
- •Other titles in the series include:
- •Overcoming chronic pain a self-help manual using Cognitive Behavioral Techniques frances cole, helen macdonald, catherine carus and hazel howden-leach
- •Isbn: 978-1-84119-970-2 eIsbn: 978-1-47210-573-8
- •Table of contents
- •Acknowledgements
- •Foreword
- •Introduction by Peter Cooper Why cognitive behavioral?
- •Introduction
- •Who might benefit from using this book?
- •What does chronic pain mean?
- •What is Cognitive Behavioral Therapy?
- •How can a book help?
- •How can I get the most out of using this book?
- •What do the chapters cover?
- •How do I start using this book?
- •Four case histories
- •Using the person-centred model
- •Maria and the person-centred model
- •How did the model help Maria make changes for the better?
- •How can the person-centred model help you get ready tomake some changes?
- •Getting started
- •Reducing the impact of pain on your daily life
- •How do you or others see these changes occurring?
- •Understanding chronic pain and pain systems
- •Understanding pain
- •Acute and chronic pain
- •What is acute pain?
- •What is chronic pain?
- •Acute and chronic pain systems
- •The acute pain system
- •The chronic pain system
- •Theories of pain The Gate Control Theory of Pain
- •Other theories of pain
- •Frequently asked questions
- •Understanding investigations for pain
- •Blood tests
- •Waiting for tests and results
- •Understanding the roles of healthcare professionals
- •Healthcare professionals
- •What is the role of a physiotherapist?
- •How do physiotherapists work?
- •What is the role of a specialist pain nurse?
- •What is the role of a pain specialist?
- •What is the role of a psychologist?
- •What is the role of a psychiatrist?
- •Talking therapies
- •Cognitive Behavioral Therapy
- •Pain management programmes
- •Understanding medicines and using them better
- •What types of medicines are used to manage chronic pain?
- •How are medicines used? Analgesics
- •Problems with medicines
- •Making better use of medicines
- •Four suggestions for using medications more helpfully
- •Stopping or reducing your medicines
- •Part two Overcoming Chronic Pain
- •Introduction
- •Setting goals
- •What are goals?
- •Informal and formal goals
- •What are smart goals?
- •Setting goals
- •Using a goal ladder
- •Achieving your goals
- •Giving yourself rewards
- •What are rewards?
- •Creating a ‘fun presciption’
- •50 Mg of fun three times a day (at least) For maximum benefit, use imagination!
- •Understanding pacing skills
- •What is pacing?
- •What are the different styles of pacing?
- •What type of pacing style do you use at present?
- •If pain levels are low, do you:
- •If pain levels are high, do you:
- •How to change your pacing style
- •Experimenting
- •Planning
- •Priorities
- •How to deal with barriers to realistic pacing
- •Getting fitter and being more active
- •How being more active can help you manage your pain
- •Trying to get fitter: What does having more pain mean?
- •Why do these types of activity cause aches and pains?
- •Assessing your present activity level
- •Frequently asked questions about increasing physical activity
- •How to get started on a basic exercise programme
- •Strength exercises – do slowly
- •Stretches for flexibility
- •Understanding problem-solving
- •What is problem-solving?
- •The main steps in problem-solving
- •Putting the problem-solving process into practise
- •Problem-solving guide
- •Understanding sleep and sleep problems
- •What sort of sleeping problems can be caused by chronic pain?
- •What kind of sleep pattern do you have at present?
- •How much sleep do you need?
- •How to use a sleep diary
- •How can you change unhelpful sleep habits?
- •Relaxation
- •What is relaxation?
- •How can relaxation help with chronic pain?
- •What can help you relax?
- •How to practise relaxing
- •Time out relaxation
- •What can make it difficult to practise relaxation?
- •Pain, communication and relationships
- •Part 1: communication and sharing concerns How close relationships can be affected by pain
- •How to manage difficulties in relationships
- •How to change behavior
- •How to communicate and share your concerns
- •Part 2: chronic pain and sexual relationships
- •How to deal with sexual problems
- •How to make sexual relationships easier
- •Managing depression, anxiety and anger
- •What moods can occur because of pain?
- •Part 1: managing depression
- •Why do people become depressed with chronic pain?
- •How depression affects people’s thinking
- •What factors can contribute to depression?
- •Unhelpful thinking in depression
- •Using anti-depressants
- •Part 2: managing anxiety
- •What is anxiety?
- •What are the effects of anxiety?
- •How does anxiety affect the body?
- •Anxiety and chronic pain
- •Managing anxiety by dealing with unhelpful thinking
- •Overcoming avoidance
- •Changing unhelpful behaviors
- •Part 3: managing anger
- •How anger affects you and your pain
- •How chronic pain and anger are linked
- •How being angry can affect other people
- •How to manage anger better
- •A coping plan
- •Acceptance
- •What is acceptance?
- •How can acceptance help you manage chronic pain?
- •What is attentional control or mindfulness?
- •1. Reasonable (thinking reasonably)
- •2. Emotional (thinking emotionally)
- •3. Wise (being mindful)
- •Mindfulness skills
- •1. Observing
- •2. Being ‘non-judgemental’
- •3. Focusing on one thing now and being in the present
- •4. Doing what works
- •Mindfulness exercises
- •Maintaining progress and managing setbacks
- •How can you maintain progress?
