
1-280 pdf (1)
.pdf
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
progressive loss of elasticity. Changes in the vessels of the kidneys in combination with a violation of the autoregulation of renal blood flow, which is typical for hypertension, lead to the development of nephrosclerosis, up to the formation of a primary wrinkled kidney. Damage to retinal vessels
in severe hypertension, it is manifested by the formation of microaneurysms, thrombosis, hemorrhages, edema of the optic nerve papilla. Elevated blood pressure causes the development of hypertrophy
and lipogi alinosis of the wall of small intracerebral arteries. Due to the narrowing of their lumen worsens perfusion and rarefaction of the white matter of the brain occurs. Occlusion of small intracerebral arteries leads to the occurrence of lacunar infarcts, and rupture of microaneurysms leads to hemorrhages in the brain tissue with subsequent formation of cysts.
Since hypertension accelerates the development of atherosclerosis of large arteries, the corresponding changes in the vascular wall of the aorta, arteries of the lower extremities, coronary, cerebral
arteries, as well as histological signs of myocardial infarction and ischemic strokes can be considered as indirect morphological manifestations of GB.
Classification. The classification of magnitude adopted in Russia and European countries BP in persons over 18 years of age is presented in Table. 1.6. If systolic BP and diastolic BP values fall into different categories, then the severity of hypertension is assessed by more
high category. The most accurate degree of hypertension can be determined in patients with for the first time diagnosed hypertension and in patients not taking antihypertensive drugs.
Table 1.6
Classification of blood pressure levels, mm Hg. Art.
*Isolated systolic hypertension should be classified into grade 1, 2, 3
according to the level of systolic blood pressure.
The results of 24-hour BP monitoring and self-monitoring of BP by the patient at home can help in the diagnosis of hypertension, but do not replace repeated BP measurements by a healthcare
professional. Criteria for diagnosing hypertension based on the results of blood pressure measurements, performed by a doctor, a patient at home, and according to the data of daily monitoring of blood pressure are different. The presence of hypertension is indicated by blood pressure levels of 8 140/90
mm Hg. Art. when measured by a healthcare professional, 8135/85 mmHg. Art. when measured by a patient at home conditions and average daily blood pressure 8 130/80 mm Hg. Art. according to daily monitoring data.
The severity of hypertension, the prognosis and tactics of treating a patient are determined not only by the level of blood pressure.
In addition to determining the degree of hypertension, the assessment of overall cardiovascular risk includes an analysis
risk factors, diagnosis of target organ damage and associated clinical states.
Risk factors that significantly affect the prognosis of patients with hypertension include:
1) the value of pulse blood pressure (in the elderly);
31

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
2)age (men > 55 years, women > 65 years); 3) smoking;
4)dyslipidemia: total cholesterol > 5.0 mmol/l (190 mg/
dl), or LDL cholesterol > > 3.0 mmol/l (115 mg/dl), or HDL cholesterol < 1.0 mmol/l (40 mg/dl) for men and <1.2 mmol/l (46 mg/dl) for women, or TG > 1.7 mmol/l (150 mg/dl);
5) fasting plasma glucose 5.6 - 6.9 mmol / l (102 - 125 mg / dl); 6) impaired glucose tolerance; 7) family history of early cardiovascular disease (in men < < 55 years, in
women < 65 years);
8) abdominal obesity (waist circumference > 102 cm for men and > > 88 cm for women) in the absence of metabolic syndrome. Signs of left ventricular hypertrophy, thickening and decreased
elasticity of the walls of large arteries, and dysfunction
kidneys.
