
Borchers Andrea Ann (ed.) Handbook of Signs & Symptoms 2015
.pdf
priapism, hypotension, anhidrosis, and bradycardia.
Stroke. Spastic paralysis may develop on the affected side following the acute stage of a stroke. Associated findings vary with the site and extent of vascular damage and may include dysarthria, aphasia, ataxia, apraxia, agnosia, ipsilateral paresthesia or sensory loss, vision disturbances, an altered LOC, amnesia and poor judgment, personality changes, emotional lability, bowel and bladder dysfunction, a headache, vomiting, and seizures.
Tetanus. Tetanus is a rare, life-threatening disease that produces varying degrees of spasticity. In generalized tetanus — the most common form — early signs and symptoms include painful jaw and neck stiffness, trismus, a headache, irritability, restlessness, a low-grade fever with chills, tachycardia, diaphoresis, and hyperactive DTRs. As the disease progresses, painful involuntary spasms may spread and cause boardlike abdominal rigidity, opisthotonos, and a characteristic grotesque grin known as risus sardonicus. Reflex spasms may occur in any muscle group with the slightest stimulus. Glottal, pharyngeal, or respiratory muscle involvement can cause death by asphyxia or cardiac failure.
Special Considerations
Prepare the patient for diagnostic tests, which may include electromyography, muscle biopsy, or intracranial or spinal magnetic resonance imaging or computed tomography. Administer pain medication and an antispasmodic. Passive range-of-motion exercises, splinting, traction, and application of heat may help relieve spasms and prevent contractures. Maintain a calm, quiet environment to help relieve spasms and prevent recurrence, and encourage bed rest. In cases of prolonged, uncontrollable spasticity, as with spastic paralysis, nerve blocks or surgical transection may be necessary for permanent relief.
Patient Counseling
Teach the patient to use assistive devices, as needed, and discuss ways to maintain independence.
Pediatric Pointers
In children, muscle spasticity may be a sign of cerebral palsy.
REFERENCES
Brainin, M. , Norrving, B. , Sunnerhagen, K. S., Goldstein, L. B., Cramer, S. C., Donnan, G. A., … Graham, G. (2011) . Post stroke chronic disease management: Towards improved identification and interventions for post stroke spasticity-related complications.
International Journal of Stroke, 6(1), 42–46.
Yelnik, A. P., Simon, O., Parratte, B., & Gracies, J. M. (2010). How to clinically assess and treat muscle overactivity in spastic paresis.
Journal of Rehabilitative Medicine, 42(9), 801–807.
Muscle Weakness
Muscle weakness is detected by observing and measuring the strength of an individual muscle or muscle group. It can result from a malfunction in the cerebral hemispheres, brain stem, spinal cord, nerve roots, peripheral nerves, or myoneural junctions and within the muscle itself. Muscle weakness occurs with certain neurologic, musculoskeletal, metabolic, endocrine, and cardiovascular disorders; as a response to certain drugs; and after prolonged immobilization.

History and Physical Examination
Begin by determining the location of the patient’s muscle weakness. Ask if he has difficulty with specific movements such as rising from a chair. Find out when he first noticed the weakness; ask him whether it worsens with exercise or as the day progresses. Also ask about related symptoms, especially muscle or joint pain, altered sensory function, and fatigue.
Obtain a medical history, noting especially chronic disease, such as hyperthyroidism; musculoskeletal or neurologic problems, including recent trauma; a family history of chronic muscle weakness, especially in males; and alcohol and drug use.
Focus your physical examination on evaluating muscle strength. Test all major muscles bilaterally. (See Testing Muscle Strength , pages 488 and 489.) When testing, make sure that the patient’s effort is constant; if it isn’t, suspect pain or other reluctance to make the effort. If the patient complains of pain, ease or discontinue testing and have him try the movements again. Remember that the patient’s dominant arm, hand, and leg are somewhat stronger than their nondominant counterparts. Besides testing individual muscle strength, test for range of motion (ROM) at all major joints (shoulder, elbow, wrist, hip, knee, and ankle). Also test sensory function in the involved areas, and test deep tendon reflexes (DTRs) bilaterally.
Medical Causes
Amyotrophic lateral sclerosis (ALS). ALS typically begins with muscle weakness and atrophy in one hand that rapidly spread to the arm and then to the other hand and arm. Eventually, these effects spread to the trunk, neck, tongue, larynx, pharynx, and legs; progressive respiratory muscle weakness leads to respiratory insufficiency.
