the level
BP in the first 48 hours after stroke and mortality. In this regard, in patients with ischemic stroke, a rapid decrease in blood pressure to values less than 140/90 mm Hg. Art. Not
recommended. In patients with hemorrhagic stroke that developed against the background of severe hyper high risk of bleeding progression, a rapid decrease in blood pressure by 25 -
30% of the original level. With medical correction of blood pressure in patients with stroke during
43

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
avoiding cerebral hypoperfusion requires careful monitoring of neurological
symptoms.
Myocardial infarction. Mortality from coronary artery disease, as well as mortality from cerebral stroke, is directly related to the level of blood pressure. The main factors contributing to the development of coronary insufficiency in hypertensive patients are atherosclerosis and left ventricular hypertrophy. Atherosclerosis leads to narrowing of the lumen of the coronary arteries and increased risk of thrombotic occlusion. Left ventricular hypertrophy is accompanied by impaired microcirculation, leads to an increase in myocardial oxygen demand and, due to the development
of perivascular fibrosis, prevents its penetration from the blood
into cardiomyocytes. Due to the violation of the electrophysiological properties of the myocardium, acute coronary insufficiency in patients with left ventricular hypertrophy is more often than in patients
with normal mass of the heart muscle, accompanied by ventricular disorders
rhythm.
Due to the fact that left ventricular hypertrophy causes a decrease in coronary
reserve, with the development of MI against the background of high blood pressure, aggressive
antihypertensive therapy is not recommended. A sharp decrease in blood pressure (especially diastolic, since coronary
arteries occurs in the phase of relaxation of the heart muscle) can lead to increased myocardial ischemia. At the same time, persistent hypertension (systolic BP > 180 mmHg and/or
diastolic blood pressure > 110 mm Hg Art.) is a relative contraindication to thrombolytic therapy, which can significantly reduce the risk of death in patients with myocardial infarction. Besides, AH due to increased afterload increases myocardial oxygen demand and increases the likelihood of developing acute left ventricular failure. In this regard, the optimal for the majority of patients
with MI that developed against the background of AH is considered to be a decrease in blood pressure by 15 - 20% of the original level.
Heart failure. The individual risk of developing chronic HF in patients with hypertension is lower than in MI, diabetes mellitus, and approximately corresponds to that in patients with valvular heart disease. However, given the significant prevalence of hypertension, it outperforms other diseases of the cardiovascular system in terms of population.
the attributable risk of developing chronic HF, which, according to the Framingham study, is 42% for men and 57% for women. In the Russian Federation, chronic HF is associated with hypertension in 80% of cases.
A feature of chronic HF in AH is the high frequency of diastolic dysfunction of the heart muscle. The main cause of increased myocardial stiffness in patients
GB is left ventricular hypertrophy. On average, half of patients with clinical
symptomatology of chronic heart failure, there is no decrease in the ejection fraction of the left ventricle. AT 70 - 90% of cases in these patients are diagnosed (or noted in the past) hypertension. Availability
Chronic HF and its pathophysiological features influence the choice of antihypertensive therapy.
Acute HF in the form of cardiac asthma or pulmonary edema usually develops with a sudden an increase in blood pressure due to an increase in total peripheral vascular resistance.
In most cases, acute left ventricular failure with an increase in blood pressure occurs in patients with coronary artery disease with reduced myocardial contractility. An additional reason for it development in some patients becomes a tachysystolic form of AF.
Hemorrhages and bleeding of various localizations. Developing with hypertension morphological changes in the vascular wall and increased intravascular pressure
increase the risk of rupture of small vessels and bleeding of various localizations. More often
As blood pressure rises, nosebleeds occur. A number of patients have bleeding from the mucous membrane of the trachea, bronchi and gastrointestinal tract. Prognostic
44

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
more unfavorable are damage to the intima of the aorta with the formation of a dissecting aneurysm and retinal hemorrhage.
