
Human_Histology
.pdf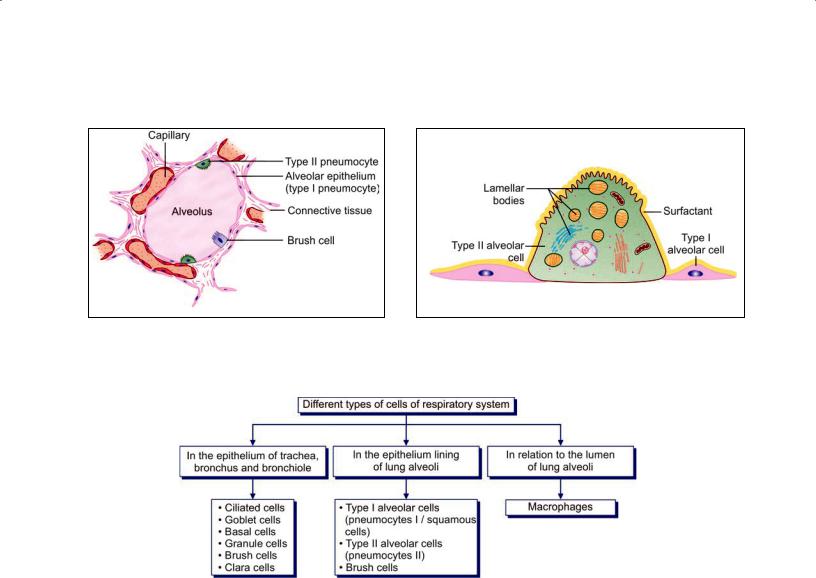
158 Textbook of Human Histology
Fig. 13.7: Some cells to be seen in relation to an alveolus Fig. 13.8: Type II pneumocytes (Schematic representation)
(Schematic representation)
Flowchart 13.1: Different types of cells of respiratory system
junctions (preventing leakage of blood from capillaries into the alveolar lumen). They form the lining of 90% of the alveolar surface.
Scattered in the epithelial lining there are rounded secretory cells bearing microvilli on their free surfaces. These are designated type II alveolar epithelial cells
(Figs. 13.7 and 13.8). Their cytoplasm contains secretory granules that appear to be made up of several layers (and are, therefore, called multilamellar bodies). These cells are believed to produce a secretion that forms a film over the alveolar epithelium. This film or pulmo nary surfactant reduces surface tension and prevents collapse of the alveolus during expiration.
Surfactant contains phospholipids, proteins and glycosaminoglycans produced in type II cells (A similar fluid is believed to be produced by the cells of Clara present in bronchial passages).
Type II cells may multiply to replace damaged type I cells.
Type III alveolar cells, or brush cells, of doubtful function, have also been described.
Different types of cells present in the respiratory system are summarized in Flowchart 13.1.
Connective Tissue
The connective tissue in the wall of the alveolus contains collagen fibers and numerous elastic fibers continuous with those of bronchioles. Fibroblasts, histiocytes, mast cells, lymphocytes and plasma cells may be present. Pericytes are present in relation to capillaries.
Some macrophages enter the connective tissue from blood and pass through the alveolar epithelium to reach its luminal surface. Dust particles phagocytosed by them are seen in their cytoplasm. They are therefore called dust cells. These dust cells are expelled to the outside through the respiratory passages. In con gestive heart failure (in which pulmonary capillaries become overloaded with blood) these macrophages phagocytose erythrocytes that escape from capillaries. The cells, therefore, acquire a brick red color and are then called heart failure cells. Macrophages also remove excessive surfactant, and secrete several enzymes.
Connective Tissue Basis of the Lung
The greater part of the surface of the lung is covered by a serous membrane, the visceral pleura. This membrane consists of a layer of flattened mesothelial cells, supported on a layer of connective tissue.
Deep to the pleura there is a layer of subserous con nective tissue. This connective tissue extends into the lung substance along bronchi and their accompanying blood vessels, and divides the lung into lobules. Each lobule has a lobular bronchiole and its ramifications, blood vessels, lymphatics, and nerves.
The epithelial lining of air passages is supported by a basal lamina deep to which there is the connective tissue of the lamina propria. Both in the basal lamina and in the lamina propria there are numerous elastic fibers. These fibers run along the length of respiratory passages and ultimately become continuous with elastic fibers present in the walls of air sacs. This elastic tissue plays a very important role by providing the physical basis for elastic recoil of lung tissue. This recoil is an important factor in expelling air from the lungs during expiration. Elastic fibers passing between lung parenchyma and pleura prevent collapse of alveoli and small bronchi during expiration.
