
1-280 pdf (1)
.pdf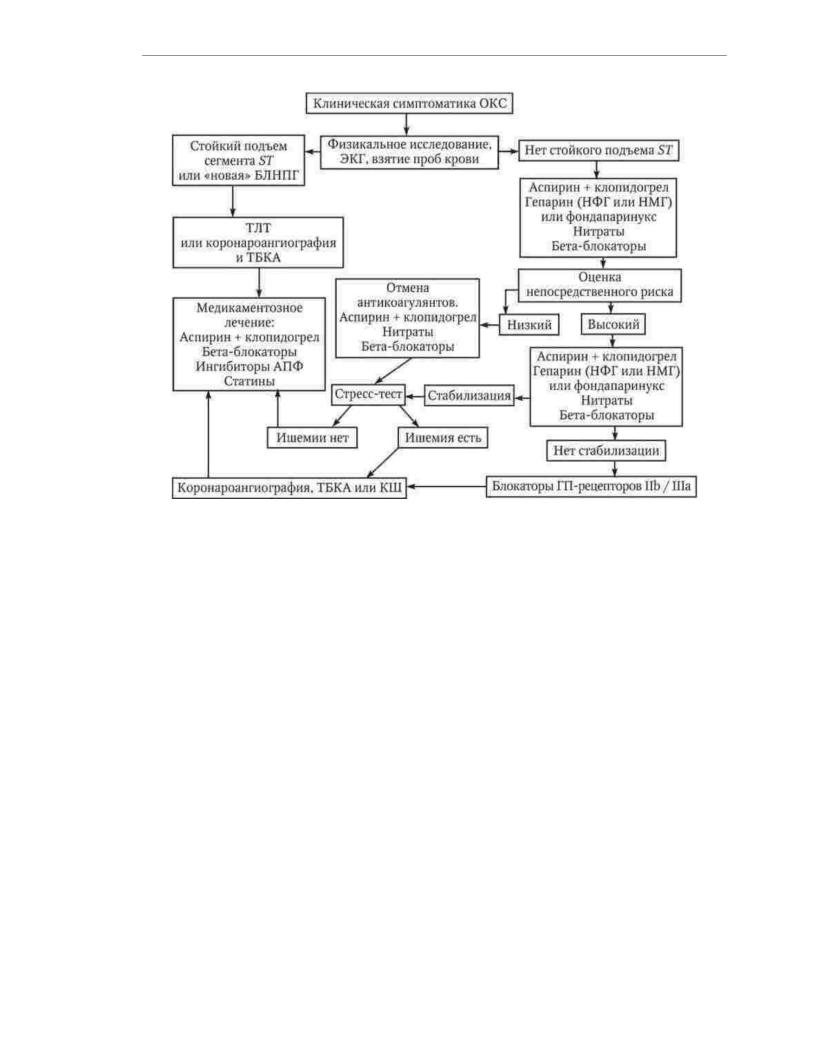
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Rice. 1.10. Algorithm of medical care for a patient with acute coronary syndrome (OKS)
Drugs used to prevent thrombosis
coronary artery occlusion in patients with acute coronary syndrome are subdivided to antithrombotic and antithrombin agents, which respectively prevent
platelet aggregation and thrombin formation.
The most widely used antiplatelet agent is acetylsalicylic acid.
(aspirin). A single dose of aspirin, which is recommended to be taken when clinical symptoms of acute coronary syndrome appear, is 150-300 mg. To speed up
absorption, the tablet should be chewed. Subsequently, it is recommended to take aspirin in dose of 75 - 100 mg / day, without chewing, once a day after meals.
Clopidogrel is given in combination with aspirin in all patients except patients requiring urgent coronary bypass surgery. Loading dose
clopidogrel is 300 mg, with the planned procedure of primary coronary balloon angioplasty - 600 mg. The maintenance dose of clopidogrel is 75 mg/day.
Duration of clopidogrel use in patients with non-ST elevation acute coronary syndrome (i.e. non-Q wave MI or episode of unstable angina) and
also for patients who underwent transluminal coronary balloon angioplasty and a drugeluting stent, is 1 year; for patients who have undergone acute coronary syndrome with ST segment elevation (i.e., MI with a Q wave), - at least
4 weeks
Dual antiplatelet therapy provides more pronounced than the application
aspirin alone, reduced risk of coronary heart disease exacerbation, but associated with an increased risk bleeding. The new platelet ADP-receptor blocker ticagrelor is characterized by
the same risk of bleeding as clopidogrel, but superior to it in the ability to prevent
91

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
rotate cardiovascular complications in patients with acute coronary syndrome. The drug is used in combination with aspirin. The loading dose of ticagrelor is 180 mg.
maintenance dose - 90 mg 2 times a day.