Forecast and outcomes. With timely diagnosis and adequate therapy, the prognosis
patients with GB is favorable. Lack of treatment or inadequate therapy is associated with an increased risk of complications and death of patients. It should be emphasized that the adequacy of therapy implies not only the achievement of the target level of blood pressure, but also the use of
drugs that have maximum effectiveness in relation to the variant of the disease characteristic of a particular patient, taking into account the totality of his individual characteristics.
Treatment. The main (strategic) goal of treating hypertensive patients is to maximize reducing the risk of developing cardiovascular complications and death from them, i.e. in improving forecast. To achieve this goal, it is necessary to solve a number of auxiliary (tactical)
tasks:
1)achievement of the target level of blood pressure;
2)correction of all modifiable risk factors (smoking, dyslipidemia, obesity
and etc.);
3)prevention and / or achievement of reverse development of damage to target organs;
4)treatment of associated diseases (CHD, cerebrovascular disease, diabetes
diabetes, etc.).
The target level of blood pressure is considered 140/90 mm Hg. Art. and less. With good tolerance prescribed therapy, it is advisable to reduce blood pressure to lower values. In patients with
high and very high risk of cardiovascular complications, reduce blood pressure to
values less than 140/90 mm Hg. Art. within 4 weeks. In the future, subject to good tolerance, it is recommended to reduce blood pressure to 130 - 139/80 - 89 mm Hg. Art. and less. When bad
tolerability of lowering blood pressure, it is recommended to slow down the pace of achieving its target level. Lowering blood pressure should be carried out in several stages. At each stage, blood pressure decreases by 10 - 15% of the baseline for 2 - 4 weeks. followed by a break for patient adaptation
to lower blood pressure levels. If the transition to the next stage causes a deterioration in the patient's well-being, you should return to the previous level of blood pressure and stay there for another
for a while. The lower limit of safe blood pressure reduction is 110 - 115/70 - 75 mm
rt. Art. In the process of treating elderly patients, it is necessary to monitor the value of the pulse Blood pressure, preventing its increase, which occurs mainly due to a decrease in diastolic blood pressure.
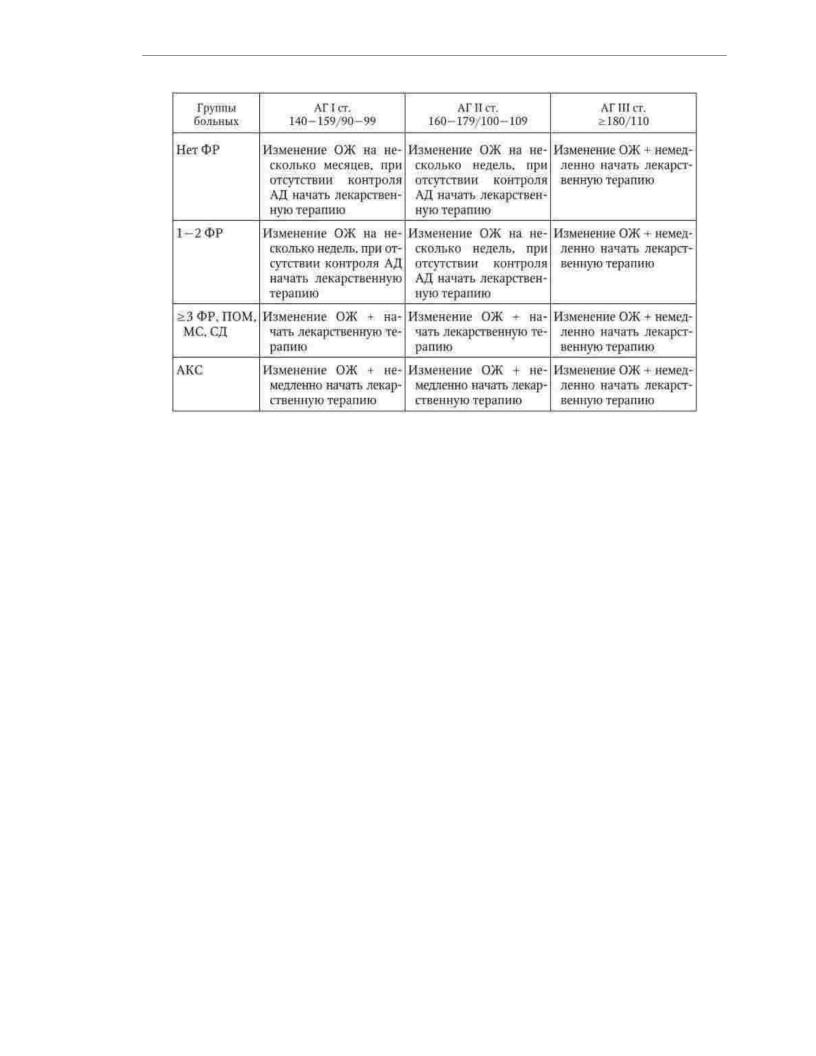
After assessing cardiovascular risk, it is necessary to determine the individual patient management (Table 1.9).