- •Obstacles to progress
- •What is a setback?
- •How can you manage a setback?
- •Looking to the future and managing work
- •How are new ways of life and new roles possible?
- •How can you use a positive data log?
- •Thinking through work, training and other options
- •How can you stay at work or return to work successfully?
- •Useful information
- •Professional organizations
- •Self-help groups and organizations
- •Books and publications
- •Self-help books
- •Tapes and cDs
- •Useful videos
- •Wordlist
How are new ways of life and new roles possible?
It is possible to change the impact of pain, steadily and slowly. You may need to start by thinking about what changes are possible in the short term or at this point in your life. It is also useful to keep a record of the changes you have made. This evidence of successes may help you realize that it is possible to return to, or stay at work, or develop new roles and skills. A Positive Data Log will enable you to build a record of your ability to cope or manage life despite the pain. Sometimes it is easy to overlook positive things that happen, so keeping a record can help to:
• Boost your confidence as changes happen
• Maintain your progress in getting active and reaching goals
• Remind you and others that change is possible, especially when you have a setback
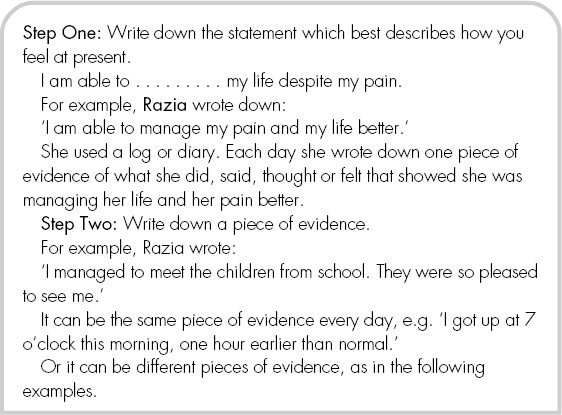
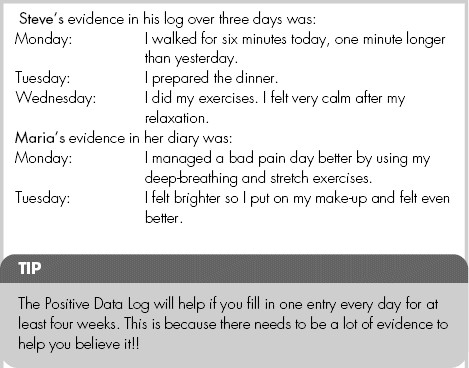
How can you use a positive data log?
A Positive Data Log helps you to gather evidence that you are able to manage or cope with your life with your pain. You can start by filling the gap in the following sentence:
I am able to . . . . . . . . . my life despite my pain.
Choose the word that seems right for you at present, in your situation. For example ‘cope with’, ‘control’ or ‘manage’. Or you can use other words that seem best for you, such as, ‘deal with’ or ‘accept’ or even ‘tolerate’. Steve chose ‘cope with’ for his log.

TIP
It can help to be aware that sometimes the way we think can change the evidence and reduce its value (see Chapter 14 on ‘Managing Depression, Anxiety and Anger’).
These three things may happen to your thinking when you look at the evidence you have recorded. You may:
1 Distort or dismiss the evidence, by saying to yourself: ‘Of course there is a change, that would happen anyhow.’
2 Ignore the evidence, by not even noticing that something positive has been said, done, thought or felt.
3 Discount the evidence, by saying: ‘It’s a fluke that I achieved my goal of walking to the shops this week.’
STARTING YOUR OWN POSITIVE DATA LOG
In your notebook, or diary, write a heading ‘My Positive Data Log’.
Begin with your statement:
I am able to . . . . . . . . . my life despite my pain.
Choose the word that seems best for you, e.g. ‘cope’, ‘control’, ‘manage’, ‘deal with’ or ‘accept’.
Then write your column headings as they are shown here:
Remember to keep your Positive Data Log for at least four weeks.
Thinking through work, training and other options
It has been found that people manage chronic or long-term conditions like heart disease better when they are doing something that they value. Doing something worthwhile can give you a sense of purpose, build confidence and boost your mood. Options might include paid work or volunteering, being a school governor, doing an evening class, or looking after grandchildren.
Improving skills in managing life despite the pain and being more confident can mean there is a real possibility of:
• Staying at work
• Returning to work
• Starting or continuing study or retraining
• Choosing other options, such as fostering or voluntary work
• Developing new roles or activities in life
Recent studies show that people with chronic pain have found many different ways to achieve their goal of staying at or returning to work. They have enjoyed themselves, had some fun, met new people and coped well with some difficult times on their route back to work or study.
It helps to think about both work and non-work activities, such as hobbies and voluntary activities. You can also consider how you would like to spend your days and nights.
It may help to revisit Chapter 1 (‘Understanding the Impact of Pain’). This chapter looked at the changes you might wish to make in particular areas of your life, including work activities.
Start by thinking about your most important reasons for staying at or returning to work.
What are your main concerns about what this would involve for you at present?
Write your thoughts under two column headings in your notebook:
‘Most important reasons for staying at or returning to work’ and ‘Main concerns’.
