
Cardiology / English / ГБ на английском языке для иностранцев
.pdfPhysical examination for secondary hypertension:
•Features of Cushing syndrome
•Skin stigmata of neurofibromatosis (pheochromocytoma)
•Palpation of enlarged kidneys (polycystic kidney)
•Auscultation of precordial or chest murmurs (aortic coarctation; aortic disease; upper extremity artery disease)
•Diminished and delayed femoral pulses and reduced femoral blood pressure compared to simultaneous arm BP (aortic coarctation; aortic disease; lower extremity artery disease)
•Left-right arm BP difference (aortic coarctation; subclavian artery stenosis)
Secondary Hypertension:
1.Renal disease: any disease of the renal parenchyma can cause hypertension, and these conditions are the most common causes of secondary hypertension. Hypertension may result from glomerular diseases, tubular interstitial disease, and polycystic kidneys. Diabetic nephropathy is another cause of chronic hypertension.
2.Renal vascular hypertension: it is due to artery stenosis, fibromuscular hyperplasia, and atherosclerotic stenoses.
It should be suspected in the following circumstances: (1) if the documented onset is below age 20 or after age 50; (2) if there are epigastric or renal artery bruits; (3) if there is atherosclerotic disease of aorta or peripheral arteries; or (4) if there is abrupt deterioration in renal function after administration of angiotensin-converting enzyme inhibitors. 3. Эндокринные: Primary hyperaldosteronism and Cushing’s syndrome: the diagnosis should be suspected when patients present with hypokalemia prior to diuretic therapy associated with excessive urinary potassium excretion, increased serum
sodium, and suppressed levels of plasma renin activity. Aldosterone concentrations in urine and blood are elevated. The lesion can be demonstrated by CT scanning or MRI. Pheochromocytoma: although hypertension due to pheochromocytoma may be episodic, most patients have sustained elevations. The majority of patients have orthostatic falls in blood pressure, the converse of essential hypertension; some develop glucose intolerance.
Acromegaly, hyperthyroidism, hypothyroidism and other causes.
4.Neurogenic secondary hypertension: variety of neurologic disorders causing increased intracranial pressure.
5.Hemodynamic secondary hypertension: aortic atherosclerosis, coarctation aorta, open aortic duct, aortic insufficiency valve and etc.