Signs of left ventricular hypertrophy include: 1) ECG criteria:
Sokolov-Lyon sign (the sum of the depth of the S wave in lead V1 and the height of the R wave in lead V5 or V6) > 38 mm, Cornell product (the sum of the height of the R wave in lead aVL and the depth S wave in lead V3 multiplied by the duration of the QRS complex) > 2440 mm/ms;
8125 g/m2 2) echocardiographic criterion: left ventricular myocardial mass index for men and 8110 g/m2
Signs of vascular damage include:for women1) ultrasound. signs of arterial wall thickening (intima-media layer thickness > 0.9 mm) or atherosclerotic plaques main vessels;
2) the speed of the pulse wave from the carotid to the femoral artery> 12 m/
s; 3) ankle-brachial index (the ratio of the maximum blood pressure in the arteries of the lower extremities - a. dorsalis pedis or a. tibialis posterior - to the maximum blood pressure in the brachial artery) < 0.9. Signs of kidney damage include: 1) a slight increase in serum creatinine: 115 - 133 µmol /
l (1.3 - 1.5 mg / dl) for men or 107 - 124 µmol / l (1.2 - 1.4 mg / dl). dl) for women;
2) low glomerular filtration rate < 60 ml/min/1.73 m 2 (MDRD formula) or low
creatinine clearance < 60 ml/min (Cockcroft-Gault formula); 3) microalbuminuria 30 - 300 mg / day; 4)
albumin/creatinine ratio in urine g (3.5 mg/mmol) for women.
³
22 mg/g (2.5 mg/mmol) for men and
Glomerular filtration rate according to the MDRD formula (ml / min / 1.73 m atinine / 0.88 ÿmol / l) - 1.154 ´ (age,byears)0.742-. 0Creatinine.203. For womeclearan,cetheaccordingresult is multipliedtothe
Cockcroft-Gault formula (ml / min):
For women, the result is multiplied by 0.85.
Diagnostic criteria for diabetes are:
32

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
1)fasting plasma glucose 8 7.0 mmol / l (126 mg / dl) with repeated measurements;
2)plasma glucose after a meal or 2 hours after taking 75 g of glucose > > 11.0 mmol / l (198 mg/dl).
The diagnosis of the metabolic syndrome is established by a combination of the main and 2 additional criteria from among the following. The main criterion is abdominal obesity (waist circumference > 94 cm for men and > 80 cm for women). Additional criteria: BP
³
130/85 mmHg. Art.; LDL cholesterol> 3.0 mmol / l; HDL cholesterol < 1.0 mmol/l for men and < 1.2 mmol/l for women, TG > 1.7 mmol/l; hyperglycemia fasting ³ 6.1 mmol/l, naru glucose tolerance - plasma glucose 2 hours after ingestion of 75 g glucose and £ 11.1 mmol / l.
Associated clinical conditions are diagnosed in the presence of the following
signs.
Cerebrovascular disease:
1)ischemic cerebral stroke;
2)hemorrhagic cerebral stroke;
3)transient ischemic attack. Heart disease:
1)IM;
2)angina pectoris;
3)coronary revascularization;
4)chronic heart failure (HF).
Kidney diseases:
1)diabetic nephropathy;
2)renal failure: serum creatinine > 133 µmol/ l (1.5 mg/dl) for men and >124 µmol/ l (1.4 mg/dl) for women.
Peripheral artery disease:
1)dissecting aortic aneurysm;
2) symptomatic lesion of peripheral arteries. Hypertensive retinopathy:
1)hemorrhages or exudates;
2)swelling of the nipple of the optic nerve.