Regardless of which chemical compound triggers the process of platelet activation, the affinity of glycoproteins sharply increases at its final stage.
fibrinogen IIb/IIIa receptors. Based on this, blockade of glycoprotein receptors
IIb/IIIa is a universal, i.e., independent of the type of activator, mechanism of inhibition of platelet aggregation. Short-term intravenous administration of glycoprotein IIb/IIIa receptor antagonists improves outcomes and reduces the incidence of
complications of percutaneous coronary balloon angioplasty, both in combination and without combination with stent placement.
It is recommended to administer unfractionated heparin to patients with acute coronary syndrome without ST segment elevation as soon as possible after the onset of clinical
symptoms intravenously according to the following scheme: a bolus of 60–80 IU/kg (but not more than 5000 IU), then infusion 12 - 18 IU / kg / h (but not more than 1250 IU / h). Optimal Speed
administration of heparin is determined by the value of activated partial thromboplastin time, which during therapy should be increased by 1.5–2.5 times compared with the normal value of this indicator for the laboratory of this medical institution. The duration of heparin therapy is determined by the time to achieve stabilization
condition of the patient, averaging 3-5 days. Patients with acute coronary syndrome with ST segment elevation, unfractionated heparin is given intravenously as follows:
scheme: bolus 60 IU/kg (but not more than 4000 IU), then infusion 12 IU/kg/h (but not more than 1000 Sword). Heparin dose adjustment is carried out taking into account the activated partial thromboplastin time, which should be 1.5 - 2 times the normal value.
for this laboratory. The duration of intravenous infusion of heparin should be at least 48 hours. In the future, it can be injected under the skin of the abdomen at 7500 - 12 500
IU 2 times a day.
Unfractionated heparin is poorly absorbed from the subcutaneous fat layer, actively binds to plasma proteins and endothelial cells, as a result of which it bioavailability when administered subcutaneously is only 15 - 20%, and the half-life
in plasma - 50 - 60 min. By reducing thrombin-induced platelet aggregation, heparin enhances the action of other aggregation inducers. In 1-5% of patients, heparin causes thrombocytopenia. After completion of heparin therapy, there is a danger
development of the "rebound" syndrome, manifested by hypercoagulability and relapses of myocardial ischemia. Finally, the very conduct of heparin therapy using an infusion
pump and the need to monitor activated partial thromboplastin time is quite laborious. In this regard, in the treatment of patients with acute coronary syndrome, low molecular weight heparins are increasingly being used, to a large extent
devoid of the disadvantages of unfractionated heparin. Enoxaparin is administered according to the
following scheme: intravenous bolus of 30 mg, then under the skin of the abdomen at a dose of 1 mg/kg 2 times a day within 2 - 8 days. During the administration of enoxaparin, monitoring of coagulation
parameters is not required.
In order to inhibit the process of thrombosis in the treatment of patients with acute coronary syndrome, fondaparinux, a drug that selectively blocks
X-activated coagulation factor. Fondaparinux is injected under the skin of the abdomen dose of 2.5 mg once a day. The duration of treatment is up to 8 days. In the treatment of
fondapar with rinux, as well as during therapy with low molecular weight heparins, there is no need for regular coagulological monitoring. Fondaparinux is preferred in
treatment of patients with non-ST elevation acute coronary syndrome, may be used
92

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
to be involved in the treatment of patients with ST-segment elevation acute coronary syndrome (including including and in combination with thrombolytic therapy), but it is not recommended to
administer it to patients referred for primary (i.e., performed instead of thrombolysis) coronary ball
pubic angioplasty.
Anticoagulant therapy can be canceled by the end of the first day of treatment, if at admission to the hospital and after 6-12 hours the level of troponin is normal
or the patient does not meet the clinical criteria for membership during follow-up at high risk of death or MI.
Restoration of blood flow in the coronary artery in patients with acute non-ST segment elevation coronary syndrome helps prevent the development of MI, and in patients with developing MI, it reduces the volume of necrotic myocardium, reduces the risk of life-
threatening arrhythmias and the development of heart aneurysm. There are two ways to restore blood flow for a thrombosed coronary artery: medication with the use of thrombolytic
means and non-drug, including percutaneous coronary interventions and coronary bypass grafting.
