
Auscultation of lungs, main and adventitious respiratory sounds
Auscultation: Prior to listening over any one area of the chest, remind yourself which lobe of the lung is heard best in that region: lower lobes occupy the bottom 3/4 of the posterior fields; right middle lobe heard in right axilla; lingula in left axilla; upper lobes in the anterior chest and at the top 1/4 of the posterior fields. This can be quite helpful in trying to pin down the location of pathologic processes that may be restricted by anatomic boundaries (e.g. pneumonia). Many disease processes (e.g. pulmonary edema,bronchoconstriction) are diffuse, producing abnormal findings in multiple fields.
auscultation of lungs
1. Put on your stethoscope so that the ear pieces are directed away from you. Adjust the head of the scope so that the diaphragm is engaged. If you're not sure, scratch lightly on the diaphragm, which should produce a noise. If not, twist the head and try again. Gently rub the head of the stethoscope on your shirt so that it is not too cold prior to placing it on the patient's skin.
2. The upper aspect of the posterior fields (i.e. towards the top of the patient's back) are examined first. Listen over one spot and then move the stethoscope to the same position on the opposite side and repeat. This again makes use of one lung as a source of comparison for the other. The entire posterior chest can be covered by listening in roughly 4 places on each side. Of course, if you hear something abnormal, you'll need to listen in more places.
3. The lingula and right middle lobes can be examined while you are still standing behind the patient.
4. Then, move around to the front and listen to the anterior fields in the same fashion. This is generally done while the patient is still sitting upright. Asking female patients to lie down will allow their breasts to fall away laterally, which may make this part of the examination easier.

Listen to the respiratory rate, including rhythm and depth of respirations. Compare rate with normal respiratory rates for the age of the client.
Auscultate the lungs, listening to inspiration and expiration at each site.

Auscultate the anterior lung fields. Listen for abnormal sounds, including rales, rhonchi, or wheezes.
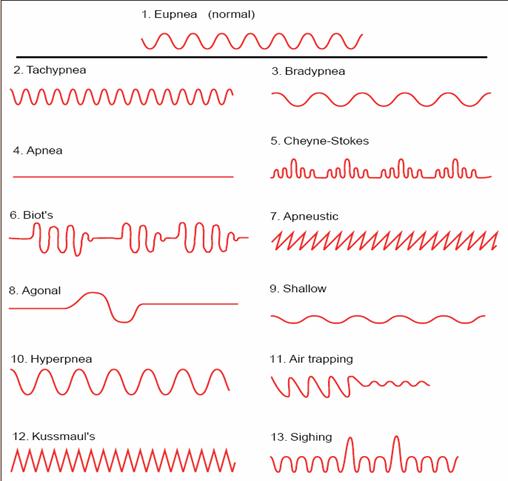
Normal and abnormal respiratory patterns
A few additional things worth noting.
1. Don't get in the habit of performing auscultation through clothing.
2. Ask the patient to take slow, deep breaths through their mouths while you are performing your exam. This forces the patient to move greater volumes of air with each breath, increasing the duration, intensity, and thus detectability of any abnormal breath sounds that might be present.
3. Sometimes it's helpful to have the patient cough a few times prior to beginning auscultation. This clears airway secretions and opens small atelectatic (i.e. collapsed) areas at the lung bases.
4. If the patient cannot sit up (e.g. in cases of neurologic disease, post-operative states, etc.), auscultation can be performed while the patient is lying on their side. Get help if the patient is unable to move on their own. In cases where even this cannot be accomplished, a minimal examination can be performed by listening laterally/posteriorly as the patient remains supine.
5. Requesting that the patient exhale forcibly will occasionally help to accentuate abnormal breath sounds (in particular, wheezing) that might not be heard when they are breathing at normal flow rates.
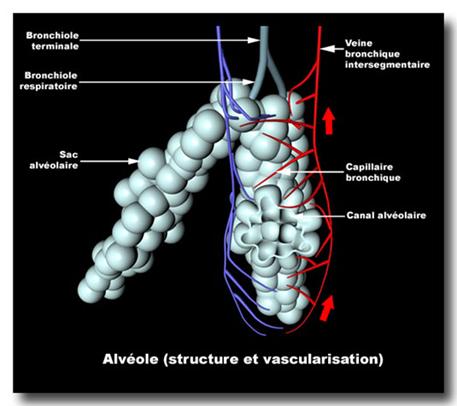
In thin bony chests, the bell may give a more airtight fit and is less likely to trap hairs underneath, which produce a crackling sound. The breath sounds are produced in the large airways, transmitted through the airways and then attenuated by the distal lung structure through which they pass. The sounds you hear at the lung surface are therefore different from the sounds heard over the trachea and are modified further if there is anything obstructing the airways, lung tissue, pleura or chest wall. When reporting on auscultatorychanges, you must distinguish between the breath sounds and the added sounds. Breath sounds are termed either vesicular or bronchial and the added sounds are divided into crackles, wheezes and rubs.
Vesicular breathing sounds
The breath sounds are produced in the large airways, transmitted through the airways and then attenuated by the distal lung structure through which they pass.

