
English Lectures / Functional chemistry 1 eng
.pdf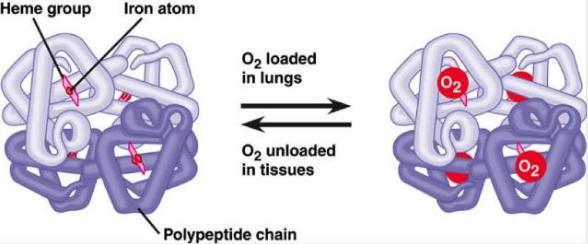
Blood oxygen transport
•When an oxygen molecule interacts with one of the 4 hemoglobin hemes, oxygen joins one of the halves of the hemoglobin molecule. As soon as such an attachment occurs, the α- polypeptide chain undergoes conformational changes that are transmitted to the β-chain that is closely related to it; the latter also undergoes conformational shifts.
•The β-chain attaches oxygen, having already a greater affinity for it. In this way, the binding of 1 oxygen molecule favors the binding of the second molecule. After oxygen saturation of one half of the hemoglobin molecule, a new, internal, stressed state of the hemoglobin molecule appears, which forces the second half of hemoglobin to change the conformation. Now 2 more oxygen molecules in turn bind to the second half of the hemoglobin molecule, forming oxyhemoglobin.

Blood Carbon Dioxide Transport
The body has several mechanisms for the transfer of CO from tissues to the lungs. Part of it is transferred in a physically dissolved form. A certain amount of CO can be transported in the form of a carbamic form. It turned out that CO can bind to hemoglobin via a carbamine bond, forming carbhemoglobin.
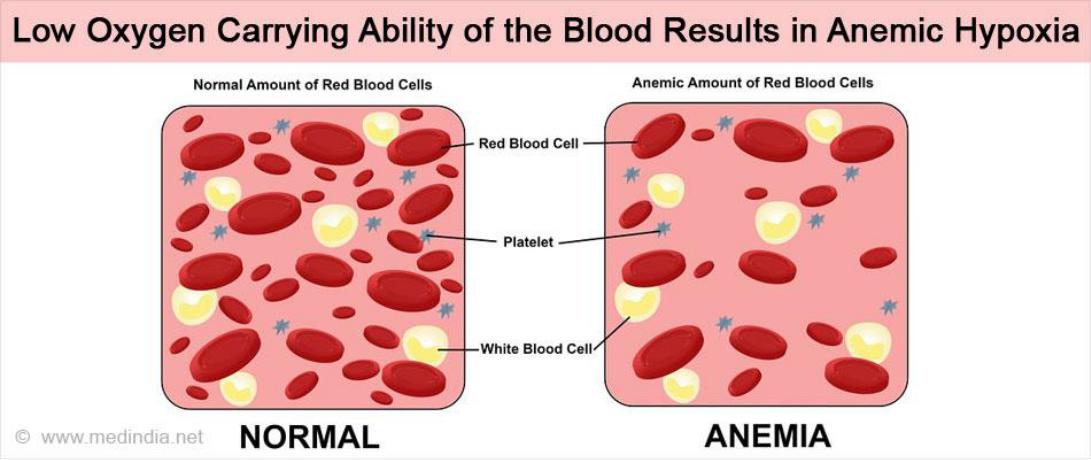
Anemic hypoxia
Anemic hypoxia occurs when there is not enough hemoglobin in the blood, resulting in a decrease in the total amount of oxygen.
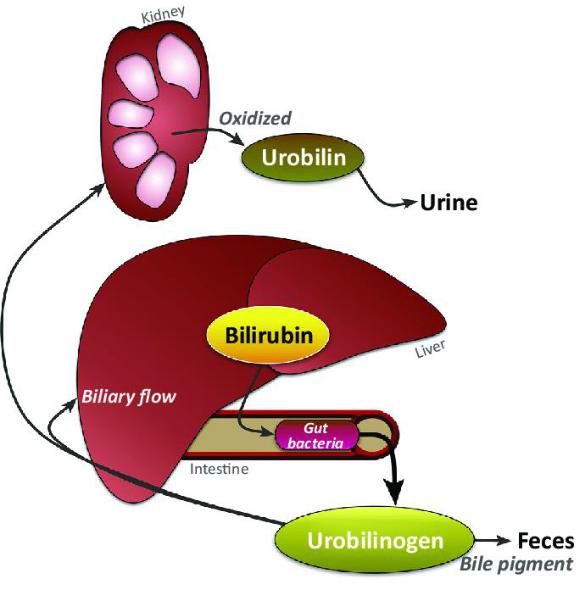
Bilirubin
Bilirubin is a bile pigment, one of the main components of bile in the human and animal body. It is formed normally as a result of the breakdown of proteins containing heme: hemoglobin, myoglobin and cytochrome.
Let’s write!
Bilirubin functions
Bilirubin is formed by the enzyme biliverdin reductase from biliverdin, a green pigment, which is also the product of the breakdown of heme. Once oxidized, bilirubin can be converted back to biliverdin. This cycle of reactions has led to the hypothesis that bilirubin is the main cellular antioxidant.
Normally, the content of total bilirubin in blood serum ranges from 1.7- 20.5 μmol / L, 75% falls on "indirect" bilirubin, it is sometimes called "free".