Thrombolytic drugs are divided into nonspecific (streptokinase) and specific (alteplase, tenecteplase, purolase). Nonspecific fibrinolytics have
systemic fibrinolytic action. Specific fibrinolytics cause activation
plasminogen directly in the thrombus and are safer drugs - their use is associated with a lower risk of bleeding than the use of non-specific fibrinolytics.
In the absence of contraindications, thrombolytic therapy is carried out in patients with acute coronary syndrome with ST segment elevation, if the time from the onset of anginal attack does not exceed 12 hours, and the ECG shows ST segment elevation of more than 0.1 mV less than 2 adjacent chest leads or 2 limb leads. The introduction of trombolitis is also considered justified when a blockade of the left leg of the bundle of His appears in
due to this anginal attack or in the presence of electrocardiographic signs of true posterior MI (high R waves in the right precordial leads and ST segment depression in leads V1–V4 with an upward R wave).
Absolute contraindications to thrombolytic therapy are:
1) previous hemorrhagic stroke or cerebrovascular accident of unknown etiology;
2)ischemic stroke within the last 3 months;
3)brain tumor, primary or metastases;
4)suspicion of aortic dissection;
5)the presence of signs of bleeding or hemorrhagic diathesis (with the exception of menstruation);
6)significant closed head injury within the last 3 months;
7)changes in the structure of cerebral vessels, such as arteriovenous malformation,
arterial aneurysms.
Thrombolytic drugs are injected into a peripheral (ulnar) vein. I recommend
The following schemes of introduction are given:
Streptokinase: 1,500,000 IU of the drug is dissolved in 100 ml of a 0.9% chloride solution
sodium and administered in 30 - 60 minutes.
Alteplase: the drug is dissolved in 100 - 200 ml of distilled water or 0.9% sodium chloride solution and 15 mg is administered by bolus, then 0.75 mg / kg drip for 30 minutes, then 0.50 mg/kg drip over 60 minutes (total dose not more than 100 mg).
93

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Tenecteplase: the drug is administered as a bolus - 30 mg with a patient weighing less than 60 kg,
35 mg with a body weight of 60 - 70 kg, 40 mg with a body weight of 70 - 80 kg, 45 mg with a body weight of 80 -
90 kg and 50 mg with body weight over 90 kg.
Purolase: the drug is dissolved in 100 - 200 ml of distilled water or 0.9% sodium chloride
solution and 2,000,000 IU is injected in a stream, then 4,000,000 IU drip for 30 – 60 min.
The effectiveness of thrombolysis can most accurately be assessed using coronary angiography. Indirect signs of reperfusion include: disappearance of anginal pain; rapid dynamics of the ECG (decrease in the ST segment in the most informative ECG lead by 50%
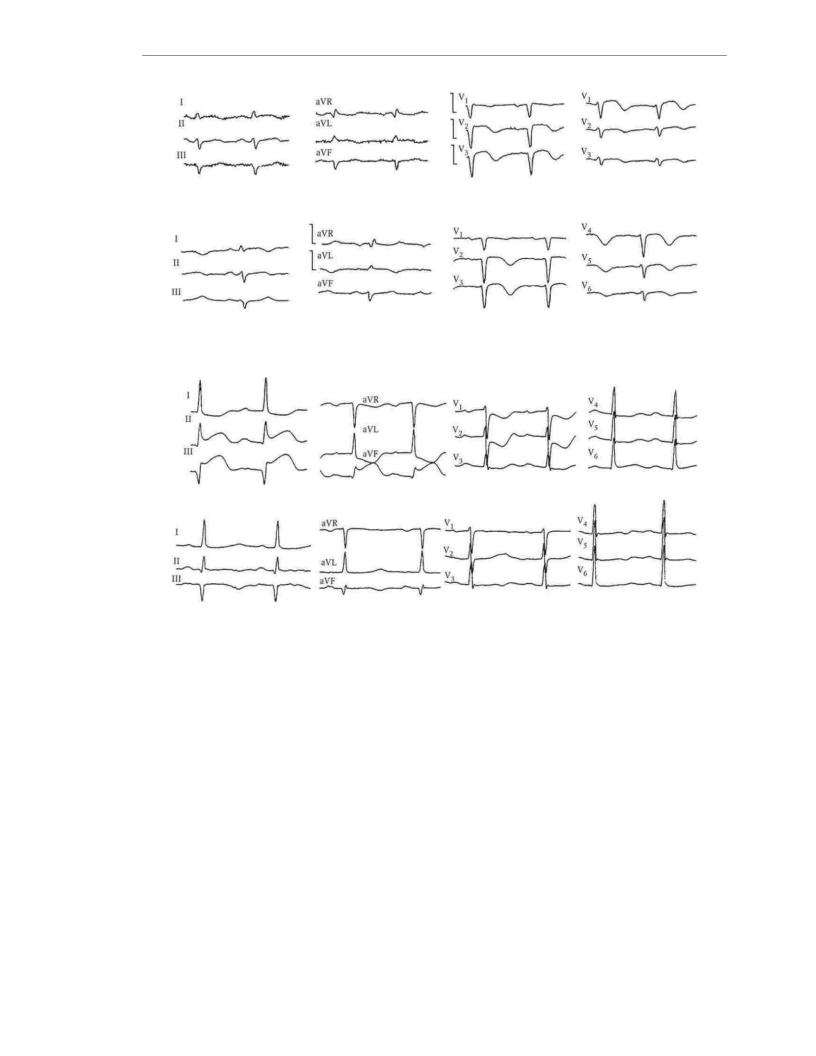
within 3 hours after thrombolytic administration); ventricular arrhythmias (often idioventricular rhythm) within 60–90 minutes after administration of a thrombolytic drug; early peak concentrations of biochemical markers of myocardial damage in the blood. ECG changes with effective thrombolysis in patients with MI are presented in fig. 1.11 - 1.12.