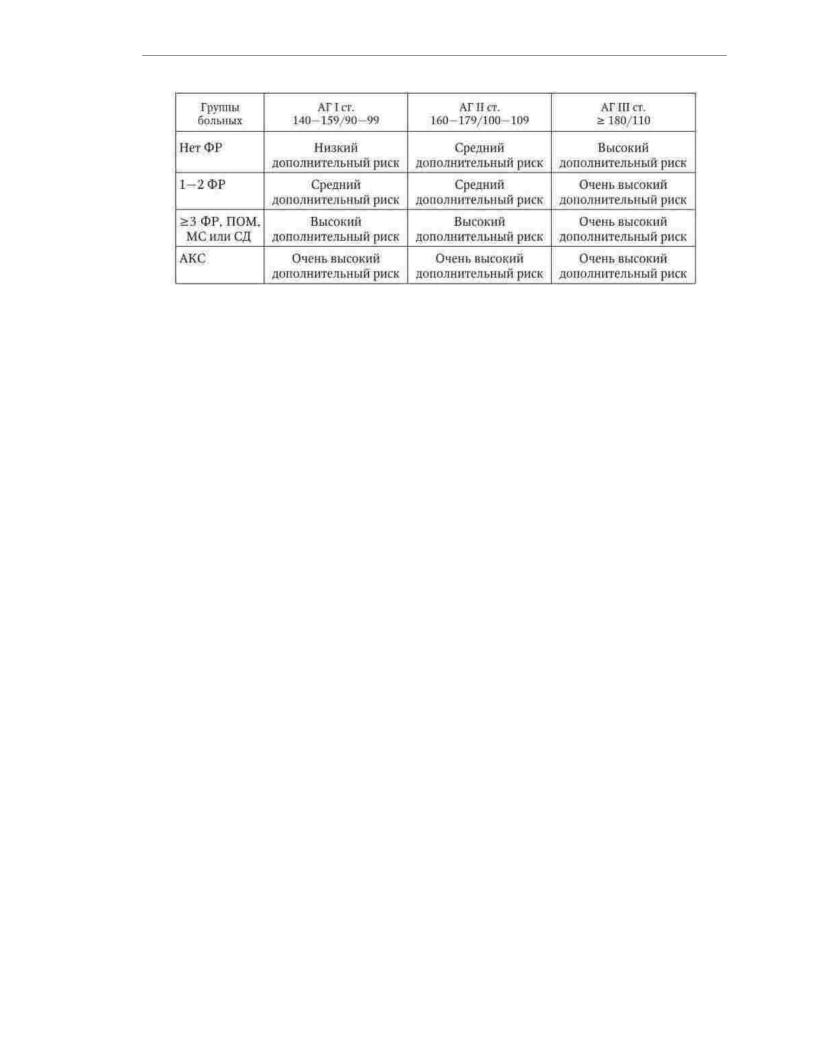
Depending on the degree of increase in blood pressure, the presence of risk factors, signs of target organ damage, diabetes mellitus, metabolic syndrome and associated clinical conditions, patients with hypertension can be assigned to one of 4 groups: low, moderate, high and very high additional risk (Table 1.7). low risk
corresponds to the probability of developing cardiovascular complications and death from them in the next 10 years < 15%, medium risk - 15 - 20%, high - 20 - 30% and very high > thirty %. Assessment of the overall cardiovascular risk is an essential component of the
diagnosis of hypertension and is of great importance when choosing the tactics of treating a patient. clinical picture. There are no specific symptoms of GB. At the initial stage of the
disease and with the slow progression of hypertension, many patients do not experience any discomfort.
Table 1.7
Risk stratification in hypertensive patients
33
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Note. The accuracy of determining the total cardiovascular risk directly depends on how complete the clinical and instrumental examination of the patient was. Without
data of ultrasound examination of the heart and blood vessels for the diagnosis of hypertrophy of the left
ventricle and thickening of the wall (or plaque) of the carotid arteries up to 50% of hypertensive patients may be
erroneously categorized as low or moderate risk instead of high or very
high.
The most characteristic complaint of a patient with GB is headache, which in most cases appears when blood pressure rises to a certain level or when it is sharp. changes. Often, headache due to hypertension is localized in the occipital region, but
often patients experience pain in the frontal, parietal, temporal regions. In addition to the head pain typical for GB are transient visual disturbances in the form of flickering "flies"
and "fog" before the eyes. Persistent visual impairment, including blindness, develops with retinal damage - degenerative changes, hemorrhages, arterial thrombosis. Many patients complain of increased fatigue, weakness, decreased performance, irritability, poor sleep, and emotional lability. In addition to neurotic disorders, HA can be manifested by moderate aching pain or heaviness in the area
hearts. Unlike angina pectoris, these sensations are not provoked by physical activity and are not treated with nitroglycerin. Their appearance is usually associated with emotional stress and
increased blood pressure. At the same time, in patients with concomitant coronary artery disease, a sharp ri AD can lead to the development of a typical anginal attack due to an increase in fasting and
an increase in myocardial oxygen demand. In some patients, with an increase in blood pressure, nosebleeds occur.