Anemia. Varying degrees of muscle weakness and fatigue are exacerbated by exertion and temporarily relieved by rest. Other signs and symptoms include pallor, tachycardia, paresthesia, and bleeding tendencies.
Brain tumor. Signs and symptoms of muscle weakness vary with the location and size of the tumor. Associated findings include a headache, vomiting, diplopia, decreased visual acuity, a decreased level of consciousness (LOC), pupillary changes, decreased motor strength, hemiparesis, hemiplegia, diminished sensations, ataxia, seizures, and behavioral changes.
Guillain-Barré syndrome. Rapidly progressive, symmetrical weakness and pain ascends from the feet to the arms and facial nerves and may progress to total motor paralysis and respiratory failure. Associated findings include sensory loss or paresthesia, muscle flaccidity, loss of DTRs, tachycardia or bradycardia, fluctuating hypertension and orthostatic hypotension, diaphoresis, bowel and bladder incontinence, facial diplegia, dysphagia, dysarthria, and hypernasality.
Herniated disk. Pressure on nerve roots leads to muscle weakness, disuse and, ultimately, atrophy. The primary symptom is severe low back pain, possibly radiating to the buttocks, legs, and feet — usually on one side. Diminished reflexes and sensory changes may also occur.
Hypercortisolism. Hypercortisolism may cause limb weakness and eventually atrophy. Related cushingoid features include buffalo hump, moon face, truncal obesity, purple striae, thin skin, acne, elevated blood pressure, fatigue, hyperpigmentation, easy bruising, poor wound healing, and diaphoresis. The male patient may be impotent; the female patient may exhibit hirsutism and menstrual irregularities.

Myasthenia gravis. Gradually progressive skeletal muscle weakness and fatigue are the cardinal symptoms of myasthenia gravis. Typically, weakness is mild upon awakening but worsens during the day. Early signs include weak eye closure, ptosis, and diplopia; blank, masklike facies; difficulty chewing and swallowing; nasal regurgitation of fluid with hypernasality; and a hanging jaw and bobbing head. Respiratory muscle involvement may eventually lead to respiratory failure.
Osteoarthritis. Osteoarthritis is a chronic disorder that causes progressive muscle disuse and weakness that lead to atrophy.
Parkinson’s disease . Muscle weakness accompanies rigidity in Parkinson’s disease, a degenerative disorder. Related findings include a unilateral pill-rolling tremor, a propulsive gait, dysarthria, bradykinesia, drooling, dysphagia, masklike facies, and a high-pitched, monotone voice.
Peripheral nerve trauma. Prolonged pressure on or injury to a peripheral nerve causes muscle weakness and atrophy. Other findings include paresthesia or sensory loss, pain, and loss of reflexes supplied by the damaged nerve.
Potassium imbalance. With hypokalemia, temporary generalized muscle weakness may be accompanied by nausea, vomiting, diarrhea, decreased mentation, leg cramps, diminished reflexes, malaise, polyuria, dizziness, hypotension, and arrhythmias.
With hyperkalemia, weakness may progress to flaccid paralysis accompanied by irritability and confusion, hyperreflexia, paresthesia or anesthesia, oliguria, anorexia, nausea, diarrhea, abdominal cramps, tachycardia or bradycardia, and arrhythmias.
Rhabdomyolysis. Signs and symptoms include muscle weakness or pain, a fever, nausea, vomiting, malaise, and dark urine. Acute renal failure, due to renal structure obstruction and injury from the kidneys’ attempt to filter myoglobin from the bloodstream, is a common complication.
Rheumatoid arthritis. With rheumatoid arthritis, symmetrical muscle weakness may accompany increased warmth, swelling, and tenderness in involved joints; pain; and stiffness, restricting motion.
Seizure disorder. Temporary generalized muscle weakness may occur after a generalized tonicclonic seizure; other postictal findings include a headache, muscle soreness, and profound fatigue.
Spinal trauma and disease. Trauma can cause severe muscle weakness, leading to flaccidity or spasticity and, eventually, paralysis. Infection, tumor, and cervical spondylosis or stenosis can also cause muscle weakness.