Prevention of coronary artery retrombosis after successful thrombolysis is ensured by the use of antiplatelet agents and anticoagulants. Regardless of which trombolic drug was used to restore coronary blood flow, all
in patients without contraindications, aspirin is indicated in combination with clopidogrel. Unfractionated heparin is the preferred treatment for patients who
streptokinase is introduced, enoxaparin - in the treatment of patients receiving fibrin-specific thrombolytics, fondaparinux is effective in combination with any thrombolytic drug and can be used in cases of heparin-induced thrombocytopenia.
Myocardial reperfusion in patients with acute coronary syndrome can be achieved
by percutaneous coronary balloon angioplasty (in most cases with vessel stenting). This method of treatment provides more frequent and more complete restoration of blood flow in the occluded artery, and eliminates residual stenosis.
coronary artery and reduce the risk of its rethrombosis, and also significantly less frequently than thrombolytic therapy, is complicated by hemorrhagic stroke. Emergency myocardial revascularization procedure is recommended for patients with acute coronary syndrome.
without ST-segment elevation if criteria for high immediate risk of death are met
or development of MI. In patients with ST-segment elevation acute coronary syndrome, percutaneous coronary balloon angioplasty is preferable in cases where from the first
contact with a healthcare professional prior to the first inflation of the balloon in the coronary artery
takes no more than 90 minutes. If the patient is admitted to the hospital no later than 3 hours from the appearance
symptoms of developing myocardial infarction, but the first inflation of the balloon in the coronary artery may be carried out 60 minutes after the start of thrombolytic administration, preference is given to
thrombolytic therapy. Percutaneous coronary balloon angioplasty can be performed instead of thrombolytic therapy and in cases where medication
did not lead to the restoration of coronary blood flow. The use of percutaneous coronary angioplasty is also acceptable in cases of successful thrombolytic therapy, if from the moment no more than 24 hours have passed since the patient sought medical help due to the appearance of clinical symptoms of MI. An invasive treatment strategy is considered inappropriate in patients with fully formed MI with pathological Q wave, no symptoms of ongoing ischemia of the heart muscle and signs of viable myocardium.
If coronary angiography reveals stenosis of the trunk of the left coronary artery or three-vessel lesion, especially in combination with left ventricular dysfunction, the optimal
coronary artery bypass grafting is the method of restoring blood flow.
94
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Rice. 1.11. ECG of a patient with anterolateral MI before (top row) and after (bottom row) effective thrombolytic therapy Diseases of the cardiovascular system
Rice. 1.12. ECG of a patient with inferior MI before (upper row) and after (lower row) effects active thrombolytic therapy
Hemodynamic and neurohumoral unloading of the heart in patients with acute coronary syndrome is provided by the use of ÿ- blockers, nitrates and inhibitors.
ACE.