With the progression of HD, the clinical picture of the disease begins to predominate symptoms caused by atherosclerosis of various vascular pools: coronary,
cerebral, peripheral arteries. Patients develop angina, signs of chronic cerebrovascular insufficiency, intermittent claudication. Often formed
and chronic HF. Moreover, the violation of the pumping function of the heart is manifested not only in patients with concomitant coronary artery disease, leading to a decrease in myocardial
contractility. With severe left ventricular hypertrophy, chronic heart failure may develop as a result of diastolic dysfunction of the heart muscle.
An objective study of patients with GB at the initial stage of the disease allows identify some non-specific changes due to an increase in blood pressure: solid pulse, moderate tachycardia, in the presence of severe left ventricular hypertrophy -
strengthening of the apex beat, accent II tone over the aorta. As the disease progresses and complications develop, additional symptoms appear: systolic murmur
over the base of the heart, due to atherosclerosis of the ascending aorta, expansion of the boundaries of relative cardiac dullness to the left with dilatation of the left ventricle, IV tone
34

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
due to a change in the strength and speed of contraction of the left atrium with an increase in diastolic pressure in the cavity of the left ventricle. Formation of associated clinical
states is accompanied by corresponding clinical signs. For example, motor and sensory disorders in patients who have undergone acute disorders of the brain
blood circulation; weakening, absence and asymmetry of the pulse, cooling and trophic disorders of the skin of the lower extremities with a pronounced atherosclerotic narrowing of the corresponding arteries. The development of chronic heart failure, in addition to dilatation of the left ventricle, is manifested by the appearance of a systolic murmur of mitral regurgitation, in the case of
a pronounced decrease in the contractile function of the myocardium - tone III, as well as congestive hri
pov in the lungs.
The accuracy of diagnosing and determining the degree of hypertension depends on compliance with the rules for
measuring blood pressure.
Measurement of blood pressure should be carried out in a calm and comfortable environment after rest, the duration of which should be at least 5 minutes. The patient should sit leaning on the back of a chair
with relaxed, uncrossed legs. The hand on which it is measured
BP, must be exposed and placed on the table so that the middle of the cuff,
placed on the shoulder, was at the level of the patient'sheart. Blood pressure is recommended to be measured 1-2 hours after a meal. Within 1 hour before measuring blood pressure, the use of coffee and strong tea, smoking is excluded, the intake of sympathomimetics, including nasal
and eye drops. The lower edge of the cuff applied to the shoulder should be located at 2 - 2.5 cm above the elbow. The inflated part of the cuff must cover at least 80%
shoulder circumference. At least two blood pressure measurements are taken on each arm with an interval of at least
less than a minute. With a difference in results exceeding 5 mm Hg. Art., produce an additional measurement and for the final value of blood pressure take the average of the results of the last two measurements. Air is pumped into the cuff quickly to a pressure value of 20 mm Hg. Art. exceeding systolic blood pressure, the approximate level of which is determined by the disappearance of the pulse in the radial artery. Blood pressure is measured with an accuracy of 2 mm Hg. Art. The rate of pressure reduction in the cuff is about 2 mm Hg. Art. per second. The value of systolic blood pressure
determined by the appearance of the first phase of Korotkoff'stones. The pressure level in the cuff at which there is a disappearance of tones (V phase of Korotkov'stones), corresponds to diastolic blood pressure. If Korotkoff sounds are heard at very low blood pressure values (which can be observed
in children, with thyrotoxicosis, fever, aortic insufficiency, in pregnant women), the value
diastolic blood pressure is determined at the beginning of phase IV, i.e., with a significant weakening of tones. Repeated measurements of blood pressure are made after complete bleeding of air from the cuff.