Stroke. Depending on the site and extent of damage, a stroke may produce contralateral or bilateral weakness of the arms, legs, face, and tongue, possibly progressing to hemiplegia and atrophy. Associated effects include dysarthria, aphasia, ataxia, apraxia, agnosia, ipsilateral paresthesia or sensory loss, vision disturbances, an altered LOC, amnesia and poor judgment, personality changes, bowel and bladder dysfunction, a headache, vomiting, and seizures.
Other Causes
Drugs. Generalized muscle weakness can result from prolonged corticosteroid use, digoxin, and excessive doses of dantrolene. Aminoglycoside antibiotics may worsen weakness in patients
with myasthenia gravis.
Immobility. Immobilization in a cast, a splint, or traction can lead to muscle weakness in the involved extremity; prolonged bed rest or inactivity results in generalized muscle weakness.
Special Considerations
Provide assistive devices as necessary, and protect the patient from injury. If he has concomitant sensory loss, guard against pressure ulcer formation and thermal injury. With chronic weakness, provide ROM exercises or splint limbs as necessary. Arrange therapy sessions to allow for adequate rest periods, and administer pain medications as needed.
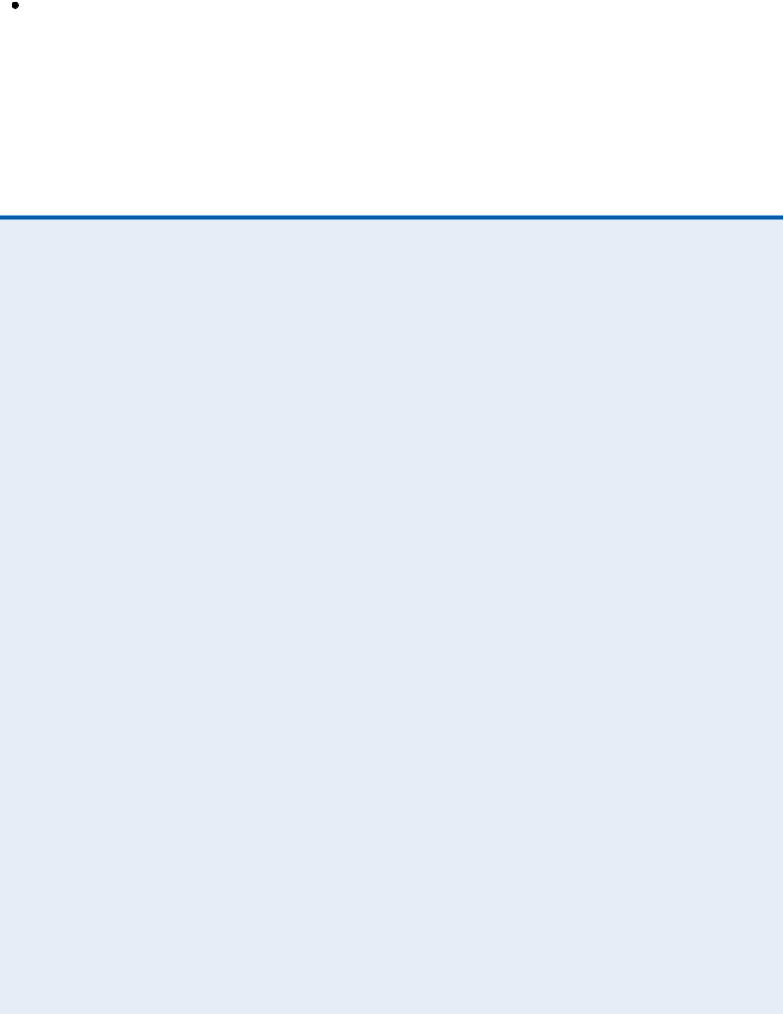
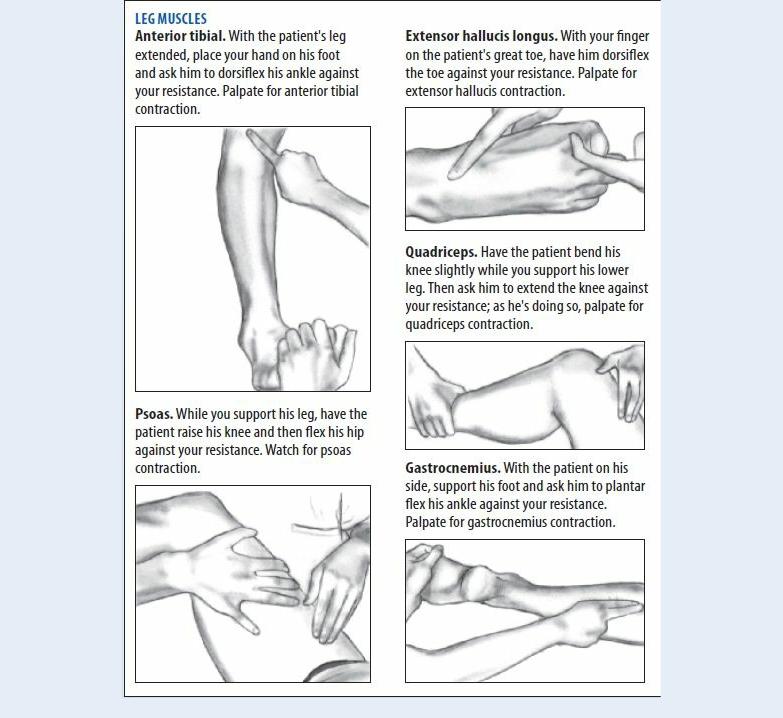
 EXAMINATION TIP Testing Muscle Strength
EXAMINATION TIP Testing Muscle Strength
Obtain an overall picture of the patient’s motor function by testing strength in 10 selected muscle groups. Ask him to attempt normal range-of-motion movements against your resistance. If the muscle group is weak, vary the amount of resistance as necessary to permit accurate assessment. If necessary, position the patient so his limbs don’t have to resist gravity, and repeat the test.
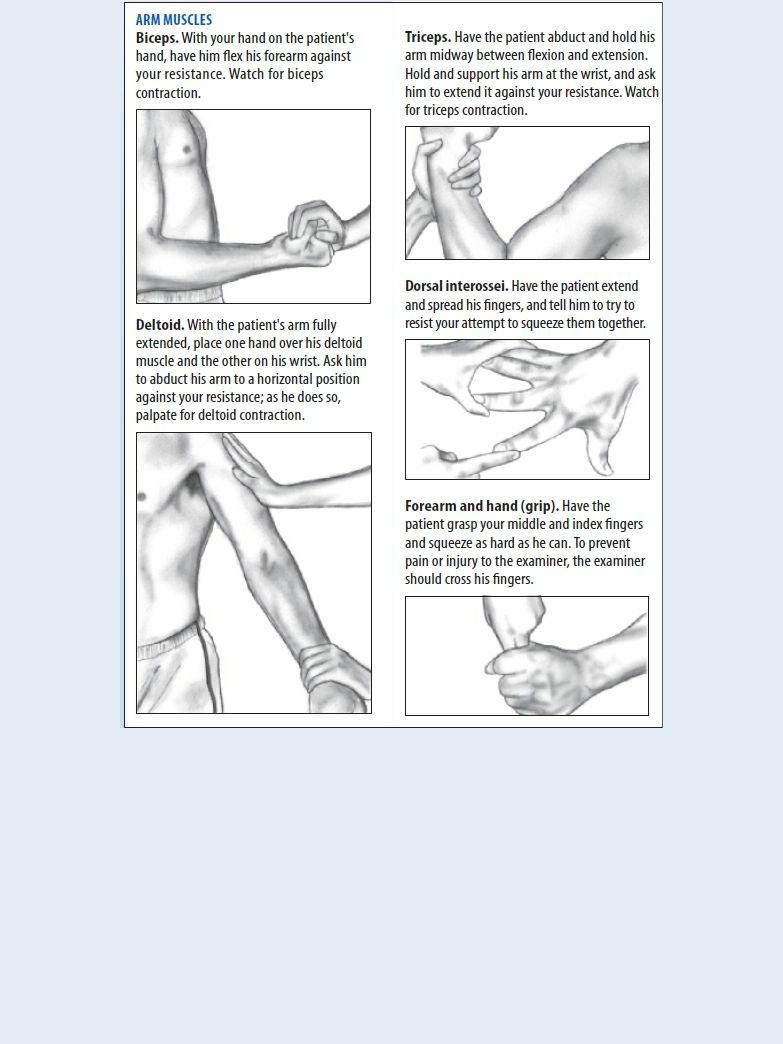
Rate muscle strength on a scale of 0 to 5:
0 = No evidence of muscle contraction
1 = Visible or palpable contraction but no movement
2 = Full muscle movement with force of gravity eliminated
3 = Full muscle movement against gravity but no movement against resistance 4 = Full muscle movement against gravity; partial movement against resistance
5 = Full muscle movement against both gravity and resistance — normal strength
Prepare the patient for blood tests, muscle biopsy, electromyography, nerve conduction studies, and X-rays or computed tomography scans.