Bilirubin forms
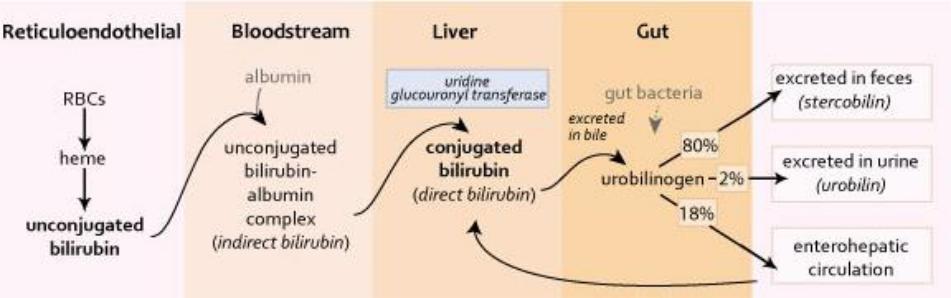
•About 96% of bilirubin in human blood is represented by non-polar insoluble indirect bilirubin, which forms complexes with albumin.
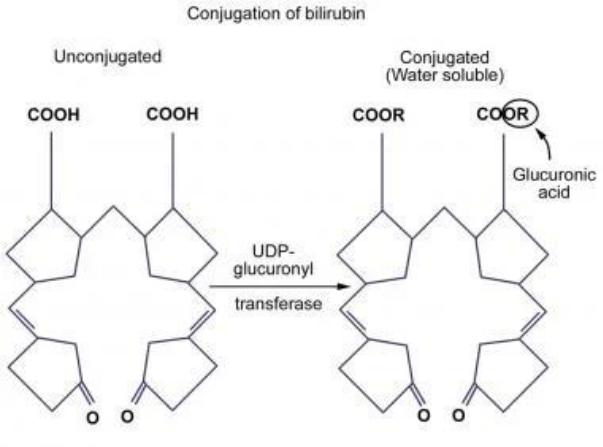
•The remaining 4% of bilirubin binds to various polar molecules, mainly with glucuronic acid. In this case, direct bilirubin is formed, which is soluble in water, filtered by the kidneys and excreted in the urine.
Bilirubin toxicity
Unconjugated bilirubin is toxic. Hydrophobic, lipophilic unconjugated bilirubin, easily dissolving in the lipids of cell membranes and penetrating into the mitochondria as a result, dissociates respiration and oxidative phosphorylation in them, disrupts protein synthesis, the flow of potassium ions through the cell membrane and organelles. This adversely affects the state of the nervous system, causing a number of characteristic neurological symptoms in patients. It can penetrate the blood-brain barrier when its concentration in blood plasma exceeds the saturation level of high-affinity sections of albumin (20-25 mg/100 ml).

Jaundice
Jaundice is usually associated with a violation of its formation and excretion, which leads to its accumulation in the blood - bilirubinemia and causes the color of the sclera, skin, mucous membranes in yellow.
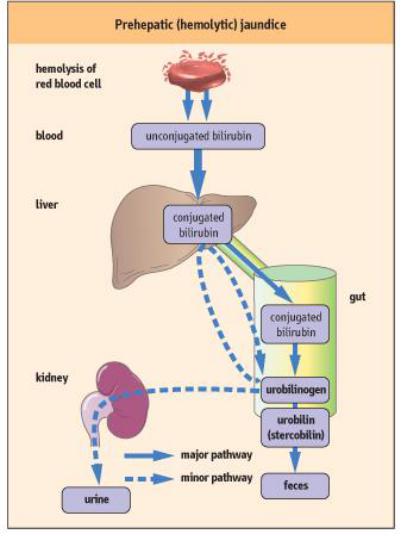
1) Hemolytic (pre-hepatic) jaundice
This jaundice develops with increased decay of red blood cells in the cells and the formation of a large amount of indirect bilirubin. Jaundice, as a result of bilirubinemia, develops because the liver does not have time to process all of the indirect bilirubin. Manifestations of the pathology: blood - a lot of indirect bilirubin; feces - intensely colored in yellow, it contains a lot of stercobilin; urine - a lot of urobilin.
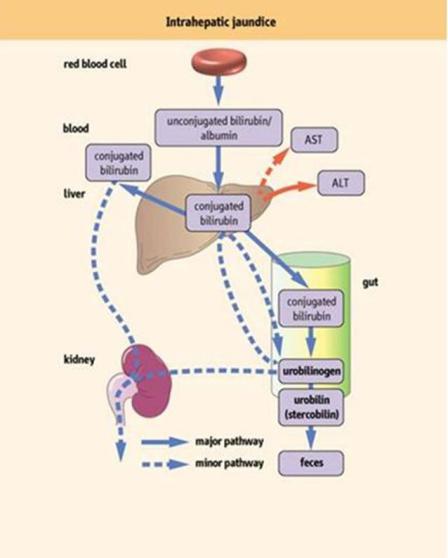
2) Hepatocellular (hepatic) jaundice
As a result of a violation of the capture of bilirubin and its conjugation with glucuronic acid and excretion. It is noted with damage to hepatocytes and, consequently, a decrease in liver function, which is why even the usual amount of extrahepatic bilirubin is not processed direct bilirubin. Manifestations of pathology: feces - pale colored, little bile, little stercobilin. Urine - little urobilin. Blood - an increase in indirect bilirubin. Parenchymal jaundice is often noted in viral hepatitis; hepatosis - toxic damage to the liver by poisonous mushrooms, medicines, salts of heavy metals, carbon tetrachloride, during pregnancy and enzymes.