Laboratory and instrumental diagnostics. Examination of a patient with hypertension begins with the use of simple methods that are mandatory for each patient. If by
the history and physical examination do not reveal signs of damage
target organs and associated clinical conditions, and there is no suggestion of secondary hypertension, the use of additional research methods is not required.
However, in some cases, for example, for a detailed assessment of the condition of a patient with a complicated the course of the disease or clarification of the causes of secondary hypertension, it becomes necessary
to conduct not only an additional, but also an in-depth study of the patient. Mandatory research methods include:
1)clinical blood test;
2)general urinalysis;
3)determination of glucose in blood plasma (on an empty stomach);
4)determination of the content in the blood serum of total cholesterol, LDL cholesterol, HDL cholesterol, TG, creatinine;
35

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
5)determination of creatinine clearance (according to the Cockcroft-Gault formula) or the rate of barrel filtration (according to the MDRD formula);
6)ECG.
Additional recommended research methods include:
1)determination of the content of uric acid and potassium in the blood serum;
2)echocardiography;
3)determination of microalbuminuria;
4)examination of the fundus;
5)ultrasound of the kidneys and adrenal glands;
6)Ultrasound of brachiocephalic and renal arteries;
7)X-ray of the chest organs;
8)daily monitoring and self-control of blood pressure;
9)determination of the ankle-brachial index;
10)determination of the speed of the pulse wave (an indicator of the rigidity of the main
arteries);
11)oral glucose tolerance test - when the level of glucose in blood plasma >
5.6mmol/l (100 mg/dl);
12)quantitative assessment of proteinuria (if the use of diagnostic strips
confirmed the presence of microalbuminuria). In-depth research methods include:
1) to assess the condition of a patient with complicated hypertension - a study of the brain, myocardium, kidneys, main arteries;
2) to identify secondary forms of hypertension - a study in the blood of the concentration of aldosterone, corticosteroids, renin activity; determination of catecholamines and their metabolites in daily urine and/or blood plasma; abdominal aortography; computed tomography or
magnetic resonance imaging of the adrenal glands, kidneys and brain.
During the laboratory and instrumental examination of a patient with hypertension
great importance is attached to the diagnosis of damage and control of the state of target organs, as this allows determining the risk of cardiovascular complications, evaluating the efficacy and safety of antihypertensive therapy.
Electrocardiography and echocardiography are used to evaluate the state of the heart. results of which it is possible to calculate the voltage criteria for left ventricular hypertrophy (Sokolov-Lyon index and Cornell product) and determine the myocardial mass index
left ventricle. According to the ratio of the thickness of the posterior wall of the left ventricle and its radius
taking into account the mass index of the myocardium of the left ventricle, echocardiography allows you to determine
type of left ventricular remodeling, which is important for assessing the prognosis. Criteria for the diagnosis of concentric, eccentric hypertrophy and concentric remodeling
left ventricle are shown in Fig. 1.2.
Prognostically the least favorable is concentric hypertrophy
left ventricle. In addition to the size of the cavities and the thickness of the walls of the heart, echocardiography makes it possible to assess the systolic and diastolic functions of the left ventricle.
To diagnose damage to the main arterial vessels, an ultrasound examination of the common carotid artery is performed. A sign of arterial wall hypertrophy is a moderate increase in the thickness of the intimamedia layer. The value of this indicator, exceeding 1.3 mm, is regarded as a sign of atherosclerotic damage to the artery. FROM
using Doppler ultrasound on the vessels of the ankle and shoulder, the ankle-brachial index can
be calculated more accurately than the results of conventional blood pressure measurements, the decrease in whi is considered an indirect sign of severe atherosclerosis of the arteries of the lower extremities. AT
in recent years, great importance in assessing the likelihood of developing cardiovascular complications
36

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
The decrease in elasticity (increase in rigidity) of large arteries, as a result of which the velocity of propagation of the pulse wave increases, is attributed to the decrease in elasticity. An increase in the speed of propagation of the pulse wave in the area between the carotid and femoral arteries associated with an increased risk of complications.