Patient Counseling
Explain the importance of frequent position changes and rest periods. Teach the patient how to use assistive devices, as needed.
Pediatric Pointers
Muscular dystrophy, usually the Duchenne type, is a major cause of muscle weakness in children.
REFERENCES

Barr, J., Fraser, G. L., & Puntillo, K. (2013) . Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Critical Care Medicine, 41, 263–306.
Berry, M. J., Rejeski, W. J., Miller, M. E., Adair, N. E., Lang, W., Foy, C. G., & Katula, J. A. (2010). A lifestyle activity intervention in patients with chronic obstructive pulmonary disease. Respiratory Medicine, 104, 829–839.
Mydriasis
Mydriasis — pupillary dilation caused by contraction of the dilator of the iris — is a normal response to decreased light, strong emotional stimuli, and topical administration of mydriatic and cycloplegic drugs. It can also result from ocular and neurologic disorders, eye trauma, and disorders that decrease the level of consciousness (LOC). Mydriasis may be an adverse effect of antihistamines or other drugs.
History and Physical Examination
Begin by asking the patient about other eye problems, such as pain, blurring, diplopia, or visual field defects. Obtain a health history, focusing on eye or head trauma, glaucoma and other ocular problems, and neurologic and vascular disorders. In addition, obtain a complete drug history.
Next, perform a thorough eye and pupil examination. Inspect and compare the pupils’ size, color, and shape — many people normally have slightly unequal pupils. (See Grading Pupil Size, page 492.) Also, test each pupil for light reflex, consensual response, and accommodation. Perform a swinging flashlight test to evaluate a decreased response to direct light coupled with a normal consensual response (Marcus Gunn pupil). Be sure to check the eyes for ptosis, swelling, and ecchymosis. Test visual acuity in both eyes with and without correction. Evaluate extraocular muscle function by checking the six cardinal fields of gaze.
Keep in mind that mydriasis appears in two ocular emergencies: acute angle-closure glaucoma and traumatic iridoplegia.
Medical Causes
Adie’s syndrome . Adie’s syndrome is characterized by abrupt unilateral mydriasis, poor or absent pupillary reflexes, visual blurring, and cramplike eye pain. Deep tendon reflexes (DTRs) may be hyperactive or absent, especially the ankle and knee jerk reflexes.
Aortic arch syndrome. Bilateral pupillary mydriasis commonly occurs late in aortic arch syndrome. Other ocular findings include visual blurring, transient vision loss, and diplopia. Related findings include dizziness and syncope; neck, shoulder, and chest pain; bruits; loss of radial and carotid pulses; paresthesia; and intermittent claudication. Blood pressure may be decreased in the arms.
Botulism. Botulism toxin causes bilateral mydriasis, usually 12 to 36 hours after ingestion. Other early findings are a loss of pupillary reflexes, visual blurring, diplopia, ptosis, strabismus and extraocular muscle palsies, anorexia, nausea, vomiting, diarrhea, and dry mouth. Vertigo, hearing loss, hoarseness, hypernasality, dysarthria, dysphagia, progressive muscle weakness, and a loss of DTRs soon follow.
Carotid artery aneurysm. With carotid artery aneurysm, unilateral mydriasis may be accompanied by bitemporal hemianopsia, decreased visual acuity, hemiplegia, a decreased LOC, a headache, aphasia, behavioral changes, and hypoesthesia.