The main theoretical prerequisites for the use of ÿ- blockers in therapy acute coronary syndromes are: a decrease in myocardial oxygen demand for
by reducing heart rate, blood pressure and negative inotropic action; weakening of the cardiotoxic effect of catecholamines; improvement of perfusion of subendocardial myocardium due to the lengthening of the diastole; antiarrhythmic action. In patients with hypertension, tachycardia, and persistent myocardial ischemia, the initial dose of ÿ- blockers can be administered intravenously, then they are switched to oral administration. Scheme of intravenous
administration of methoprolol: 5 mg for 5 minutes 3 times with an interval between injections of 5 minutes. The d oral intake is selected individually under the control of heart rate, blood pressure, the state of
AV conduction, the severity of symptoms of heart failure and manifestations of side effects of therapy. Nitrates cause peripheral vasodilation, dilatation of the epicardial coronary arteries and
coronary collaterals. Due to a decrease in intraventricular
pressure under the influence of nitrates improves blood supply and subendocardial
areas of the myocardium. An important property of nitrates is the redistribution of coronary
95

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
blood flow towards ischemic areas of the heart muscle. In patients with persistent pain or signs of left ventricular failure, nitrates are administered intravenously after sublingual use of nitroglycerin. The initial rate of nitroglycerin infusion is 5-10 µg/ min. Initial infusion rate
isosorbide dinitrate should not exceed 25 mcg/min. Every 5 - 10 minutes, the rate of administration is increased by 5 - 10 mcg / min under the control of the level of blood pressure and the patient's condition. Systolic blood pressure should not be reduced by more than 15% of baseline. Duration nitrate infusion usually does not exceed 24 hours. Subsequently, patients with persistent
episodes of anginal pain, nitrates are administered orally.
A prerequisite for the use of ACE inhibitors in the treatment of patients with MI is an important the role of activation of the renin-angiotensin system in the process of postinfarction heart remodeling. Taking into account the fact that the remodeling of the heart begins from the first day of the disease
and continues for many months, early administration and long-term use
ACE inhibitors as part of complex therapy for MI is considered reasonable for most patients. Unconditional indications for the use of ACE inhibitors are congestive heart failure and / or a decrease in the ejection fraction of the left ventricle. Treatment starts with small doses
ACE inhibitors, gradually increasing them to therapeutic. The recommended initial doses of drugs are: captopril - 25 mg / day, enalapril - 5 mg / day, perindopril - 2.5 mg / day, ramipril - 2.5 mg / day; lisinopril - 5 mg / day.
If the patient did not take statins before the development of acute coronary syndrome, treatment this class of drugs should be started as early as possible. Statins are prescribed in medium therapeutic doses to all patients who do not have contraindications. Target cholesterol level
LDL for this category of patients is 1.8 mmol/L.
The development of complications of myocardial infarction requires appropriate changes in pharmacotherapy and
changes in non-pharmacological methods of treatment.
The program of physical rehabilitation at the stage of inpatient treatment is compiled on
on the basis of assessing the belonging of a patient with MI to one of the 4 classes of severity of the condition. Determination of the severity class is carried out on the 2nd - 3rd day of the disease after the relief of
pain and complications such as cardiogenic shock, pulmonary edema, severe arrhythmias.
When determining the severity class, the depth and extent of myocardial damage are taken into account, the presence and nature of complications, the severity of coronary insufficiency. Therapeutic gymnastics begins from the 2nd - 3rd day of illness in all categories of patients. Each activity level corresponds to a set of exercises designed taking into account the physical capabilities of the patient. The transition to each subsequent set of exercises is carried out in
depending on the severity class and individual tolerance of physical activity.
Prevention. Prevention of exacerbations of coronary artery disease in patients after myocardial infarction involves a non-drug effect on modifiable risk factors (smoking, hypertension, dyslipidemia, overweight, physical inactivity, etc.) and prolonged use
4 classes of drugs with a proven positive effect on the prognosis: antiplatelet agents, ÿ- blockers, ACE inhibitors and statins.
96

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
1.5. INFECTIOUS ENDOCARDITIS
Definition. Infective endocarditis is an inflammatory disease in which
an infectious agent circulating in the blood affects the valves of the heart, the parietal endocardium and the endothelium of the main vessels, which is accompanied by general infectious-toxic manifestations and damage to the internal organs of thromboembolic, hemorrhagic
chemical and immunocomplex character.
Prevalence. Information about the prevalence of infective endocarditis
contradictory. According to various sources, the incidence ranges from 10 to 60 cases per 1 million person per year. In large cities of the USA, Western Europe and the Russian Federation,
80-150 cases of infective endocarditis are registered per 1 million people per year. In the last 10
– 15 years, the incidence of infective endocarditis has increased markedly due to an increase in number of patients undergoing heart surgery and invasive diagnostic and
therapeutic nature, as well as in connection with the increase in the number of "intravenous" drug addicts.