Rice. 1.2. Types of left ventricular remodeling
Diagnosis of kidney pathology and clarification of their functional state are based
on the results of the study of the level of creatinine in the blood serum and the excretion of protein in the urine. In all patients, creatinine clearance is calculated using the Cockcroft-Gault formula or glomerular
filtration rate using the MDRD formula. All patients are tested
the presence of protein in the urine using test strips. If the result is negative, it is recommended the use of special methods for detecting microalbuminuria, the diagnostic criterion of which is the
loss of protein in the amount of 30–300 mg/day. Microalbuminuria is regarded not only as a diagnostic criterion for nephropathy, but also as a sign of systemic
vascular pathology. There is a continuous direct relationship between the amount of albumin in the urine and the risk of cardiovascular complications.
The study of the fundus is advisable to perform in young patients and patients with severe AH. Small changes in retinal vessels are nonspecific and often
37

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
are found out of connection with AG. Pronounced changes (exudates, hemorrhages, swelling of the nipple optic nerve) are associated with increased cardiovascular risk.
To assess the state of the brain, such highly informative research methods as computed tomography and magnetic resonance imaging are increasingly being used. With the help of these methods, transferred (including
asymptomatic) cerebral strokes, the localization and nature of pathological changes in the brain tissue were clarified. When examining elderly patients, an assessment is sometimes required cognitive functions. For this purpose, special tests and questionnaires are used.
A promising direction in the examination of patients with GB is genetic analysis,
the results of which can provide important information about the individual etiopathogenetic features of the disease, as well as predict the efficacy and safety of antihypertensive therapy.
Diagnosis. GB is diagnosed by excluding symptomatic (secondary) hypertension. In general, the proportion of patients with secondary hypertension is relatively small and amounts to
about 5% of the total number of patients with high blood pressure. However, the diagnosis of HD becomes valid only after the assumptions have been proven wrong.
about the presence of other pathological processes in the patient, accompanied by hypertension.
The diagnosis must indicate the stage of the disease. Stage I GB suggests the absence target organ damage, stage II AH - the presence of changes in one or more target organs, stage III AH - the presence of associated clinical conditions. In the diagnosis
The main risk factors, target organ damage and associated clinical conditions should be reflected. The degree of hypertension must be indicated in patients with for the first time
revealed increase in blood pressure. In other cases (against the background of therapy), the achieved degree of AG. In the absence of associated clinical conditions due to its high
The predictive value of HD in the diagnosis is indicated first. In patients with associated clinical conditions that are characterized by a stronger negative impact on the prognosis, especially those that occur in an acute form, HA may occupy the structure
diagnosis is not the first position.
Examples of diagnoses:
1.GB I stage. Degree of hypertension - 2. Dyslipidemia. Risk 2 (medium).
2.GB stage II. Degree of hypertension - 3. Dyslipidemia. Hypertrophy of the left ventricle. Risk 4 (very high).
3.GB stage II. Degree of hypertension - 2. Dyslipidemia. Obesity I degree. Impaired glucose tolerance. Risk 3 (high).
4.Stage III GB. Achieved degree of arterial hypertension - 1. Obliterating atherosclerosis of the vessels of the lower extremities, intermittent claudication. Risk 4 (very tall).
5.IHD, acute coronary syndrome. 27.08.09. GB stage III. Degree
AH - 1. Risk 4 (very high).
differential diagnosis. There are many diseases whose clinical presentation includes hypertension. To signs of a general nature, allowing to suspect
symptomatic hypertension, refers to early (under the age of 20 years) or, on the contrary, later (in persons older than 65 years) onset of the disease, rapid achievement of grade III hypertension (> 180/100 mm Hg), severe damage to target organs, refractoriness to antihypertensive therapy. The main groups of
diseases accompanied by an increase in blood pressure are indicated in Table. 1.8.