Pleura
The pleura is lined by flat mesothelial cells that are sup ported by loose connective tissue rich in elastic fibers, blood vessels, nerves and lymphatics. There is considerable adipose tissue under parietal pleura.
Blood Supply of Lungs
The lungs receive deoxygenated blood from the right ventricle of the heart through pulmonary arteries. Within the lung the arteries end in an extensive capillary network in the walls of alveoli. Blood oxygenated here is returned to the left atrium of the heart through pulmonary veins.
Oxygenated blood required for nutrition of the lung itself reaches the lungs through bronchial arteries. They are distributed to the walls of bronchi as far as the respiratory bronchioles. Blood reaching the lung through these arteries is returned to the heart partly through bronchial veins, and partly through the pulmonary veins.
Chapter 13 The Respiratory System 159
Plexuses of lymph vessels are present just deep to the pleura and in the walls of bronchi.
Nerve Supply of Lungs
The lungs receive autonomic nerves, both sympathetic and parasympathetic, and including both afferent and efferent fibers. Efferent fibers supply the bronchial musculature. Vagal stimulation produces bronchoconstriction. Efferent fibers also innervate bronchial glands. Afferent fibers are distributed to the walls of bronchi and of alveoli. Afferent impulses from the lungs play an important role in control of respiration through respiratory reflexes.
Clinical Correlation
Acute respiratory distress syndrome (ARDS) is a severe, at times life-threatening, form of progressive respiratory insufficiency which involves pulmonary tissues diffusely, i.e. involvement of the alveolar epithelium, alveolar lumina and interstitial tissue.ARDSexistsin2forms:neonatalandadulttype.Bothhave the common morphological feature of formation of hyaline membrane in the alveoli, and hence, is also termed as hyaline membrane disease (HMD).
Bacterial pneumonia: Bacterial infection of the lung parenchyma is the most common cause of pneumonia or consolidation of one or both the lungs. Two types of acute bacterial pneumonias are distinguished—lobar pneumonia and broncho- (lobular-) pneumonia, each with distinct aetiologic agent and morphologic changes.
Chronic bronchitis is a common condition defined clinically as persistent cough with expectoration on most days for at least three months of the year for two or more consecutive years. The cough is caused by oversecretion of mucous. In spite of its name, chronic inflammation of the bronchi is not a prominent feature.Theconditionismorecommoninmiddle-agedmalesthan females.
Asthma is a disease of airways that is characterized by increased responsiveness of the tracheobronchial tree to a variety of stimuli resulting in widespread spasmodic narrowing of the air passages which may be relieved spontaneously or by therapy. Asthma is an episodic disease manifested clinically by paroxysms of dyspnoea, cough and wheezing. However, a severe and unremitting form of the disease termed status asthmaticus may prove fatal.
Immotile cilia syndrome that includes Kartagener’s syndrome (bronchiectasis, situs inversus and sinusitis) is characterized by ultrastructural changes in the microtubules causing immotility of cilia of the respiratory tract epithelium, sperms and other cells. Males in this syndrome are often infertile.
Digestive System: Oral Cavity and Related Structures
The abdominal part of the alimentary canal (consisting of the stomach and intestines) is often referred to as the gastrointestinal tract. Closely related to the alimentary canal there are several accessory organs that form part of the alimentary system. These include the structures of the oral cavity (lips, teeth, tongue, salivary glands) and the liver and pancreas.
ORAL CAVITY
The wall of the oral cavity is made up partly of bone (jaws and hard palate), and partly of muscle and connective tissue (lips, cheeks, soft palate, and floor of mouth). These structures are lined by mucous membrane which is lined by stratified squamous epithelium that rests on connective tissue, similar to that of the dermis.
The epithelium differs from that on the skin in that it is not keratinized. Papillae of connective tissue (similar to dermal papillae) extend into the epithelium. The size of these papillae varies considerably from region to region. Over the alveolar processes (where the mucosa forms the gums), and over the hard palate, the mucous membrane is closely adherent to underlying periosteum. Elsewhere it is connected to underlying structures by loose connective tissue. In the cheeks, this connective tissue contains many elastic fibers and much fat (specially in children).