The sounds you hear at the lung surface are therefore different from the sounds heard over the trachea and are modified further if there is anything obstructing the airways, lung tissue, pleura or chest wall. When reporting on auscultatory changes, you must distinguish between me breath sounds and thVaddcd sounds. Breath sounds arc- termed either vesicular or bronchial and the Vesicular breath sounds This is the sound heard over normal lungs, it has a rustling quality and is heard on inspiration and the first part of expiration .Reduction in vesicular breath sounds can be expected with airways obstruction as in asthma, emphysema or tumour. The so-called 'silent chest' is a sign of severe asthma: so little air enters the lung that no sound is produced. The breath sounds can be strikingly reduced in emphysema, particularly over a bulla. Generalised reduction in breath sounds also occurs with a thick chest wall or obesity. Anything interspersed between the lung and the chest wall (air, fluid or pleural thickening) will reduce the breath sounds: this is likely to be unilateral and therefore more easily detected. Avoid the term 'diminished air entry' when you mean diminished breath sounds. The two are not necessarily synonymous.
Bronchial breathing
Bronchial breathing causes much confusion because the essential feature of bronchial breathing, the quality of the sound, is difficult or impossible to put into words. Traditionally, it is described by its timing as occurring in both inspiration and expiration with a gap in between. The diagram of bronchial breath sounds is:

In this way it is contrasted with vesicular breathing. These features are undoubtedly true but lead to the confusion in the mind of the student that if anything is heard in middle or late expiration it must be bronchia] breathing. Many normal people and individuals with airways obstruction have prolonged expiratory component to the breath sounds (this is sometimes designated “bronchovesicular” but this term increases the confusion rather than diminishing it). It is best to forget about the timing and concentrate on the essential feature, the quality of the sound. It can be mimicked to some extent by listening over the trachea with the stethoscope, although a better imitation can be obtained by putting the tip of your tongue on to roof of your mouth and breathing in and out through the open mouth. Bronchial breathing is heard when sound generated in the Central airways is transmitted more or less unchanged through the lung substance. This occurs when the lung substance itself is solid as in consolidation but the air passages remain open. Sound is conducted normally to the small airways but then instead of being modified by air in the alveoli, the solid lung conducts the sound better to the lung surface and, hence, to the stethoscope. If the central airways are obstructed by say a carcinoma, then no transmission of sound will take place and no bronchial breathing will occur even though the lung may be solid. An exception is seen in the upper lobes. Here, if the bronchi to either lobe are blocked, sounds from the central airways can still be transmitted directly from die trachea through the solid lung to the chest wall.
The main cause of bronchial breathing is consolidation particularly from pneumonia, so much so that in the minds of most clinicians the three terms are synonymous. Lung abscess, if near the chest wall, can cause bronchial breathing probably because of the consolidation around it. Dense fibrosis is an occasional cause. Breath sounds over an effusion will be diminished but bronchial breathing may be heard over its upper level perhaps because the effusion compresses the lung. Bronchial breathing is only heard over a collapsed lung if the airway is patent. This is rare as the collapse is usually caused by an obstructing carcinoma. Nevertheless, there is an exception with the upper lobes (see above). Bronchial breathing has been divided into tubular, cavernous and amphoric but attempts to score points on ward rounds by using these terms are best left to others.