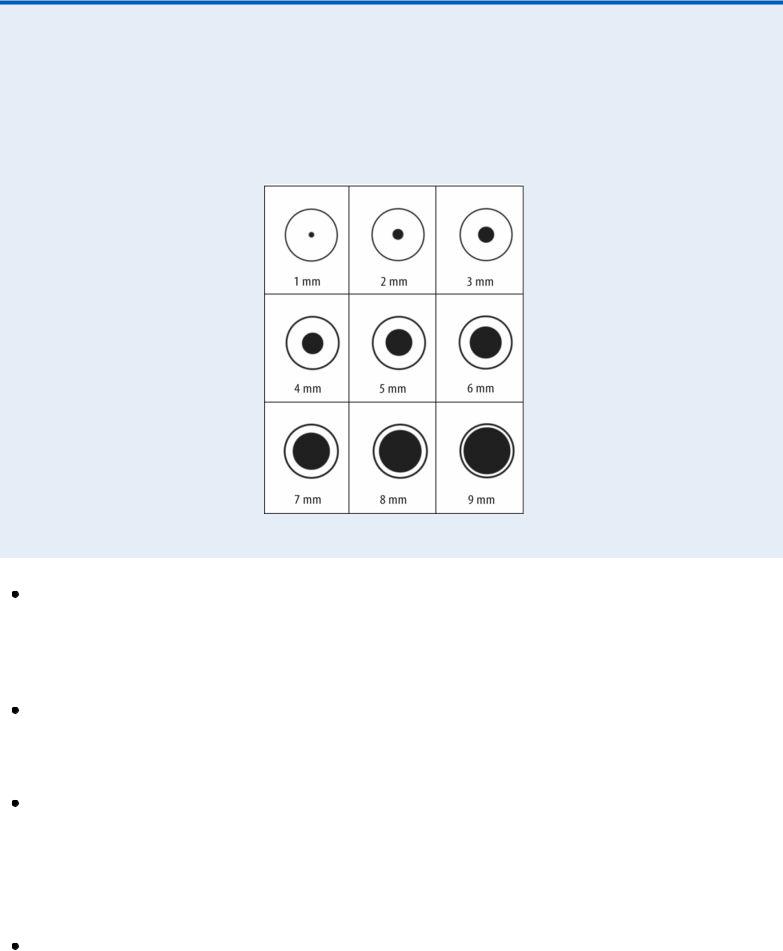
 EXAMINATION TIP Grading Pupil Size
EXAMINATION TIP Grading Pupil Size
To accurately evaluate pupil size, compare the patient’s pupils with the scale shown here. Keep in mind that the maximum constriction may be less than 1 mm and the maximum dilation greater than 9 mm.
Glaucoma (acute angle-closure). Acute angle-closure glaucoma is an ocular emergency that’s characterized by moderate mydriasis and the loss of pupillary reflex in the affected eye, accompanied by an abrupt onset of excruciating pain, redness, decreased visual acuity, visual blurring, halo vision, conjunctival injection, and a cloudy cornea. Without treatment, permanent blindness occurs in 2 to 5 days.
Oculomotor nerve palsy. Unilateral mydriasis is commonly the first sign of oculomotor nerve palsy. It’s soon followed by ptosis, diplopia, decreased pupillary reflexes, exotropia, and complete loss of accommodation. Focal neurologic signs may accompany signs of increased intracranial pressure (ICP).
Traumatic iridoplegia. Eye trauma can paralyze the sphincter of the iris, causing mydriasis and the loss of pupillary reflex; usually, this is transient. Associated findings include a quivering iris (iridodonesis), ecchymosis, pain, and swelling.
Other Causes
Drugs. Mydriasis can be caused by anticholinergics, antihistamines, sympathomimetics, barbiturates (in overdose), estrogens, and tricyclic antidepressants; it also commonly occurs early in anesthesia induction. Topical mydriatics and cycloplegics, such as phenylephrine, atropine, homatropine, scopolamine, cyclopentolate, and tropicamide, are administered

specifically for their mydriatic effects.
Surgery. Traumatic mydriasis commonly results from ocular surgery.
Special Considerations
Diagnostic tests may vary, depending on your findings, but may include a complete ophthalmologic examination and a thorough neurologic workup. Explain any diagnostic tests to the patient.
Patient Counseling
Discuss the effects of mydriatic drugs and ways to reduce their adverse effects.
Pediatric Pointers
Mydriasis occurs in children as a result of ocular trauma, drugs, Adie’s syndrome and, most commonly, increased ICP.
REFERENCES
Conway, B. N., May, M. E., Signorello, L. B., & Blot, W. J. (2012). Mortality experience of a low-income population with young-onset diabetes. Diabetes Care, 35, 542–548.
Gerstenblith, A. T., & Rabinowitz, M. P. (2012). The wills eye manual. Philadelphia, PA: Lippincott Williams & Wilkins.
Huang, J. J., & Gaudio, P. A. (2010). Ocular inflammatory disease and uveitis manual: Diagnosis and treatment. Philadelphia, PA : Lippincott Williams & Wilkins.