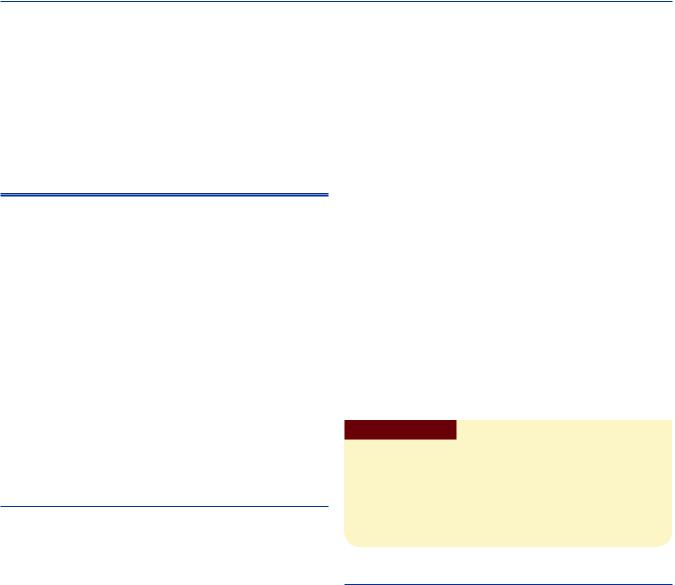
THE LIPS
Lips are fleshy folds which on the “external” surface are lined by skin, and on “internal” surface are lined by mucous membrane. It must be noted, however, that part of the mucosal surface is “free” and constitutes the region the lay person thinks of as the lip. The substance of each lip (upper or lower) is predominantly muscular (skeletal muscle) (Fig. 14.1).
The upper and lower lips close along the red margin which represents the mucocutaneous junction. There is a transitional zone between the skin and mucous membrane which is sometimes referred to as the vermilion, because
of its pink color in fair skinned individuals. This part meets the skin along a distinct edge.
The “external” surface of the lip is lined by true skin in which hair follicles and sebaceous glands can be seen.
The mucous membrane is lined by stratified squamous nonkeratinized epithelium (Plate 14.1). This epithelium is much thicker than that lining the skin (specially in infants). The epithelium has a well marked rete ridge system. The term rete ridges is applied to finger-like projections of epithelium that extend into underlying connective tissue, just like the epidermal papillae. This arrangement anchors the epithelium to underlying connective tissue, and enables it to withstand friction. A similar arrangement is seen in the mucosa over the palate.
Subjacent to the epithelium the mucosa has a layer of connective tissue (corresponding to the dermis), and a deeper layer of loose connective tissue. The latter contains numerous mucous glands. Sebaceous glands, not associated with hair follicles, may be present. Their secretions prevent dryness and cracking of the exposed part of the mucosa.
Clinical Correlation
Fordyce’s granules: Fordyce’s granules are symmetric, small, light yellow macular spots on the lips and buccal mucosa and represent collections of sebaceous glands.
Pyogenic granuloma: This is an elevated, bright red swelling of variable size occurring on the lips, tongue, buccal mucosa,Pregnancy tumor is a variant of pyogenic granuloma.
THE TEETH
General Structure
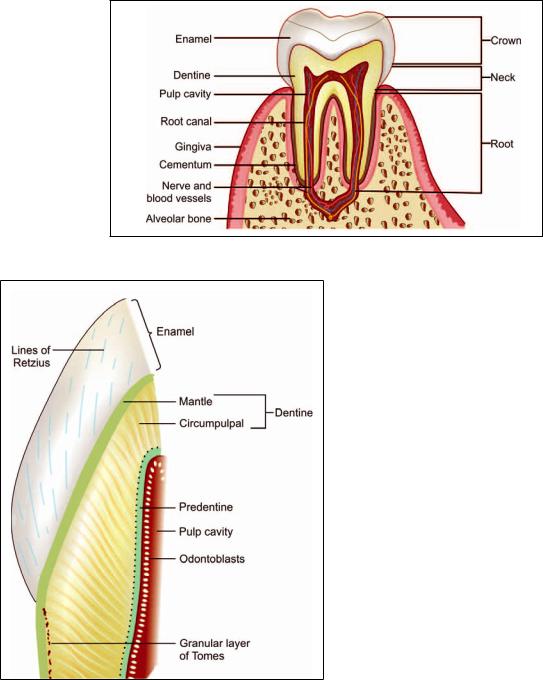
A tooth consists of an “upper” part, the crown, which is seen in the mouth; and of one or more roots which are embedded in sockets in the jaw bone (mandible or maxilla). It is composed of 3 calcified tissues, namely: enamel, dentine, and the pulp (Fig. 14.2).