More than 70% of cases of infective endocarditis are diagnosed in people aged 31
up to 60 years old. Men suffer from infective endocarditis 2-3 times more often than women. Most predisposed to infective endocarditis are patients with heart diseases: acquired and
congenital heart defects, mitral valve prolapse, previously suffered infective endocarditis, as well as patients who have undergone prosthetic surgery
heart valves and other cardiac surgery.
Etiology. Inflammation of the endocardium can be caused by various microorganisms (including including anaerobes), but the main causative agents of infective endocarditis are staphylococci (30-50% of cases) and streptococci (20-40% of cases).
Staphylococci (more often S. aureus) are commonly found in the blood of patients who have the development of infective endocarditis is associated with the performance of invasive instrumental studies, the use of intravenous catheters, the implantation of an artificial driver
rhythm, purulent diseases, as well as drug addicts. Streptococci (usually Str. viridians) are usually the causative agents of infective endocarditis in patients who have undergone surgical interventions in the oral cavity, tonsillitis, pharyngitis and sinusitis. infectious Enterococcal endocarditis is often preceded by tooth extraction, urogenital infection, adenomectomy, induced abortion, and other gynecological interventions. Gram-negative
microorganisms (Pseudomonas aeruginosa, Salmonella, Enterobacteriaceae), pathogens of the NASEC group (this abbreviation denotes
representatives of the genus Haemophilus influenzae), as well as fungi, usually cause infectious endocarditis in patients undergoing cardiac surgery, patients who received infusion therapy
for a long time using catheters inserted into the center
veins, and drug addicts.
In 8-10% of patients with infective endocarditis, blood cultures reveal
several pathogens. The increase in the number of cases of polymicrobial infective endocarditis is associated with the widespread and often unjustified use of antibiotics, the spread of drug addiction, and immunosuppressive conditions. In 10-30% of patients with infectious endocarditis fails to identify the pathogen even with repeated blood tests due to
with the preliminary prescription of antibiotics, the use of insensitive nutrient media in laboratories, and for other reasons - in these cases, the etiology of the disease remains unrecognized.
Pathogenesis. Infective endocarditis develops as a result of the interaction of three main factors: bacteremia, endothelial damage and weakening of organ resistance
nism.
97

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Short-term bacteremia occurs quite often in connection with the extraction of teeth, various inflammatory diseases (tonsillitis, sinusitis, furunculosis, etc.),
surgical interventions on the heart, abdominal organs, urinary tract, intravenous injections, invasive instrumental studies (cystoscopy, gastroscopy,
bronchoscopy, etc.). In a healthy body, due to the mechanisms of macrophage and capillary-tissue protection, the destruction of the infectious agent occurs quickly. Endothelium that covers the valves of the heart and endovascular surfaces
normal prevents the fixation of microorganisms. Damage to the endothelium is facilitated
by hemodynamic and blood flow disorders that occur with heart defects (especially in the presence of high pressure gradient between two chambers), mechanical effects associated
with cardiac surgery and vascular catheterization, as well as metabolic disorders, toxic effects and other factors. Local property violations
of the endothelium cause increased adhesion, platelet aggregation and stimulate the processes of local hemocoagulation, as a result of which wall microthrombi are formed at the sites of damage to the endothelium - non-bacterial thrombotic endocarditis develops. At transient bacteremia, loose thrombotic masses serve as a favorable environment for
settling and colonization of microorganisms. Transformation of non-bacterial endocarditis into infectious contribute to the invasiveness of microorganisms (i.e. increased adhesiveness
and resistance to the effects of protective mechanisms), as well as a decrease in the reactivity of the patient'sbody, which occurs under the influence of overwork, hypothermia, malnutrition, long-term illnesses, prolonged therapy with glucocorticoids and antibiotics.
The formation of antigens, caused by infective endocarditis, both directly by the infectious agent and by the products of tissue decay, causes the active production of antibodies. Along with high antibody titers, in the blood of a patient with infectious endo
carditis, the complement content decreases and the number of circulating
immune complexes. Immunopathological reactions lead to the development of aseptic myopericarditis, glomerulonephritis, vasculitis and dystrophic changes in internal organs.
