
- •Other titles in the series include:
- •Overcoming chronic pain a self-help manual using Cognitive Behavioral Techniques frances cole, helen macdonald, catherine carus and hazel howden-leach
- •Isbn: 978-1-84119-970-2 eIsbn: 978-1-47210-573-8
- •Table of contents
- •Acknowledgements
- •Foreword
- •Introduction by Peter Cooper Why cognitive behavioral?
- •Introduction
- •Who might benefit from using this book?
- •What does chronic pain mean?
- •What is Cognitive Behavioral Therapy?
- •How can a book help?
- •How can I get the most out of using this book?
- •What do the chapters cover?
- •How do I start using this book?
- •Four case histories
- •Using the person-centred model
- •Maria and the person-centred model
- •How did the model help Maria make changes for the better?
- •How can the person-centred model help you get ready tomake some changes?
- •Getting started
- •Reducing the impact of pain on your daily life
- •How do you or others see these changes occurring?
- •Understanding chronic pain and pain systems
- •Understanding pain
- •Acute and chronic pain
- •What is acute pain?
- •What is chronic pain?
- •Acute and chronic pain systems
- •The acute pain system
- •The chronic pain system
- •Theories of pain The Gate Control Theory of Pain
- •Other theories of pain
- •Frequently asked questions
- •Understanding investigations for pain
- •Blood tests
- •Waiting for tests and results
- •Understanding the roles of healthcare professionals
- •Healthcare professionals
- •What is the role of a physiotherapist?
- •How do physiotherapists work?
- •What is the role of a specialist pain nurse?
- •What is the role of a pain specialist?
- •What is the role of a psychologist?
- •What is the role of a psychiatrist?
- •Talking therapies
- •Cognitive Behavioral Therapy
- •Pain management programmes
- •Understanding medicines and using them better
- •What types of medicines are used to manage chronic pain?
- •How are medicines used? Analgesics
- •Problems with medicines
- •Making better use of medicines
- •Four suggestions for using medications more helpfully
- •Stopping or reducing your medicines
- •Part two Overcoming Chronic Pain
- •Introduction
- •Setting goals
- •What are goals?
- •Informal and formal goals
- •What are smart goals?
- •Setting goals
- •Using a goal ladder
- •Achieving your goals
- •Giving yourself rewards
- •What are rewards?
- •Creating a ‘fun presciption’
- •50 Mg of fun three times a day (at least) For maximum benefit, use imagination!
- •Understanding pacing skills
- •What is pacing?
- •What are the different styles of pacing?
- •What type of pacing style do you use at present?
- •If pain levels are low, do you:
- •If pain levels are high, do you:
- •How to change your pacing style
- •Experimenting
- •Planning
- •Priorities
- •How to deal with barriers to realistic pacing
- •Getting fitter and being more active
- •How being more active can help you manage your pain
- •Trying to get fitter: What does having more pain mean?
- •Why do these types of activity cause aches and pains?
- •Assessing your present activity level
- •Frequently asked questions about increasing physical activity
- •How to get started on a basic exercise programme
- •Strength exercises – do slowly
- •Stretches for flexibility
- •Understanding problem-solving
- •What is problem-solving?
- •The main steps in problem-solving
- •Putting the problem-solving process into practise
- •Problem-solving guide
- •Understanding sleep and sleep problems
- •What sort of sleeping problems can be caused by chronic pain?
- •What kind of sleep pattern do you have at present?
- •How much sleep do you need?
- •How to use a sleep diary
- •How can you change unhelpful sleep habits?
- •Relaxation
- •What is relaxation?
- •How can relaxation help with chronic pain?
- •What can help you relax?
- •How to practise relaxing
- •Time out relaxation
- •What can make it difficult to practise relaxation?
- •Pain, communication and relationships
- •Part 1: communication and sharing concerns How close relationships can be affected by pain
- •How to manage difficulties in relationships
- •How to change behavior
- •How to communicate and share your concerns
- •Part 2: chronic pain and sexual relationships
- •How to deal with sexual problems
- •How to make sexual relationships easier
- •Managing depression, anxiety and anger
- •What moods can occur because of pain?
- •Part 1: managing depression
- •Why do people become depressed with chronic pain?
- •How depression affects people’s thinking
- •What factors can contribute to depression?
- •Unhelpful thinking in depression
- •Using anti-depressants
- •Part 2: managing anxiety
- •What is anxiety?
- •What are the effects of anxiety?
- •How does anxiety affect the body?
- •Anxiety and chronic pain
- •Managing anxiety by dealing with unhelpful thinking
- •Overcoming avoidance
- •Changing unhelpful behaviors
- •Part 3: managing anger
- •How anger affects you and your pain
- •How chronic pain and anger are linked
- •How being angry can affect other people
- •How to manage anger better
- •A coping plan
- •Acceptance
- •What is acceptance?
- •How can acceptance help you manage chronic pain?