Chapter 14 Digestive System: Oral Cavity and Related Structures 161
PLATE 14.1: Longitudinal Section through the Lip
The substance of the lip is formed by a mass of muscle
Each lip has an 'external' surface covered by skin and an “internal” surface lined by mucous membrane
Key
! "
# $ % & (
) *
+ ,
- .
Longitudinal Section through the Lip as seen in drawing
Fig. 14.1: Some relationships of the lips (Schematic representation)
The greater part of the tooth is formed by a bone-like material called dentine. In the region of the crown the dentine is covered by a much harder white material called the enamel. Over the root the dentine is covered by a thin layer of cementum. The cementum is united to the wall of the bony socket in the jaw by a layer of fibrous tissue that is called the periodontal ligament.
Within the dentine there is a pulp canal (or pulp cavity) that contains a mass of cells, blood vessels, and nerves that constitute the pulp. The blood vessels and nerves enter the pulp canal through the apical foramen which is located at the apex of the root.
The Enamel
The enamel is the hardest material in the body. It is made up almost entirely (96%) of inorganic salts. These salts are mainly in the form of complex crystals of hydroxyapatite (as in bone). The crystals contain calcium phosphate and calcium carbonate. Some salts are also present in amorphous form. The crystals of hydroxyapatite are arranged in the form of rod-shaped prisms, which run from the deep surface of the enamel (in contact with dentine) to its superficial (or free) surface.
Prisms are separated by interprismatic material. There is no essential difference in the structure of prisms and of interprismatic material, the two appearing different only because of differing orientation of the hydroxyapatite crystals in them. The most superficial part of the enamel is devoid of prisms.
162 Textbook of Human Histology
Fig. 14.2: Vertical section through a tooth (Schematic representation)
Fig. 14.3: Part of a tooth to show some features of the structure of enamel and dentine (Schematic representation)
During development, enamel is laid down in the form of layers. When seen in section these layers can be distinguished as they are separated by lines running more or less parallel to the surface of the enamel. These lines are called the incremental lines or the lines of Retzius
(Fig. 14.3). In some teeth, in which enamel formation takes
place partly before birth and partly after birth (e.g. in milk teeth), one of the incremental lines is particularly marked. It represents the junction of enamel formed before birth with that formed after birth, and is called the neonatal line.
At places, the enamel is penetrated by extraneous material. Projections entering the enamel from the dentineenamel junction are called enamel tufts; and projections entering it from the free surface are called enamel lamellae (because of their shape). Dentineal tubules (see below) may extend into the enamel forming enamel spindles.
The Dentine
Structure and Composition
Dentine is a hard material having several similarities to bone. It is made up basically of calcified ground substance (glycosaminoglycans) in which there are numerous collagen fibers (type 1). The calcium salts are mainly in the form of hydroxyapatite. Amorphous salts are also present. The inorganic salts account for 70% of the weight of dentine. Like bone, dentine is laid down in layers that are parallel to the pulp cavity. The layers may be separated by less mineralized tissue that forms the incremental lines of Von Ebner. Dentine is permeated by numerous fine canaliculi that pass radially from the pulp cavity toward the enamel (or toward cement). These are the dentinal tubules. The tubules may branch specially near the enamel-dentine junction. We have seen (above) that some dentinal tubules extend into the enamel as enamel spindles.
The ground substance of dentine is more dense (than elsewhere) immediately around the dentinal tubules, and forms the peritubular dentine or the dentineal sheath (of Newmann). Each dentineal tubule contains a protoplasmic
Chapter 14 Digestive System: Oral Cavity and Related Structures 163
process arising from cells called odontoblasts, that line the pulp cavity. These protoplasmic processes are called the fibers of Tomes.
Near the surface of the root of the tooth (i.e. just deep to the cementum) the dentine contains minute spaces that give a granular appearance. This is the granular layer of Tomes.