Table 1.8
The main causes of secondary arterial hypertension
38

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Most often, secondary hypertension develops as a result of kidney pathology. Nephrogenic hypertension may be due to diseases that cause damage to the renal parenchyma, narrowing of the renal arteries
and impaired outflow of urine from the kidneys. The second place in frequency is occupied by symptomatic AH developing as a result of endocrine diseases - the main
Thus, the pathology of the pituitary and adrenal glands. The third group of causes of symptomatic hypertension - these are pathological conditions associated with anatomical defects in the vascular system,
as a result of which violations of the central hemodynamics are formed. From secondary hypertension hemodynamic genesis in practice, coarctation of the aorta is most common. Fourth
the group of secondary hypertension is caused by neurological diseases: encephalitis, brain tumors, diencephalic syndrome, etc. Finally, the fifth and sixth groups
The reasons for the increase in blood pressure of a symptomatic nature are toxic and drug effects.
These include lead poisoning, alcohol-induced hypertension, and
39

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
the use of a number of drugs with a hypertensive effect (glucocorticoids, hormonal contraceptives, erythropoietin, etc.).
Patients in whom history, physical examination, and the results of the use of mandatory diagnostic methods suggest secondary hypertension require careful investigation using more sophisticated laboratory and diagnostic methods.
instrumental diagnostics, such as a study of the concentration of hormones in plasma blood and urine, radionuclide renography, Doppler ultrasound and
angiography of the renal arteries, aortography, computer and / or magnetic resonance
tomography of the kidneys, adrenal glands, brain, etc. Identification of the cause of secondary hypertension is of fundamental importance, since it allows you to choose the option of pathogenetically
substantiated medical or surgical treatment that provides
significant improvement in quality of life and prognosis, and in some cases complete cure
patient.
Flow. HD is a chronic disease with a relatively benign course. Along with general symptoms, there are some features of the clinical manifestations of the disease that are characteristic of certain groups of patients.
In elderly and senile patients, isolated systolic AH is often (in 60–70% of cases) noted. The pathophysiological basis of the predominant increase in systolic blood pressure is a decrease in the elasticity of the aorta and large arteries. Normal release
blood from the left ventricle is accompanied by their stretching, which prevents a sharp increase in blood pressure on the vascular wall. With age, the main arteries become
more rigid, the speed of the pulse wave increases, which leads to an increase in systolic blood pressure due to insufficient repayment of the direct hemodynamic shock and due to movement of the reflection wave from diastole to systole. In addition to an increase in systolic
and pulse blood pressure, in elderly patients, the variability of blood pressure increases, orthostatic and postprandial hypotension is often noted. Morphological and
functional changes in the kidneys contribute to the development of hypersensitivity to
salt. In addition, in elderly patients, the clinical picture of GB, along with an increase in blood pressure, often includes symptoms of atherosclerosis of the cerebral, coronary and femoral arteries.
Hypertension in children and adolescents is much more likely than in adults to be secondary. The early onset of HD is associated primarily with a genetic predisposition to this disease. An increase in blood pressure in childhood and adolescence is usually noted in patients
with obesity and low physical activity. In children, hypertension is often combined with hypersympatic ticotonia. In this regard, they are characterized by tachycardia and a hyperdynamic type of central hemodynamics, and the most common option for increasing blood pressure is
isolated systolic hypertension. A typical feature of the course of hypertension in children and adolescents is the lability of blood pressure: patients of this age group are characterized by "hypertension
white coat”, periods of stable hypertension may be replaced by long episodes of normoand even hypotension, which creates objective difficulties in diagnosing GB.
In women, menopause is a strong risk factor for hypertension. The frequency of hypertension in postmenopausal women increases by 2-4 times compared with the period of preserved fertile
function. It is believed that the main reasons for the increase in blood pressure in postmenopausal women are a decre
sex hormones and increased salt sensitivity. In addition, middle-aged women are more likely than men to have such a risk factor for hypertension as abdominal obesity, with
closely related to the development of insulin resistance. Another adverse consequence of menopause is the development (progression) of dyslipidemia, mainly
by increasing LDL and lowering HDL, as well as hypertriglyceridemia.
One of the reasons for the increase in blood pressure in young women is the use of hormonal contraceptives. Against the background of taking contraceptives, the frequency of hypertension increases
40