Table 1.9
Tactics of managing patients with hypertension depending on the risk of cardiovascular complications
45
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
The most important aspect of the tactics of managing a patient with GB is the decision on the need administration and choice of drug therapy. The main indication for the appointment of antihypertensive drugs is the degree of cardiovascular risk. Should
note that there is strong evidence for the benefit of antihypertensive therapy in individuals with high normal BP in combination with high and very high
the risk of cardiovascular complications. Recommendations for lifestyle changes should
be given to all patients with hypertension or high normal BP associated with at least one risk factor. In individuals with high and very high total cardiovascular risk, antihypertensive therapy is prescribed immediately, regardless of the level of blood pressure. With an average
risk in patients with hypertension 1 - 2nd st. lifestyle changes are recommended with an assessment of the result and
decision to start drug therapy after a few weeks, in individuals with high
normal blood pressure, the duration of the period of only non-drug exposure is determined individually. The prescription of drugs is certainly justified in patients with high normal blood pressure in combination with the metabolic syndrome, in the presence of
signs of target organ damage and several risk factors. Persons with high normal BP, with no more than 2 risk factors, are prescribed only image change
life.
Non-drug effects. Carrying out activities to change the image
of life is a mandatory component of the treatment of each patient with GB. In a significant proportion of
patients with high normal blood pressure and arterial hypertension of the 1st tbsp. in the absence or presence of 1 - 2 fact
risk only lifestyle changes without the use of antihypertensive drugs
means to achieve normalization of blood pressure. In patients requiring pharmacotherapy, lifestyle changes increase sensitivity to antihypertensive drugs
drugs.
Non-drug methods of exposure include:
1)smoking cessation;
2)normalization of body weight (BMI < 25 kg/m2 );
3)reduced consumption of alcoholic beverages (less than 30 g of alcohol per day for men
and less than 20 g per day for women);
46
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
4)increase in physical activity - regular aerobic (dynamic) physical load for 30 - 40 minutes at least 4 times a week;
5)reducing the consumption of table salt to 5 g/day;
6)change in diet with an increase in the consumption of plant foods, an increase in the diet of foods containing potassium, calcium (vegetables, fruits, grains), magnesium
(dairy products), as well as reducing the consumption of animal fats.
Medical treatment. In the process of drug treatment of patients with GB, it is necessary to achieve a gradual decrease in blood pressure to the target level. The rate of decrease in blood
pressure is determined individually. Particular care should be taken to reduce blood pressure in elderly patients a patients with stroke and myocardial infarction.