Types of Dentin
At the junction of dentine with the pulp cavity there is a layer of predentine that is not mineralized. Dentine near the enamel-dentine junction is less mineralized (than elsewhere) and is called the mantle dentine. The main part of dentine (between predentine and mantle dentine) is called the circumpulpal dentine (Fig. 14.3). Dentine formed before eruption of the tooth is called primary dentine, while that formed after eruption is called secondary dentine.
The Cementum
Cementum is the portion of tooth which covers the dentine at the root of tooth and is the site where periodontal ligament is attached. In old people, cementum may be lost, exposing the dentine. Cementum is similar to bone in morphology and composition and may be regarded as a layer of true bone that covers the root of the tooth.
Toward the apex of the tooth, the cementum contains lacunae and canaliculi as in bone. The lacunae are occupied by cells similar to osteocytes (cementocytes). Some parts of cementum are acellular.
Cementum is covered by a fibrous membrane called the periodontal membrane (or ligament). This membrane may be regarded as the periosteum of the cementum. Collagen fibers from this membrane extend into the cementum, and also into the alveolar bone (forming the socket in which the root lies) as fibers of Sharpey. The periodontal membrane fixes the tooth in its socket. It contains numerous nerve endings that provide sensory information.
The Pulp
Dental pulp lies inner to dentine and occupies the pulp cavity and root canal. The dental pulp is made up of very loose connective tissue resembling embryonic mesenchyme (mucoid tissue). The ground substance is gelatinous and abundant. In it there are many spindleshaped and star-shaped cells. Delicate collagen fibers, numerous blood vessels, lymphatics and nerve fibers are present. The nerve fibers are partly sensory and partly sympathetic.
Clinical Correlation
Dental caries
Dental caries is the most common disease of dental tissues,
themolars and premolars, where food retention occurs, and in the cervical part of the tooth.
The earliest change is the appearance of a small, chalky-white spot on the enamel which subsequently enlarges and often becomes yellow or brown and breaks down to form carious cavity. Eventually, the cavity becomes larger due to fractures of enamel. Once the lesion reaches enamel-dentine junction, destruction of dentine also begins.
Pulpitis
isaccompanied by severe pain and requires immediate intervention or it may be chronic where the pulp is exposed widely. It may protrude through the cavity forming polyp of the pulp.
Stages in Tooth Development
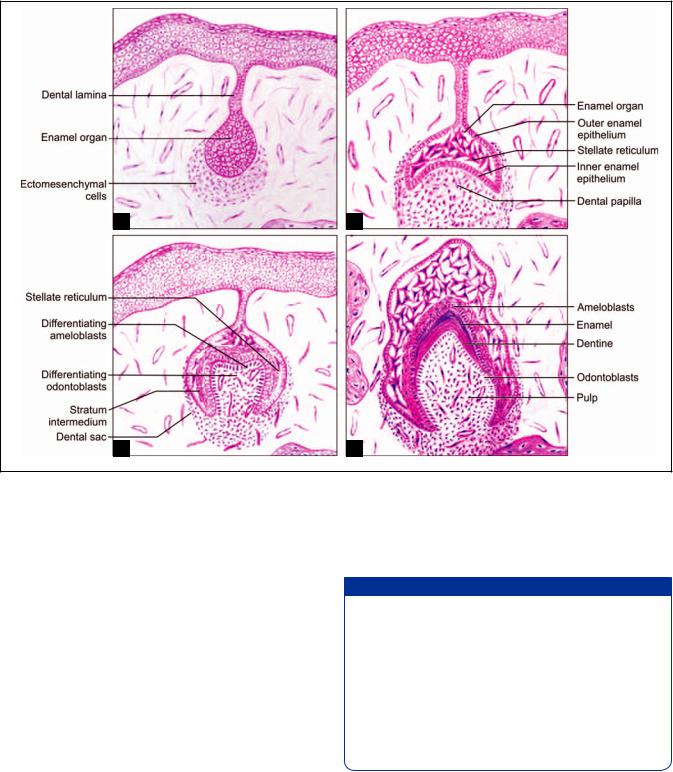
Each tooth may be regarded as a highly modified form of the stratified squamous epithelium covering the developing jaw (alveolar process). A thickening of epithelium grows downwards into the underlying connective tissue and enlarges to form an enamel organ (Figs. 14.4A to D).
Bud Stage (Fig. 14.4A)
The enamel organ resembles a small bud, which is surrounded by the condensation of ectomesenchymal cells. In this stage, the enamel organ is made up of peripherally located low columnar cells and centrally located polygonal cells.