Morphology. Typical morphological feature of infective endocarditis
is the formation of erosions, ulcerations and polypous infected formations (vegetations) on the surface of the valve, ranging in size from 2–5 to 15–20 mm. Often there are
perforations and tears of the valve leaflets, ruptures of chords, abscesses in the area of the valve rings a myocardium. Polyposis-ulcerative changes can also spread to the parietal endocardium,
leading to the formation of fistulas in the interventricular septum. With an infectious prosthetic valve endocarditis, the main changes occur in the tissues of the annulus fibrosus, where a paravalvular fistula can form.
Histological examination of the affected valve usually reveals necrotic tissues, vegetations consisting of fibrin, platelets, histiolimphocytic
elements, colonies of microorganisms. The presence of microbial colonies in thrombotic masses indicates active infective endocarditis. Against the background of antimicrobial treatment, the damaged valve and vegetations are fibrosed, hyalinized, calcified,
often covered by endothelium. Examination of the vascular wall and kidneys reveals deposits of immune complexes in the subendothelium and mesangium with secondary proliferative-inflammatory and necrotic changes. The course of infective endocarditis is often complicated by vegetation fragmentation. In this regard, during a morphological study with thromboembolism of the arteries of the large and small circles of blood circulation with the formation of infarcts of the corresponding organs are detected at a high frequency.
98
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
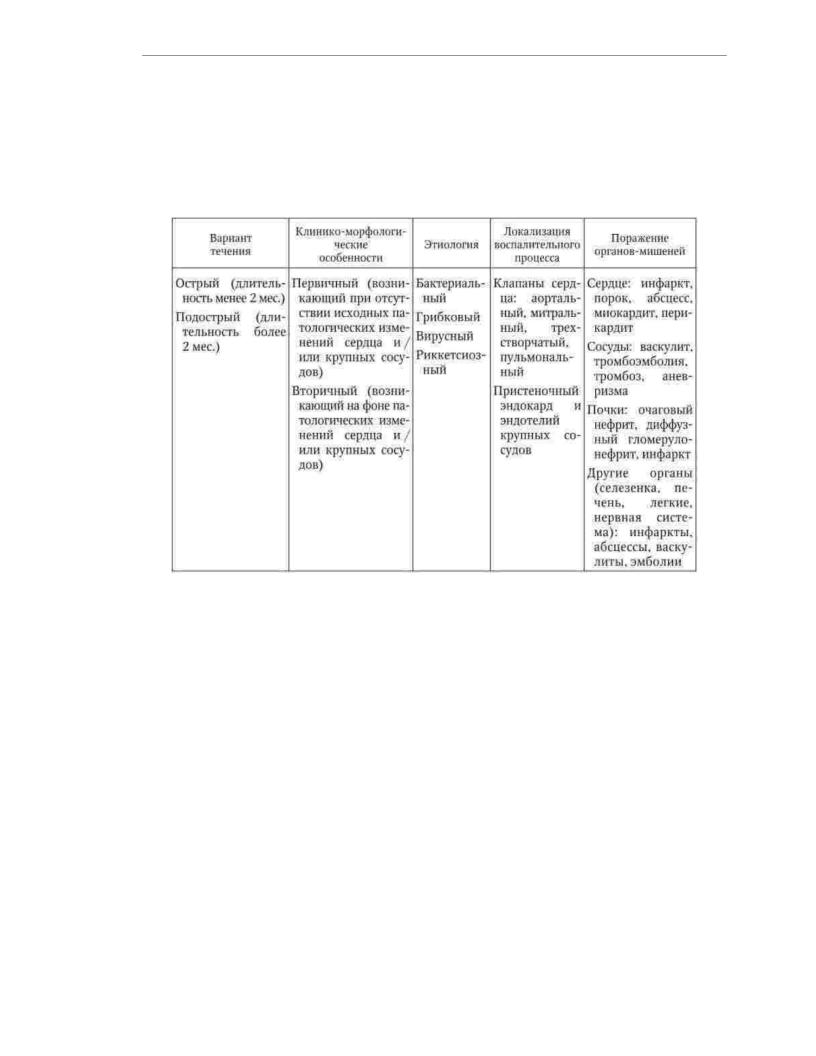
Classification. The clinical classification of infective endocarditis reflects the course options, clinical and morphological features, etiology, predominant localization of the inflammatory process, and the nature of target organ damage (Table 1).
1.25).