- •What is attentional control or mindfulness?
- •1. Reasonable (thinking reasonably)
- •2. Emotional (thinking emotionally)
- •3. Wise (being mindful)
- •Mindfulness skills
- •1. Observing
- •2. Being ‘non-judgemental’
- •3. Focusing on one thing now and being in the present
- •4. Doing what works
- •Mindfulness exercises
- •Maintaining progress and managing setbacks
- •How can you maintain progress?
- •Obstacles to progress
- •What is a setback?
- •How can you manage a setback?
- •Looking to the future and managing work
- •How are new ways of life and new roles possible?
- •How can you use a positive data log?
- •Thinking through work, training and other options
- •How can you stay at work or return to work successfully?
- •Useful information
- •Professional organizations
- •Self-help groups and organizations
- •Books and publications
- •Self-help books
- •Tapes and cDs
- •Useful videos
- •Wordlist
What type of pacing style do you use at present?
You can identify your pacing style by using the lists below. Tick those behaviors or actions you use at present. If you are having problems identifying your current pacing style using the lists, ask a friend, partner or family member to help you. They will often be more aware of your pattern of activity and unhelpful pacing styles.
LIST A
If pain levels are low, do you:
1 Try to make up for all the things you haven’t done or achieved because the pain stopped you?
2 Fit in as much as possible until the pain level is very high?
3 Do activities as fast as possible until the pain level is very high?
4 Do very little so as to keep the pain level low?
5 Focus on doing important activities at a steady pace with regular breaks?
LIST B
If pain levels are high, do you:
1 Keep going with all your activities, despite the pain, with few or no breaks?
2 Put a brave face on it and keep ‘battling on’ with activities?
3 Reduce all your activity until pain gets lower?
4 Reduce high standards for activities for the high pain period?
5 Plan activities that are realistic?
6 Decide on important activities?
7 Focus on doing important activities at a steady pace, with regular breaks?
If you ticked the first three items in list A or or the first two items in list B, then you are using an overactive style. If you ticked number 4 in list A or number 3 in list B, then you may be using an underactive type of pacing. Alternatively, you may have ticked a mix of both pacing styles, which is quite common.
If you are finding this task hard, read about Jim’s and Razia’s daily routines over the next few pages. This may help you work out your current pacing style.
LIST C
Helpful pacing style
Below are the features of a helpful pacing style:
• Focus on doing important activities at a steady pace with regular breaks.
• Reduce high standards for activities for the high pain period.
• Plan activities that are realistic.
• Decide on important activities.
These are ways of pacing activities that will put you in control and help you manage the pain.
Consider these two examples of pacing styles.
Jim
Jim is 59 years old. He is married to Ann who has a heart problem. Jim retired as a teacher two years ago, because of his chest and abdomen pain. Since his retirement, he has taken on many household tasks to fill his day and to help Ann because of her heart problems. He shops every day, prepares and cooks all the meals. He does all the washing and ironing. He has a large garden and spends the rest of his time weeding, planting out and mowing the lawn. He thinks he must get these jobs done so that Ann won’t feel worried or stressed. He used to enjoy walking and reading but he has difficulty finding time. He is becoming exhausted and has noticed, to his surprise, that his pain is worse.
Jim’s pacing style can be described as overactive. It has advantages and disadvantages.
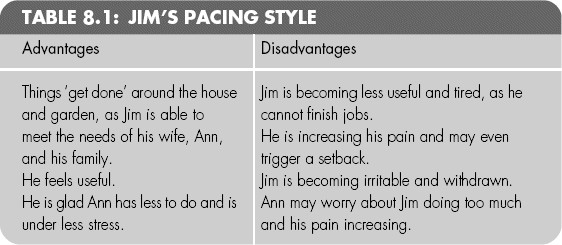
What would you suggest to help Jim pace better? Use your notebook and write four ways he could improve his pacing?
Razia
Razia finds the pain from her fibromyalgia unpredictable and often rests when she has bad pain days. She wanted to stay active because of the children. She saw the physiotherapist and was given stretch exercises to help her become more active. The stretches made her body hurt more, so she did not keep her next appointment. The doctor has told Razia that physiotherapy can’t help her if she doesn’t go to the appointments. Razia finds that if she does very few activities then her pain eases up. She has stopped all housework and sleeps a lot. Her parents are doing all the shopping and childcare, especially after school. She thinks she should meet all her children’s needs herself. She believes the pain is making her tired and irritable, and spoiling daily life. Razia has lost confidence and sees herself as a ‘useless mother’.
Razia’s pacing style can be described as underactive. It has advantages and disadvantages.

What would you suggest to help Razia pace better? Using your notebook and write four ways she could improve her pacing?
• What are the advantages and disadvantages of your own pacing style?
• Would you say your style is overactive, underactive, a mixture of overactive and underactive, or sensible (as in List C on page 121)?