Cap Stage (Fig. 14.4B)
The enamel organ then proliferates to form a cap over the central condensation of ectomesenchymal cells which is called the dental papilla. The dental papilla and the dental sac become well-defined. Three layers are differentiated from the enamel organ.
Inner dental/inner enamel epithelium
Stellate reticulum
Outer dental/outer enamel epithelium
Early Bell Stage (Fig. 14.4C)
The enamel organ resembles bell shape as a result of deepening of the undersurface of the epithelial cap. A cell layer forms in between the inner dental epithelium and stellate reticulum, called the stratum intermedium.
The inner dental epithelium differentiates into tall columnar cells called the ameloblasts. The peripheral cells of the dental papilla differentiate into odontoblasts
164 Textbook of Human Histology
A B
C D
Figs. 14.4A to D: Stages of tooth development. (A) Bud stage; (B) Cap stage; (C) Early bell stage;
(D) Advance bell stage (Schematic representation)
under the organizing influence of inner dental epithelium. Ameloblasts form enamel and odontoblasts produce dentine.
Advance Bell Stage (Fig. 14.4D)
In this stage, apposition of dental hard tissues occurs. Odontoblasts are dentine forming cells; ameloblasts are enamel forming cells. A layer of predentine is secreted by the odontoblasts. Both ameloblasts and odontoblasts behave in a way very similar to that of osteoblasts and lay down layer upon layer of enamel, or of dentine. The deposition of enamel and dentine continues until the crown formation is complete.
The formation of layers of enamel and dentine results in separation of ameloblasts and odontoblasts. The original line at which enamel and dentine formation begins is known as the enamel-dentine junction. At last, ameloblasts
come to line the external aspect of the enamel. The odontoblasts persist as a lining for the pulp cavity.
Added Information
When examined by EM both ameloblasts and odontoblasts show the features typical of actively secreting cells. They have prominent Golgi complexes and abundant rough ER. The apical part of each cell is prolonged into a process. In the case of odontoblasts, the process runs into the proximal part of a dentineal tubule. In ameloblasts, the projection is called Tomes process. This process contains numerous microtubules, and many secretory vesicles. Other smaller processes are present near the base of Tomes process. The organic matrix of enamel is released mainly by Tomes process, which also appears to be responsible for forming prisms of enamel.
Root Formation
Root formation is carried out by Hertwig’s epithelial root sheath which is formed by the cervical portion of the
Chapter 14 Digestive System: Oral Cavity and Related Structures 165
enamel organ. It molds the shape of the roots and initiates radicular dentine formation.
The root sheath encloses the dental pulp except at apical portion. The rim of root sheath, the epithelial diaphragm surrounds the primary apical foramen. The root apex remains wide open until about 2 to 3 years after the eruption of the tooth, when the root development is completed.
THE TONGUE
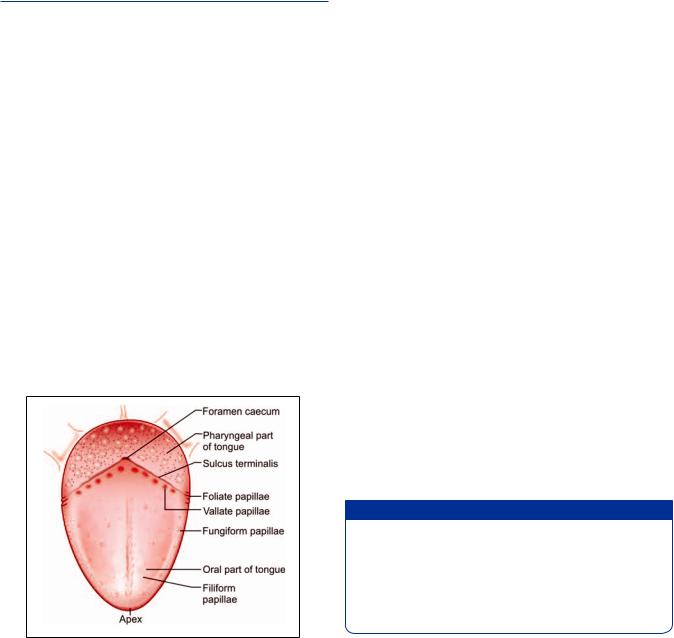
The tongue lies in the floor of the oral cavity. It has a dorsal surface that is free; and a ventral surface that is free anteriorly, but is attached to the floor of the oral cavity posteriorly. The dorsal and ventral surfaces become continuous at the lateral margins, and at the tip (or apex) of the tongue.