Table 1.25
Classification of infective endocarditis
Acute is called infective endocarditis, the duration of clinical manifestations
which does not exceed 2 months, subacute - infective endocarditis, the symptoms of which appeared for more than 2 months. back. Relapses of infective endocarditis, depending on the timing of their occurrence, are divided into early (occurred within 2–3 months after
completion of treatment) and late (occurred in the range from 2–3 months to 1 year after completion of tr treatment). However, the concept of "chronic recurrent infective endocarditis"
is controversial because early relapses tend to be the result of mistakes
diagnosis and treatment of acute or subacute infective endocarditis, i.e., the continuation of an untreated disease, and late relapses (especially if they occur after
year or more) are often a manifestation of a new infective endocarditis that has developed against the background of heart disease and caused by another pathogen. Primary
infective endocarditis develops in patients with intact heart and blood vessels, secondary infectious endocarditis - in patients with heart defects, prolapse of the valve leaflets, anomalies of
large arteries, prostheses of valves and large vessels, after heart surgery. According to the etiology, infective endocarditis is divided into bacterial, fungal, viral, rickettsial. In addition, there are forms of the disease caused by microbial coalitions, and
also infective endocarditis with negative blood culture. Inflammatory process with infective endocarditis, it can be localized on the heart valves, parietal
endocardium and endothelium of large vessels. Among the target organs that are affected by infective endocarditis include the heart, blood vessels, kidneys, liver, spleen, lungs,
nervous system. The main reasons for the development of morphological and functional changes
99

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
internal organs in infective endocarditis are inflammation (including
with the formation of an abscess), thromboembolism, hemorrhage, heart attacks.
In connection with clinical expediency, special forms of infectious diseases are distinguished. endocarditis, which include infective endocarditis of artificial valves,
infective endocarditis in patients on program hemodialysis, infective endocarditis of transplanted heart valves, infective endocarditis of drug addicts, infective endocarditis in elderly and senile patients.
clinical picture. The clinical manifestations of infective endocarditis are varied. The symptomatology of the disease is determined by many factors, the main ones
which are the virulence of the pathogen microbe, the severity of immunopathological reactions, the localization and degree of damage to the heart valves and target organs, the nature of thromboembolic complications.
Symptoms of infective endocarditis usually appear after 1 to 2 weeks. after episodes of bacteremia. For primary infective endocarditis caused by a highly virulent pathogen (staphylococcus, enterococcus, gram-negative bacteria),
characterized by an acute onset with chills, high fever (up to 39–40 °C), profuse cold sweat. The gradual development of clinical symptoms with progressive malaise, general weakness, loss of appetite, weight loss, subfebrile temperature is more typical for secondary infective endocarditis, as well as for patients
with reduced reactivity and in cases where the disease is caused by a low-virulence pathogen. In some cases, the first manifestation of infective endocarditis is cerebral embolism with the development of hemiplegia, hemiparesis, aphasia, or retinal vessels, which manifests itself as sudden blindness.
When examining a patient with infective endocarditis, pallor of the skin is often noted. In
20 - 40% of patients, petechiae are detected on the mucous membrane of the cheeks, gums, conjunctiva (Lukin-Libman spots), subungual hemorrhages and small hemorrhagic rashes on
palms and feet (Janway spots). For acute staphylococcal infective endocar
dita is characterized by a large hemorrhagic rash and hemorrhages in the skin of the fingers and toes
with the development of necrosis. In 3-5% of cases of infective endocarditis, retinal hemorrhages with a white center (Roth spots) are detected. For infective endocarditis subacute course is characterized by the appearance of small painful nodules on the fingers, caused by microvascular septic emboli (Osler'snodes).
Most patients with infective endocarditis present with tachycardia, cardiomegaly, and symptoms of congestive heart failure (peripheral edema, moist
wheezing in the lungs, hepatomegaly). The appearance of a new heart murmur (diastolic and/or systolic) due to the formation of valvular disease is observed in more than 80%
sick. Intravenous drug addicts are characterized by damage to the tricuspid valve.
In the event of gross anatomical disorders (perforation or separation of the valve leaflet, rupture of the chord), heart murmurs appear or change suddenly. half
patients noted arthralgia, myalgia, splenomegaly. Manifestations of myocarditis, pericarditis
and thromboembolism (in the brain, kidneys, heart, lungs and other organs, often with subsequent abscess formation) are observed in 10-20% of patients.
Criteria for the likelihood of infective endocarditis, proposed by the experts of the European Society of Cardiology (2003):
High probability of IE (echocardiography for emergency indications and hospitalization is indicated):
1)new murmurs of regurgitation;
2)embolism of unknown nature (especially cerebral and renal arteries);
3)sepsis with an unknown source;
100