Rhodes, E. T., Prosser, L. A. , Hoerger, T. J. , Lieu, T. , Ludwig, D. S., & Laffel, L. M. (2012) . Estimated morbidity and mortality in adolescents and young adults diagnosed with type 2 diabetes mellitus. Diabetic Medicine, 29, 453–463.
Roy, F. H. (2012). Ocular differential diagnosis. Clayton, Panama: Jaypee–Highlights Medical Publishers, Inc.
Myoclonus
Myoclonus — sudden, shocklike contractions of a single muscle or muscle group — occurs with various neurologic disorders and may herald the onset of a seizure. These contractions may be isolated or repetitive, rhythmic or arrhythmic, symmetrical or asymmetrical, synchronous or asynchronous, and generalized or focal. They may be precipitated by bright flickering lights, a loud sound, or unexpected physical contact. One type, intention myoclonus, is evoked by intentional muscle movement.
Myoclonus occurs normally just before falling asleep and as a part of the natural startle reaction. It also occurs with some poisonings and, rarely, as a complication of hemodialysis.
 EMERGENCY INTERVENTIONS
EMERGENCY INTERVENTIONS
If you observe myoclonus, check for seizure activity. Take the patient’s vital signs to rule out arrhythmias or a blocked airway. Have resuscitation equipment on hand.
If the patient has a seizure, gently help him lie down. Place a pillow or a rolled-up towel under his head to prevent concussion. Loosen constrictive clothing, especially around the neck, and turn his head (gently, if possible) to one side to prevent airway occlusion or aspiration of secretions.

History and Physical Examination
If the patient is stable, evaluate his level of consciousness (LOC) and mental status. Ask about the frequency, severity, location, and circumstances of myoclonus. Has he ever had a seizure? If so, did myoclonus precede it? Is myoclonus ever precipitated by a sensory stimulus? During the physical examination, check for muscle rigidity and wasting, and test deep tendon reflexes.
Medical Causes
Alzheimer’s disease. Generalized myoclonus may occur in advanced stages of Alzheimer’s disease, a slowly progressive dementia. Other late findings include mild choreoathetoid movements, muscle rigidity, bowel and bladder incontinence, delusions, and hallucinations.
Creutzfeldt-Jakob disease. Diffuse myoclonic jerks appear early in Creutzfeldt-Jakob disease, a rapidly progressive dementia. Initially random, they gradually become more rhythmic and symmetrical, usually occurring in response to sensory stimuli. Associated effects include ataxia, aphasia, hearing loss, muscle rigidity and wasting, fasciculations, hemiplegia, and vision disturbances or, possibly, blindness.
Encephalitis (viral). With viral encephalitis, myoclonus is usually intermittent and either localized or generalized. Associated findings vary but may include a rapidly decreasing LOC, a fever, a headache, irritability, nuchal rigidity, vomiting, seizures, aphasia, ataxia, hemiparesis, facial muscle weakness, nystagmus, ocular palsies, and dysphagia.
Encephalopathy. Hepatic encephalopathy occasionally produces myoclonic jerks in association with asterixis and focal or generalized seizures.
Hypoxic encephalopathy may produce generalized myoclonus or seizures almost immediately after restoration of cardiopulmonary function. The patient may also have a residual intention myoclonus.
Uremic encephalopathy commonly produces myoclonic jerks and seizures. Other signs and symptoms include apathy, fatigue, irritability, a headache, confusion, a gradually decreasing LOC, nausea, vomiting, oliguria, edema, and papilledema. The patient may also exhibit elevated blood pressure, dyspnea, arrhythmias, and abnormal respirations.
Epilepsy. With idiopathic epilepsy, localized myoclonus is usually confined to an arm or leg and occurs singly or in short bursts, usually upon awakening. It’s usually more frequent and severe during the prodromal stage of a major generalized seizure, after which it diminishes in frequency and intensity.
Myoclonic jerks are usually the first signs of myoclonic epilepsy, the most common cause of progressive myoclonus. At first, myoclonus is infrequent and localized, but over a period of months, it becomes more frequent and involves the entire body, disrupting voluntary movement (intention myoclonus). As the disease progresses, myoclonus is accompanied by generalized seizures and dementia.
Other Causes
Drug withdrawal. Myoclonus may be seen in patients with alcohol, opioid, or sedative withdrawal or delirium tremens.
Poisoning. Acute intoxication with methyl bromide, bismuth, or strychnine may produce an