Near its posterior end the dorsum of the tongue is marked by a V-shaped groove called the sulcus terminalis (Fig. 14.5). The apex of the “V” points backwards and is marked by a depression called the foramen caecum. The limbs of the sulcus terminalis run forwards and laterally. The sulcus terminalis divides the tongue into a larger (2/3) anterior, or oral part; and a smaller (1/3) posterior, or pharyngeal part.
The substance of the tongue is made up chiefly of skeletal muscle supported by connective tissue (Plate 14.2). The muscle is arranged in bundles that run in vertical, transverse and longitudinal directions. This arrangement of muscle permits intricate movements of the tongue associated with the chewing and swallowing of food, and those necessary for speech. The substance of the tongue is divided into right and left halves by a connective tissue septum.
Fig. 14.5: Dorsal surface of the tongue
(Schematic representation)
The surface of the tongue is covered by mucous membrane lined by stratified squamous epithelium. The epithelium is supported on a layer of connective tissue. On the undersurface (ventral surface) of the tongue the mucous membrane resembles that lining the rest of the oral cavity, and the epithelium is not keratinized.
The mucous membrane covering the dorsum of the tongue is different over the anterior and posterior parts. Over the part lying in front of the sulcus terminalis the mucosa bears numerous projections or papillae.
Papillae
Each papilla consists of a lining of epithelium and a core of connective tissue. The epithelium over the papillae is partially keratinized (parakeratinized).
The papillae are of various types (Figs. 14.6A to D):
Filiformpapillae:Theyarethemostnumerouspapillae. They are small and conical in shape. The epithelium at the tips of these papillae is keratinized. It may project in the form of threads.
Fungiform papillae: At the apex of the tongue and along its lateral margins there are larger fungiform papillae with rounded summits and narrower bases. Fungiform papillae bear taste buds (described below). In contrast to the filiform papillae the epithelium on fungiform papillae is not keratinized.
Circumvallate papillae: These are the largest papillae of the tongue. They are arranged in a row just anterior to the sulcus terminalis. When viewed from the surface each papilla is seen to have a circular top demarcated from the rest of the mucosa by a groove. In sections through the papilla it is seen that the papilla has a circumferential “lateral wall” that lies in the depth of the groove (Figs. 14.6A to D and Plate 14.3). Taste buds are present on this wall, and also on the “outer” wall of the groove.
Foliate papillae: These are rudimentary in man. They can be seen along the posterior part of lateral margin of tongue.
Added Information
Another variety of papilla sometimes mentioned in relation to the tongue is the papilla simplex. Unlike the other papillae which can be seen by naked eye, the papillae simplex are microscopic and are quite distinct from other papillae. They are not surface projections at all, but are projections of subjacent connective tissue into the epithelium. In other words these papillae are equivalent to dermal papillae of the skin.