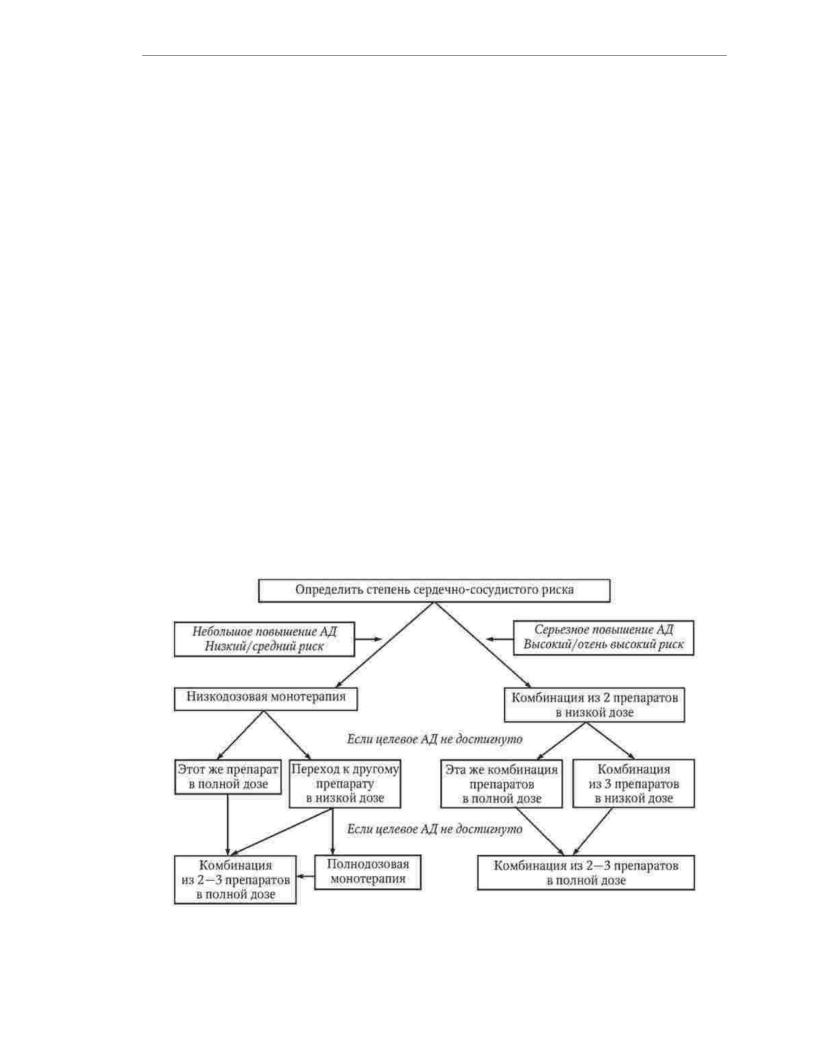
The strategy of starting pharmacotherapy is determined depending on the initial blood pressure and degree of cardiovascular risk (Fig. 1.3).
Monotherapy at the beginning of treatment is recommended for patients with a slight increase in blood pressure.
and low or moderate risk of cardiovascular complications. The combination of two drugs at low doses is preferable for patients with 2nd - 3rd stage hypertension, high or very high
the risk of cardiovascular complications. In the absence of the desired result in patients with low or moderate risk of cardiovascular complications, they switch to taking
the prescribed drug at a full dose or another drug is prescribed at a low dose, and then, at necessary, in a full dose and only at the next stage of treatment, combined pharmacotherapy is used. In patients at high or very high risk of CV events, if low-dose 2-drug combinations fail, switch to
to a full-dose combination of the same drugs or additionally prescribe a third drug
at a low dose. If this increase in therapy does not lead to the achievement of the target BP level,
³
use a full-dose combination of 2-3 drugs. Patients with blood pressure 160/100 mm Hg. Art., having a high and very high risk of cardiovascular complications, combined
therapy with two drugs at a full dose can be prescribed at the start of treatment.
Rice. 1.3. The choice of initial therapy to achieve the target level of blood pressure
47
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
For long-term antihypertensive therapy, it is necessary to use long-acting drugs that provide 24-hour control with a single dose.
BP, which not only reduces its variability, but also increases the adherence of patients to treatment. For combination therapy, drugs with different mechanisms of action should be chosen, which allows for better control of blood pressure, minimizing side effects. effects and suppress counter-regulatory mechanisms for increasing blood pressure. In order to increase patient adherence to doctor'sprescriptions, it is recommended to use fixed combinations of antihypertensive drugs - drugs containing two drug compounds in one tablet.
Five classes of antihypertensive drugs are recommended for the pharmacotherapy of HD: angiotensin-converting enzyme (ACE) inhibitors - ACE inhibitors, receptor blockers angiotensin II (ARB), ÿ- blockers (BAB), calcium antagonists (AK), diuretics.