6.Exogenous secondary hypertension: associated with the use of contraceptives containing estrogens, glucocorticoids, nonsteroidal anti-inflammatory drugs, catecholamines, amphitamines, sympathomimetics, tricyclic antidepressants, monoamine oxidase inhibitors.
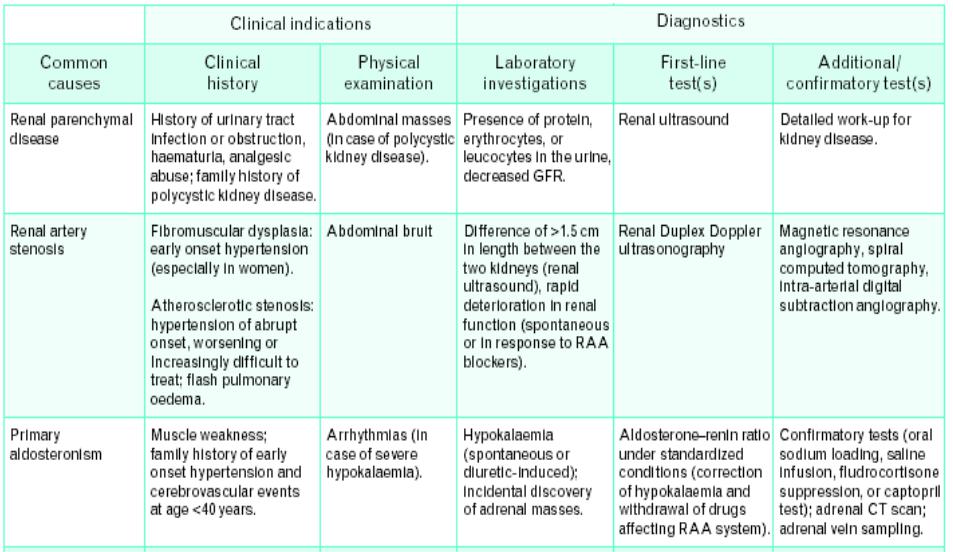
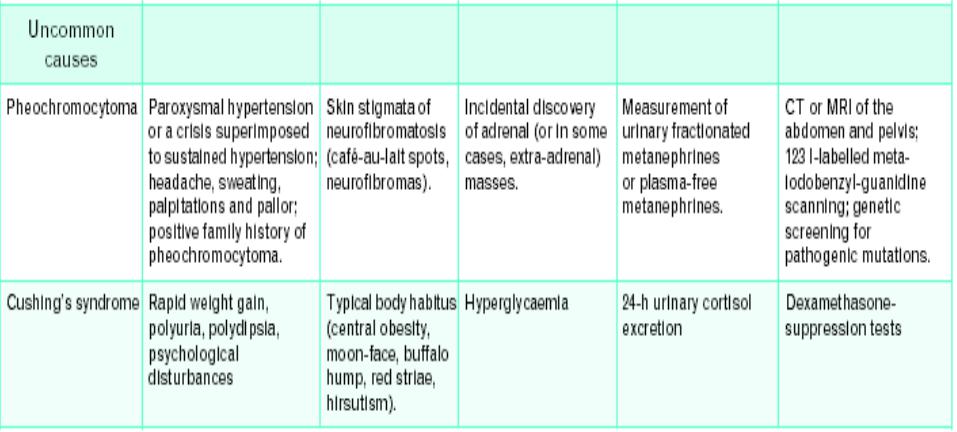
Clinical indications and diagnostics of secondary hypertension:
(CT, computed tomography; GFR, glomerular filtration rate; MRI, magnetic resonance imaging; RAA, renin-andiotensin-aldosterone):
Hypertensive crisis:
an acute increase in blood pressure to high values for a given individual, accompanied by a deepening of the existing symptoms of hypertension or the appearance of new signs.
Etiology:
Psychoemotional stress, a sharp change in atmospheric pressure and weather, cancellation of certain medications unauthorized by the doctor, pregnancy pathology, acute renal pathology, pheochromacytoma, etc.
Classification of hypertensive crises: complicated and uncomplicated:
HA is considered complicated in the following cases:
•hypertensive encephalopathy;
•cerebral stroke;
•OKS; acute LV failure;
•dissecting aortic aneurysm;
•HA for pheochromocytoma;
•preeclampsia of pregnant women;
•severe hypertension associated with subarachnoid hemorrhage or brain injury;
•AH in postoperative patients and with the threat of bleeding;
•HA while taking amphetamines, cocaine, etc..
Urgent care:
Blood pressure should be reduced gradually, in order to avoid deterioration of blood supply to the brain, heart and kidneys, as a rule, by no more than 25% in the first 1–2 hours. The most rapid decrease in blood pressure is necessary with dissecting aortic aneurysm (by 25% of the initial value in 5– 10 minutes, as well as with severe acute LV failure (pulmonary edema).
With complicated HA - a rapid decrease in blood pressure by 15-20% of the initial within an hour.
Parenteral drugs:
ACE inhibitors:
-enalaprilat (with acute LV failure); Nitrates:
-nitroglycerin (with ACS and acute LV failure);
-sodium nitroprusside (it is the drug of choice for hypertensive encephalopathy, but it should be borne in mind that it can increase intracranial pressure). Alpha blocker:
-Urapedil (ebrantil) (refractory crisis, hypertension) Diuretics (furosemide for acute LV failure).
β-AB (propranolol, metoprolol, esmolol are preferred for dissecting aortic aneurysm and ACS). Antipsychotics (droperidol).
Ganglion blockers (pentamine).
Antiadrenergic drugs (phentolamine if pheochromocytoma is suspected). Magnesium sulfate IV (during pregnancy,
cerebrovascular accident, convulsive syndrome)