Note: The mucous membrane of the posterior (pharyngeal) part of the dorsum of the tongue bears numerous rounded
166 Textbook of Human Histology
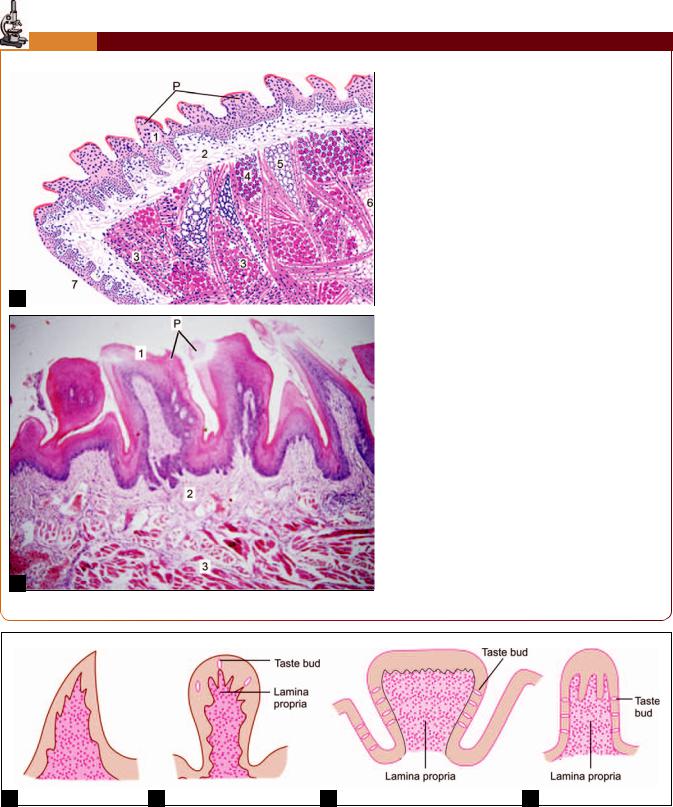
PLATE 14.2: Tongue: Anterior Part
A
B
Tongue. A. As seen in drawing; B. Photomicrograph
/ % & (
The ventral surface of the tongue is smooth, but on1 or papillae
2 3 % 4/ 5 papilla is circumvallate, the top of this papilla is broad and lies at the same level as the surrounding mucosa
The main mass of the tongue is formed by skeletal6 %/ ( tudinally and some transversely
Numerous serous and mucous glands are present / %
Key
3 % &! 7
# 3
) 3 /
+ 6 /
- 5
8 3 ventral surface of tongue
9 9
A B C D
Figs. 14.6A to D: Papillae, (A) Filliform; (B) Fungiform; (C) Circumvallate; (D) Foliate (Schematic representation)
Chapter 14 Digestive System: Oral Cavity and Related Structures 167
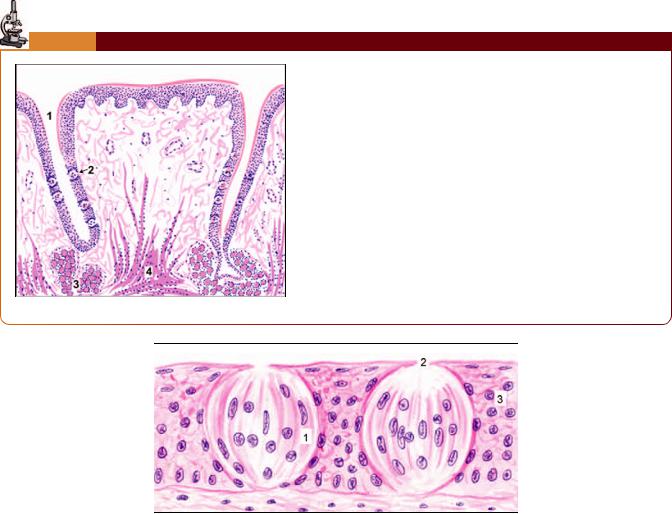
PLATE 14.3: Vallate Papilla
: (% &
Numerous oval shaped lightly stained taste buds can be seen on the
/ / ; 2
3 < /
Key
*
!
# 3 / ; 2
) 6 < /
As seen in drawing
Fig. 14.7:
elevations that are quite different from the papillae described above. These elevations are produced by collections of lymphoid tissue present deep to the epithelium which are collectively called the lingual tonsil.
Mucous and serous glands: Numerous mucous and serous glands are present in the connective tissue deep to the epithelium of the tongue. Mucous glands are most numerous in the pharyngeal part, in relation to the masses of lymphoid tissue. They open into recesses of mucosa that dip into the masses of lymphoid tissue. The serous glands are present mainly in relation to circumvallate papillae, and open into the furrows surrounding the papillae. Serous glands also open in the vicinity of other taste buds. It is believed that the secretions of these glands dissolve the substance to be tasted and spread it over the taste bud; and wash it away after it has been tasted.
The largest glands in the tongue are present on the ventral aspect of the apex. They contain both mucous and serous acini and are referred to as the anterior lingual glands.
Taste Buds
Taste buds are present in relation to circumvallate papillae, to fungiform papillae, and to leaf-like folds of mucosa (folia linguae) present on the posterolateral part of the tongue. Taste buds are also present on the soft palate, the epiglottis, the palatoglossal arches, and the posterior wall of the oropharynx.
Each taste bud is a piriform structure made up of modified epithelial cells (Fig. 14.7). It extends through the entire thickness of the epithelium. Each bud has a small cavity that opens to the surface through a gustatory pore. The cavity is filled by a material rich in polysaccharides.