As additional classes of antihypertensive drugs for combined therapy, ÿ- blockers and imidazoline receptor agonists can be used.
The choice of drug for a particular patient is determined by many factors. Most important of them are the presence and nature of risk factors, signs of damage to target organs, associated clinical conditions, concomitant diseases; features of the patient's individual reaction to drugs of various classes in the past;
the likelihood of interactions between antihypertensive drugs and drugs that the patient accepts for other reasons. Given that the treatment of hypertension is a process that requires most cases of prolonged use of several drugs,
their choice should be made taking into account socio-economic factors, including and cost of pharmacotherapy.
Indications for the use of the main classes of antihypertensive drugs and
recommendations for the choice of pharmacotherapy for hypertension depending on the clinical situation in table. 1.10 and 1.11. When choosing a drug treatment for a particular patient, it is necessary to
take into account contraindications to the use of antihypertensive drugs
(Table 1.12).
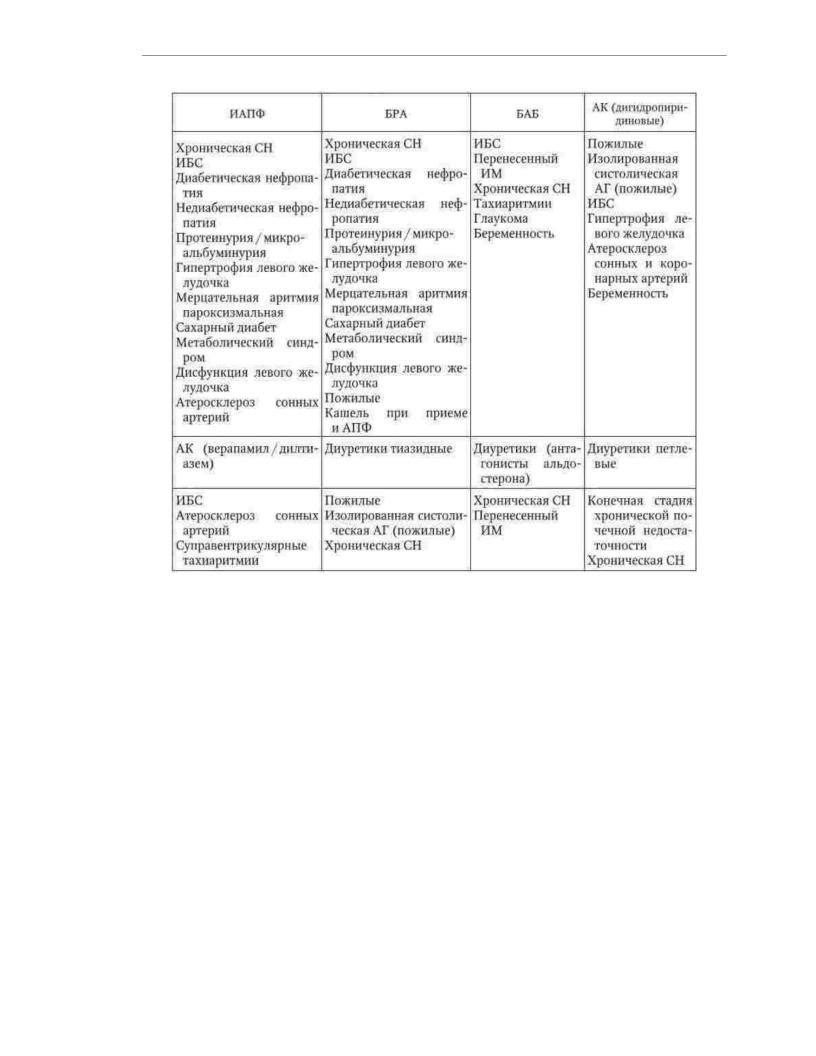
Table 1.10
Primary indications for the appointment of antihypertensive drugs various classes
48
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Table 1.11
Recommendations for the choice of antihypertensive drugs depending on the clinical situation
49

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Table 1.12
Contraindications for different classes of antihypertensive drugs
drugs
fifty
